biotecHOPE™ 2023

biotecHOPE™ 2023
Crinecerfont
APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF)
AFM13 IN COMBINATION WITH ALLONK®
Neurocrine Biosciences Announces Positive Top-Line Data from Phase 3 Study of Crinecerfont in Adults for the Treatment of Congenital Adrenal Hyperplasia (CAH)
09/12/23
CAHtalyst™ Met Primary Endpoint Demonstrating a Statistically Significant Decrease from Baseline Daily Glucocorticoid Dose with Androgen Control
Key Secondary Endpoint Achieved Statistically Significant Decrease in Androstenedione at Week 4 versus Placebo
Key Secondary Endpoint Demonstrated a Statistically Significant Number of Patients on Crinecerfont Achieved a Reduction to a Physiologic Glucocorticoid Dose versus Placebo
Crinecerfont Was Generally Well-Tolerated
SAN DIEGO, Sept. 12, 2023 /PRNewswire/ -- Neurocrine Biosciences, Inc. (Nasdaq: NBIX) today announced positive top-line data from the Phase 3 CAHtalyst™ Adult Study evaluating the efficacy, safety, and tolerability of crinecerfont in adults with classic congenital adrenal hyperplasia (CAH) due to 21-hydroxylase deficiency (21-OHD).
The Phase 3 study met its primary endpoint at Week 24, demonstrating that treatment with crinecerfont resulted in a statistically significant percent reduction in daily glucocorticoid (GC) dose versus placebo while maintaining androgen control (p-value <0.0001).
The study also met important key secondary endpoints, with a statistically significant decrease in androstenedione at Week 4 versus placebo (p-value <0.0001). At Week 24, approximately 63% of patients on crinecerfont achieved a reduction to a physiologic GC dose versus approximately 18% on placebo (p-value <0.0001).
Crinecerfont was generally well tolerated. The most common adverse events during the double-blind, placebo-controlled period of the trial were fatigue, headache, and coronavirus infection. There were few serious adverse events, with none assessed as related to crinecerfont.
"I am gratified to see the extremely positive and clinically meaningful results from this study, the largest ever interventional trial conducted in this rare disease. It required a global effort, and the top-line results confirm our confidence in crinecerfont as a potential first-in-class medication and first-ever non-glucocorticoid treatment option for patients living with CAH," said Richard Auchus, M.D., Ph.D., Principal Investigator, Professor of Pharmacology and Internal Medicine, Division of Metabolism, Endocrinology, and Diabetes at the University of Michigan. "It has been 60 years since we've seen a significant treatment advance for patients with CAH, and the data from this study suggest that crinecerfont might improve their outcomes and quality of life."
"CAH patients suffer from a number of debilitating symptoms and have had suboptimal treatment options with existing standard of care for their whole lives. These data, along with data from the open label treatment period, will allow us to proceed with our regulatory submissions to the FDA in 2024 and European Medicines Agency afterwards," said Kevin Gorman, Ph.D., Chief Executive Officer, Neurocrine Biosciences.
"CAH is a difficult disorder to live with for patients and their caregivers, taking a huge toll physically and mentally," said Eiry Roberts, M.D., Chief Medical Officer at Neurocrine Biosciences. "For physicians, the current treatment paradigm is problematic, relying on glucocorticoids for a dual purpose: not only to address the underlying cortisol deficiency but typically at supraphysiologic doses to treat androgen excess resulting in well-known complications over the long-term. The CAHtalyst Phase 3 Adult data bring us one step closer to a new approach to treating CAH with a therapy that has demonstrated the ability to substantially reduce glucocorticoid doses while maintaining or improving androgen control."
Additional information regarding the results from the Phase 3 CAHtalyst study will be discussed at the Morgan Stanley 21st Annual Global Healthcare Conference at 10:50 a.m. Eastern Time on September 12 in New York. The live presentation will be webcast and may be accessed on the Company's website under Investors at www.neurocrine.com.
A replay of the presentation will be available on the website approximately one hour after the conclusion of the event and will be archived for approximately one month. Additional data from the Phase 3 CAHtalyst study will be provided in a peer-reviewed medical journal or at a medical conference at a future date.
Data from the Phase 3 CAHtalyst Pediatric Study will be available, as planned, in early Q4 2023.
About Classic Congenital Adrenal Hyperplasia
Congenital adrenal hyperplasia (CAH) refers to a group of genetic conditions that result in an enzyme deficiency that alters the production of adrenal hormones which are essential for life. Approximately 95% of CAH cases are caused by a mutation that leads to deficiency of the enzyme 21-hydroxylase (21-OHD). In classic CAH, severe deficiency of this enzyme leads to an inability of the adrenal glands to produce cortisol and, in approximately 75% of cases, aldosterone. If left untreated, classic CAH can result in salt wasting, dehydration, and even death.
There are currently no non-glucocorticoid treatments approved by the U.S. Food and Drug Administration (FDA) for classic CAH. Glucocorticoids (GCs), the current standard of care, are used not only to correct the endogenous cortisol deficiency but typically used at greater than physiologic (supraphysiologic) doses to try to suppress the high levels of corticotropin-releasing factor (CRF) and adrenocorticotropic hormone (ACTH) that result in androgen excess. However, glucocorticoid treatment at supraphysiologic doses has been associated with serious and significant complications of steroid excess, including metabolic issues such as weight gain and diabetes, cardiovascular disease, and osteoporosis. Additionally, long-term treatment with supraphysiologic GC doses may have psychological and cognitive impact such as changes in mood and memory. Androgen excess has been associated with abnormal bone growth and development in pediatric patients, female health problems such as acne, excess hair growth and menstrual irregularities, testicular rest tumors in males, and fertility issues in both sexes. To learn more about CAH, click here.
About Crinecerfont
Crinecerfont is an investigational, oral, selective corticotropin-releasing factor type 1 receptor (CRF1) antagonist being developed to reduce and control excess adrenal androgens through a steroid-independent mechanism for the treatment of congenital adrenal hyperplasia (CAH) due to 21-hydroxylase deficiency (21-OHD). Antagonism of CRF type 1 receptors in the pituitary has been shown to decrease adrenocorticotropic hormone (ACTH) levels, which in turn decreases the production of adrenal androgens and potentially the symptoms associated with classic CAH. Our data demonstrates that lowering androgen levels enables lower, more physiologic dosing of glucocorticoids and thus could potentially reduce the complications associated with exposure to greater than normal glucocorticoid doses in patients with classic CAH.
To learn more about crinecerfont, click here.
About the CAHtalyst™ Phase 3 Study in Adults
The CAHtalyst™ Phase 3 global registrational study was designed to evaluate the safety, efficacy, and tolerability of crinecerfont in adults (18 years of age and older) with classic congenital adrenal hyperplasia (CAH) due to 21-OHD. The study enrolled 182 female and male patients with CAH and consisted of a 24-week randomized, double-blind, placebo-controlled period followed by one-year of open-label crinecerfont treatment and optional open-label extension. The study started in December 2020, and the open-label treatment portion is still ongoing.
For more information about the CAHtalyst Phase 3 study in adults, please visit Clinical TrialsAdult.gov.
For more information about the CAHtalyst Pediatric Phase 3 study, please visit ClinicalTrialsPediatric.gov.
About Neurocrine Biosciences
Neurocrine Biosciences is a leading neuroscience-focused, biopharmaceutical company with a simple purpose: to relieve suffering for people with great needs, but few options. We are dedicated to discovering and developing life-changing treatments for patients with under-addressed neurological, neuroendocrine and neuropsychiatric disorders. The company's diverse portfolio includes FDA-approved treatments for tardive dyskinesia, chorea associated with Huntington's disease, Parkinson's disease, endometriosis* and uterine fibroids*, as well as a robust pipeline including multiple compounds in mid- to late-phase clinical development across our core therapeutic areas. For three decades, we have applied our unique insight into neuroscience and the interconnections between brain and body systems to treat complex conditions. We relentlessly pursue medicines to ease the burden of debilitating diseases and disorders, because you deserve brave science. For more information, visit neurocrine.com, and follow the company on LinkedIn, Twitter, and Facebook.
(*in collaboration with AbbVie)
NEUROCRINE, CAHtalyst, and the Neurocrine logo are registered trademarks of Neurocrine Biosciences, Inc.
View original content to download multimedia:https://www.prnewswire.com/news-releases/neurocrine-biosciences-announces-positive-top-line-data-from-phase-3-study-of-crinecerfont-in-adults-for-the-treatment-of-congenital-adrenal-hyperplasia-cah-301924494.html
SOURCE Neurocrine Biosciences, Inc.
Neurocrine gains after Phase 3 win for genetic disorder drug
Sep. 12, 2023 11:57 AM ET
Neurocrine Biosciences, Inc. (NBIX)
By: Dulan Lokuwithana, SA News Editor
- Neurocrine Biosciences (NASDAQ:NBIX) traded higher Tuesday after announcing that its Phase 3 CAHtalyst trial for crinecerfont met its primary endpoint in adults with classic congenital adrenal hyperplasia (CAH), a group of genetic disorders.
- CAHtalyst was a global registrational study designed to evaluate the corticotropin-releasing factor type 1 receptor (CRF1) antagonist in adults with CAH due to 21-hydroxylase deficiency (21-OHD).
- Glucocorticoids are considered standard care in CAH despite potential implications such as androgen excess, weight gain, and diabetes at high doses.
- https://seekingalpha.com/news/4011036-neurocrine-stock-gains-after-phase-3-win-crinecerfont
- Neurocrine Biosciences, Inc. (NBIX)
- https://www.neurocrine.com/
- https://www.neurocrine.com/pipeline/
- https://seekingalpha.com/symbol/NBIX
AFM13 IN COMBINATION WITH ALLONK®
APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF)
AFM13 IN COMBINATION WITH ALLONK®
AFFIMED RECEIVES FDA FAST TRACK DESIGNATION FOR AFM13 IN COMBINATION WITH ALLONK® FOR THE TREATMENT OF PATIENTS WITH RELAPSED OR REFRACTORY HODGKIN LYMPHOMA
Press Release - September 12, 2023
- AFM13 in combination with AlloNK® (also known as AB-101) will be investigated in the LuminICE-203 open-label, multi-center, multi-cohort, phase 2 study evaluating the efficacy and safety of the treatment in patients with relapsed/refractory Hodgkin lymphoma
- The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need
Mannheim, Germany, September 12, 2023 – Affimed N.V. (Nasdaq: AFMD) (“Affimed”, or the “Company”), a clinical-stage immuno-oncology company committed to giving patients back their innate ability to fight cancer, today announced that the FDA has granted fast track designation to the combination of its innate cell engager (ICE®) AFM13 with AlloNK® for the potential treatment of relapsed/refractory (r/r) Hodgkin lymphoma (HL). The combination treatment is entering Phase 2 development and will be investigated in Affimed’s LuminICE-203 study (NCT05883449), which received IND-clearance earlier this year; the study also includes an exploratory cohort of CD30-positive peripheral T-cell lymphoma patients.
“Our clinical data of AFM13 in combination with allogeneic NK cells has shown outstanding efficacy and a well-managed safety profile in late-stage, muti-refractory, patients with r/r Hodgkin and Non-Hodgkin lymphoma,” said Dr. Wolfgang Fischer, Chief Operating Officer at Affimed. “The FDA fast track designation is a testament to the powerful potential our combination approach may deliver for these patients in high need, and we remain committed to working closely with the FDA to expedite development of this important therapy.”
Fast Track is a process designed to facilitate the development, and expedite the review, of new drugs that are intended to treat or prevent serious conditions and have the potential to address an unmet medical need. The FDA’s decision is based on available data showing the potential of the AFM13 and AlloNK® combination therapy to overcome current limitations in the treatment of r/r HL. With the Fast Track Designation, the therapeutic development of the combination can benefit from more frequent engagement with the FDA, which will support the collection of appropriate data needed to accelerate its development.
LuminICE-203 builds on the clinical findings from the phase 1/2 AFM13-104 trial (NCT04074746), in which investigators assessed AFM13 in combination with cord blood-derived natural killer cells in heavily pretreated patients with CD30-positive Hodgkin lymphoma and non-Hodgkin lymphoma. Data presented to date from this trial have shown outstanding clinical results in late-stage, multi-refractory, patients with a 94% overall response rate (ORR), a 71% complete response (CR) rate and a well-managed safety profile at the recommended phase 2 dose (RP2D); specifically in the 31 r/r HL patients treated, the ORR and CR were 97% and 77% respectively (see press release here).
About FDA Fast Track Designation
Fast track is a process designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need. Its purpose is to get important new drugs to patients earlier. Fast Track addresses a broad range of serious conditions. With Fast Track Designation, a new therapy is eligible for some or all of the following:
- More frequent meetings with FDA to discuss the drug’s development plan and ensure collection of appropriate data needed to support drug approval
- More frequent written communication from FDA about such things as the design of the proposed clinical trials and use of biomarkers
- Eligibility for Accelerated Approval and Priority Review, if relevant criteria are met
- Rolling Review, which means that a drug company can submit completed sections of its Biologic License Application (BLA) or New Drug Application (NDA) for review by FDA, rather than waiting until every section of the NDA is completed before the entire application can be reviewed. BLA or NDA review usually does not begin until the drug company has submitted the entire application to the FDA.
Please refer to Fast Track | FDA for further information.
About AFM13
AFM13 is a first-in-class innate cell engager (ICE®) that uniquely activates the innate immune system to destroy CD30-positive hematologic tumors. AFM13 induces specific and selective killing of CD30-positive tumor cells, leveraging the power of the innate immune system by engaging and activating natural killer (NK) cells and macrophages. AFM13 is Affimed’s most advanced ICE® clinical program and was evaluated as monotherapy in a phase 2B trial in patients with relapsed/refractory peripheral T cell lymphoma (REDIRECT). Additional details can be found at www.clinicaltrials.gov (NCT04101331). The study achieved an ORR of 32.4% demonstrating anti-tumor activity with a DOR of 2.3 months and a well-managed safety profile. AFM13 is a tetravalent bispecific innate cell engager designed to act as a bridge between the innate immune cells and the tumor creating the necessary proximity for the innate immune cells to specifically destroy the tumor cells. About Affimed N.V. Affimed (Nasdaq: AFMD) is a clinical-stage immuno-oncology company committed to giving patients back their innate ability to fight cancer by actualizing the untapped potential of the innate immune system. The Company’s proprietary ROCK® platform enables a tumor-targeted approach to recognize and kill a range of hematologic and solid tumors, enabling a broad pipeline of wholly-owned and partnered single agent and combination therapy programs. The ROCK® platform predictably generates customized innate cell engager (ICE®) molecules, which use patients’ immune cells to destroy tumor cells. This innovative approach enabled Affimed to become the first company with a clinical-stage ICE®. Headquartered in Mannheim, Germany, with offices in New York, NY, Affimed is led by an experienced team of biotechnology and pharmaceutical leaders united by a bold vision to stop cancer from ever derailing patients’ lives. For more about the Company’s people, pipeline and partners, please visit: www.affimed.com
About AlloNK®
AlloNK® (also known as AB-101) is a non-genetically modified, cord blood-derived, allogeneic, cryopreserved, ADCC-enhancing NK cell therapy candidate for use in combination with monoclonal antibodies or innate-cell engagers in the out-patient setting. Artiva is investigating AlloNK® in a Phase 1/2 multicenter clinical trial (ClinicalTrials.gov Identifier: NCT04673617 ) to assess the safety and clinical activity of AlloNK® alone and in combination with the anti-CD20 monoclonal antibody, rituximab, in patients with relapsed or refractory B-cell-non-Hodgkin lymphoma (B-NHL). Artiva is also investigating the safety and clinical activity of AlloNK® in combination with rituximab in patients with lupus nephritis. Artiva selects cord blood units with the high affinity variant of the CD16 receptor and a KIR-B haplotype for enhanced product activity. Using the company’s cell therapy manufacturing platform, Artiva can generate thousands of doses of AlloNK® from a single umbilical cord blood unit while retaining the high and consistent expression of CD16 and other activating NK receptors, without the need for engineering. AlloNK® is being administered in the outpatient setting over multiple doses and multiple cycles.
About Artiva Biotherapeutics
Artiva’s mission is to deliver highly effective, off-the-shelf, allogeneic NK cell-based therapies that are safe and accessible to patients. Artiva has taken a Manufacturing-First approach to create a highly scaled process integrating cell expansion, activation, and engineering technology developed by Artiva’s strategic partner, GC Cell Corporation, a member of the GC family of companies, a leading healthcare company in Korea. Artiva’s pipeline includes AlloNK®, an ADCC enhancer NK-cell therapy candidate for use in combination with monoclonal antibodies or innate-cell engagers. Artiva’s pipeline also includes AB-201, an anti-HER2 CAR-NK cell therapy candidate for the treatment of HER2-overexpressing tumors, such as breast, gastric, and bladder cancers, and for which an IND has been allowed by FDA, and a pipeline of CAR-NK candidates. Artiva is headquartered in San Diego. For more information, visit www.artivabio.com.
Affimed gains on FDA fast track tag for lymphoma therapy
Sep. 12, 2023 7:20 AM ET
By: Dulan Lokuwithana, SA News Editor
- German biotech Affimed N.V. (NASDAQ:AFMD) added ~10% pre-market Tuesday after announcing that the U.S. Food and Drug Administration (FDA) issued its fast-track designation for an experimental therapy for Hodgkin lymphoma.
- The treatment is composed of Affimed’s (AFMD) innate cell engager (ICE) AFM13 and Artiva Biotherapeutics’ (RTVA) NK cell therapy candidate AlloNK. The fast track designation covers its use in relapsed/refractory (r/r) Hodgkin lymphoma (HL).
- A Phase 2 trial, known as LuminICE-203, is expected to test the combo in patients with r/r HL and those with CD30-positive peripheral T-cell lymphoma.
- https://seekingalpha.com/news/4010889-affimed-stock-gains-fda-fast-track-tag-lymphoma-drug
- Affimed N.V. (AFMD), RTVA
- https://www.affimed.com/
- https://www.affimed.com/pipeline/
APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF)
APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF)
APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF)
BioLineRx Announces FDA Approval of APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF) to Mobilize Hematopoietic Stem Cells for Collection and Subsequent Autologous Transplantation in Patients with Multiple Myeloma
September 11, 2023
- APHEXDA is the first innovation in stem cell mobilization for multiple myeloma to be approved in the U.S. in a decade -
- One dosage of APHEXDA plus filgrastim enabled a majority of patients to achieve the collection goal of ≥ 6 million hematopoietic stem cells among a contemporary population of multiple myeloma patients -
- Management to hold conference call on Tuesday, September 12, 2023 at 8:00 a.m. U.S. EDT -
TEL AVIV, Israel, Sept. 11, 2023 /PRNewswire/ -- BioLineRx Ltd. (NASDAQ/TASE: BLRX), a commercial stage biopharmaceutical company focused on certain cancers and rare diseases, today announced that the U.S. Food and Drug Administration (FDA) has approved APHEXDA™ (motixafortide) in combination with filgrastim (G-CSF) to mobilize hematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation in patients with multiple myeloma. APHEXDA is administered by injection, for subcutaneous use.
Experience the full interactive Multichannel News Release here: https://www.multivu.com/players/English/9174951-biolinerx-fda-approval-aphexda/
Multiple myeloma is the second most-common hematologic malignancy. Autologous stem cell transplantation (ASCT) is part of the standard of care treatment paradigm for multiple myeloma and delivers prolonged survival for patients with this cancer type.1 The success of ASCT depends on adequate mobilization of stem cells during the treatment process. The American Society for Transplantation and Cellular Therapy (ASTCT) guidelines recommend a collection target of 3-5 x 106 CD34+ cells/kg.2 Additionally, collection of a sufficient number of stem cells to perform two transplantations is recommended.2-5 Historically, depending on induction regimens and mobilization strategies, up to 47% of patients have had challenges collecting target numbers of hematopoietic stem cells for ASCT after one apheresis session.6-7
"Greater numbers of patients with multiple myeloma are candidates for autologous stem cell therapy; however, achieving target collection goals can be difficult in some patients given modern barriers, including the treatment of older patients and use of contemporary induction regimens," said John DiPersio, MD, PhD, primary investigator for the GENESIS trial and
Professor of Medicine, Pathology and Immunology and Director of the Center for Gene and Cellular Immunotherapy at Washington University School of Medicine in St. Louis. "Innovation in this area of medicine has been needed, and today's approval of APHEXDA addresses the demand for new therapies that can meet today's challenges by delivering more reliability in stem cell mobilization, versus filgrastim alone, with fewer days of apheresis sessions and fewer doses of filgrastim for people living with this cancer."
The FDA approval of APHEXDA is based on results from the 2-part, Phase 3 GENESIS trial, a randomized, double-blind, placebo-controlled study evaluating the safety and efficacy of APHEXDA (motixafortide) plus filgrastim, compared to placebo plus filgrastim, for the mobilization of hematopoietic stem cells for autologous transplantation in multiple myeloma patients. Part 1 was a single center, lead-in, open-label study involving 12 patients treated with motixafortide plus filgrastim designed to ascertain the dose. Part 2 involved 122 patients who were randomized 2:1 in a double-blind, placebo-controlled, multicenter study.8
The assessment of CD34+ cells was performed by central and local laboratories. Central laboratory assessments were used for the efficacy results. Local laboratory results were used for clinical treatment decisions. APHEXDA plus filgrastim enabled 67.5% of patients to achieve the stem cell collection goal of ≥ 6 × 106 CD34+ cells/kg within two apheresis sessions, versus 9.5% for the placebo plus filgrastim regimen, as measured by central laboratory.9 Additionally, 92.5% of patients reached the stem cell collection goal in up to two apheresis sessions in the APHEXDA arm and 21.4% in the placebo arm, as measured by local laboratories.9 Local laboratory data were used for a sensitivity analysis. The data are descriptive and were not statistically powered nor prespecified. The information should be cautiously interpreted.
In GENESIS, the safety was evaluated in 92 patients with multiple myeloma who received APHEXDA 1.25 mg/kg subcutaneously plus filgrastim, and 42 patients who received placebo plus filgrastim. Serious adverse reactions occurred in 5.4% of patients receiving APHEXDA plus filgrastim. These reactions included vomiting, injection site reaction, hypersensitivity reaction, injection site cellulitis, hypokalemia and hypoxia. The most common adverse reactions occurring in GENESIS (incidence >20%) were injection site reactions (pain, erythema and pruritus), pruritus, flushing, and back pain.9
"Given the strong efficacy data shown in the GENESIS trial, which included patients who are representative of the current multiple myeloma patient population, we believe APHEXDA will play a critical role in addressing unmet needs and introduce a new treatment paradigm for this challenging cancer," said Philip Serlin, Chief Executive Officer of BioLineRx Ltd. "The company is working relentlessly to make this important innovation in stem cell mobilization available to appropriate patients, their physicians and transplant teams."
"FDA approval of APHEXDA, the company's first approved therapeutic, is a tremendously exciting and important moment in our history and validates our drug development programs," said Ella Sorani, PhD, Chief Development Officer of BioLineRx Ltd. "We would like to thank all of the patients and families who have contributed to the research and development of APHEXDA."
Increased age, as well as exposure to lenalidomide-containing induction regimens, including 3-4 drug combination regimens, have been associated with impaired stem cell mobilization.2-3 The GENESIS study included patients considered representative of the typical multiple myeloma population undergoing ASCT, with a median age of 63 years and with ~70% of patients in both arms of the trial receiving lenalidomide-containing induction therapy.8 In this contemporary population, patients in the APHEXDA plus filgrastim arm were able to mobilize more than four times the amount of stem cells with a single dose over a 24-hour period compared with placebo plus filgrastim.8
BioLineRx expects to make APHEXDA available later this month. For further information about APHEXDA, please see the Important Safety Information below and the full Prescribing Information, and visit www.APHEXDA.com.
APHEXDA Investor Conference Call
The Company will host an investor conference call on September 12, 2023 at 8:00 a.m. EDT featuring remarks by Philip Serlin, Chief Executive Officer.
To access the conference call, please dial +1-888-281-1167 from the U.S. or +972-3-918-0685 internationally. A live webcast and a replay of the call can be accessed through the event page on the Company's website. Please allow extra time prior to the call to visit the site and download any necessary software to listen to the live broadcast. The call replay will be available approximately two hours after completion of the live conference call. A dial-in replay of the call will be available until September 14, 2023; please dial +1-888-295-2634 from the US or +972-3-925-5904 internationally.
About Multiple Myeloma
Multiple myeloma is an incurable blood cancer that affects some white blood cells called plasma cells, which are found in the bone marrow. When damaged, these plasma cells rapidly spread and replace normal cells in the bone marrow. According to the American Cancer Society, in 2023, it is estimated that more than 35,000 people will be diagnosed with multiple myeloma, and nearly 13,000 people will die from the disease in the U.S.10 While some people diagnosed with multiple myeloma initially have no symptoms, most patients are diagnosed due to symptoms that can include bone fracture or pain, low red blood cell counts, tiredness, high calcium levels, kidney problems, or infections.
About Autologous Stem Cell Transplantation
Autologous stem cell transplantation (ASCT) is part of the standard treatment paradigm for a number of blood cancers, including multiple myeloma. In the U.S., as many as 8,000 ASCTs are performed each year in patients with multiple myeloma.11 The current ASCT standard of care includes 4-6 cycles of induction therapy (an initial drug-combination regimen to position the patient for as deep a treatment response as possible). To begin the stem cell mobilization process, a patient will receive a daily dose of filgrastim (G-CSF) for four days. Daily doses of filgrastim will continue until the target collection goal is met with the addition of up to four daily doses of plerixafor as needed.12 For patients unable to mobilize sufficient numbers of cells for harvesting during this primary mobilization phase, rescue therapy may be carried out followed by an additional number of apheresis sessions as necessary.2
About the GENESIS Trial
GENESIS (NCT 03246529) is a 2-part, Phase-3, randomized, double-blind, placebo-controlled, multicenter study evaluating the safety and efficacy of APHEXDA (motixafortide) plus filgrastim (G-CSF), compared to placebo plus filgrastim, for the mobilization of hematopoietic stem cells for autologous transplantation in multiple myeloma patients. Part 1 was a single center, lead-in, open-label study involving 12 patients treated with motixafortide plus filgrastim designed to ascertain the dose. Part 2 involved 122 patients who were randomized 2:1 in a double-blind, placebo-controlled, multicenter study.8
The primary objective of the study was to evaluate if one dose of motixafortide plus filgrastim is superior to placebo plus filgrastim in the ability to mobilize ≥ 6 million CD34+ cells in up to two apheresis sessions. A key secondary objective of the study was to evaluate if one dose of motixafortide plus filgrastim is superior to placebo plus filgrastim in the ability to mobilize ≥ 6 million CD34+ cells in one apheresis session.8
The study met the primary endpoint with a high degree of statistical significance (p<0.0001). The assessment of CD34+ cells was performed by central and local laboratories. Central laboratory assessments were used for the efficacy results. Local laboratory results were used for clinical treatment decisions. APHEXDA plus filgrastim enabled 67.5% of patients to achieve the cell collection goal of ≥ 6 × 106 CD34+ cells/kg in up to two apheresis sessions with a single administration, versus 9.5% for the placebo plus filgrastim regimen, as measured by central laboratory.9 Additionally, 92.5% of patients reached the stem cell collection goal in up to two apheresis sessions in the APHEXDA arm and 21.4% in the placebo arm, as measured by local laboratories.13 Local laboratory data were used for a sensitivity analysis. The data are descriptive and were not statistically powered nor prespecified. The information should be cautiously interpreted.
The safety of APHEXDA was evaluated in 92 patients with multiple myeloma who received APHEXDA 1.25 mg/kg subcutaneously plus filgrastim and 42 patients who received placebo plus filgrastim for mobilization of hematopoietic stem cells for collection and apheresis. Serious adverse reactions occurred in 5.4% of patients receiving APHEXDA plus filgrastim. Serious adverse reactions included vomiting, injection site reaction, hypersensitivity reaction, injection site cellulitis, hypokalemia and hypoxia. The most common adverse reactions occurring in GENESIS (incidence >20%) were injection site reactions (pain, erythema, and pruritus), pruritus, flushing and back pain.9
Please see important safety information below.
About APHEXDA™
APHEXDA (motixafortide) is a CXCR4 antagonist with long receptor occupancy (greater than 72 hours) that, in combination with filgrastim (G-CSF), enables mobilization of hematopoietic stem cells to the peripheral blood for collection and subsequent autologous stem cell transplantation in patients with multiple myeloma.9
INDICATION AND IMPORTANT SAFETY INFORMATION
INDICATION
APHEXDA is indicated in combination with filgrastim (G-CSF) to mobilize hematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation in patients with multiple myeloma.
https://biolinerx.com/motixafortide-in-hsc-mobilization/
Please see the accompanying full Prescribing Information.
About BioLineRx
BioLineRx Ltd. (NASDAQ/TASE: BLRX) is a commercial stage biopharmaceutical company pursuing life-changing therapies for certain cancers and rare diseases. The company's first approved product is APHEXDA™ (motixafortide) with an indication in the U.S. for stem cell mobilization for autologous transplantation in multiple myeloma. BioLineRx is advancing a pipeline of investigational medicines for patients with sickle cell disease, pancreatic cancer, and other solid tumors. Headquartered in Israel, and with operations in the U.S., the company is driving innovative therapeutics with end-to-end expertise in development and commercialization, ensuring life-changing discoveries move beyond the bench to the bedside.
Learn more about who we are, what we do, and how we do it at www.biolinerx.com, or on Twitter and LinkedIn.
Cision View original content:
SOURCE BioLineRx Ltd.
BioLineRx gains after winning first FDA approval
Sep. 11, 2023 7:47 AM ET
BioLineRx Ltd. (BLRX)By: Dulan Lokuwithana, SA News Editor
- Israel-based biotech BioLineRx Ltd. (NASDAQ:BLRX) added ~23% pre-market Monday after announcing that the FDA greenlighted its lead asset Aphexda (motixafortide) for patients with multiple myeloma, marking the company's first regulatory approval.
- Accordingly, the subcutaneous injection will be indicated in the U.S. with filgrastim for multiple myeloma patients to mobilize hematopoietic stem cells to the peripheral blood. The company expects to launch the product later this month.
- https://seekingalpha.com/news/4010520-biolinerx-stock-gains-first-fda-approva
- BioLineRx Ltd. (BLRX)
- https://ir.biolinerx.com/
- https://biolinerx.com/pipeline/
- https://biolinerx.com/motixafortide-in-hsc-mobilization/
PALTUSOTINE (ORAL SST2 AGONIST)
PALTUSOTINE (ORAL SST2 AGONIST)
APHEXDA™ (motixafortide) in Combination with Filgrastim (G-CSF)
CRINETICS’ ONCE-DAILY ORAL PALTUSOTINE ACHIEVED THE PRIMARY AND ALL SECONDARY ENDPOINTS IN THE PHASE 3 PATHFNDR-1 STUDY EVALUATING TREATMENT OF PATIENTS WITH ACROMEGALY
- 83% of Participants on Paltusotine Maintained IGF-1 ≤1.0 xULN vs. 4% on placebo (p<0.0001)
- Mean IGF-1 Levels Were Maintained on Paltusotine vs. an Increase on Placebo (p<0.0001) After Switching from Injected Depot Standard of Care
- Mean Acromegaly Symptom Diary Scores Were Maintained on Paltusotine vs. an Increase on Placebo (p=0.02) After Switching from Injected Depot Standard of Care
- Paltusotine Was Well-Tolerated with No Severe or Serious Adverse Events
- Management Will Host a Conference Call Monday, September 11, 2023 at 8:00 a.m. Eastern Time
SAN DIEGO, September 10, 2023 — Crinetics Pharmaceuticals, Inc. (Nasdaq: CRNX) today announced that paltusotine, an oral, once-daily investigational compound, achieved positive results by meeting the primary endpoint and all secondary endpoints of the Phase 3 PATHFNDR-1 study (NCT04837040). PATHFNDR-1 was a randomized, double-blind, placebo-controlled 36-week treatment period followed by an optional open-label extension study evaluating paltusotine in participants with acromegaly switching from standard-of-care injected depot somatostatin analogs. The study enrolled participants with acromegaly who were biochemically controlled on octreotide or lanreotide depot monotherapy. PATHFNDR-1 is one of two ongoing, placebo-controlled Phase 3 studies of once-daily, oral paltusotine.
The study met statistical significance (p<0.0001) on the primary endpoint, based on the proportion of participants taking paltusotine (83%) who maintained an insulin-like growth factor 1 (IGF-1) level ≤ 1.0 times the upper limit of normal (xULN) compared to those taking placebo (4%). All secondary endpoints also met statistical significance:
“The results of PATHFNDR-1 are relevant to the patients we see every day in clinical practice who are biochemically controlled on standard-of-care injections. My colleagues and I are increasingly convinced many patients would appreciate an oral alternative which confers similar benefits without the burden and discomfort of the injections,” stated Monica R. Gadelha, M.D., Ph.D., professor of endocrinology at the Medical School of the Universidade Federal do Rio de Janeiro and a principal investigator in the PATHFNDR program. “This study demonstrated that the transition to paltusotine was done seamlessly and the results showed once-daily, oral paltusotine maintained both symptom control as well as biochemical control when switching from monthly injections.”
In PATHFNDR-1, paltusotine was well tolerated and no serious or severe adverse events were reported in participants treated with paltusotine. The frequency of participants with at least one treatment emergent adverse event (TEAE) was comparable in the paltusotine (PAL) treatment arm vs placebo (PBO) arm (80% vs. 100% respectively). The most commonly reported TEAEs in paltusotine included: arthralgia (27% PAL vs. 57% PBO), headache (20% PAL vs. 36% PBO), diarrhea (23% PAL vs. 14% PBO), abdominal pain (17% PAL vs. 11% PBO) and nausea (10% PAL vs. 7% PBO). The frequency of adverse events considered related to acromegaly was notably lower in paltusotine treated participants compared to placebo treated participants (30% vs. 86% respectively).
“We designed paltusotine to be the preferred therapeutic option for people living with acromegaly. We could not be more excited by the results from PATHFNDR-1, which further reinforce our conviction that, if approved, paltusotine could address patients’ unmet need for a simple, oral, once-daily therapy. These data showed that upon switching from injected standard of care, paltusotine provided reliable, durable control of their disease. We intend to seek regulatory approval as quickly as possible once we complete the PATHFNDR-2 study early next year,” said Scott Struthers, Ph.D., founder and chief executive officer of Crinetics. “I would like to express my deep gratitude to the study participants, clinical staff, and Crinetics’ employees around the world who contributed to the success of this high-quality clinical study and who have worked so hard to bring this potential medicine for people living with acromegaly one major step closer to fruition.”
“These robust results for paltusotine reaffirm the strength of Crinetics’ core platform for creating high quality, small molecule, oral drugs that act at G-protein coupled receptors,” added Stephen Betz, Ph.D., founder and chief scientific officer of Crinetics. “I am extremely excited to continue to explore the utility of paltusotine for the treatment of carcinoid syndrome, as well as advance the rest of our innovative pipeline of internally discovered investigational compounds for people who live with other endocrine diseases including congenital adrenal hyperplasia, Cushing’s disease, hyperparathyroidism, Graves’ disease, hyperinsulinism, diabetes, and obesity. Paltusotine is an important lead program, and we’re just getting started.”
A full analysis of the PATHFNDR-1 results is underway, which the Company expects to present at upcoming scientific conferences. PATHFNDR-2, a Phase 3 study of oral paltusotine in participants with acromegaly who are treatment-naïve or not currently receiving medical therapy, is fully enrolled and topline data are expected in the first quarter of 2024. Pending successful findings from the PATHFNDR-2 study, Crinetics plans to submit a new drug application to the U.S. Food and Drug Administration in 2024 seeking regulatory approval for all acromegaly patients who require pharmacotherapy, including newly diagnosed patients and those switching from other therapies.
The Company is also conducting an open-label Phase 2 study to evaluate paltusotine in patients with carcinoid syndrome and intends to report preliminary results later this year.
DATA REVIEW CONFERENCE CALL
Crinetics will hold a conference call and live webcast on Monday, September 11, 2023 at 8:00 a.m. Eastern Time to discuss topline results from the PATHFNDR-1 study. To participate, please dial 1-877-451-6152 (domestic) or 1-201-389-0879 (international) and refer to conference ID 13740941. To access the webcast, click here. Following the live event, a replay will be available on the of the Company’s website.
ABOUT THE PATHFNDR PROGRAM
The PATHFNDR Program consists of two Phase 3 double-blind, placebo-controlled studies. PATHFNDR-1 (NCT04837040) enrolled a total of 58 adults with acromegaly who entered with an IGF-1 level ≤ 1.0x ULN on octreotide or lanreotide depot monotherapy. They were randomized to receive once-daily, oral paltusotine for 36 weeks or placebo. PATHFNDR-2 (NCT05192382) enrolled 112 adults with acromegaly who had elevated IGF-1 levels but were medication naïve or were not being treated with pharmacotherapy (untreated patients).
The primary endpoint for both studies is the proportion of patients achieving IGF-1 ≤1.0 xULN compared to placebo. If successful, Crinetics believes these studies could support registration of paltusotine in the United States and Europe for all acromegaly patients who require pharmacotherapy, including untreated patients and those switching from standard of care.
ABOUT ACROMEGALY
Acromegaly is a serious rare disease generally caused by a pituitary adenoma, a benign tumor in the pituitary that secretes growth hormone (GH). Excess GH secretion causes excess secretion of IGF-1 from the liver. Prolonged exposure to increased levels of IGF-1 and GH leads to progressive and serious systemic complications, often resulting in bone, joint, cardiovascular, metabolic, cerebrovascular, or respiratory disease. Acromegaly symptoms include headache, joint aches, fatigue, sleep apnea, severe sweating, hyperhidrosis/oily skin, bone and cartilage overgrowth, abnormal growth of hands and feet, enlargement of heart, liver, and other organs and alteration of facial features. Uncontrolled acromegaly results in increased mortality and has a debilitating impact on daily functioning and quality of life.
Surgical removal of pituitary adenomas, if possible, is the preferred initial treatment for most acromegaly patients. Pharmacotherapy is used for patients who are not candidates for surgery, or when surgery is unsuccessful in achieving treatment goals. Approximately 50% of patients with acromegaly prove to be candidates for pharmacotherapy. Injectable depot somatostatin analogues are the most common initial pharmacologic treatment; however, these drugs require monthly depot injections with large gauge needles that are commonly associated with pain, injection site reactions, and an increased burden on the lives of patients.
ABOUT PALTUSOTINE
Paltusotine is the first oral, once-daily selectively targeted somatostatin receptor type 2 (SST2) agonist and is currently in Phase 3 investigational studies. It was designed by the Crinetics discovery team to provide an efficacious and convenient once-daily option for people living with acromegaly and neuroendocrine tumors. In Phase 2 studies and the recently completed PATHFNDR-1 Phase 3 study, paltusotine maintained IGF-1 levels in acromegaly patients who switched from monthly injectable medications to paltusotine. IGF-1 is the primary biomarker endocrinologists use to manage their acromegaly patients.
ABOUT CRINETICS PHARMACEUTICALS
Crinetics Pharmaceuticals is a clinical stage pharmaceutical company focused on the discovery, development, and commercialization of novel therapeutics for endocrine diseases and endocrine-related tumors. Paltusotine, an investigational, first-in-class, oral somatostatin receptor type 2 (SST2) agonist, is in Phase 3 clinical development for acromegaly and Phase 2 clinical development for carcinoid syndrome associated with neuroendocrine tumors. Crinetics has demonstrated pharmacologic proof-of-concept in a Phase 1 clinical study for CRN04894 a first-in-class, investigational, oral ACTH antagonist, that is currently in Phase 2 clinical studies for the treatment of Cushing’s disease and congenital adrenal hyperplasia. All of the Company’s drug candidates are orally delivered, small molecule new chemical entities resulting from in-house drug discovery efforts, including additional discovery programs addressing a variety of endocrine conditions such as hyperparathyroidism, polycystic kidney disease, Graves’ disease, thyroid eye disease, hyperinsulinism, diabetes and obesity.
Source: Crinetics Pharmaceuticals, Inc.

Crinetics climbs as lead asset succeeds in Phase 3 trial for acromegaly
Sep. 11, 2023 6:53 AM ET
Crinetics Pharmaceuticals, Inc. (CRNX)
By: Dulan Lokuwithana, SA News Editor
- Crinetics Pharmaceuticals (NASDAQ:CRNX) added ~74% pre-market Monday after announcing that its lead candidate, paltusotine, achieved the primary endpoint and all secondary endpoints in a Phase 3 trial for patients with the rare disease acromegaly.
- https://seekingalpha.com/news/4010493-crinetics-stock-climbs-paltusotine-succeeds-acromegaly
- Crinetics Pharmaceuticals, Inc. (CRNX)
- https://crinetics.com/
- https://crinetics.com/pipeline/paltusotine-acromegaly-nets-carcinoid-syndrome/
INO-3107
PALTUSOTINE (ORAL SST2 AGONIST)
Zilebesiran (ALN-AGT)
INOVIO Announces U.S. FDA Breakthrough Therapy Designation Granted for INO-3107 for the Treatment of Recurrent Respiratory Papillomatosis
September 07, 2023
DownloadPDF Format (opens in new window)
• Designation based on clinical evidence indicating INO-3107 may demonstrate substantial improvement over existing therapies
• First Breakthrough Therapy designation for an INOVIO DNA medicine candidate
PLYMOUTH MEETING, Pa., Sept. 7, 2023 /PRNewswire/ -- INOVIO (NASDAQ:INO), a biotechnology company focused on developing and commercializing DNA medicines to help treat and protect people from HPV-related diseases, cancer, and infectious diseases, today announced that the U.S. Food and Drug Administration (FDA) has granted Breakthrough Therapy designation for INO-3107 as a potential treatment for patients with Recurrent Respiratory Papillomatosis (RRP). The FDA's Breakthrough Therapy designation is a process designed to expedite the development and review of drug candidates that are intended to treat a serious or life-threatening condition and for which preliminary clinical evidence indicates that the drug may demonstrate substantial improvement over available therapy on a clinically significant endpoint(s).
"This is yet another important step for INO-3107 and recognition that this first-in-class DNA medicine candidate has the potential to improve the lives of patients with RRP," said INOVIO's President and Chief Executive Officer, Dr. Jacqueline Shea. "As we recently announced, we have been interacting with the FDA with the goal to launch a pivotal trial for INO-3107 in the near term. With this Breakthrough Therapy designation, we look forward to continuing to work with the agency so that we can generate the evidence needed to support approval of INO-3107 as quickly and efficiently as possible, with an ultimate aim to help RRP patients and deliver on the promise of DNA medicine."
The President of the Recurrent Respiratory Papillomatosis Foundation, Kim McClellan, said: "RRP patients will tell you that even one reduction in the number of disruptive, invasive surgeries they face would be life-changing. The potential impact of this treatment gives me great hope for the future and I'm happy to see that RRP is finally getting the attention it deserves."
INO-3107 is an investigational DNA medicine candidate designed to elicit a targeted T cell response against HPV-6 and HPV-11, the HPV types that cause RRP and other HPV-related disease. This Breakthrough Therapy designation for INO-3107 follows receipt of Orphan Drug designation from the European Commission in May 2023 and from the FDA in 2020.
INOVIO plans to initiate a pivotal trial of INO-3107 in the first quarter of 2024, subject to FDA clearance. As part of its development efforts, the company has engaged a leading Clinical Research Organization to help run the pivotal trial, as well as key opinion leaders and investigators interested in developing a new treatment option for RRP patients.
The Breakthrough Therapy designation is supported by data from INOVIO's completed Phase 1/2 open-label, multicenter trial that assessed INO-3107's safety, tolerability, immunogenicity, and efficacy in patients with HPV-6 and/or HPV-11-related RRP (NCT:04398433). Overall, 81.3% (26/32) patients in the trial had a decrease in surgical interventions in the year after INO-3107 administration compared to the prior year, including 28.1% (9/32) that required no surgical intervention during or after the dosing window. Patients in the trial had a median range of 4 surgeries (2-8) in the year prior to dosing. After dosing, there was a median decrease of 3 surgical interventions (95% confidence interval -3, -2). Patients received four doses of INO-3107 on Day 0, and Weeks 3, 6, and 9. At the outset of the study (Day 0), patients could have RRP tissue surgically removed, but any surgery performed after Day 0 during the dosing window was counted against the efficacy endpoint. INO-3107 was well-tolerated by participants in the trial.
Data from this Phase 1/2 trial has been presented at scientific and medical conferences, including the 2023 Annual Meeting of the American Broncho-Esophageal Association (ABEA) in May and at the European Laryngological Association's Annual Meeting in June. Data from the trial was also published in May in the peer-reviewed journal, The Laryngoscope, under the title "Interim Results of a Phase 1/2 Open-Label Study of INO-3107 for HPV-6 and/or HPV-11–Associated RRP." The Laryngoscope is the official journal of the Triological Society (TRIO), the American Laryngological Association (ALA), and the ABEA.
About RRP
RRP is a debilitating and rare disease caused primarily by HPV-6 and/or HPV-11. RRP is characterized by the development of small, wart-like growths, or papillomas, in the respiratory tract. While papillomas are generally benign, they can cause severe, life-threatening airway obstruction and respiratory complications. RRP can also significantly affect quality of life for patients by affecting the voice box, limiting the ability to speak effectively. Surgery to remove papillomas is the standard of care for RRP; however, the papillomas often grow back because the underlying HPV infection has not been eradicated.
The most widely cited U.S. epidemiology data published in 1995 estimated that there were 14,000 active cases and about 1.8 per 100,000 new cases in adults each year. More recent pediatric epidemiology data cites a range of 0.5 - 0.7 per 100,000 new cases in children in the U.S. each year.
About INO-3107
INO-3107 is INOVIO's clinical-stage DNA medicine product candidate being developed as a potential treatment for RRP. INO-3107 is designed to elicit a targeted T cell response against HPV-6 and HPV-11, the HPV types responsible for causing RRP among other HPV-related diseases. These targeted T cells are designed to seek out and kill infected cells, with the aim of potentially preventing or slowing the growth of new papillomas. INO-3107 received Orphan Drug designation from the European Commission in May 2023 and from the U.S. Food and Drug Administration in 2020. For more information about our HPV franchise, please visit https://ir.inovio.com/events-and-presentations/default.aspx.
About INOVIO
INOVIO is a biotechnology company focused on developing and commercializing DNA medicines to help treat and protect people from HPV-related diseases, cancer, and infectious diseases. INOVIO's DNA medicines in development are delivered using its investigational proprietary device, CELLECTRA®, to produce immune responses against targeted pathogens and cancers. For more information, visit www.inovio.com.
View original content:https://www.prnewswire.com/news-releases/inovio-announces-us-fda-breakthrough-therapy-designation-granted-for-ino-3107-for-the-treatment-of-recurrent-respiratory-papillomatosis-301920321.html
SOURCE INOVIO Pharmaceuticals, Inc.
Inovio gains FDA breakthrough status for DNA therapy
Sep. 07, 2023 9:03 AM ET
Inovio Pharmaceuticals, Inc. (INO)
By: Dulan Lokuwithana, SA News Editor4 Comments
- Inovio Pharmaceuticals (NASDAQ:INO) added ~9% pre-market Thursday after the U.S. FDA issued Breakthrough Therapy designation for its experimental DNA medicine INO-3107 as a treatment for the rare disease, recurrent respiratory papillomatosis (RRP).
- With the decision, INO-3107 becomes INO's first DNA candidate to receive FDA breakthrough status.
- Previously, the Pennsylvania-based company had received the orphan drug designation for INO-3107 from the European Commission and the FDA in 2023 and 2020, respectively.
- https://seekingalpha.com/news/4009900-inovio-gains-fda-breakthrough-status-for-dna-therapy
- Inovio Pharmaceuticals, Inc. (INO)
- https://inovio.com/
- https://inovio.com/dna-medicines-pipeline/
Zilebesiran (ALN-AGT)
PALTUSOTINE (ORAL SST2 AGONIST)
Zilebesiran (ALN-AGT)
Alnylam Reports Positive Topline Results from KARDIA-1 Phase 2 Dose-Ranging Study of Zilebesiran, an Investigational RNAi Therapeutic in Development to Treat Hypertension in Patients at High Cardiovascular Risk
Sep 07, 2023
- Zilebesiran Met Primary Endpoint Demonstrating Greater than 15 mmHg Reduction of Systolic Blood Pressure at Three Months of Treatment Compared to Placebo at Two Highest Single Doses Evaluated -
- Study Met Key Secondary Endpoints Showing Consistent and Sustained Reductions of Systolic Blood Pressure at Six Months, Supporting Quarterly or Biannual Dosing -
- Zilebesiran Demonstrated an Encouraging Safety and Tolerability Profile in Adult Patients with Mild-to-Moderate Hypertension -
- Full Study Results to be Presented at an Upcoming Scientific Conference -
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Sep. 7, 2023-- Alnylam Pharmaceuticals, Inc. Nasdaq: ALNY), the leading RNAi therapeutics company, today announced that the KARDIA-1 Phase 2 study of zilebesiran, an investigational RNAi therapeutic targeting liver-expressed angiotensinogen (AGT) in development for the treatment of hypertension, met the primary endpoint demonstrating a dose-dependent, clinically significant reduction in 24-hour mean systolic blood pressure (SBP) measured by ambulatory blood pressure monitoring (ABPM) at Month 3, achieving a placebo-subtracted reduction greater than 15 mmHg (p less than 0.0001) with both 300 mg and 600 mg doses. The study also met key secondary endpoints including significant change in 24-hour mean SBP as measured by ABPM at Month 6, as well as significant change in office SBP at Month 3 and Month 6, for all zilebesiran arms, compared to placebo. The study results indicate zilebesiran was associated with dose-dependent, potent and durable knockdown of serum AGT levels through Month 6. Zilebesiran also demonstrated an encouraging safety and tolerability profile that the company believes supports continued development. These findings of robust and tonic blood pressure control will help determine the optimal dose and regimen of zilebesiran for future studies.
“Hypertension is a growing global health crisis responsible for around 10 million deaths worldwide each year. Despite the availability of several classes of oral anti-hypertensive treatments, up to 80% of individuals globally remain uncontrolled, leaving them at an increased risk of cardiovascular, cerebrovascular and renal disease, which is further exacerbated by blood pressure variability, lack of nighttime blood pressure control and poor adherence,” said Professor George L. Bakris, M.D., Board-Certified Hypertension Specialist and Director of the American Heart Association Comprehensive Hypertension Center, University of Chicago Medicine. “As a physician, I believe these KARDIA-1 results, which demonstrate clinically significant reductions in systolic blood pressure of greater than 15 mmHg, along with the ability to achieve durable tonic blood pressure control, provide hope that we may one day have access to a novel therapy with the potential to address the significant unmet needs of patients with uncontrolled hypertension who are at high risk of future cardiovascular events.”
Zilebesiran demonstrated an encouraging safety and tolerability profile. There was one death due to cardiopulmonary arrest in a zilebesiran-treated patient that was considered unrelated to study drug. Serious adverse events were reported in 3.6% of zilebesiran-treated patients and 6.7% of placebo-treated patients. None were considered related to study drug. Adverse events occurring in 5% or more of zilebesiran-treated patients in any dose arm included COVID-19, injection site reaction (ISR), hyperkalemia, hypertension, upper respiratory tract infection, arthralgia and headache.
The KARDIA-1 Phase 2 trial is a randomized, double-blind (DB), placebo-controlled, multi-center global dose-ranging study designed to evaluate the efficacy and safety of zilebesiran as monotherapy in adults with mild-to-moderate hypertension. The study enrolled 394 adults representing a diverse patient population with untreated hypertension or who were on stable therapy with one or more anti-hypertensive medications. Any patients taking prior anti-hypertensive medications completed at least a two- to four-week wash-out before randomization. Patients were randomized to one of five treatment arms during a 12-month DB period and DB extension period: 150 mg zilebesiran subcutaneously once every six months; 300 mg zilebesiran subcutaneously once every six months; 300 mg zilebesiran subcutaneously once every three months; 600 mg zilebesiran subcutaneously once every six months; or placebo. Patients who received placebo were randomized to one of the four initial zilebesiran dose regimens beginning at Month 6.
The primary endpoint is the change from baseline in SBP at Month 3, assessed by 24-hour ABPM. Key secondary and exploratory endpoints in this study include additional measures of blood pressure reduction at six months, time-adjusted change in blood pressure, and change in daytime average and night-time average blood pressure.
“We are thrilled that the KARDIA-1 Phase 2 results show zilebesiran’s ability to achieve sustained blood pressure reductions of greater than 15 mmHg, as well as long-term efficacy out to six months with infrequent dosing. We believe these results further validate the differentiated profile we observed in Phase 1. Moreover, they reinforce the potential for zilebesiran to be a transformative therapy to reduce cardiovascular risk in patients with hypertension and to offer new possibilities in a field of medicine that has seen limited innovation in nearly 20 years,” said Simon Fox, Ph.D., Vice President, Zilebesiran Program Lead at Alnylam. “We look forward to sharing the full KARDIA-1 results at an upcoming scientific conference and to reporting topline results from our KARDIA-2 Phase 2 study of zilebesiran in combination with one of three standard classes of anti-hypertensive medications in patients with mild-to-moderate hypertension in early 2024. It is a very exciting time for Alnylam, as these results build on the momentum from the recent strategic agreement to co-develop and co-commercialize zilebesiran with our collaboration partner, Roche, to potentially transform the landscape for patients with cardiovascular diseases.”
The KARDIA-2 Phase 2 study of zilebesiran used in combination with one of three standard classes of anti-hypertensive medications completed enrollment in June 2023. Topline results are expected in early 2024.
About Zilebesiran
Zilebesiran is an investigational, subcutaneously administered RNAi therapeutic targeting angiotensinogen (AGT) in development for the treatment of hypertension in high unmet need populations. AGT is the most upstream precursor in the Renin-Angiotensin-Aldosterone System (RAAS), a cascade which has a demonstrated role in blood pressure (BP) regulation and its inhibition has well-established anti-hypertensive effects. Zilebesiran inhibits the synthesis of AGT in the liver, potentially leading to durable reductions in AGT protein and ultimately, in the vasoconstrictor angiotensin (Ang) II. Zilebesiran utilizes Alnylam's Enhanced Stabilization Chemistry Plus (ESC+) GalNAc-conjugate technology, which enables infrequent subcutaneous dosing with increased selectivity and the potential to achieve tonic blood pressure control demonstrating consistent and durable blood pressure reduction throughout a 24-hour period, sustained up to six months after a single dose of zilebesiran. The safety and efficacy of zilebesiran have not been established or evaluated by the FDA, EMA or any other health authority. Zilebesiran is being co-developed and co-commercialized by Alnylam and Roche.
About Hypertension
Uncontrolled hypertension is the chronic elevation of blood pressure (BP), defined by the 2017 ACC/AHA guidelines as ≥130 mmHg systolic blood pressure (SBP) and ≥80 mmHg diastolic blood pressure (DBP). More than one billion people worldwide live with hypertension.i Approximately one in three adults are living with hypertension worldwide, with up to 80% of individuals remaining uncontrolled despite the availability of several classes of oral anti-hypertensive treatments. Despite the availability of anti-hypertensive medications, there remains a significant unmet medical need, especially given the poor rates of adherence to existing daily oral medications, resulting in inconsistent BP control and an increased risk for stroke, heart attack and premature death.ii In particular, there are a number of high unmet need settings where novel approaches to hypertension warrant additional development focus, including patients with poor medication adherence and in patients with high cardiovascular risk.
About RNAi
RNAi (RNA interference) is a natural cellular process of gene silencing that represents one of the most promising and rapidly advancing frontiers in biology and drug development today. Its discovery has been heralded as “a major scientific breakthrough that happens once every decade or so,” and was recognized with the award of the 2006 Nobel Prize for Physiology or Medicine. By harnessing the natural biological process of RNAi occurring in our cells, a new class of medicines known as RNAi therapeutics is now a reality. Small interfering RNA (siRNA), the molecules that mediate RNAi and comprise Alnylam's RNAi therapeutic platform, function upstream of today’s medicines by potently silencing messenger RNA (mRNA) – the genetic precursors – that encode for disease-causing or disease pathway proteins, thus preventing them from being made. This is a revolutionary approach with the potential to transform the care of patients with genetic and other diseases.
About Alnylam Pharmaceuticals
Alnylam Pharmaceuticals (Nasdaq: ALNY) has led the translation of RNA interference (RNAi) into a whole new class of innovative medicines with the potential to transform the lives of people afflicted with rare and prevalent diseases with unmet need. Based on Nobel Prize-winning science, RNAi therapeutics represent a powerful, clinically validated approach yielding transformative medicines. Since its founding in 2002, Alnylam has led the RNAi Revolution and continues to deliver on a bold vision to turn scientific possibility into reality. Alnylam’s commercial RNAi therapeutic products are ONPATTRO® (patisiran), AMVUTTRA® (vutrisiran), GIVLAARI® (givosiran), OXLUMO® (lumasiran), and Leqvio® (inclisiran), which is being developed and commercialized by Alnylam’s partner, Novartis. Alnylam has a deep pipeline of investigational medicines, including multiple product candidates that are in late-stage development. Alnylam is executing on its “Alnylam P5x25” strategy to deliver transformative medicines in both rare and common diseases benefiting patients around the world through sustainable innovation and exceptional financial performance, resulting in a leading biotech profile. Alnylam is headquartered in Cambridge, MA. For more information about our people, science and pipeline, please visit www.alnylam.com and engage with us on X (formerly Twitter) at @Alnylam, or on LinkedIn, Facebook, or Instagram.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230907817269/en/
Alnylam Pharmaceuticals, Inc.
Source: Alnylam Pharmaceuticals, Inc.
Alnylam succeeds in Phase 2 trial for blood pressure drug
Sep. 07, 2023 8:25 AM ET
Alnylam Pharmaceuticals, Inc. (ALNY), RHHBY, RHHBF
By: Dulan Lokuwithana, SA News Editor
- Alnylam Pharmaceuticals (NASDAQ:ALNY) announced Thursday that its experimental RNAi therapeutic, zilebesiran, reached the primary endpoint in a Phase 2 study for adults with mild-to-moderate hypertension.
- Roche (OTCQX:RHHBY) (OTCQX:RHHBF) has partnered with Alnylam to develop and commercialize the subcutaneously delivered therapy.
- Citing topline data from the KARDIA-1 trial at month three, Alnylam (ALNY) said that zilebesiran led to a decline in 24-hour mean systolic blood pressure (SBP) with a dose-dependent, clinically significant effect in achieving its primary goal.
- https://seekingalpha.com/news/4009869-alnylam-succeeds-phase-2-trial-blood-pressure-drug?mailingid=32631948&messageid=2900&serial=32631948.4015&utm_campaign=rta-stock-news&utm_content=link-1&utm_medium=email&utm_source=seeking_alpha&utm_term=32631948.4015
- Alnylam Pharmaceuticals, Inc. (ALNY)
- https://www.alnylam.com/sites/default/files/pdfs/ALN-AGT-Fact-Sheet.pdf
- https://www.alnylam.com/
VLA15
BRII-179 (VBI-2601) in Combination With PEG-IFNα
BRII-179 (VBI-2601) in Combination With PEG-IFNα
Valneva and Pfizer Report Positive Pediatric and Adolescent Phase 2 Booster Results for Lyme Disease Vaccine Candidate
September 7, 2023
- Strong immune response shown in both children and adolescents one month after booster dose (month 19) in VLA15-221 study
- Previously observed high anamnestic antibody response in adults confirmed
- VLA15 well-tolerated in all age groups following booster dose
Saint-Herblain (France) & New York, September 7, 2023 – Valneva SE (Nasdaq: VALN; Euronext Paris: VLA) and Pfizer Inc. (NYSE: PFE) announced today positive pediatric and adolescent immunogenicity and safety data for their Lyme disease vaccine candidate, VLA15, when given as a booster. These results from the VLA15-221 Phase 2 study showed a strong anamnestic antibody response for all serotypes in pediatric (5 to 11 years of age) and adolescent participants (12 to 17 years of age), as well as in adults (18 to 65 years of age), one month after administration of a booster dose (month 19).
Depending on the primary schedule they received (month 0-2-6 or month 0-6), participants seroconverted after the booster dose, yielding seroconversion1 rates (SCRs) of 95.3% and 94.6% for all outer surface protein A (OspA) serotypes in all age groups, respectively. Additionally, OspA antibody titers were significantly higher one month after the booster dose compared to one month after the primary schedule with 3.3- to 3.7-fold increases (Geometric Mean Fold Rises) in adults, 2.0- to 2.7- fold increases in adolescents and 2.3- to 2.5-fold increases in children for all serotypes.
Juan Carlos Jaramillo M.D., Chief Medical Officer of Valneva, said, “We are pleased with these data which validate the use of a booster dose in all age groups. Lyme disease continues to spread, representing an important unmet medical need that impacts the lives of many people in the Northern Hemisphere. With each new set of positive data, we come one step closer to potentially bringing this vaccine to both adults and children living in areas where Lyme disease is endemic.”
The Phase 2 booster results emphasize the vaccine candidate’s potential to provide immunity against Lyme disease in pediatric and adolescent populations. Geometric Mean Titers (GMTs) one month following the booster dose were similarly high for children and adolescents.
The safety and tolerability profile of VLA15 after a booster dose was consistent with previous studies as the vaccine candidate was well-tolerated in all age groups regardless of the primary vaccination schedule. No vaccine-related serious adverse events (SAEs) and no safety concerns were observed by an independent Data Safety Monitoring Board (DSMB).
“Protection against Lyme disease is important for anyone who lives or spends time outdoors in areas where Lyme disease is endemic. This data from the VLA15-221 study is vital to improve our understanding of how vaccination may help to protect both adults and children from this potentially devastating disease,” said Annaliesa Anderson, Ph.D., Senior Vice President and Head Vaccine Research and Development at Pfizer. “We are encouraged by the positive Phase 2 results for VLA15, and, in partnership with Valneva, look forward to continuing to study the vaccine candidate in ongoing Phase 3 clinical trials.”
These results follow six-month antibody persistence data in children and adults reported for the VLA15-221 study in December 20222 and positive immunogenicity and safety data reported in April 20223.
In August 2022, Pfizer and Valneva initiated the currently ongoing Phase 3 clinical study, Vaccine Against Lyme for Outdoor Recreationists (VALOR) (NCT05477524), to investigate the efficacy, safety and immunogenicity of VLA15 in participants five years of age and older in highly endemic regions in the United States (U.S.) and Europe4. A second Phase 3 study (VLA15-1012), aiming to provide further evidence on the safety profile of VLA15 in the pediatric population, is also ongoing.
Pfizer aims to submit a Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA) and Marketing Authorisation Application (MAA) to the European Medicines Agency (EMA) in 2026, subject to positive Phase 3 data.
About VLA15
There are currently no approved human vaccines for Lyme disease, and VLA15 is the most advanced Lyme disease vaccine candidate currently in clinical development, with a Phase 3 study in progress. This investigational multivalent protein subunit vaccine uses an established mechanism of action for a Lyme disease vaccine that targets the outer surface protein A (OspA) of Borrelia burgdorferi, the bacteria that cause Lyme disease. OspA is a surface protein expressed by the bacteria when present in a tick. Blocking OspA inhibits the bacterium’s ability to leave the tick and infect humans. The vaccine covers the six most common OspA serotypes expressed by the Borrelia burgdorferi sensu lato species that are prevalent in North America and Europe. VLA15 has demonstrated a strong immune response and satisfactory safety profile in pre-clinical and clinical studies so far. Valneva and Pfizer entered into a collaboration agreement in April 2020 to co-develop VLA15, with updates to the terms within this agreement made in June 2022.5,6 The program was granted Fast Track designation by the U.S. FDA in July 2017.7
About Clinical Study VLA15-221
VLA15-221 is a randomized, observer-blind, placebo-controlled Phase 2 study. It is the first clinical study with VLA15 which enrolled a pediatric population (5-17 years old).
585 healthy participants received VLA15 in two immunization schedules (month 0-2-6 [N=190] or month 0-6 [N=187]) or three doses of placebo (month 0-2-6 [N=208]). Vaccine recipients received VLA15 at a dose of 180 µg, which was selected based on data generated in the two previous Phase 2 studies. The main safety and immunogenicity readout was performed one month after the primary vaccination series. All eligible subjects received a booster dose of VLA15 or placebo at month 18 (booster phase) and will be followed for three additional years to monitor antibody persistence. In addition, all eligible subjects will be asked to receive an additional booster dose of VLA15 or placebo at month 30, in order to generate additional data and assess the need for periodic booster doses.
VLA15 is tested as an alum-adjuvanted formulation and administered intramuscularly. The study is being conducted at U.S. sites located in areas where Lyme disease is endemic and has enrolled both volunteers with a prior infection with Borrelia burgdorferi as well as Borrelia burgdorferi-naïve volunteers.
About Lyme Disease
Lyme disease is a systemic infection caused by Borrelia burgdorferi bacteria transmitted to humans by the bite of an infected Ixodes ticks.8 It is considered the most common vector-borne illness in the Northern Hemisphere.9 While the true incidence of Lyme disease is unknown, it is estimated to annually affect approximately 476,000 people in the U.S. and 129,000 people in Europe.10,11 Early symptoms of Lyme disease (such as a gradually expanding erythematous rash called Erythema migrans or more nonspecific symptoms like fatigue, fever, headache, mild stiff neck, arthralgia or myalgia) are often overlooked or misinterpreted. Left untreated, the disease can disseminate and cause more serious complications affecting the skin, joints (arthritis), the heart (carditis) or the nervous system.10 The medical need for vaccination against Lyme disease is steadily increasing as the geographic footprint of the disease widens.12
About Pfizer: Breakthroughs That Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world’s premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.Pfizer.com. In addition, to learn more, please visit us on www.Pfizer.com and follow us on Twitter at @Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
About Valneva SE
We are a specialty vaccine company focused on the development, manufacturing and commercialization of prophylactic vaccines for infectious diseases. We take a highly specialized and targeted approach to vaccine development by focusing on vaccine solutions addressing unmet medical needs to ensure we can make a difference to peoples’ lives. We apply our deep understanding of vaccine science, including our expertise across multiple vaccine modalities, and our established vaccine development capabilities, to develop vaccines against diseases which are not yet vaccine-preventable, or for which there are limited effective treatment options. Today, we are leveraging our expertise and capabilities to rapidly advance a broad range of vaccines into and through the clinic, including candidates against the chikungunya virus and Lyme disease.
Pfizer, Valneva post Phase 2 booster data for Lyme disease vaccine
Sep. 07, 2023 6:56 AM ET
By: Dulan Lokuwithana, SA News Editor
Pfizer (PFE) and its French partner Valneva SE (NASDAQ:VALN) announced Thursday that the companies’ Lyme disease vaccine candidate, VLA15, caused a robust immune response in children and adolescents as a booster shot.
Citing results from their 585-subject VLA15-221 trial, the companies said that the antibody levels against outer surface protein A (OspA) indicated a 2.0–2.7-fold increase one month after VLA15 as a booster in adolescents compared to one month after the primary schedule.
https://seekingalpha.com/news/4009828-pfizer-valneva-post--booster-data-lyme-disease-vaccine
BRII-179 (VBI-2601) in Combination With PEG-IFNα
BRII-179 (VBI-2601) in Combination With PEG-IFNα
BRII-179 (VBI-2601) in Combination With PEG-IFNα
VBI Vaccines Partner Brii Biosciences Announces Topline Interim Results of Phase 2 Study Evaluating BRII-179 (VBI-2601) in Combination With PEG-IFNα for the Treatment of Chronic Hepatitis B
September 6, 2023
- BRII-179 (VBI-2601) as an add-on therapy to standard of care PEG-IFNα increases HBsAg loss rate at the end of treatment and 12 weeks follow up
- Significantly increased seroconversion rate is strongly associated with BRII-179 (VBI-2601) treatment and correlates with the increased rate of HBsAg loss
- Safety findings are similar to those of PEG-IFNα and BRII-179 (VBI-2601) as previously reported
CAMBRIDGE, Mass. –
VBI Vaccines Inc. (Nasdaq: VBIV) (“VBI” or the “Company”) today announced that its strategic hepatitis B (HBV) partner, Brii Biosciences (Brii Bio) (Stock code: 2137.HK), announced topline cohort-level unblinded Week 36 data from interim analysis of a randomized, placebo-controlled and double-blinded Phase 2 study of BRII-179 (VBI-2601), a first-in-class Pre-S1/Pre-S2/S therapeutic vaccine, in combination treatment with pegylated interferon-alpha (PEG-IFNα) in chronic hepatitis B virus (HBV) patients compared with PEG-IFNα only treatment. VBI and Brii Bio reported in previous studies that BRII-179 (VBI-2601) induced broad antibody and T-cell responses against Pre-S1, Pre-S2, and S epitopes in HBV patients. Brii Bio’s detailed press release can be found here: https://www.briibio.com/en/media/press-release/20230906/.
“We share Brii Bio’s excitement about this data and congratulate them on their continued ability to move quickly and execute clinical programs as they seek to deliver higher hepatitis B functional cure rates,” said Jeff Baxter, President and CEO of VBI. “Brii Bio’s ongoing commitment, investments, and partnerships in this field continue to reinforce the strategic potential of our partnership and we look forward to seeing further data from this study and future studies of this first-in-class immunotherapeutic candidate.”
In July 2023, VBI and Brii Bio announced an expansion of their HBV partnership to include an exclusive global license to develop and commercialize BRII-179 (VBI-2601), and an exclusive license to develop and commercialize PreHevbri®, VBI’s prophylactic 3-antigen adult HBV vaccine, in the Asia Pacific region, excluding Japan.
About BRII-179 (VBI-2601) + PEG-IFNα Combination Study
The Phase 2 study is a multicenter, randomized, double-blind, placebo-controlled, parallel study designed to evaluate the safety and efficacy of BRII-179 (VBI-2601) as an add-on therapy to PEG-IFNα and NrtI therapy for the treatment of chronic HBV infection. This study enrolled adult HBV patients in mainland China who had received 24 to 28 doses of PEG-IFNα per treatment guideline, at least 12 months of NrtI therapy, and met a pre-defined criteria for partial response. Subjects were randomized 1:1 to receive BRII-179 (VBI-2601) or placebo every three weeks for a total of 7 doses over 18 weeks while continuing PEG-IFNα treatment for 48 weeks. Subjects who met Nrtl discontinuation criteria would stop Nrtl treatment and would be followed up for additional 48 weeks.
About BRII-179 (VBI-2601)
BRII-179 (VBI-2601) is a novel recombinant, protein-based HBV immunotherapeutic candidate that builds upon the 3-antigen conformation of VBI’s prophylactic 3-antigen HBV vaccine candidate and is designed to target enhanced and broad B-cell and T-cell immunity. BRII-179 (VBI-2601) has been licensed to Brii Biosciences (Brii Bio) under an exclusive global development and licensing agreement. BRII-179 (VBI-2601) is currently being investigated in two Phase 2 clinical trials in combination with BRII-835 (VIR-2218) and PEG-IFNα as part of a potential functional cure regimen for the treatment of chronic HBV infection.
About PreHevbri®
PreHevbri is the only 3-antigen hepatitis B vaccine, comprised of the three hepatitis B surface antigens of the hepatitis B virus – Pre-S1, Pre-S2, and S. It is approved for use in the United States, European Union/European Economic Area, United Kingdom, Canada, and Israel. The brand names for this vaccine are: PreHevbrio® (US/Canada), PreHevbri® (EU/EEA/UK), and Sci-B-Vac® (Israel).
Please visit www.PreHevbrio.com for U.S. Important Safety Information for PreHevbrio® [Hepatitis B Vaccine (Recombinant)], or please see U.S. Full Prescribing Information.
U.S. Indication
PreHevbrio is indicated for prevention of infection caused by all known subtypes of hepatitis B virus. PreHevbrio is approved for use in adults 18 years of age and older.
Please see Full Prescribing Information.
About VBI Vaccines Inc.
VBI Vaccines Inc. (“VBI”) is a biopharmaceutical company driven by immunology in the pursuit of powerful prevention and treatment of disease. Through its innovative approach to virus-like particles (“VLPs”), including a proprietary enveloped VLP (“eVLP”) platform technology, VBI develops vaccine candidates that mimic the natural presentation of viruses, designed to elicit the innate power of the human immune system. VBI is committed to targeting and overcoming significant infectious diseases, including hepatitis B, coronaviruses, and cytomegalovirus (CMV), as well as aggressive cancers including glioblastoma (GBM). VBI is headquartered in Cambridge, Massachusetts, with research operations in Ottawa, Canada, and a research and manufacturing site in Rehovot, Israel.
Website Home: http://www.vbivaccines.com/
News and Resources: http://www.vbivaccines.com/news-and-resources/
Investors: http://www.vbivaccines.com/investors/
View source version on businesswire.com: https://www.businesswire.com/news/home/20230906245918/en/
VBI Vaccines gains after Phase 2 data for Hep B candidate
Sep. 06, 2023 7:33 AM ET
VBI Vaccines Inc. (VBIV), BRIBF
By: Dulan Lokuwithana, SA News Editor
VBI Vaccines (NASDAQ:VBIV) traded ~13% higher pre-market Wednesday after its partner, Hong Kong-listed Brii Biosciences Limited (OTCPK:BRIBF), announced mid-stage data for BRII-179, an experimental immunotherapy targeted at the hepatitis B virus (HBV).
https://seekingalpha.com/news/4009419-vbi-vaccines-stock-gains-after-data-hep-b-candidate
VBI Vaccines Inc. (VBIV), BRIBF
MGD024
BRII-179 (VBI-2601) in Combination With PEG-IFNα
MGD024
Sep 5, 2023
MacroGenics Announces Achievement of $15 Million Milestone Related to Gilead’s Nomination of a Bispecific Research Program
ROCKVILLE, MD, Sept. 05, 2023 (GLOBE NEWSWIRE) -- MacroGenics, Inc. (NASDAQ: MGNX), a biopharmaceutical company focused on developing, manufacturing and commercializing innovative antibody-based therapeutics for the treatment of cancer, today announced that its partner, Gilead Sciences, Inc. (NASDAQ: GILD), nominated the first of two research programs, leveraging MacroGenics’ DART® and TRIDENT® platforms for generating bispecific antibodies. This nomination grants Gilead an exclusive option, upon achievement of a pre-defined preclinical milestone, to license worldwide rights to the research program.
Under the October 2022 agreement, MacroGenics will receive $15 million related to the nomination of a bispecific research program to be conducted by MacroGenics and funded by Gilead. Pursuant to this agreement, which covers MGD024, an investigational, bispecific antibody that binds CD123 and CD3 using MacroGenics’ DART platform, and up to two additional bispecific research programs, MacroGenics remains eligible to receive up to $1.7 billion in target nomination, option fees, and development, regulatory and commercial milestones. MacroGenics will also be eligible to receive tiered, double-digit royalties on worldwide net sales of MGD024 and a flat royalty on worldwide net sales of products under the two research programs.
About MacroGenics, Inc.
MacroGenics (the Company) is a biopharmaceutical company focused on developing, manufacturing and commercializing innovative monoclonal antibody-based therapeutics for the treatment of cancer. The Company generates its pipeline of product candidates primarily from its proprietary suite of next-generation antibody-based technology platforms, which have applicability across broad therapeutic domains. The combination of MacroGenics' technology platforms and protein engineering expertise has allowed the Company to generate promising product candidates and enter into several strategic collaborations with global pharmaceutical and biotechnology companies. For more information, please see the Company's website at www.macrogenics.com. MacroGenics, the MacroGenics logo, MARGENZA and DART are trademarks or registered trademarks of MacroGenics, Inc.
Source: MacroGenics, Inc.
MacroGenics achieves $15M milestone related to Gilead's nomination of bispecific research program
Sep. 05, 2023 4:46 PM ET
By: Jaskiran Singh, SA News Editor
- MacroGenics (NASDAQ:MGNX) Tuesday announced the achievement of a pre-defined preclinical milestone, enabling MacroGenics to receive $15 million related to the nomination of a bispecific research program.
- https://seekingalpha.com/news/4009286-macrogenics-achieves-15m-milestone-related-to-gileads-nomination-of-bispecific-research-program
- MacroGenics, Inc. (MGNX)
- https://macrogenics.com/pipeline/mgd024-cd123-x-cd3/
- https://macrogenics.com/
KB408
CAMZYOS® (mavacamten)
MGD024
Krystal Biotech Announces Orphan Drug Designation Granted to KB408 for the Treatment of Alpha-1 Antitrypsin Deficiency
September 5, 2023
- KB408 IND filed on August 15, 2023
PITTSBURGH, Sept. 05, 2023 (GLOBE NEWSWIRE) -- Krystal Biotech, Inc. (the “Company”) (NASDAQ: KRYS), a commercial-stage biotechnology company focused on the discovery, development and commercialization of genetic medicines to treat diseases with high unmet medical needs, announced today that the U.S. Food and Drug Administration (FDA) granted Orphan Drug Designation for KB408 for the treatment of alpha-1 antitrypsin deficiency (AATD).
AATD is caused by mutations in the SERPINA1 gene that lead to decreased levels and/or decreased functionality of alpha-1 antitrypsin protein. The protein is primarily produced in the liver and secreted into the bloodstream, where it acts as a circulating serine protease inhibitor whose principal substrate is neutrophil elastase in the lungs. Over time, the deficiency can lead to progressive enzymatic destruction of the lung tissue, ultimately causing life-threatening pulmonary impairment and severe respiratory insufficiency. In severe cases, current disease management includes intravenous augmentation therapy which requires weekly infusions, the clinical benefit of which remains to be established.
KB408 is an inhaled (nebulized) formulation of the Company’s novel replication-defective, non-integrating HSV-1-based vector designed to deliver two copies of the SERPINA1 transgene, that encodes for human alpha-1 antitrypsin protein, for the treatment of AATD.
"This important designation is a milestone in the advancement of KB408, and this decision by the FDA underscores the need for potential new treatment options for patients with AATD," said Suma Krishnan, President, Research & Development, Krystal Biotech, Inc. "We are encouraged by the profile of KB408 in preclinical studies to date and look forward to dosing patients once we receive clearance from the FDA."
About Orphan Drug Designation
Orphan Drug Designation is granted by the FDA to investigational therapies addressing rare medical diseases or conditions that affect fewer than 200,000 people in the U.S. Orphan drug status provides benefits to drug developers, including assistance in the drug development process, tax credits for clinical costs, exemptions from certain FDA fees and seven years of post-approval marketing exclusivity.
About Krystal Biotech, Inc.
Krystal Biotech, Inc. (NASDAQ: KRYS) is a commercial-stage biotechnology company focused on the discovery, development and commercialization of genetic medicines to treat diseases with high unmet medical needs. VYJUVEK™ is the Company’s first commercial product, the first-ever redosable gene therapy, and the only medicine approved by the FDA for the treatment of dystrophic epidermolysis bullosa. The Company is rapidly advancing a robust preclinical and clinical pipeline of investigational genetic medicines in respiratory, oncology, dermatology, ophthalmology, and aesthetics. Krystal Biotech is headquartered in Pittsburgh, Pennsylvania. For more information, please visit http://www.krystalbio.com, and follow @KrystalBiotech on LinkedIn and Twitter.

![]()
Source: Krystal Biotech, Inc.
Krystal Biotech gets FDA orphan drug designation for AATD drug candidate
Sep. 05, 2023 11:40 AM ET
By: Val Brickates Kennedy, SA News Editor
Krystal Biotech (NASDAQ:KRYS) said it has received FDA orphan drug designation for its drug candidate KB408 in the treatment of alpha-1 antitrypsin deficiency, or AATD.
CAMZYOS® (mavacamten)
CAMZYOS® (mavacamten)
CAMZYOS® (mavacamten)
Long-Term Follow-Up Data from Two Phase 3 Studies of CAMZYOS® (mavacamten) Demonstrate Consistent and Durable Response in Patients with Symptomatic Obstructive Hypertrophic Cardiomyopathy (HCM)
08/28/2023
CATEGORY:
Results from VALOR-HCM LTE (56 weeks) demonstrated that with longer follow-up, CAMZYOS continued to reduce eligibility for invasive SRT at 56 weeks
EXPLORER-LTE data (cumulative analysis up to 120 weeks) showed sustained improvements in LVOT obstruction, symptoms, and NT-proBNP levels in patients with symptomatic obstructive HCM, with no new safety signals observed
CAMZYOS was recently approved in the European Union, following its approval in the U.S. and other markets worldwide, and is the first and only cardiac myosin inhibitor approved to treat adult patients with symptomatic obstructive HCM
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE: BMY) today announced new long-term follow-up results from two Phase 3 studies evaluating CAMZYOS® (mavacamten), a first-in-class cardiac myosin inhibitor, in adult patients with symptomatic obstructive hypertrophic cardiomyopathy (HCM). Results from the 56-week analysis of the VALOR-HCM long-term extension (LTE) study were presented as a late-breaking oral presentation, with simultaneous publication in JAMA Cardiology, and results from the cumulative 120-week analysis of the EXPLORER cohort of the MAVA-LTE study were presented as an oral presentation at the European Society of Cardiology (ESC) Congress 2023.
“The new long-term data presented at ESC were consistent with the primary analyses from each study, further underscoring the benefit our first-in-class therapy can provide to patients with symptomatic obstructive HCM,” said Amy Sehnert, M.D., Vice President, Head of Cardiomyopathy and Heart Failure Clinical Development, Bristol Myers Squibb. “These positive data reinforce the clinically meaningful significance of these two Phase 3 trials that led to the approval of CAMZYOS in the United States, the European Union and other countries around the globe. We are excited for the ongoing exploration of the potential of CAMZYOS and remain dedicated to providing support for obstructive HCM patients worldwide.”
Key findings from the 56-week analysis of VALOR-HCM LTE include:
- Treatment with CAMZYOS demonstrated sustained improvements across key study endpoints in both the original CAMZYOS group over 56 weeks and those transitioned to the placebo cross-over group over 40 weeks.
- At Week 56, 5 of 56 patients (8.9%) in the original CAMZYOS group and 10 of 52 patients (19.2%) in the placebo cross-over group at Week 40 decided to proceed with septal reduction therapy (SRT) or were SRT-eligible.
- CAMZYOS demonstrated sustained reduction in peak resting LVOT gradient (-34.0 mmHg for the original CAMZYOS group [95% CI -43.5 to -24.5] and -33.2 mmHg for the placebo cross-over group [95% CI -41.9 to -24.5]).
- Proportion with NYHA class improvement of ≥1 class was observed in 93% of patients in the original CAMZYOS group at Week 56 and 73% of patients from the placebo cross-over group at Week 40.
- On the patient-reported 23-item Kansas City Cardiomyopathy Questionnaire Clinical Summary Score (KCCQ-23 CSS)*, average scores of symptom frequency, symptom burden and physical limitation continued to improve with a 14.1 point increase for the original CAMZYOS group (95% CI 9.9 to 18.3) and 11.7 point increase for the placebo crossover group (95% CI 6.9 to 16.4).
- CAMZYOS was also associated with sustained reduction across biomarkers of cardiac wall stress and myocardial injury including reduction in N-terminal pro brain natriuretic peptide (NT-proBNP), with -376 ng/L for the original CAMZYOS group (95% CI -723 to -225) and -423 ng/L for the placebo cross-over group (95% CI -624 to -252) and reduction in cardiac troponin I with -7.0 ng/L for the original CAMZYOS group (95% CI -10 to -2.3) and -6.2 ng/L for the placebo cross-over group (95% CI -11.5 to -3.3).
- No new safety signals were observed, and safety and efficacy were consistent across both patient groups.
*The KCCQ‑23 CSS is derived from the Total Symptom Score (TSS) and the Physical Limitations (PL) score of the KCCQ‑23. The CSS ranges from 0 to 100 with higher scores representing better health status.
“The 56-week late-breaking analysis of VALOR-HCM LTE builds upon previous findings and demonstrates the consistent impact of this oral treatment for severely symptomatic obstructive HCM patients by showing that nearly 9 out of 10 patients treated with this drug have continued in this long-term extension trial without SRT at either 40 or 56 weeks of treatment,” said Milind Desai, M.D., MBA, director, center for hypertrophic cardiomyopathy and vice chair of education in the Heart, Vascular & Thoracic Institute at Cleveland Clinic. “These findings are important for our continued understanding of this treatment and encouraging for patients hoping for non-surgical options.”
Key findings from the cumulative 120-week analysis of EXPLORER-LTE include:
- No new safety signals were observed.
- Overall, 75.9% of patients improved by ≥1 NYHA class from baseline at the start of the LTE study to Week 120.
- Of the 14 patients who were in NYHA class I, 12 remained in NYHA class I at the latest available assessment.
- Treatment with CAMZYOS was associated with sustained improvements from baseline at the start of the LTE study in echocardiographic parameters, including E/e’ average and NT-proBNP.
- Mean LVEF remained within the normal range at all study visits.
- Since the previous interim analysis in August 2021, one new patient experienced a transient reduction in LVEF <50% resulting in temporary treatment interruption.
“The presentation of data − the largest and longest analysis of patients on CAMZYOS to-date − illustrates the promise of this game-changing treatment for patients with symptomatic obstructive HCM,” said Pablo García-Pavia, M.D., Ph.D., head of the Inherited Cardiac Diseases and Heart Failure Unit at the Department of Cardiology of Hospital Universitario Puerta de Hierro and professor at the Spanish Cardiovascular Research Institute (CNIC) in Madrid, Spain. “Studies like EXPLORER-LTE are important for understanding longer-term results that assess key cardiac measures and support the use of CAMZYOS in patients living with this chronic condition.”
About the VALOR-HCM and LTE Trial
VALOR-HCM (NCT04349072) was a randomized, double-blind, placebo-controlled, multicenter Phase 3 study of patients with symptomatic, obstructive HCM (NYHA class II-IV) who met guideline criteria for septal reduction therapy (SRT; LVOT gradient of ≥50 mmHg and NYHA class III-IV, or class II with exertional syncope or near syncope) and had been referred or under active consideration (within the past 12 months) for an invasive procedure. Patients were required to have LVOT peak gradient ≥50 mmHg at rest or with provocation, and LVEF ≥60%. The study enrolled 112 patients (mean age of 60 years; 51% men; 93% ≥ NYHA class III) randomized on a 1:1 basis to receive mavacamten or placebo. At baseline, 95% of patients were on background therapies of a beta blocker, calcium channel blocker, disopyramide or a combination. The primary endpoint was a composite of the proportion of patients who decided to proceed with SRT prior to or at Week 16 or who remained SRT-guideline eligible (LVOT gradient of ≥50 mmHg and NYHA class III-IV, or class II with exertion induced syncope or near syncope) at Week 16. Key secondary endpoints included the change from baseline on post-exercise LVOT gradient, NYHA class, Kansas City Cardiomyopathy Questionnaire (KCCQ-23) Clinical Summary Score and cardiac biomarkers (NT-proBNP and Cardiac Troponin I) at Week 16.
The group initially randomized to CAMZYOS continued the drug for 32 weeks, and the placebo group crossed over to dose-blinded CAMZYOS from Week 16 to Week 32. From the 112 randomized patients with obstructive HCM, 108 (mean age, 60.3 years; 50% men; 94% in NYHA class III/IV) qualified for Week 32 evaluation (56 in the original CAMZYOS group and 52 in the placebo cross-over group) and continued once-daily CAMZYOS until Week 128. During this LTE period, CAMZYOS dose remained blinded.
About the EXPLORER-HCM and the MAVA-LTE Trials
The EXPLORER-HCM Phase 3 trial (NCT03470545) was a double-blind, randomized, placebo-controlled, parallel group trial that enrolled a total of 251 adult patients with symptomatic (NYHA class II or III) obstructive hypertrophic cardiomyopathy. All participants had measurable left ventricular ejection fraction (LVEF) ≥55% and at least one peak LVOT gradient ≥50 mmHg (at rest or with provocation at diagnosis); in addition, Valsalva LVOT gradient ≥30 mmHg at baseline was required at screening. Ninety-two percent of patients were on background therapies of a beta blocker or calcium channel blocker. The primary endpoint was a composite functional endpoint, assessed at 30 weeks, and was defined as the proportion of patients who achieved either improvement of mixed venous oxygen tension (pVO2) by ≥1.5 mL/kg/min plus improvement in NYHA class by at least 1 or improvement of pVO2 by ≥3.0 mL/kg/min plus no worsening in NYHA class. Key secondary endpoints include impact on exercise gradient LVOT, pVO2, NYHA class and Kansas City Cardiomyopathy Questionnaire (KCCQ) and Hypertrophic Cardiomyopathy Symptom Questionnaire (HCMSQ) at Week 30.
EXPLORER-LTE is a cohort of the MAVA-LTE study (NCT03723655), an ongoing, dose-blinded, 5-year study of CAMZYOS in patients with symptomatic obstructive HCM who completed the EXPLORER-HCM trial. All participants in the EXPLORER-LTE cohort started on 5 mg of CAMZYOS daily and dose adjustments were made at Weeks 4, 8 and 12 based on site-read echocardiography measures of Valsalva LVOT gradient and LVEF only. Dose adjustment was also possible at Week 24 following site-read echocardiography assessment of post-exercise LVOT gradient. Subsequent to Week 24, dose adjustment was possible if site-read Valsalva LVOT gradient was >30 mmHg and LVEF ≥50%.
About CAMZYOS (mavacamten)
CAMZYOS® (mavacamten) is the first and only cardiac myosin inhibitor approved in the U.S., indicated for the treatment of adults with symptomatic New York Heart Association (NYHA) class II-III obstructive hypertrophic cardiomyopathy (HCM) to improve functional capacity and symptoms, and in the European Union, indicated for the treatment of symptomatic (NYHA, class II-III) obstructive HCM in adult patients. It has also received regulatory approvals in Australia, Brazil, Canada, Great Britain, Macau, Singapore, South Korea and Switzerland. CAMZYOS is an allosteric and reversible inhibitor selective for cardiac myosin. CAMZYOS modulates the number of myosin heads that can enter “on actin” (power-generating) states, thus reducing the probability of force-producing (systolic) and residual (diastolic) cross-bridge formation. Excess myosin actin cross-bridge formation and dysregulation of the super-relaxed state are mechanistic hallmarks of HCM. CAMZYOS shifts the overall myosin population towards an energy-sparing, recruitable, super-relaxed state. In HCM patients, myosin inhibition with CAMZYOS reduces dynamic left ventricular outflow tract (LVOT) obstruction and improves cardiac filling pressures.
Further information is available at www.CAMZYOSREMS.com or by telephone at 1-833-628-7367.
Please see U.S. Full Prescribing Information, including Boxed WARNING and Medication Guide.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
Multimedia Files:
 Download:Download original 99 KB 1505 x 211Download thumbnail 5 KB 200 x 28Download lowres 15 KB 480 x 67Download square 7 KB 250 x 250
Download:Download original 99 KB 1505 x 211Download thumbnail 5 KB 200 x 28Download lowres 15 KB 480 x 67Download square 7 KB 250 x 250
https://seekingalpha.com/symbol/BMY
BMY Dividend History
https://www.nasdaq.com/market-activity/stocks/bmy/dividend-history
Bristol's Camzyos shows long-term benefit for heart condition
Aug. 28, 2023 2:05 PM ET
Bristol-Myers Squibb Company (BMY)
By: Jonathan Block, SA News Editor
New phase 3, long-term data shows that Bristol-Myers Squibb's (NYSE:BMY) Camzyos (mavacamten) led to a reduced need for invasive cardiac therapies and a sustained reduction in an indicator of cardiovascular failure.
Bristol (BMY) presented results for two trials, VALOR-HCM LTE (56 weeks follow-up) and EXPLORER-LTE (up to 120 weeks).
https://seekingalpha.com/news/4006799-bristol-camzyos-long-term-benefit-heart-condition
Acoramidis
CAMZYOS® (mavacamten)
CAMZYOS® (mavacamten)
bridgebio presents detailed positive results from phase 3 attribute-cm study of acoramidis for patients with transthyretin amyloid cardiomyopathy (attr-cm) at european society of cardiology congress 2023
08.27.2023 at 6:15 AM EDT
- The primary endpoint was met (Win Ratio of 1.8) with a highly statistically significant p-value (p<0.0001); this primary endpoint result consistently favored acoramidis treatment across key subgroups, including across both variant and wild-type ATTR patients as well as across New York Heart Association (NYHA) Class I, II, and III patients. In particular, in contrast to results observed in prior studies of TTR stabilizers, consistency against cardiovascular-related hospitalizations (CVH) was observed across all prespecified subgroups at 30 months
- Absolute values observed across all-cause mortality (ACM), cardiovascular mortality (CVM) and CVH showed that over 30 months, patients survived more and were hospitalized less than has been seen in prior controlled studies of ATTR-CM to the company’s knowledge
- The 81% survival rate on acoramidis approaches the survival rate in the age-matched US database (~85%)
- The 0.29 mean annual CVH rate on acoramidis approaches the annual hospitalization rate observed in the broader US Medicare population (~0.26)
- Assessment of measures of disease progression in the trial suggest that on acoramidis, 45% of subjects experienced an improvement from baseline in N-terminal prohormone of brain natriuretic peptide (NT-proBNP) versus 9% on placebo, and 40% of subjects experienced an improvement from baseline on 6-minute walk distance (6MWD) versus 24% on placebo; to the company’s knowledge, the proportions of treated patients improving on these measures over 30 months are higher than have been observed in prior controlled studies in ATTR-CM
- Acoramidis achieved near-complete stabilization of transthyretin (TTR) in both wild-type and variant ATTR patients; serum TTR was promptly and consistently elevated throughout the study
- In an exploratory post-hoc analysis of the relationship between on-treatment serum TTR levels and on-treatment measures of CVH, NT-proBNP, and Kansas City Cardiomyopathy Questionnaire (KCCQ), there was an association between the mean on-treatment TTR level and each of these three variables, consistent with the premise that ever-higher degrees of stabilization lead to ever-better outcomes for patients
- As was previously reported, in a comparative exploratory post hoc analysis enabled by tafamidis drop-in, albeit at low patient numbers, acoramidis showed a 42% greater increase in serum TTR levels relative to placebo + tafamidis
- Acoramidis was well-tolerated, with no safety signals of potential clinical concern identified
- Company intends to file a New Drug Application (NDA) with the U.S. Food and Drug Administration (FDA) by end of 2023
PALO ALTO, Calif., Aug. 27, 2023 (GLOBE NEWSWIRE) -- BridgeBio Pharma, Inc. (Nasdaq: BBIO) (“BridgeBio” or the “Company”), a commercial-stage biopharmaceutical company focused on genetic diseases and cancers, today announced the presentation of detailed positive results from its Phase 3 ATTRibute-CM study of acoramidis for patients with ATTR-CM by Julian Gillmore, MBBS, M.D., Ph.D., FRCP, FRCPath, in a Hot Line session at the European Society of Cardiology Congress 2023. In July, BridgeBio announced positive topline results from ATTRibute-CM, which was designed to study the efficacy and safety of acoramidis, an investigational, next-generation, orally-administered, highly potent small molecule stabilizer of transthyretin (TTR). BridgeBio will host an investor call on August 28, 2023, at 8:30 am ET to discuss these results.
“The results of the ATTRibute-CM study of acoramidis in ATTR cardiomyopathy stand out for me as a clinician, not only for the highly significant outcome on the primary endpoint but for the consistency of treatment benefit across components of the primary and key secondary endpoints,” said Dr. Gillmore. “These results contribute to my anticipation that acoramidis will provide patients and their providers with an attractive new treatment option that will surely be welcomed across the community.”
A highly statistically significant result, demonstrated by a Win Ratio of 1.8 (p<0.0001), was observed on the primary endpoint (a hierarchical analysis prioritizing in order: ACM, then frequency of CVH, then change from baseline in NT-proBNP, then change from baseline in 6MWD). This result was consistent across both variant and wild-type ATTR-CM patients, as well as across NYHA Class I, II and III patients.
Other key results from the study at Month 30 included:
- An 81% survival rate on acoramidis (versus a 74% survival rate on placebo) for an absolute risk reduction of 6.4% and a relative risk reduction of 25%, despite a ~50% higher rate of tafamidis use on the placebo arm relative to the treatment arm
- The on-treatment 81% survival rate, the highest observed rate in a controlled, prospective study of ATTR-CM patients to the Company’s knowledge, approaches the survival rate in the age-matched US database (~85%)
- Of note, overall 79% of deaths in the study were cardiovascular (CV) in nature, and the results for CV-related mortality were consistent with what was observed on ACM
- The treatment group experienced a 14.9% CV-related mortality rate versus a 21.3% CV-related mortality rate in the placebo group, for a relative risk reduction of 30% on CV-related mortality
- A highly statistically significant relative risk reduction of 50% (p<0.0001) on frequency of CVH
- The 0.29 mean annual CVH frequency on acoramidis approaches the annual hospitalization rate observed in the broader US Medicare population (~0.26)
- A highly statistically significant treatment effect (p<0.0001 in each case) at 30 months on change from baseline in each of NT-proBNP, KCCQ, and 6MWD
- A higher proportion of individuals experienced a reduction (improvement from baseline) in NT-proBNP on acoramidis (45%) relative to placebo (9%)
- A higher proportion of individuals experienced an increase (improvement from baseline) in 6MWD on acoramidis (40%) relative to placebo (22%)
- To the company’s knowledge, these on-treatment proportions of improving patients are higher than have been observed in prior controlled studies of ATTR-CM
- As measured by ex vivo assays of TTR stabilization, acoramidis achieved a greater degree of TTR stabilization as compared to clinically relevant concentrations of tafamidis, independent of TTR genotype
- Serum TTR was promptly and consistently elevated throughout the study in patients receiving acoramidis
- In an exploratory post-hoc analysis of the relationship between on-treatment serum TTR levels and on-treatment measures of CVH, NT-proBNP, and KCCQ, there appears to be an association between the mean on-treatment TTR level and each of these three variables
- In a comparative exploratory post hoc analysis enabled by tafamidis drop-in, albeit at low patient numbers, acoramidis showed a 42% greater increase in serum TTR levels relative to placebo + tafamidis
- Acoramidis was generally well-tolerated with no safety findings of potential clinical concern
“The consistently positive results of ATTRibute-CM, from the primary endpoint and its components to secondary endpoints of mortality, morbidity, physical function and quality of life, further substantiate our hypothesis that highly potent TTR stabilization has the potential to deliver differential benefits to patients,” said Jonathan Fox, M.D., Ph.D., President, and Chief Medical Officer of BridgeBio Cardiorenal. “In particular, we observed absolute survival and hospitalization rates approaching those of similarly aged populations not afflicted with ATTR-CM. That 45% of completers displayed improvement from baseline in NT-proBNP, and 40% walked farther in 6 minutes at study end compared to baseline, are to me remarkable observations in a cohort with a disease commonly described as relentlessly progressive. The prompt and sustained observed increase in serum TTR, an in vivo reflection of increased stabilization, serves to further strengthen the relationship between measures of acoramidis’ ability to avidly bind and stabilize TTR and the read-through to robust clinical benefits for patients with ATTR-CM. We look forward to engaging with health authorities in our continuing efforts to secure acoramidis’ registration that will lead to our bringing acoramidis to ATTR-CM patients as quickly as possible.”
The Company intends to submit its NDA to the US FDA before the end of 2023, with regulatory filings in additional markets to follow in 2024. Acoramidis has intellectual property protection out to at least 2039.
Webcast Information
BridgeBio will host an investor call and simultaneous webcast to discuss the additional data presented at ESC 2023 for the ATTRibute-CM Phase 3 trial on Monday, August 28 at 8:30 am ET. A link to the webcast may be accessed from the event calendar page of BridgeBio’s website at https://investor.bridgebio.com/. A replay of the conference call and webcast will be archived on the Company’s website and will be available for at least 30 days following the event.
About BridgeBio Pharma, Inc.
BridgeBio Pharma Inc. (BridgeBio) is a commercial-stage biopharmaceutical company founded to discover, create, test and deliver transformative medicines to treat patients who suffer from genetic diseases and cancers with clear genetic drivers. BridgeBio’s pipeline of development programs ranges from early science to advanced clinical trials. BridgeBio was founded in 2015 and its team of experienced drug discoverers, developers, and innovators are committed to applying advances in genetic medicine to help patients as quickly as possible. For more information visit bridgebio.com and follow us on LinkedIn and Twitter.
BridgeBio heart drug meets primary endpoint in late-stage trial
Aug. 28, 2023 12:16 AM ET
By: Jonathan Block, SA News Editor
- Acoramidis, in development by BridgeBio (NASDAQ:BBIO) for transthyretin amyloid cardiomyopathy (ATTR-CM), met its primary goal in a phase 3 trial.
- https://seekingalpha.com/news/4006589-bridgebio-heart-drug-meets-primary-endpoint-late-stage-trial
- BridgeBio Pharma, Inc. (BBIO)
- https://bridgebio.com/what-is-attr/
- https://bridgebio.com/
biotecHOPE™ 2023
WELIREG® (belzutifan)
Repotrectinib (TPX-0005, BMS-986472)
WELIREG® (belzutifan)
Merck Announces WELIREG® (belzutifan) Phase 3 LITESPARK-005 Trial Met Primary Endpoint of Progression-Free Survival in Certain Previously Treated Patients With Advanced Renal Cell Carcinoma
August 18, 2023 6:45 am ET
First positive Phase 3 results for WELIREG from LITESPARK-005 showed statistically significant improvements in PFS versus everolimus in these patients
RAHWAY, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced topline results from LITESPARK-005, the first positive Phase 3 trial investigating WELIREG, Merck’s oral hypoxia-inducible factor-2 alpha (HIF-2α) inhibitor. LITESPARK-005 is evaluating WELIREG for the treatment of adult patients with advanced renal cell carcinoma (RCC) that has progressed following PD-1/L1 checkpoint inhibitor and vascular endothelial growth factor-tyrosine kinase inhibitor (VEGF-TKI) therapies. In the trial, WELIREG showed a statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to everolimus, based on a pre-specified interim analysis conducted by an independent Data Monitoring Committee. A statistically significant improvement in the trial’s key secondary endpoint of objective response rate (ORR) was also demonstrated. A trend toward improvement in overall survival (OS), a dual primary endpoint, was observed; however, this result did not reach statistical significance. OS will be tested at a subsequent analysis. The safety profile of WELIREG in this trial was consistent with that observed in previously reported studies. Results will be presented at an upcoming medical meeting and shared with regulatory authorities.
“Patients with advanced RCC face low survival rates, and for those whose cancer progresses following PD-1/L1 and VEGF-TKI therapies, there is a need for new treatment options that can reduce their risk of disease progression or death,” said Dr. Marjorie Green, senior vice president and head of late-stage oncology, global clinical development, Merck Research Laboratories. “This is the first Phase 3 trial to show positive results in advanced RCC following these therapies and the first new mechanism to demonstrate potential in advanced RCC in recent years. We look forward to discussing these results with health authorities.”
WELIREG was the first HIF-2α inhibitor therapy approved in the U.S. and is currently approved in the U.S., Great Britain, Canada and several other countries for the treatment of adult patients with von Hippel-Lindau (VHL) disease who require therapy for associated RCC, central nervous system hemangioblastomas, or pancreatic neuroendocrine tumors, not requiring immediate surgery, based on ORR and duration of response (DOR) data from the Phase 2 LITESPARK-004 trial. Additional applications are currently under regulatory agency review worldwide based on LITESPARK-004.
LITESPARK-005 is part of a comprehensive development program for WELIREG comprised of four Phase 3 trials in RCC, including LITESPARK-011 and LITESPARK-012, evaluating WELIREG in the second-line and treatment-naïve advanced disease settings, and LITESPARK-022, evaluating WELIREG in the adjuvant setting.
About LITESPARK-005
LITESPARK-005 is a randomized, open-label Phase 3 trial (ClinicalTrials.gov, NCT04195750) evaluating WELIREG compared to everolimus for the treatment of patients with advanced RCC that has progressed after prior treatment with PD-1/L1 and VEGF-TKI therapies, in sequence or in combination. The dual primary endpoints are PFS and OS. Secondary endpoints include ORR, DOR and safety and tolerability. The trial enrolled 746 patients who were randomized to receive WELIREG (120 mg orally once daily) or everolimus (10 mg orally once daily).
About renal cell carcinoma
Renal cell carcinoma is by far the most common type of kidney cancer; about nine out of 10 kidney cancer diagnoses are RCCs. Renal cell carcinoma is about twice as common in men than in women. Most cases of RCC are discovered incidentally during imaging tests for other abdominal diseases. In the U.S., approximately 15% of patients with kidney cancer are diagnosed at an advanced stage.
About WELIREG® (belzutifan) 40 mg tablets, for oral use
Indication in the U.S.
WELIREG (belzutifan) is indicated for the treatment of adult patients with von Hippel-Lindau (VHL) disease who require therapy for associated renal cell carcinoma (RCC), central nervous system (CNS) hemangioblastomas, or pancreatic neuroendocrine tumors (pNET), not requiring immediate surgery.
Merck’s focus on cancer
Our goal is to translate breakthrough science into innovative oncology medicines to help people with cancer worldwide. At Merck, the potential to bring new hope to people with cancer drives our purpose and supporting accessibility to our cancer medicines is our commitment. As part of our focus on cancer, Merck is committed to exploring the potential of immuno-oncology with one of the largest development programs in the industry across more than 30 tumor types. We also continue to strengthen our portfolio through strategic acquisitions and are prioritizing the development of several promising oncology candidates with the potential to improve the treatment of advanced cancers. For more information about our oncology clinical trials, visit www.merck.com/clinicaltrials.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on Twitter, Facebook, Instagram, YouTube and LinkedIn.
Please see Prescribing Information, including information for the Boxed Warning about embryo-fetal toxicity, for WELIREG (belzutifan) at https://www.merck.com/product/usa/pi_circulars/w/welireg/welireg_pi.pdf and Medication Guide for WELIREG at https://www.merck.com/product/usa/pi_circulars/w/welireg/welireg_mg.pdf .
Source: Merck & Co., Inc.
Merck succeeds in Phase 3 trial for kidney cancer drug
Aug. 18, 2023 7:20 AM ET
By: Dulan Lokuwithana, SA News Editor
Merck (NYSE:MRK) announced Friday that its Phase 3 LITESPARK-005 trial reached the primary endpoint of progression-free survival in adults with advanced renal cell carcinoma who received its FDA-approved rare disease drug Welireg.
Welireg is an oral therapy indicated in the U.S. for adults with von Hippel-Lindau disease, a rare multi-system disorder characterized by non-cancerous tumor growth in various parts of the body.
Citing topline data from LITESPARK-005, the New Jersey-based pharma giant said Welireg indicated an improvement in progression-free survival (PFS) with statistically significant and clinically meaningful effects against the comparator.
https://seekingalpha.com/news/4004283-merck-wins-phase-3-trial-kidney-cancer-drug-welireg
ODRONEXTAMAB
Repotrectinib (TPX-0005, BMS-986472)
WELIREG® (belzutifan)
August 17, 2023 at 8:30 AM EDT
ODRONEXTAMAB RECEIVES EMA FILING ACCEPTANCE FOR TREATMENT OF RELAPSED/REFRACTORY FOLLICULAR LYMPHOMA AND DIFFUSE LARGE B-CELL LYMPHOMA
TARRYTOWN, N.Y., Aug. 17, 2023 (GLOBE NEWSWIRE) -- Regeneron Pharmaceuticals, Inc. (NASDAQ: REGN) today announced that the European Medicines Agency (EMA) has accepted for review the Marketing Authorization Application (MAA) for odronextamab to treat adult patients with relapsed/refractory (R/R) follicular lymphoma (FL) or R/R diffuse large B-cell lymphoma (DLBCL), who have progressed after at least two prior systemic therapies. The EMA previously granted odronextamab Orphan Drug Designation for FL and DLBCL. Odronextamab is an investigational CD20xCD3 bispecific antibody designed to bridge CD20 on cancer cells with CD3-expressing T cells to facilitate local T-cell activation and cancer-cell killing.
FL and DLBCL are the two most common subtypes of B-cell non-Hodgkin lymphoma (B-NHL). FL is a slow-growing subtype, with patients often relapsing within five years. DLBCL is an aggressive subtype, with up to 50% of high-risk patients experiencing progression after first-line treatment (e.g., relapsing or refractory to treatment). As these blood cancers progress, they become increasingly hard to treat, especially in the third-line setting and beyond, leaving patients with few treatment options.
The MAA is supported by data from a Phase 1 and pivotal Phase 2 trial (ELM-1 and ELM-2) investigating odronextamab in FL and DLBCL, which were last presented at the 64th American Society of Hematology Annual Meeting.
Regeneron is conducting a broad Phase 3 development program to further investigate odronextamab in earlier lines of therapy and additional B-NHLs, representing one of the largest clinical programs in lymphoma. Odronextamab is currently under clinical development, and its safety and efficacy have not been fully evaluated by any regulatory authority.
About the Odronextamab Trials
ELM-2 is an ongoing, open-label, multicenter Phase 2 trial investigating odronextamab in more than 500 patients across five independent disease-specific cohorts, including DLBCL, FL, mantle cell lymphoma, marginal zone lymphoma and other subtypes of B-NHL. The primary endpoint is objective response rate according to the Lugano Classification, and secondary endpoints include complete response, progression-free survival, overall survival, duration of response, disease control rate, safety and quality of life.
ELM-1 is an ongoing, open-label, multicenter Phase 1 trial to investigate the safety and tolerability of odronextamab in patients with CD20+ B-cell malignancies previously treated with CD20-directed antibody therapy.
About Regeneron’s Approach to Cancer Research
At Regeneron, we’re applying more than three decades of scientific innovation with the goal of developing paradigm-changing therapies for patients with cancer.
Our portfolio is built around two foundational approaches – our approved PD-1 inhibitor Libtayo and investigational bispecific antibodies – which are being evaluated both as monotherapies and in combination with emerging therapeutic modalities. Together, they provide us with unique combinatorial flexibility to develop potentially synergistic treatments for a wide range of solid tumors and blood cancers.
If you are interested in learning more about our clinical trials, please contact us (clinicaltrials@regeneron.com or 844-734-6643) or visit our clinical trials website.
About Regeneron
Regeneron (NASDAQ: REGN) is a leading biotechnology company that invents, develops and commercializes life-transforming medicines for people with serious diseases. Founded and led for 35 years by physician-scientists, our unique ability to repeatedly and consistently translate science into medicine has led to numerous FDA-approved treatments and product candidates in development, almost all of which were homegrown in our laboratories. Our medicines and pipeline are designed to help patients with eye diseases, allergic and inflammatory diseases, cancer, cardiovascular and metabolic diseases, hematologic conditions, infectious diseases and rare diseases.
Regeneron is accelerating and improving the traditional drug development process through its proprietary VelociSuite® technologies, such as VelocImmune®, which uses unique genetically humanized mice to produce optimized fully human antibodies and bispecific antibodies, and through ambitious research initiatives such as the Regeneron Genetics Center®, which is conducting one of the largest genetics sequencing efforts in the world.
For additional information about Regeneron, please visit www.regeneron.com or follow Regeneron on LinkedIn.
![]()
Source: Regeneron Pharmaceuticals, Inc.
Regeneron lymphoma therapy accepted for EU review
Aug. 17, 2023 9:28 AM ET
Regeneron Pharmaceuticals, Inc. (REGN)
By: Dulan Lokuwithana, SA News Editor
- Regeneron (NASDAQ:REGN) announced Thursday that the European Medicines Agency (EMA) accepted its marketing application for the bispecific antibody odronextamab to review it as a late-line option for adults with lymphoma, a cancer of the lymphatic system.
- Regeneron’s (REGN) marketing authorization application (MAA) for odronextamab targets adults with relapsed or refractory (R/R) follicular lymphoma or R/R diffuse large B-cell lymphoma who have received at least two prior lines of therapy.
- https://seekingalpha.com/news/4003958-regeneron-granted-eu-review-lymphoma-drug
- Regeneron Pharmaceuticals, Inc. (REGN)
- https://www.regeneron.com/
Repotrectinib (TPX-0005, BMS-986472)
Repotrectinib (TPX-0005, BMS-986472)
AKEEGA™ (Niraparib and Abiraterone Acetate)
Updated Data from TRIDENT-1 Trial Show Durable Efficacy Benefits with Repotrectinib for Patients with Locally Advanced or Metastatic ROS1-Positive Non-Small Cell Lung Cancer
08/16/2023
CATEGORY:
Repotrectinib continued to demonstrate high response rates and durable responses, including robust intracranial responses, in patients with ROS1-positive locally advanced or metastatic non-small cell lung cancer who were TKI-naïve or previously treated with one TKI and no chemotherapy
Median duration of response and progression-free survival to be disclosed for the first time in the pooled Phase 1/2 population alongside updated results at the IASLC 2023 World Conference on Lung Cancer hosted by the International Association for the Study of Lung Cancer
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE: BMY) today announced updated results from the registrational TRIDENT-1 study, demonstrating that repotrectinib, a next-generation ROS1/TRK tyrosine kinase inhibitor (TKI), continued to show high response rates and durable responses in patients with ROS1-positive locally advanced or metastatic non-small cell lung cancer (NSCLC). Updated results will be featured in an oral presentation (Abstract #OA03.06) at the IASLC 2023 World Conference on Lung Cancer (#WCLC23) hosted by the International Association for the Study of Lung Cancer on September 10, 2023, from 1:02 a.m. to 1:12 a.m. EDT / 1:02 p.m. to 1:12 p.m. SGT.
Based on results from the TRIDENT-1 trial, the U.S. Food and Drug Administration accepted the New Drug Application for repotrectinib for the treatment of patients with ROS1-positive locally advanced or metastatic NSCLC and granted Priority Review; a Prescription Drug User Fee Act goal date of November 27, 2023 was assigned.
In this updated analysis, repotrectinib continued to demonstrate durable efficacy in patients with ROS1-positive NSCLC, including intracranial activity, in patients who were TKI-naïve or previously treated with one TKI and no chemotherapy. Median duration of response (DOR) and median progression-free survival (PFS) will also be disclosed for the first time in the pooled Phase 1 and Phase 2 population of patients with ROS1-positive NSCLC:
- In TKI-naïve patients (n=71) with median follow-up of 24.0 months, confirmed objective response rate (cORR) by Blinded Independent Central Review (BICR) was 79%, median DOR and PFS were 34.1 months and 35.7 months, respectively. In patients with measurable brain metastases at baseline (n=9), intracranial ORR per BICR was 89% and responses were prolonged.
- In patients who had been previously treated with one TKI and no chemotherapy (n=56) with median follow-up of 21.5 months, cORR by BICR was 38%, and median DOR and PFS were 14.8 months and 9.0 months, respectively. In this subset of patients with measurable brain metastases at baseline (n=13), intracranial ORR per BICR was 38%.
- At the recommended dose for Phase 2, the safety profile of repotrectinib was manageable and remained consistent with previous reports.
“The data from the TRIDENT-1 trial hold great significance in the field of non-small cell lung cancer research, as they add to the growing body of evidence pointing toward durable results with repotrectinib in patients who test positive for ROS1 gene fusions,” said Byoung Chul Cho, M.D., Ph.D., Yonsei Cancer Center, Yonsei University College of Medicine, DAAN Cancer Laboratory. “With these results, we are seeing durable benefit, including in the brain, in patients with ROS1-positive NSCLC that differentiates repotrectinib from existing agents and is especially impressive in the context of historic data with current ROS1 TKIs. This targeted therapy has true potential to change the treatment landscape and become a new standard of care for patients with ROS1-positive NSCLC.”
“These updated results reflect the potential of repotrectinib as a best-in-class ROS1 inhibitor. Furthermore, the data offer hope for the patients with ROS1-positive non-small cell lung cancer who still face high remaining unmet needs,” said Joseph Fiore, executive director, global program lead, repotrectinib, Bristol Myers Squibb. “Building on our heritage of transformational science with immunotherapy in the treatment of NSCLC, we are excited to advance this next-generation precision medicine, which has shown an unprecedented level of durability of responses and robust intracranial responses in patients with ROS1-positive NSCLC, so that it can hopefully help patients in their fight against cancer.”
The study remains ongoing to assess long-term outcomes and additional endpoints across patient populations with ROS1-positive locally advanced or metastatic NSCLC and NTRK-positive advanced solid tumors. Bristol Myers Squibb thanks the patients and investigators involved with the TRIDENT-1 clinical trial.
Turning Point Therapeutics is a wholly owned subsidiary of the Bristol-Myers Squibb Company. As of August 2022, Bristol Myers Squibb acquired the leading clinical stage precision oncology company and its pipeline of investigational drugs across precision oncology and advanced solid tumors, including repotrectinib.
About TRIDENT-1
TRIDENT-1 is a Phase 1/2 open-label, global, multi-center, first-in-human clinical trial evaluating the safety, tolerability, pharmacokinetics and anti-tumor activity of repotrectinib (TPX-0005, BMS-986472) in patients with advanced solid tumors, including non-small cell lung cancer (NSCLC). Phase 1 of the trial includes several primary and secondary safety and pharmacokinetics endpoints. Phase 2 of the trial has a primary endpoint of overall response rate (ORR) as assessed by Blinded Independent Central Review (BICR) using RECIST v1.1 and key secondary endpoints including duration of response (DOR), time to response (TTR), progression-free survival (PFS), overall survival (OS) and clinical benefit rate (CBR) in six distinct expansion cohorts, including tyrosine kinase inhibitor (TKI)-naïve and TKI-pretreated patients with ROS1-positive locally advanced or metastatic NSCLC and NTRK-positive advanced solid tumors.
About Lung Cancer
Lung cancer is the leading cause of cancer deaths globally. Non-small cell lung cancer (NSCLC) is one of the most common types of lung cancer, representing up to 84% of diagnoses. Survival rates vary depending on the stage and type of the cancer when diagnosed. ROS1 fusions are rare and occur in about 1-2% of patients with NSCLC. Patients with tumors that are ROS1-positive tend to be younger than the average patient with lung cancer, more often female and may have little to no smoking history. Per international treatment guidelines, ROS1 targeted agents are preferred in patients with a tumor harboring this alteration.
Bristol Myers Squibb: Creating a Better Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision — transforming patients’ lives through science. The goal of the company’s cancer research is to deliver medicines that offer each patient a better, healthier life and to make cure a possibility. Building on a legacy across a broad range of cancers that have changed survival expectations for many, Bristol Myers Squibb researchers are exploring new frontiers in personalized medicine, and through innovative digital platforms, are turning data into insights that sharpen their focus. Deep scientific expertise, cutting-edge capabilities and discovery platforms enable the company to look at cancer from every angle. Cancer can have a relentless grasp on many parts of a patient’s life, and Bristol Myers Squibb is committed to taking actions to address all aspects of care, from diagnosis to survivorship. Because as a leader in cancer care, Bristol Myers Squibb is working to empower all people with cancer to have a better future.
About Repotrectinib
Repotrectinib (TPX-0005, BMS-986472) is a next-generation, potential best-in-class tyrosine kinase inhibitor (TKI) targeting ROS1- or NTRK-positive locally advanced or metastatic solid tumors, including non-small cell lung cancer (NSCLC), where there remain significant unmet medical needs for patients. Repotrectinib was designed to improve durability of response and with favorable properties to enhance intracranial activity. It is being studied in a registrational Phase 1/2 trial primarily in adults and a Phase 1/2 trial in pediatric patients.
In June 2017, repotrectinib was granted an Orphan Drug designation by the U.S. Food and Drug Administration (FDA). Since then, repotrectinib has demonstrated clinically meaningful results and was granted three Breakthrough Therapy Designations (BTDs) by the FDA for the treatment of patients with: ROS1-positive metastatic NSCLC who have not been treated with a ROS1 TKI; ROS1-positive metastatic NSCLC who have been previously treated with one ROS1 TKI and who have not received prior platinum-based chemotherapy; and advanced solid tumors that have an NTRK gene fusion who have progressed following treatment with one or two prior tropomyosin receptor kinase (TRK) TKIs (with or without prior chemotherapy) and have no satisfactory alternative treatments.
Repotrectinib was also previously granted four fast-track designations in patients with: ROS1-positive advanced NSCLC who have been treated with disease progression following one prior line of platinum-based chemotherapy and one prior line of a ROS1 TKI; ROS1-positive advanced NSCLC who have not been treated with a ROS1 TKI; ROS1-positive advanced NSCLC who have been previously treated with one ROS1 TKI and who have not received prior platinum-based chemotherapy; and advanced solid tumors that have an NTRK gene fusion who have progressed following treatment with at least one prior line of chemotherapy and one or two prior TRK TKIs and have no satisfactory alternative treatments.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
Multimedia Files:
 Download:Download original 99 KB 1505 x 211Download thumbnail 5 KB 200 x 28Download lowres 15 KB 480 x 67Download square 7 KB 250 x 250
Download:Download original 99 KB 1505 x 211Download thumbnail 5 KB 200 x 28Download lowres 15 KB 480 x 67Download square 7 KB 250 x 250
BMY Dividend History
https://www.nasdaq.com/market-activity/stocks/bmy/dividend-history
BMY Bristol-Myers Squibb Company
AKEEGA™ (Niraparib and Abiraterone Acetate)
REQORSA® Immunogene Therapy (quratusugene ozeplasmid),
AKEEGA™ (Niraparib and Abiraterone Acetate)
U.S. FDA Approves AKEEGA™ (Niraparib and Abiraterone Acetate), the First-And-Only Dual Action Tablet for the Treatment of Patients with BRCA-Positive Metastatic Castration-Resistant Prostate Cancer
Approval is based on the Phase 3 MAGNITUDE study, a prospectively designed precision medicine study including the largest population of BRCA-positive patients in combination trials to date with metastatic castration-resistant prostate cancer (mCRPC)
AKEEGA™ plus prednisone significantly improved radiographic progression-free survival compared to abiraterone acetate plus prednisone (AAP) in patients with BRCA-positive mCRPC
HORSHAM, Pa., August 11, 2023 – The Janssen Pharmaceutical Companies of Johnson & Johnson today announced that the U.S. Food & Drug Administration (FDA) has approved AKEEGA™ (niraparib and abiraterone acetate), the first-and-only dual action tablet combining a PARP inhibitor with abiraterone acetate, given with prednisone, for the treatment of adult patients with deleterious or suspected deleterious BRCA-positive mCRPC, as detected by an FDA-approved test.1
“As a physician, identifying patients with a worse prognosis is a priority, especially those whose cancers have a BRCA mutation,” said Kim Chi, M.D.*, Medical Oncologist at BC Cancer – Vancouver and principal investigator of the Phase 3 MAGNITUDE study. “We prospectively designed the MAGNITUDE study to identify the subset of patients most likely to benefit from targeted treatment with AKEEGA and to help us understand how we can potentially achieve better health outcomes for patients.”
Prostate cancer is one of the most common cancers in the U.S., with an estimated 288,300 new cases and nearly 35,000 deaths expected in 2023.2 Approximately 10 to 15 percent of patients with mCRPC have BRCA gene alterations. Patients with BRCA-positive mCRPC are more likely to have aggressive disease and may experience poor outcomes and a shorter survival time.3,4,5,6,7
“The approval of AKEEGA brings an important treatment option to patients with prostate cancer as they consider their road ahead, and it also highlights the importance of genetic testing and precision medicine for this disease,” said Shelby Moneer, MS, CHES**, Vice President of Patient Programs and Education, ZERO Prostate Cancer. “All individuals diagnosed with prostate cancer should consider genetic testing, especially those from racial and ethnic minority groups who tend to have worse cancer outcomes. This is imperative to close the racial and ethnic disparities in prostate cancer health outcomes.”
The FDA approval is based on positive results from the randomized, double-blind, placebo-controlled multi-center Phase 3 MAGNITUDE study. In BRCA-positive patients treated with the combination AKEEGA™ plus prednisone, a statistically significant 47 percent risk reduction was observed for radiographic progression-free survival (rPFS) (Hazard ratio [HR], 0.53; p=0.001). At the second interim analysis (IA2), with median follow-up at 24.8 months in the BRCA-positive subgroup, rPFS by central review demonstrated a consistent trend favoring AKEEGA™ plus prednisone, with a median rPFS of 19.5 months compared with 10.9 months for placebo and AAP (HR, 0.55 [95 percent confidence interval (CI), 0.39-0.78]). Additionally, there was an observed improvement in the secondary endpoints of time to symptomatic progression (TSP) (HR, 0.54 [95 percent CI, 0.35-0.85]) and time to initiation of cytotoxic chemotherapy (TCC) (HR, 0.56 [95 percent CI, 0.35-0.90]) for AKEEGA™ plus prednisone compared with AAP alone, supported by a trend towards improvement in overall survival (OS) (HR, 0.88 [95 percent CI, 0.58-1.34]).
The observed safety profile of the combination of AKEEGA™ plus prednisone was consistent with the known safety profile of each FDA-approved monotherapy. Of the patients in the MAGNITUDE study with a BRCA gene alteration, 41 percent who received AKEEGA™ experienced a serious adverse event (AE). The most common AEs occurring in 20 percent or more of patients who received AKEEGA™ plus prednisone versus patients who received placebo and AAP were musculoskeletal pain (44 percent vs. 42 percent, respectively), fatigue (43 percent vs. 30 percent), constipation (34 percent vs. 20 percent), hypertension (33 percent vs. 27 percent) and nausea (33 percent vs. 21 percent). Permanent discontinuation of any component of AKEEGA™ due to an adverse reaction occurred in 15 percent of patients.
“Janssen’s legacy of advancing the science of prostate cancer has contributed to the evolution of transformational treatment approaches for more than a decade,” said Kiran Patel, M.D., Vice President, Clinical Development, Solid Tumors, Janssen Research & Development, LLC. “This milestone, which marks the approval of Janssen’s third prostate cancer treatment, highlights the importance of advancing precision medicine approaches and genetic testing for the treatment of patients with BRCA-positive mCRPC.”
About AKEEGA™
AKEEGA™ (niraparib and abiraterone acetate) is the first-and-only orally administered, once daily dual action tablet (DAT) of niraparib, a highly selective poly (ADP-ribose) polymerase (PARP) inhibitor, and abiraterone acetate, an androgen biosynthesis inhibitor. The novel DAT combination therapy targets two oncogenic drivers in patients with mCRPC and HRR gene alterations. AKEEGA™ is indicated with prednisone for the treatment of adults with mCRPC and BRCA-positive mutations. The recommended starting dose is 200 mg niraparib/1,000 mg abiraterone acetate (two tablets). The 100 mg niraparib/1,000 mg abiraterone acetate dose option (two tablets) is available for dose reduction.
In April 2016, Janssen Biotech, Inc. entered a worldwide (except Japan) collaboration and license agreement with TESARO, Inc. (acquired by GlaxoSmithKline [GSK] in 2019) for exclusive rights to niraparib in prostate cancer.
About Metastatic Castration-Resistant Prostate Cancer
Metastatic castration-resistant prostate cancer characterizes cancer that no longer responds to androgen deprivation therapy and has spread to other parts of the body. The most common metastatic sites are bones, followed by lungs and liver. Prostate cancer is the second most common cancer in men worldwide, behind lung cancer. More than one million patients around the world are diagnosed with prostate cancer each year. Patients with mCRPC and HRR gene alterations, of which BRCA mutations are the most common, are more likely to have aggressive disease, poor outcomes and a shorter survival time.2,3,4,5
About MAGNITUDE
MAGNITUDE (NCT03748641) is a Phase 3, randomized, double-blind, placebo-controlled, multi-center clinical study evaluating the safety and efficacy of the combination of AKEEGA™ plus prednisone for patients with mCRPC, with or without certain HRR gene alterations, and who have not received prior therapy for mCRPC except for up to four months of AAP.
The study included patients with (HRR biomarker [BM] positive; ATM, BRCA1, BRCA2, BRIP1, CDK12, CHEK2, FANCA, HDAC2, PALB2) and without specified gene alterations (HRR BM negative), who were randomized 1:1 to receive niraparib 200 mg once daily plus AAP or placebo plus AAP.8 A total of 423 patients with HRR gene alterations were enrolled, 225 (53.2 percent) of whom had BRCA mutations.9,10,11 The primary endpoint of the MAGNITUDE trial was rPFS assessed by blinded independent central review.12 Secondary endpoints included TCC, TSP and OS. Analysis of the group of patients with BRCA alterations was alpha controlled for rPFS and prespecified for other endpoints.
Access to AKEEGA™ (niraparib and abiraterone acetate)
Once a patient and their doctor have decided that AKEEGA™ is right for the patient, Janssen can help find the resources patients may need to get started and stay on therapy. Janssen offers support navigating the payer processes to assist patients in gaining access to AKEEGA™. We can provide information on insurance coverage and potential out-of-pocket costs and identify options that may help make AKEEGA™ more affordable. If patients have commercial or private health insurance and need help paying for AKEEGA™, the Janssen CarePath Savings Program may be able to help. To learn more about access and affordability support visit JanssenCarePath.com or call 1-877-CarePath (1-877-227-3728). We also offer personalized support for patients that provides one-on-one guidance, information, and educational resources, which includes helping them explore cost support options. Patients can get connected to dedicated support from our Care Navigators by calling Janssen Compass® directly at 844-628-1234 or by visiting JanssenCompass.com and requesting an introductory call. Janssen Compass® is limited to education for patients about their Janssen therapy, its administration, and/or their disease. It is intended to supplement a patient’s understanding of their therapy and is not intended to provide medical advice, replace a treatment plan from the patient’s doctor or nurse, provide case management services, or serve as a reason to prescribe a Janssen medication.
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we’re creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com. Follow us at @JanssenGlobal and @JanssenUS. Janssen Biotech, Inc. and Janssen Research & Development, LLC are part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
JNJ Dividend History
https://www.nasdaq.com/market-activity/stocks/jnj/dividend-history
TALVEY™ (talquetamab-tgvs)
REQORSA® Immunogene Therapy (quratusugene ozeplasmid),
REQORSA® Immunogene Therapy (quratusugene ozeplasmid),
U.S. FDA Approves TALVEY™ (talquetamab-tgvs), a First-in-Class Bispecific Therapy for the Treatment of Patients with Heavily Pretreated Multiple Myeloma
Bispecific antibody targeting GPRC5D receptor showed an overall response rate of more than
70 percent with durable responses, including in patients previously treated with a bispecific antibody or CAR-T cell therapy
HORSHAM, Pa., Aug. 10, 2023 – The Janssen Pharmaceutical Companies of Johnson & Johnson announced today that the U.S. Food and Drug Administration (FDA) has granted accelerated approval of TALVEY™ (talquetamab-tgvs), a first-in-class bispecific antibody for the treatment of adult patients with relapsed or refractory multiple myeloma who have received at least four prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 antibody.1 This indication is approved under accelerated approval based on response rate and durability of response.1 Continued approval for this indication is contingent upon verification and description of clinical benefit in confirmatory trial(s).1
TALVEY™ is a bispecific T-cell engaging antibody that binds to the CD3 receptor on the surface of T cells and G protein-coupled receptor class C group 5 member D (GPRC5D) expressed on the surface of multiple myeloma cells, non-malignant plasma cells and healthy tissue such as epithelial cells in keratinized tissues of the skin and tongue.1 TALVEY™ is approved as a weekly or biweekly subcutaneous (SC) injection after an initial step-up phase, offering physicians the flexibility to determine the optimal treatment regimen for patients.1
“The clinically meaningful efficacy and safety profile observed with talquetamab in heavily pretreated patients in this clinical trial, which included patients treated with prior BCMA-targeted bispecific or CAR-T cell therapy, has been notable,” said Ajai Chari, M.D., Director of Multiple Myeloma Program, Professor of Clinical Medicine at the University of California, San Francisco.* “Patients at this stage of disease have a poor prognosis. Talquetamab as a first-in-class therapy is a new option for patients with this difficult-to-treat blood cancer.”
The talquetamab Phase 2 MonumenTAL-1 study, which included patients who had received at least four prior lines of therapy and who were not exposed to prior T-cell redirection therapy (n=187), showed meaningful overall response rates (ORR).1 At the SC biweekly dose of 0.8 mg/kg, 73.6 percent of patients (95 percent Confidence Interval [CI], range, 63.0 to 82.4) achieved an ORR.1 With a median follow-up of nearly 6 (range, 0 to 9.5) months from first response among responders, 58 percent of patients achieved a very good partial response (VGPR) or better, including 33 percent of patients achieving a complete response (CR) or better.1 At the SC weekly dose of 0.4 mg/kg, 73.0 percent of patients (95 percent CI, range, 63.2 to 81.4) achieved an ORR.1 With a median follow-up of nearly 14 (range, 0.8 to 15.4) months from first response among responders, 57 percent of patients achieved a VGPR or better, including 35 percent of patients achieving a CR or better.1 Responses were durable with a median duration of response not reached in the 0.8 mg/kg SC biweekly dose group and 9.5 months in the 0.4 mg/kg SC weekly dose group.1 Among patients receiving the 0.8 mg/kg SC biweekly dose, an estimated 85 percent of responders maintained response for at least 9 months.1
The MonumenTAL-1 study also included 32 patients who were exposed to prior bispecific antibody or CAR-T cell therapy (94 percent B-cell maturation antigen [BCMA]-directed therapy) and had received at least four prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody, received TALVEY at the 0.4 mg/kg SC weekly dose.1 With a median duration of follow-up of 10.4 months, 72 percent of patients (95 percent CI, range, 53 to 86) achieved an ORR per an Independent Review Committee assessment, and an estimated 59 percent of responders maintained response for at least 9 months.1
The Safety Profile for TALVEY™ includes a Boxed Warning for cytokine release syndrome (CRS) and neurologic toxicity including immune effector cell-associated neurotoxicity syndrome (ICANS); Warnings and Precautions include Oral Toxicity and Weight Loss, Infections, Cytopenias, Skin Toxicity, Hepatoxicity and Embryo-fetal toxicity. The most common adverse reactions (≥20 percent) are pyrexia, CRS, dysgeusia, nail disorder, musculoskeletal pain, skin disorder, rash, fatigue, weight decreased, dry mouth, xerosis, dysphagia, upper respiratory tract infection, diarrhea, hypotension, and headache. The most common Grade 3 or 4 laboratory abnormalities (≥30 percent) are lymphocyte count decreased, neutrophil count decreased, white blood cell decreased, and hemoglobin decreased.1
"Although options for the treatment of multiple myeloma have expanded significantly in recent years, the disease remains incurable, and therefore, patients are in need of new treatment options,” said Michael Andreini, President and Chief Executive Officer, Multiple Myeloma Research Foundation.† “Today’s approval of talquetamab provides patients with a new treatment approach for relapsed or refractory disease that is a welcome addition to the myeloma community.”
“The approval of TALVEY, our fifth innovative therapy and second bispecific antibody approved for the treatment of multiple myeloma, demonstrates our commitment to expanding our portfolio of medicines to help address unmet needs for patients who continue to face challenges with this complex hematologic malignancy,” said Peter Lebowitz, M.D., Ph.D., Global Therapeutic Area Head, Oncology, Janssen Research & Development, LLC. “Our team of scientists never settles in their determination to discover and develop effective therapies. With the discovery of this new antigen, we continue to strive for research breakthroughs while remaining focused on delivering curative regimens in our commitment to eliminate cancer.”
TALVEY™ is available only through a restricted program called the TECVAYLI® and TALVEY™ Risk Evaluation and Mitigation Strategy (REMS).1 Details of the Important Safety Information are included below.
The most common non-hematologic adverse events observed in the study were oral toxicities, which occurred in 80 percent of patients, with Grade 3 occurring in 2.1 percent of patients.1 The most frequent oral toxicities were dysgeusia (49 percent), dry mouth (34 percent), dysphagia (23 percent), and ageusia (18 percent).1 In addition, 62 percent of patients experienced weight loss, including 29 percent with Grade 2 weight loss and 2.7 percent with Grade 3 weight loss.1 Serious infections occurred in 16 percent of patients, with fatal infections occurring in 1.5 percent of patients.1 Grade 3 or 4 serious infections occurred in 17 percent of patients.1 Grade 3 or 4 decreased neutrophils occurred in 35 percent of patients and decreased platelets occurred in 22 percent of patients.1 Skin reactions occurred in 62 percent of patients, with Grade 3 skin reactions in 0.3 percent.1 Permanent discontinuation of TALVEY™ due to an adverse reaction occurred in 9 percent of patients.1
About the MonumenTAL-1 Study
MonumenTAL-1 (Phase 1: NCT03399799, Phase 2: NCT04634552) is a Phase 1/2 single-arm, open-label, multicohort, multicenter dose-escalation study involving over 300 patients.2,3 Phase 1 evaluated the safety and efficacy of TALVEY™ in adults with relapsed or refractory multiple myeloma who received three or more prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.1,2 The study excluded patients who experienced T-cell redirection therapy within 3 months, prior Grade 3 or higher CRS related to any T-cell redirection therapy, an autologous stem cell transplant within the past 12 weeks, an allogenic stem cell transplant within the past 6 months, Eastern Cooperative Oncology Group (ECOG) performance score of 3 or higher, stroke or seizure within the past 6 months, CNS involvement or clinical signs of meningeal involvement of multiple myeloma, and plasma cell leukemia, active or documented history of autoimmune disease (exception of vitiligo, resolved childhood atopic dermatitis or resolved Grave’s Disease that is euthyroid based on clinical and laboratory testing).1,2
Phase 2 of the study evaluated the efficacy of TALVEY™ in participants with relapsed or refractory multiple myeloma at the recommended Phase 2 dose(s) (RP2Ds), established at SC 0.4 mg/kg weekly and 0.8 mg/kg every two weeks, respectively.3 Efficacy was based on overall response rate (ORR) and duration of response (DOR) as assessed by an Independent Review Committee using IMWG criteria.3
TECVAYLI® and TALVEY™ REMS: TALVEY™ is available only through a restricted program under a REMS called the TECVAYLI® and TALVEY™ REMS because of the risks of CRS and neurologic toxicity, including ICANS.
Further information about the TECVAYLI® and TALVEY™ REMS program is available at www.TEC-TALREMS.com or by telephone at 1-855-810-8064.
Please read full Prescribing Information including Boxed Warning for TALVEY™.
About TALVEY™
TALVEY™ is a bispecific T-cell engaging antibody that binds to the CD3 receptor expressed on the surface of T cells and G protein-coupled receptor class C group 5 member D (GPRC5D), a novel multiple myeloma target which is highly expressed on the surface of multiple myeloma cells and non-malignant plasma cells, as well as some healthy tissues such as epithelial cells of the skin and tongue.1
TALVEY™ is currently being investigated in combination and in sequence across all lines of multiple myeloma in studies with other bispecific antibodies as well as with existing standards of care. In addition to a Phase 1/2 clinical study of TALVEY™ for the treatment of relapsed or refractory multiple myeloma, TALVEY™ is also being evaluated in combination studies (NCT04586426, NCT04108195, NCT05050097, NCT05338775) and in a randomized Phase 3 study (NCT05455320).
In May 2021 and August 2021, TALVEY™ was granted Orphan Drug Designation for the treatment of multiple myeloma by the U.S. FDA and the European Commission, respectively. TALVEY™ was also granted Breakthrough Therapy Designation from the U.S. FDA in June 2022 for the treatment of adult patients with relapsed or refractory multiple myeloma who have previously received at least four prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 antibody. The approval follows the FDA’s decision in February 2023 to initiate a Priority Review of the Biologics License Application (BLA) submitted in December 2022.
About Multiple Myeloma
Multiple myeloma is an incurable blood cancer that affects a type of white blood cell called plasma cells, which are found in the bone marrow.4 In multiple myeloma, these plasma cells change, spread rapidly and replace normal cells in the bone marrow with tumors.5 Multiple myeloma is the third most common blood cancer and remains an incurable disease.6 In 2023, it is estimated that more than 35,000 people will be diagnosed with multiple myeloma in the U.S. and more than 12,000 people will die from the disease.7 People living with multiple myeloma have a 5-year relative survival rate of 59.8 percent.8 While some people diagnosed with multiple myeloma initially have no symptoms, most patients are diagnosed due to symptoms that can include bone fracture or pain, low red blood cell counts, tiredness, high calcium levels and kidney problems or infections.9,10
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we are creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com. Follow us at @JanssenUS and @JanssenGlobal. Janssen Biotech, Inc., and Janssen Research & Development, LLC, are part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
* Dr. Chari has served as a paid consultant to Janssen; he has not been paid for any media work.
† Mr. Andreini has not been paid for any media work.
Johnson & Johnson wins FDA nod for new multiple myeloma therapy
Aug. 10, 2023 8:06 AM ET
By: Dulan Lokuwithana, SA News Editor1 Comment
- The Janssen Pharmaceutical unit of Johnson & Johnson (NYSE:JNJ) announced Thursday that the U.S. FDA granted accelerated approval for its bispecific antibody Talvey as a late-line option for adults with relapsed or refractory multiple myeloma.
- https://seekingalpha.com/news/4000875-johnson-johnson-wins-fda-nod-multiple-myeloma-therapy?mailingid=32355042&messageid=2900&serial=32355042.14041&utm_campaign=rta-stock-news&utm_content=link-1&utm_medium=email&utm_source=seeking_alpha&utm_term=32355042.14041
- Johnson & Johnson (JNJ)LGND
- https://www.jnj.com/
- https://www.janssen.com/
REQORSA® Immunogene Therapy (quratusugene ozeplasmid),
REQORSA® Immunogene Therapy (quratusugene ozeplasmid),
REQORSA® Immunogene Therapy (quratusugene ozeplasmid),
Genprex Granted FDA Orphan Drug Designation (ODD) for REQORSA® Immunogene Therapy for the Treatment of Small Cell Lung Cancer
August 10, 2023
ODD is in addition to Three FDA Fast Track Designations
Genprex expects to dose the first patient in the Acclaim-3 clinical trial in the fourth quarter of 2023
AUSTIN, Texas — (August 10, 2023) — Genprex, Inc. (“Genprex” or the “Company”) (NASDAQ: GNPX), a clinical-stage gene therapy company focused on developing life-changing therapies for patients with cancer and diabetes, today announced the United States Food and Drug Administration (FDA) has granted Orphan Drug Designation (ODD) to the Company’s lead drug candidate, REQORSA® Immunogene Therapy (quratusugene ozeplasmid), for the treatment of small cell lung cancer (SCLC).
In addition to ODD for the treatment of SCLC, in June 2023, the FDA granted Fast Track Designation (FTD) for REQORSA Immunogene Therapy, in combination with Genentech, Inc’s Tecentriq® in patients with extensive-stage small cell lung cancer (ES-SCLC) who did not develop tumor progression after receiving Tecentriq and chemotherapy as initial standard treatment. With ES-SCLC, the cancer has spread from one lung to the other, or to other parts of the body. Extensive-stage is the most common type of SCLC. FDA has also granted Genprex FTD for two other indications of REQORSA Immunogene Therapy, including REQORSA in combination with Tagrisso for non-small cell lung cancer (NSCLC) in patients who have progressed after Tagrisso treatment, and REQORSA in combination with Keytruda for NSCLC in patients who have progressed after Keytruda treatment.
“We are excited to receive Orphan Drug Designation from the FDA for REQORSA for patients with SCLC,” said Rodney Varner, President, Chairman and Chief Executive Officer at Genprex. “This FDA Orphan Drug Designation in combination with our recently received FDA Fast Track designation underscores the great need for better treatment options for patients with SCLC, ES-SCLC and NSCLC. We look forward to initiating the Acclaim-3 clinical trial expected in the fourth quarter of 2023 in order to bring hope of an effective new therapy to patients suffering with this life-limiting cancer.”
The FDA grants ODD status to investigational therapies being developed to treat, diagnose, or prevent a rare disease or condition affecting fewer than 200,000 people in the United States. Further, ODD provides benefits to drug developers, including assistance in the drug development process, tax credits for qualified trials, waiver of certain FDA fees, and potential for seven years of post-approval marketing exclusivity.
Genprex’s method of treating cancer is to reexpress tumor suppressor genes in cancers. Tumor suppressor genes are deleted or inactivated early in the process of cancer development. REQORSA contains a plasmid that expresses a tumor suppressor gene protein called TUSC2. Virtually 100% of small cell lung cancers have reduced or no TUSC2 protein expression, and 41% completely lack TUSC2 protein expression. Pre-clinical studies in mice suggest that re-expressing the TUSC2 protein may lead to clinical efficacy. ES-SCLC has a very poor prognosis, with a median progression free survival (PFS) of only 5.2 months. Importantly, median PFS for patients receiving Tecentriq as maintenance therapy is only 2.6 months from the start of maintenance treatment, so there is a great need for improvement in maintenance therapy.
About Acclaim-3 Clinical Trial
The Acclaim-3 clinical trial is a Phase 1/2 open-label, dose escalation and clinical response study of maintenance therapy evaluating REQORSA in combination with Tecentriq® in patients with ES-SCLC who did not develop tumor progression after receiving Tecentriq and chemotherapy as initial standard treatment.
Patients in the Acclaim-3 clinical trial will be enrolled after receiving initial treatment with 3-4 cycles of carboplatin, etoposide, and Tecentriq, and achieving complete response, partial response or stable disease. They will then receive treatment with REQORSA and Tecentriq as maintenance therapy every 21 days until disease progression.
The Phase 1 dose escalation portion of the Acclaim-3 clinical trial is expected to enroll up to 12 patients at 3-5 U.S. clinical sites to determine the Maximum Tolerated Dose (MTD). If no dose limiting toxicities occur during Phase 1, then the highest dose evaluated will be the Recommended Phase 2 Dose. The Phase 2 portion of the study will then enroll approximately 50 patients at 5-10 sites. Patients will be treated with REQORSA and Tecentriq until disease progression or unacceptable toxicity is experienced.
The primary endpoint of the Phase 2 portion of the trial is to determine the 18-week progression-free survival rate from the time of the start of maintenance therapy with REQORSA and Tecentriq in patients with ES-SCLC. Patients will also be followed for survival. A Phase 2 futility analysis will be performed after the 25th patient enrolled and treated reaches 18 weeks of follow up.
About Genprex, Inc.
Genprex is a clinical-stage gene therapy company focused on developing life-changing therapies for patients with cancer and diabetes. Genprex’s technologies are designed to administer disease-fighting genes to provide new therapies for large patient populations with cancer and diabetes who currently have limited treatment options. Genprex works with world-class institutions and collaborators to develop drug candidates to further its pipeline of gene therapies in order to provide novel treatment approaches. Genprex’s oncology program utilizes its proprietary, non-viral ONCOPREX® Nanoparticle Delivery System which encapsulates the gene-expressing plasmids using lipid nanoparticles. The resultant product is administered intravenously, where it is taken up by tumor cells that then express tumor suppressor proteins that were deficient in the tumor. The Company’s lead product candidate, REQORSA® (quaratusugene ozeplasmid), is being evaluated in three clinical trials as a treatment for non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Each of Genprex’s three lung cancer clinical programs have received a Fast Track Designation from the Food and Drug Administration (FDA), and its SCLC program has received an FDA Orphan Drug Designation. Genprex’s diabetes gene therapy approach is comprised of a novel infusion process that uses an adeno-associated virus (AAV) vector to deliver Pdx1 and MafA genes directly to the pancreas. In models of Type 1 diabetes, GPX-002 transforms alpha cells in the pancreas into functional beta-like cells, which can produce insulin but may be distinct enough from beta cells to evade the body’s immune system. In a similar approach, GPX-003 for Type 2 diabetes, where autoimmunity is not at play, is believed to rejuvenate and replenish exhausted beta cells.
Interested investors and shareholders are encouraged to sign up for press releases and industry updates by visiting the Company Website, registering for Email Alerts and by following Genprex on Twitter, Facebook and LinkedIn.
Genprex wins FDA orphan drug designation for lead asset
Aug. 10, 2023 8:30 AM ET
By: Dulan Lokuwithana, SA News Editor
- Gene therapy developer Genprex (NASDAQ:GNPX) announced Thursday that the U.S. FDA granted Orphan Drug Designation for its lead therapeutic candidate, Reqorsa Immunogene Therapy, as a treatment for small cell lung cancer (SCLC).
- With its orphan drug designation, the FDA aims to offer financial incentives such as tax credits for clinical trial costs and seven years of marketing exclusivity for treatments targeted at rare diseases and conditions.
- https://seekingalpha.com/news/4000900-genprex-stock-gains-fda-orphan-drug-tag-lead-asset
- Genprex, Inc. (GNPX)
- https://www.genprex.com/
- https://www.genprex.com/technology/reqorsa/
- https://www.genprex.com/clinical-trials/pipeline/
ZURZUVAE™ (zuranolone)
TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab)
TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab)
FDA Approves ZURZUVAE™ (zuranolone), the First and Only Oral Treatment Approved for Women with Postpartum Depression, and Issues a Complete Response Letter for Major Depressive Disorder
AUGUST 4, 2023 • NEWS RELEASE
Postpartum depression (PPD) approval based on results from two Phase 3 clinical trials; in the SKYLARK Study treatment with ZURZUVAE rapidly improved symptoms of PPD at Day 15 and as early as Day 3 with sustained effect to Day 45
Mental health conditions are the leading cause of maternal mortality1 with PPD among the most common complications during and after pregnancy2
CAMBRIDGE, Mass., Aug. 04, 2023 (GLOBE NEWSWIRE) -- Biogen Inc. (Nasdaq: BIIB) and Sage Therapeutics, Inc. (Nasdaq: SAGE) announced the U.S. Food and Drug Administration (FDA) approved ZURZUVAE™ (zuranolone) 50 mg for adults with postpartum depression (PPD). ZURZUVAE is the first and only oral, once-daily, 14-day treatment that can provide rapid improvements in depressive symptoms for women with PPD. ZURZUVAE is expected to launch and be commercially available in the fourth quarter of 2023 shortly following scheduling as a controlled substance by the U.S. Drug Enforcement Administration, which is anticipated to occur within 90 days.
Additionally, the FDA issued a Complete Response Letter (CRL) for the New Drug Application (NDA) for zuranolone in the treatment of adults with major depressive disorder (MDD). The CRL stated that the application did not provide substantial evidence of effectiveness to support the approval of zuranolone for the treatment of MDD and that an additional study or studies will be needed. Biogen and Sage are reviewing the feedback and evaluating next steps.
“The approval of ZURZUVAE to treat postpartum depression is a major milestone for the hundreds of thousands of women who experience this underdiagnosed and undertreated condition,” said Christopher A. Viehbacher, President and Chief Executive Officer at Biogen. “We appreciate the support of patients, patient advocates and researchers who helped to reach this milestone. We believe that ZURZUVAE will be an important option to treat PPD and we will thoroughly review the feedback from the FDA on the use of zuranolone in MDD to determine next steps.”
“Maternal mental health has been sidelined for far too long, but today’s approval of ZURZUVAE helps to change that. Women have been waiting for an oral medicine that can specifically and rapidly improve the symptoms of PPD and we are proud to be able to deliver that,” said Barry Greene, Chief Executive Officer at Sage Therapeutics. “In regard to the CRL for MDD, we are highly disappointed for patients, particularly amid the current mental health crisis and millions of people with MDD struggling to find symptom relief. We remain committed to our mission to deliver life-changing brain health medicines.”
The approval of ZURZUVAE to treat women with PPD is based on the NEST clinical development program, which included two studies in adult women with PPD (ROBIN and SKYLARK Studies). Both studies met their primary endpoint, a significant mean reduction from baseline in the 17-item Hamilton Rating Scale for Depression (HAMD-17) total score, a common measure of depression severity, at Day 15 as compared to placebo. In the SKYLARK Study evaluating ZURZUVAE 50 mg, all key secondary endpoints were met, with significant reduction in depressive symptoms seen as early as Day 3 and sustained through Day 45. ZURZUVAE was generally well-tolerated with a consistent safety profile across both studies. The most common side effects ≥ 5% and greater than placebo in patients treated with ZURZUVAE 50 mg were somnolence, dizziness, diarrhea, fatigue and urinary tract infection. The labeling includes a boxed warning that instructs healthcare providers to advise people that ZURZUVAE causes driving impairment due to central nervous system (CNS) depressant effects. People who take ZURZUVAE should not drive a motor vehicle or engage in other potentially hazardous activities that require complete mental alertness until at least 12 hours after ZURZUVAE administration for the duration of the 14-day treatment course. Patients may not be able to assess their own degree of impairment.
“Today marks a groundbreaking day for the treatment of PPD, as with ZURZUVAE we now have an oral treatment option that can provide rapid improvements in depressive symptoms in as early as three days for women with PPD,” said Dr. Kristina Deligiannidis, a principal investigator in the ZURZUVAE clinical development program and Professor, The Feinstein Institutes for Medical Research in Manhasset, New York. “As a perinatal psychiatrist, I see the devastating impact PPD has on mothers particularly on the important mother-infant bond and long-term child development. Once available, I believe ZURZUVAE will be a meaningful option for patients in need.”
According to the Centers for Disease Control and Prevention, mental health conditions are the leading cause of maternal mortality1 with PPD among the most common complications during and after pregnancy.2 In the U.S., it is estimated approximately 1 in 8 women experience symptoms of PPD.3 Approximately half of all PPD cases may go undiagnosed without appropriate screening.4,5 Research shows only 15.8% of women with PPD symptoms receive treatment.6 PPD symptoms may persist beyond the postpartum period and can lead to prolonged maternal morbidity.7-9 Symptoms of PPD can include depressed mood, loss of interest in activities, changes in sleep patterns and appetite, decreased energy, feelings of guilt or worthlessness, trouble concentrating and in some cases thoughts of suicide.9
“Today’s approval is welcome news for the estimated 500,000 women in the United States who report experiencing symptoms of this devastating and often misunderstood illness each year,” said Wendy N. Davis, Ph.D., PMH-C, Executive Director at Postpartum Support International. “Women with PPD desperately need prompt care and additional treatment options that can provide quick relief so they can be healthy and present during this momentous time in their lives.”
Indication and Important Safety Information for ZURZUVAE
What is ZURZUVAE?
ZURZUVAE is a prescription medicine used to treat adults with postpartum depression (PPD).
It is not known if ZURZUVAE is safe and effective in children.
Please see the Full Prescribing Information, including Boxed WARNING, and Medication Guide for ZURZUVAE.
About ZURZUVAE™ (zuranolone)
ZURZUVAE is a once-daily, oral, 14-day medicine for the treatment of adults with postpartum depression (PPD). ZURZUVAE is a neuroactive steroid (NAS) GABA-A receptor positive allosteric modulator (PAM). The GABA system is the major inhibitory signaling pathway of the brain and central nervous system and contributes to regulating brain function.
About Biogen
Founded in 1978, Biogen is a leading global biotechnology company that has pioneered multiple breakthrough innovations including a broad portfolio of medicines to treat multiple sclerosis, the first approved treatment for spinal muscular atrophy, and two co-developed treatments to address a defining pathology of Alzheimer’s disease. Biogen is advancing a pipeline of potential novel therapies across neurology, neuropsychiatry, specialized immunology and rare diseases and remains acutely focused on its purpose of serving humanity through science while advancing a healthier, more sustainable and equitable world.
We routinely post information that may be important to investors on our website at www.biogen.com. Follow us on social media - Twitter, LinkedIn, Facebook, YouTube.
About Sage Therapeutics
Sage Therapeutics is a biopharmaceutical company fearlessly leading the way to create a world with better brain health. Our mission is to pioneer solutions to deliver life-changing brain health medicines, so every person can thrive. For more information, please visit www.sagerx.com.
Sage, Biogen postpartum depression pill zuranolone wins FDA approval
Aug. 04, 2023 7:53 PM ET
Sage Therapeutics, Inc. (SAGE)BIIB
By: Jonathan Block, SA News Editor10 Comments
- The US FDA has approved Sage Therapeutics' (NASDAQ:SAGE) and Biogen' (BIIB) Zurzuvae (zuranolone), the first oral treatment for postpartum depression.
- https://seekingalpha.com/news/3997942-sage-biogen-postpartum-depression-pill-zuranolone-wins-fda-approval
- Sage Therapeutics, Inc. (SAGE)BIIB
- https://www.biogen.com/
- https://www.sagerx.com/
TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab)
TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab)
TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab)
Janssen Receives Positive CHMP Opinions for Novel Bispecific Antibodies TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab) for the Treatment of Patients with Relapsed and Refractory Multiple Myeloma
Talquetamab is the first therapy targeting GPRC5D to receive a positive CHMP Opinion
Teclistamab, the first BCMA-targeting bispecific antibody to be approved in Europe, receives positive CHMP Opinion for reduced, biweekly dosing schedule
BEERSE, Belgium, 21 July 2023 –
The Janssen Pharmaceutical Companies of Johnson & Johnson announced today that the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) has recommended conditional marketing authorisation (CMA) for TALVEY® (talquetamab) as monotherapy for the treatment of adult patients with relapsed and refractory multiple myeloma (RRMM) who have received at least three prior therapies, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 antibody and have demonstrated disease progression on the last therapy. Talquetamab is a subcutaneous bispecific antibody that binds G protein-coupled receptor class C group 5 member D (GPRC5D), a novel target on multiple myeloma cells, and CD3, on T-cells.1
The CHMP also recommended the approval of a Type II variation for teclistamab, providing a reduced, biweekly dosing schedule of 1.5mg/kg every other week in patients who have achieved a complete response or better for six months or longer. Teclistamab is the first bispecific antibody targeting B-cell maturation antigen (BCMA) on myeloma cells, and CD3 on T-cells to be licensed in Europe for the treatment of adult patients with RRMM who have had at least three prior therapies, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 antibody and have demonstrated disease progression on the last therapy.2
Despite recent advances, multiple myeloma remains a highly heterogenous and incurable disease that is unique to every patient.3 As the disease progresses and with each successive line of treatment, responses tend to decrease and patient outcomes become progressively worse.4 An unmet need remains for more therapeutic options with different modes of action, including for patients treated with prior bispecific or CAR-T cell therapies, to better address the unique characteristics of every patient’s individual needs through different cellular targets.3
“With talquetamab, a novel bispecific antibody targeting GPRC5D, we look to build on our legacy of innovation and bring forward a vital new treatment option for patients with relapsed and refractory multiple myeloma, who have a poor prognosis,” said Edmond Chan, MBChB M.D. (Res), Senior Director EMEA Therapeutic Area Lead Haematology, Janssen-Cilag Limited. “Today’s recommendation from the CHMP marks an exciting step for patients who continue to face the challenges of this difficult-to-treat blood cancer. We look forward to working with health authorities to bring talquetamab to patients in need across the region as soon as possible, while we continue our focus on enhancing a robust multiple myeloma portfolio of therapeutics and regimens.”
The CHMP recommendation for talquetamab is based on data from the Phase 1/2 MonumenTAL-1 study (Phase 1: NCT03399799; Phase 2: NCT04634552), evaluating the safety profile and efficacy of talquetamab in patients with RRMM. The latest data from the study were recently presented at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting (2-6 June, Chicago) and the 2023 European Hematology Association (EHA) Hybrid Congress (8-11 June, Frankfurt).
The CHMP recommendation for teclistamab is based on data from the Phase 1/2 MajesTEC-1 study (Phase 1: NCT03145181; Phase 2: NCT04557098), evaluating the safety profile and efficacy of teclistamab in patients with RRMM. Data from the study were recently presented at the 2023 ASCO Annual Meeting.
“Pending approval, this variation for teclistamab will be an important step forward for this first BCMA bispecific therapy, offering flexible, less frequent dosing depending on a patient’s response,” said Sen Zhuang, M.D., Ph.D., Vice President, Clinical Research and Development, Janssen Research & Development, LLC. “Today's positive recommendations for talquetamab and teclistamab, two novel bispecific antibodies discovered and developed at Janssen, reinforce our commitment to delivering innovative treatment options for patients with multiple myeloma.”
#ENDS#
About Talquetamab
Talquetamab is a bispecific T-cell engaging antibody that binds to CD3, on T-cells, and GPRC5D, a novel multiple myeloma target which is highly expressed on myeloma cells and hard keratinised tissues, with minimal to no expression detected on B-cells or B-cell precursors.1,5
Talquetamab, which is administered by subcutaneous injection, is currently being evaluated in several monotherapy and combination studies.6,7,8,9,10,11,12
CMA is the approval of a medicine that addresses unmet medical needs of patients based on less comprehensive data than normally required, where the available data suggest that the benefits of the medicine outweigh the risks, and the applicant can provide comprehensive clinical data in the future.13 Prior to the CHMP recommending this CMA, the EMA granted talquetamab PRIority Medicines (PRIME) designation in January 2021 and accelerated assessment in November 2022. The U.S. Food and Drug Administration (FDA) granted talquetamab Breakthrough Therapy Designation in June 2022. Janssen also received Orphan Drug Designation for talquetamab from the EMA in August 2021 and the FDA in May 2021.
About Teclistamab
Teclistamab is an off-the-shelf (or ready to use) bispecific antibody.2 Teclistamab, a subcutaneous injection, redirects T-cells through two cellular targets (BCMA and CD3) to activate the body’s immune system to fight the cancer. Teclistamab is currently being evaluated in several monotherapy and combination studies.14,15,16,17,18,19
Teclistamab received European Commission (EC) approval in August 2022. The application for CMA was reviewed by the CHMP under an accelerated timetable to enable faster patient access to this medicine.20 This was also supported through the EMA’s PRIME scheme, which provides early and enhanced scientific and regulatory support to medicines that have a particular potential to address patients’ unmet medical needs.21
For a full list of adverse events and information on dosage and administration, contraindications and other precautions when using teclistamab please refer to the Summary of Product Characteristics. In line with EMA regulations for new medicines and those given conditional approval, teclistamab is subject to additional monitoring.
About Multiple Myeloma
Multiple myeloma is an incurable blood cancer that affects a type of white blood cell called plasma cells, which are found in the bone marrow.3,22 In multiple myeloma, these malignant plasma cells change and grow out of control.22 In Europe, more than 50,900 people were diagnosed with multiple myeloma in 2020, and more than 32,400 patients died.23 While some patients with multiple myeloma initially have no symptoms, others can have common symptoms of the disease which can include bone fracture or pain, low red blood cell counts, tiredness, high calcium levels or kidney failure.24
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we’re creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com/emea. Follow us at www.linkedin.com/janssenEMEA for our latest news. Janssen Pharmaceutica NV, Janssen-Cilag Limited and Janssen Research & Development, LLC are part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
J&J gets expanded approval for cardiac ablation products
Aug. 04, 2023 11:42 AM ET
By: Val Brickates Kennedy, SA News Editor
Johnson & Johnson's (NYSE:JNJ) BioSense Webster unit said that it has received FDA approval for several of its cardiac ablation products for use in workflow without fluoroscopy.
J&J said the approval covers the Thermocool Smarttouch SF catheter, Carto Vizigo Bi-Directional Guiding Sheath, Pentaray Nav Eco High Density Mapping Catheter, Decanav Mapping Catheters and Webster CS Catheter. The devices are used for cardiac ablation procedures to treat atrial fibrillation, a common type of irregular heartbeat.
UGN-102
TALVEY®▼ (talquetamab) and TECVAYLI®▼ (teclistamab)
UGN-102
UGN-102, in Development as the Potential First Non-Surgical Therapy for LG-IR-NMIBC, Met Primary Endpoints in Both Phase 3 ATLAS and ENVISION Clinical Trials
July 27, 2023 at 9:50 AM EDT
-- In ATLAS, UGN-102 Demonstrated Superiority to TURBT with a 55% Reduction of Risk for Recurrence, Progression or Death in Patients who Received UGN-102 --
-- ENVISION Showed a Complete Response Rate of 79.2% at 3-Months --
-- Side Effect Profile in ATLAS and ENVISION Consistent with Previous Clinical Trials of UGN-102 --
-- UroGen Will Review ATLAS and ENVISION Top-line Data Today at 10:00 a.m. Eastern Time --
PRINCETON, N.J.--(BUSINESS WIRE)--Jul. 27, 2023-- UroGen Pharma Ltd. (Nasdaq: URGN), a biotech company dedicated to developing and commercializing novel solutions that treat urothelial and specialty cancers, today announced positive topline data from its Phase 3 trials ATLAS and ENVISION studying UGN-102 (mitomycin) for intravesical solution in patients with low-grade, intermediate-risk non-muscle invasive bladder cancer (LG-IR-NMIBC). Both ATLAS and ENVISION trials met their primary endpoints.
In the ATLAS trial, UGN-102 met its primary endpoint of disease-free survival, reducing risk of recurrence, progression, or death by 55%. UGN-102 also showed a 64.8% complete response rate at three months for patients who only received UGN-102, compared to a 63.6% complete response rate at three months for patients who only received a TURBT.
The ENVISION trial met its primary endpoint by demonstrating that patients treated with UGN-102 had a 79.2% rate of complete response at 3-months following the initial treatment. Additional data evaluating the secondary endpoint of duration of response from ENVISION, and the submission of a New Drug Application (NDA) (assuming additional positive findings) to the U.S. Food and Drug Administration (FDA) are anticipated in 2024.
“UGN-102 has demonstrated a robust and consistent therapeutic profile across multiple clinical trials, providing a compelling picture of its potential to be a transformational product and advance the standard of care away from repetitive surgery to a minimally invasive, non-surgical option for LG-IR-NMIBC,” says Liz Barrett, President and Chief Executive Officer of UroGen. “If approved, we anticipate UGN-102 to be a significant growth driver for UroGen as the first-ever non-surgical treatment option for a disease afflicting approximately 82,000 new patients in the U.S. each year. We are on track to deliver on our previously shared guidance for JELMYTO and now find ourselves on the precipice of a new era in bladder cancer care, and that is a very exciting place to be.”
In both trials, UGN-102, a sustained release, hydrogel-based formulation that is designed to enable longer exposure of bladder tissue to mitomycin, thereby enabling the treatment of tumors by non-surgical means, was generally well tolerated, with a side effect profile similar to that of previous clinical trials.
“While TURBT is the standard treatment for bladder cancer, the recurrent nature of LG-IR-NMIBC means that patients will undergo multiple surgeries that come with risks for this older patient population,” says Sandip Prasad, MD, M.Phil., Director of Genitourinary Surgical Oncology, Morristown Medical Center/Atlantic Health System, NJ. “Based on these compelling data, I am optimistic that UGN-102, if approved, may change the treatment paradigm for these patients who lack non-surgical options to manage the ongoing burden of this highly recurrent disease.”
The Phase 3 ATLAS clinical trial, the predecessor to ENVISION, evaluated the efficacy, durability, and safety of UGN-102 with or without TURBT vs. TURBT alone in 282 patients with LG-IR-NMIBC. ENVISION evaluated the efficacy and safety of UGN-102 as a primary chemoablative therapy in 240 patients with LG-IR-NMIBC.
UGN-102 ATLAS & ENVISION Top-line Data Review
The company is hosting a data event featuring a panel discussion with leading bladder cancer experts on Thursday, July 27, 2023 at 10:00 a.m. Eastern Time to discuss these findings and will highlight topline results from the Phase 3 ATLAS and ENVISION clinical trials.
Please register for the webinar under the Events & Presentations section of the Company’s Investor Relations site (https://investors.urogen.com/events-and-presentations).
Following the live webcast, a replay will be available on the Company's website (https://urogen.com).
About UGN-102
UGN-102 (mitomycin) for intravesical solution is an investigational drug formulation of mitomycin in Phase 3 development for the treatment of LG-IR-NMIBC. Utilizing UroGen’s proprietary RTGel® technology, a sustained release, hydrogel-based formulation, UGN-102 is designed to enable longer exposure of bladder tissue to mitomycin, thereby enabling the treatment of tumors by non-surgical means. UGN-102 is delivered to patients using a standard urinary catheter in an outpatient setting. Assuming positive findings from the ENVISION Phase 3 study, UroGen anticipates submitting a New Drug Application (NDA) for UGN-102 in 2024. If approved, UGN-102 would be the first non-surgical primary therapeutic to treat a subset of bladder cancer characterized by high recurrence rates and multiple surgeries.
About ENVISION
The Phase 3 ENVISION trial is a single-arm, multinational, multicenter study evaluating the efficacy and safety of UGN-102 (mitomycin) for intravesical solution as primary chemoablative therapy in patients with low-grade, intermediate-risk NMIBC. The Phase 3 ENVISION trial completed target enrollment with approximately 240 patients across 56 sites. Study participants received six once-weekly intravesical instillations of UGN-102. The primary endpoint evaluated the complete response rate at the 3-month assessment after the first instillation, and the key secondary endpoint will evaluate durability over time in patients who achieved a complete response at the three-month assessment. Based on discussions with the FDA, and assuming positive findings, UroGen anticipates submitting an NDA for UGN-102 in 2024. Learn more about the Phase 3 ENVISION trial at www.clinicaltrials.gov (NCT05243550)
About ATLAS
ATLAS is a global, open-label, randomized controlled Phase 3 trial designed to assess the efficacy and safety of UGN-102, with or without TURBT, vs. TURBT alone in patients diagnosed with LG-IR-NMIBC. The trial enrolled 282 patients in clinical sites in the U.S., Europe and Israel. Patients were randomized 1:1 to either UGN-102 or TURBT. Patients in the UGN-102 arm were treated with six weekly intravesical instillations of UGN-102. At the 3-month time point, patients were assessed for response. Patients who demonstrated a complete response to either UGN-102 or TURBT, were assessed for long-term follow-up for evidence of recurrence. Patients who demonstrated presence of persistent disease at 3-months, in either arm, underwent a TURBT and continued for long-term follow-up for evidence of recurrence. The primary endpoint of the study is disease-free survival. Learn more about the ATLAS trial at www.clinicaltrials.gov (NCT04688931)
About UroGen Pharma Ltd.
UroGen is a biotech company dedicated to developing and commercializing innovative solutions that treat urothelial and specialty cancers because patients deserve better options. UroGen has developed RTGel® reverse-thermal hydrogel, a proprietary sustained release, hydrogel-based platform technology that has the potential to improve therapeutic profiles of existing drugs. UroGen’s sustained release technology is designed to enable longer exposure of the urinary tract tissue to medications, making local therapy a potentially more effective treatment option. JELMYTO® (mitomycin) for pyelocalyceal solution and investigational treatment UGN-102 (mitomycin) for intravesical solution for patients with low-grade non-muscle invasive bladder cancer are designed to ablate tumors by non-surgical means. UroGen is headquartered in Princeton, NJ with operations in Israel. Visit www.urogen.com to learn more or follow us on Twitter, @UroGenPharma.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230727005666/en/
Source: UroGen Pharma Ltd.
UroGen says bladder cancer therapy met main goals in Phase 3 trials
Jul. 27, 2023 10:43 AM ET
By: Dulan Lokuwithana, SA News Editor2 Comments
UroGen Pharma (NASDAQ:URGN) announced Thursday that its lead product candidate, UGN-102, reached primary endpoints in two Phase 3 trials for patients with bladder cancer.
The ATLAS and ENVISION trials were designed to evaluate UGN-102 in over 500 patients with low-grade, intermediate-risk non-muscle invasive bladder cancer.
After a brief trading halt, UroGen (URGN) surged ~41% intraday following the announcement.
https://seekingalpha.com/news/3992173-urogen-stock-gains-bladder-cancer-trials-succeed
KB707
V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab)
UGN-102
Krystal Biotech Announces Pipeline Expansion into Oncology and FDA Acceptance of IND Application for Lead Oncology Candidate KB707
July 26, 2023
PITTSBURGH, July 26, 2023 (GLOBE NEWSWIRE) -- Krystal Biotech, Inc. (the “Company”) (NASDAQ: KRYS), a commercial-stage biotechnology company focused on the discovery, development and commercialization of genetic medicines to treat diseases with high unmet medical needs, announced today that it has expanded its R&D pipeline to oncology and that the US Food and Drug Administration (FDA) has accepted its Investigational New Drug (IND) application of its lead oncology drug candidate KB707 for the treatment of locally advanced or metastatic solid tumor malignancies. The Company will host an investor conference call and webcast, Thursday, July 27, 2023, at 8:00 am ET, to discuss the KB707 program. To join the investor conference call, please see the instructions below. The presentation for the investor conference call is attached to the Company’s Form 8-K.
“The KB707 program leverages our learnings and clinical experience in two tissue areas, the skin and the lung, and underscores the broader potential of our HSV-1 platform to deliver all types of exogenous genetic material and improve outcomes for patients with debilitating diseases,” said Krish S. Krishnan, Chairman and CEO of Krystal Biotech.
KB707 is a modified HSV-1 vector designed to deliver genes encoding both human IL-12 and IL-2 to the tumor microenvironment and promote systemic immune-mediated tumor clearance. Two formulations of KB707 are in development, a solution formulation for transcutaneous injection and an inhaled (nebulized) formulation for lung delivery.
“We believe KB707 is a unique and highly differentiated drug candidate with the potential to unlock the capabilities of cytokine-based immunotherapy,” said Suma Krishnan, President of Research & Development at Krystal Biotech. “By enabling localized and sustained cytokine expression within a treated tumor, KB707 has the potential to maximize therapeutic efficacy while avoiding the tolerability challenges of systemic cytokine treatments.”
The FDA has accepted the Company’s IND to evaluate intratumoral KB707 in patients with solid tumors accessible by transcutaneous injection, and the Company expects to initiate a Phase 1 study in the second half of 2023. The Company is planning to file an amendment to the KB707 IND in the second half of 2023 to evaluate inhaled KB707 in a clinical trial in the first half of 2024.
Interleukin-2 (IL-2) and interleukin-12 (IL-12) are secreted cytokines with complementary functions promoting cell-mediated immunity in humans. Both IL-2 and IL-12 have been shown to elicit anti-tumor immune responses in preclinical or clinical models and have been extensively studied for their potential in cancer immunotherapy. Despite promising signs of efficacy, it has proven difficult to effectively harness IL-2 and IL-12 for therapeutic benefit, as systemic administration is often poorly tolerated, and their inherently short half-lives necessitate high dose levels and extremely frequent dose intervals. KB707 leverages the Company’s modified HSV-1 vector – and its ability to efficiently deliver a durable DNA payload without active replication and minimal cytotoxicity – to drive local and sustained cytokine expression within the tumor microenvironment and maximize the therapeutic window and benefit of IL-2 and IL-12.
“There remains an urgent unmet need for new therapies in cutaneous oncology, including for patients that do not respond to current first-line options and for the many who eventually progress on available therapy,” said Jason Luke, MD, Associate Professor of Medicine in the Division of Hematology/Oncology and Director of the Cancer Immunotherapeutic Center within UPMC Hillman Cancer Center Immunology and Immunotherapy Program in Pittsburgh, PA. “As the lead investigator on multiple practice changing immunotherapy trials, I have seen first-hand the benefits that can be realized through effective immune modulation and am excited about the potential of Krystal's approach for localized, sustained cytokine delivery.”
In preclinical studies, KB707 has been shown to efficiently transduce mammalian cells in vitro leading to the secretion of bioactive IL-2 and IL-12 and can drive localized, durable cytokine expression in mouse skin after intradermal injection. Furthermore, in stringent checkpoint inhibitor refractory ‘cold’ syngeneic mouse models, HSV-1 vector based delivery of murine equivalent IL2 and IL12 elicited robust antitumor responses and survival benefits, including via intratumoral injection in single and dual flank B16F10 melanoma models, as well as via intratracheal delivery in a metastatic K7M2 osteosarcoma model, with evidence of protection from tumor rechallenge in both models suggestive of prolonged adaptive immunity.
The intratumoral KB707 Phase 1/Opal 1 study is an open-label, multi-center, monotherapy, dose escalation and expansion study, enrolling patients with locally advanced or metastatic solid tumors, who relapsed or are refractory to standard of care, with at least one measurable and injectable tumor accessible by transcutaneous route. The primary objective of the study is to evaluate safety and tolerability of KB707. Efficacy will also be assessed by multiple measures including overall response rate, progression free survival, and overall survival, and the immune effects of KB707 monotherapy will be assessed in tumor tissue, lymph nodes, and blood.
For those unable to listen to the live conference call, a replay will be available on the Investor’s section of the Company’s website at www.krystalbio.com.
About Krystal Biotech, Inc.
Krystal Biotech, Inc. (NASDAQ: KRYS) is a commercial-stage biotechnology company focused on the discovery, development and commercialization of genetic medicines to treat diseases with high unmet medical needs. VYJUVEKTM is the Company’s first commercial product, the first-ever redosable gene therapy, and the only medicine approved by the FDA for the treatment of dystrophic epidermolysis bullosa. The Company is rapidly advancing a robust preclinical and clinical pipeline of investigational genetic medicines in respiratory, oncology, dermatology, ophthalmology, and aesthetics. Krystal Biotech is headquartered in Pittsburgh, Pennsylvania. For more information, please visit http://www.krystalbio.com, and follow @KrystalBiotech on LinkedIn and Twitter.

![]()
Source: Krystal Biotech, Inc.
Krystal Biotech IND application for solid tumor candidate accepted by FDA
Jul. 26, 2023 6:10 PM ET
By: Jonathan Block, SA News Editor
- The US FDA has accepted an Investigational New Drug application submitted by Krystal Biotech (NASDAQ:KRYS) for its solid tumor malignancies candidate KB707.
- The company said the asset is a "modified HSV-1 vector designed to deliver genes encoding both human IL-12 and IL-2 to the tumor microenvironment and promote systemic immune-mediated tumor clearance."
- Krystal Biotech, Inc. (KRYS)
- https://seekingalpha.com/news/3991754-krystal-biotech-ind-application-solid-tumor-candidate-accepted-fda
- https://www.krystalbio.com/
V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab)
V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab)
V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab)
Merck and Moderna Initiate Phase 3 Study Evaluating V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab) for Adjuvant Treatment of Patients with Resected High-Risk(Stage IIB-IV) Melanoma
July 26, 2023 6:45 am ET
V940-001 is the first Phase 3 study of a planned comprehensive clinical development program being initiated following the positive primary analysis of the Phase 2b KEYNOTE-942/mRNA-4157-P201 trial reported at AACR and ASCO earlier this year
RAHWAY, N.J. & CAMBRIDGE, Mass.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, and Moderna, Inc. (Nasdaq: MRNA), a biotechnology company pioneering messenger RNA (mRNA) therapeutics and vaccines, today announced the initiation of the pivotal Phase 3 randomized V940-001 clinical trial evaluating V940 (mRNA-4157), an investigational individualized neoantigen therapy (INT), in combination with KEYTRUDA, Merck’s anti-PD-1 therapy, as an adjuvant treatment in patients with resected high-risk (Stage IIB-IV) melanoma. Global recruitment in V940-001 has begun, and the first patients are now enrolling in Australia.
“As we continue our efforts to advance novel treatment options for patients with high-risk Stage IIB-IV melanoma, the initiation of the V940-001 Phase 3 trial represents an important step forward in these efforts and our study of individualized neoantigen therapy,” said Dr. Marjorie Green, senior vice president and head of late-stage oncology, global clinical development, Merck Research Laboratories. “We look forward to continuing to collaborate with Moderna to evaluate this promising new approach with V940 (mRNA-4157), while also building on a standard of care laid by KEYTRUDA.”
“The initiation of the V940-001 Phase 3 trial is an exciting and important milestone for us as we work with our colleagues at Merck and the melanoma patient community to investigate how individualized neoantigen therapy may potentially transform the treatment of the most serious form of skin cancer,” said Kyle Holen, M.D., Moderna's Senior Vice President and Head of Development, Therapeutics and Oncology. “We thank the patients, investigators, and clinical trial sites across the world for helping us advance our efforts in this area.”
V940-001 is a Phase 3 global, randomized, double-blind, placebo- and active-comparator-controlled study designed to evaluate the safety and efficacy of V940 (mRNA-4157) in combination with KEYTRUDA in people with resected high-risk (Stage IIB-IV) melanoma compared to KEYTRUDA alone. The trial is slated to enroll approximately 1,089 patients at more than 165 sites in over 25 countries around the world. The primary endpoint of the study is recurrence-free survival (RFS), and secondary endpoints include distant metastasis-free survival (DMFS), overall survival (OS), and safety.
Based on data from the Phase 2b KEYNOTE-942/mRNA-4157-P201 study, the U.S. Food and Drug Administration and European Medicines Agency granted Breakthrough Therapy Designation and the Priority Medicines (PRIME) scheme, respectively, for V940 (mRNA-4157) in combination with KEYTRUDA for the adjuvant treatment of patients with high-risk melanoma. The companies presented the study’s primary endpoint, RFS, in April 2023 at the American Association for Cancer Research (AACR) Annual Meeting and presented the study’s key secondary endpoint, DMFS, in June 2023 at the American Society of Clinical Oncology (ASCO) Annual Meeting. The companies also plan to expand the development program to additional tumor types, including non-small cell lung cancer.
About V940 (mRNA-4157)
V940 (mRNA-4157) is a novel investigational messenger ribonucleic acid (mRNA)-based individualized neoantigen therapy (INT) consisting of a single synthetic mRNA coding for up to 34 neoantigens that is designed and produced based on the unique mutational signature of the DNA sequence of the patient’s tumor. Upon administration into the body, the algorithmically derived and RNA-encoded neoantigen sequences are endogenously translated and undergo natural cellular antigen processing and presentation, a key step in adaptive immunity.
Individualized neoantigen therapies are designed to train and activate the immune system so that a patient can generate an antitumor response specific to their tumor mutation signature. V940 (mRNA-4157) is designed to stimulate an immune response by generating specific T-cell responses based on the unique mutational signature of a patient’s tumor. KEYTRUDA is an immunotherapy that works by increasing the ability of the body’s immune system to help detect and fight tumor cells. Based on early clinical studies and data from the Phase 2b KEYNOTE-942/mRNA-4157-P201 trial, combining V940 (mRNA-4157) with KEYTRUDA may provide an additive benefit over KEYTRUDA alone.
About V940-001 ( NCT05933577 )
V940-001 is a global, randomized, double-blind, placebo- and active-comparator-controlled Phase 3 trial evaluating 1,089 patients with resected high-risk (Stage IIB-IV) melanoma. Following complete surgical resection, participants 18 years and older will be randomized 2:1 to receive V940 (mRNA-4157) (1 mg every three weeks for up to nine doses) and KEYTRUDA (400 mg every six weeks up to nine cycles [approximately one year]) versus KEYTRUDA alone for approximately one year until disease recurrence or unacceptable toxicity, or for a total treatment duration of up to approximately 56 weeks, whichever is sooner. The primary endpoint is RFS, defined as the time from randomization to any type of disease recurrence as assessed by the investigator, or death due to any cause. The secondary endpoints are DMFS, OS, safety and quality of life.
Key eligibility criteria for the trial include: patients who have surgically resected and histologically/pathologically confirmed diagnosis of Stage IIB or IIC, III or IV cutaneous melanoma, patients who have not received any prior systemic therapy for their melanoma beyond surgical resection and no more than 13 weeks have passed between final surgical resection.
For further information, please see: https://clinicaltrials.gov/study/NCT05933577
About melanoma
Melanoma, the most serious form of skin cancer, is characterized by the uncontrolled growth of pigment-producing cells. The rates of melanoma have been rising over the past few decades, with nearly 325,000 new cases diagnosed worldwide in 2020. In the U.S., skin cancer is one of the most common types of cancer diagnosed, and melanoma accounts for a large majority of skin cancer deaths. It is estimated there will be nearly 100,000 new cases of melanoma diagnosed and almost 8,000 deaths resulting from the disease in the U.S. in 2023.
About KEYTRUDA® (pembrolizumab) injection, 100 mg
KEYTRUDA is an anti-programmed death receptor-1 (PD-1) therapy that works by increasing the ability of the body’s immune system to help detect and fight tumor cells. KEYTRUDA is a humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD- L1 and PD-L2, thereby activating T lymphocytes which may affect both tumor cells and healthy cells.
Merck has the industry’s largest immuno-oncology clinical research program. There are currently more than 1,600 trials studying KEYTRUDA across a wide variety of cancers and treatment settings. The KEYTRUDA clinical program seeks to understand the role of KEYTRUDA across cancers and the factors that may predict a patient's likelihood of benefitting from treatment with KEYTRUDA, including exploring several different biomarkers.
Selected KEYTRUDA® (pembrolizumab) Indications in the U.S.
Melanoma
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic melanoma.
KEYTRUDA is indicated for the adjuvant treatment of adult and pediatric (12 years and older) patients with stage IIB, IIC, or III melanoma following complete resection.
Moderna, Merck begin phase 3 trial on mRNA melanoma combo treatment
Jul. 26, 2023 9:26 AM ET
By: Jonathan Block, SA News Editor5 Comments
- Moderna (NASDAQ:MRNA) and Merck (MRK) have begun a phase 3 trial testing a combination of the former's neoantigen therapy V940 (mRNA-4157) and the latter's Keytruda (pembrolizumab) for resected high-risk melanoma.
- https://seekingalpha.com/news/3991182-moderna-merck-begin-phase-3-trial-mrna-melanoma-combo-treatment
- https://www.merck.com/
- https://www.modernatx.com/
- Moderna, Inc. (MRNA)MRK
Axatilimab (SNDX-6352)
V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab)
V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab)
Syndax And Incyte Announce Positive Topline Results From The Pivotal AGAVE-201 Trial Of Axatilimab In Chronic Graft-Versus-Host Disease
July 24, 2023 at 7:00 AM EDT
– Trial met its primary endpoint across all cohorts with an overall response rate (ORR) of 74% at a dose of 0.3 mg/kg administered every two weeks –
– Data highlight durable response to treatment. At the 0.3 mg/kg dose, 60% of patients who responded to axatilimab were still responding at one year –
– Results continue to support axatilimab's promising safety and efficacy profile, and reinforce its potential as a first-in-class CSF-1R monoclonal antibody in chronic graft-versus-host disease (GVHD) –
– Syndax and Incyte intend to file a Biologics License Application (BLA) by year-end 2023; full dataset to be presented at a future medical meeting –
– Syndax to host conference call today at 8:30 a.m. ET –
WALTHAM, Mass. and WILMINGTON, Del., July 24, 2023 /PRNewswire/ -- Syndax Pharmaceuticals (Nasdaq: SNDX) and Incyte (Nasdaq: INCY) today announced positive topline data from the pivotal AGAVE-201 trial of axatilimab, an anti-CSF-1R antibody, in adult and pediatric patients with chronic graft-versus-host disease (GVHD) following two or more prior lines of therapy.
The trial achieved its primary endpoint across all cohorts, with patients treated with axatilimab at doses of 0.3 mg/kg every two weeks, 1.0 mg/kg every two weeks and 3.0 mg/kg every four weeks demonstrating overall response rates (ORR) within the first six months of treatment of 74%, 67% and 50%, respectively (95% Confidence Interval [CI]: [63,83], [55,77] and [39,61], respectively). Responses were achieved across key patient subgroups, including those with prior exposure to ruxolitinib, belumosudil and/or ibrutinib.
Based on these results, and pending agreement from the U.S. Food and Drug Administration (FDA), Syndax and Incyte intend to submit a Biologics License Application (BLA) to the FDA by year-end 2023.
"Today marks an important day not only for Syndax and Incyte, but, more importantly, for patients suffering from chronic GVHD," said Michael A. Metzger, Chief Executive Officer of Syndax. "Axatilimab is the first investigational chronic GVHD treatment to target inflammation and fibrosis through the inhibition of disease associated macrophages, and the AGAVE-201 data demonstrates the potentially pronounced impact this mechanism, alone or in combination with standard of care therapies already available for the management of this disease, may have on patients suffering from chronic GVHD. These results underscore our belief that axatilimab could provide a valuable and highly differentiated therapeutic option for this devastating disease. We look forward to working with our partners at Incyte as we move axatilimab towards regulatory filing. On behalf of the entire Syndax team, I would like to thank the patients, their caregivers and the investigators who made this trial possible."
"The results from the AGAVE-201 study are extremely compelling and underscore the potential benefits axatilimab may offer appropriate patients facing the serious complications associated with chronic GVHD," said Steven Stein, M.D., Chief Medical Officer of Incyte. "At Incyte, we remain committed to advancing our research and understanding of this complex disease and will work closely with Syndax and regulatory authorities to bring this innovative medicine to chronic GVHD patients."
The AGAVE-201 pivotal study enrolled a total of 241 patients across 121 sites in 16 countries. Patients enrolled in the trial had received a median of four prior systemic therapies with 74% having previously received ruxolitinib, 23% having previously received belumosudil and 31% having previously received ibrutinib. 54% of these patients had at least four organs involved at baseline including 45% with lung involvement.
Among responders treated with 0.3 mg/kg of axatilimab, 60% of patients maintained a response at 12 months (measured from first response to new systemic therapy or death, based on the Kaplan Meier estimate). The median duration of response in this population has not been reached. Additionally, in the 0.3 mg/kg group, 55% of patients experienced a clinically meaningful improvement in symptoms, as measured by at least a seven-point decrease in the modified Lee chronic GVHD Symptom Scale score.
The most common adverse events were consistent with the on-target effects of CSF-1R inhibition and with what was previously observed with axatilimab treatment. In the overall population, adverse events in greater than 20% of patients include an increase in aspartate aminotransferase, blood creatine phosphokinase, lipase, blood lactate dehydrogenase, alanine aminotransferase and fatigue (n=239). Serious adverse events in the overall population occurred in 101 (42.3%) patients, with 37 (15.5%) patients experiencing adverse events leading to discontinuation of study treatment. In the 0.3 mg/kg dose group (n=79), fatigue was the only serious adverse event that occurred in greater than 20% of patients. Serious adverse events in the 0.3 mg/kg group occurred in 30 (38%) patients, with five (6.3%) patients experiencing adverse events leading to discontinuation of study treatment.
"Chronic GVHD is a very common complication post allogeneic hematopoietic stem cell transplant that can have profound effects on patient medical burden and quality of life. More effective treatment options for this significant complication are desperately needed," said Carrie Kitko, M.D., Medical Director of the Pediatric Stem Cell Transplant Program at the Vanderbilt-Ingram Cancer Center. "I am highly encouraged by these data which demonstrate robust responses in a heavily pre-treated patient population. These findings further support that axatilimab has the potential to provide a clinically meaningful response for patients suffering from this morbid condition."
Conference Call and Webcast
Syndax will host a conference call and webcast to discuss the results of the Phase 2 AGAVE-201 trial today, July 24, 2023 at 8:30 a.m. ET.
The live webcast may be accessed through the Events & Presentations page in the Investors section of the Company's website. Alternatively, the conference call may be accessed through the following:
Conference ID: SNDXSPEC
Domestic Dial-in Number: 800-579-2543
International Dial-in Number: 785-424-1789
Live webcast: https://www.veracast.com/webcasts/syndax/events/specconf.cfm
For those unable to participate in the conference call or webcast, a replay will be available on the Investors section of the Company's website at www.syndax.com approximately 24 hours after the conference call and will be available for 90 days following the call.
About Chronic Graft-Versus-Host Disease
Chronic graft-versus-host disease (GVHD), an immune response of the donor-derived hematopoietic cells against recipient tissues, is a serious, potentially life-threatening complication of allogeneic hematopoietic stem cell transplantation which can last for years. Chronic GVHD is estimated to develop in approximately 40% of transplant recipients, and affects approximately 14,000 patients in the U.S.1,2. Chronic GVHD typically manifests across multiple organ systems, with skin and mucosa being commonly involved, and is characterized by the development of fibrotic tissue3.
About Axatilimab
Axatilimab is an investigational monoclonal antibody that targets colony stimulating factor-1 receptor, or CSF-1R, a cell surface protein thought to control the survival and function of monocytes and macrophages. In pre-clinical models, inhibition of signaling through the CSF-1 receptor has been shown to reduce the number of disease-mediating macrophages along with their monocyte precursors, which has been shown to play a key role in the fibrotic disease process underlying diseases such as chronic GVHD and IPF. Phase 1/2 data of Axatilimab in chronic GVHD demonstrating its broad activity and tolerability was last presented at the 63rd American Society of Hematology Annual Meeting and data was published in the Journal of Clinical Oncology. Axatilimab was granted Orphan Drug Designation by the U.S. Food and Drug Administration for the treatment of patients with chronic GVHD and IPF. In September 2021, Syndax and Incyte entered into an exclusive worldwide co-development and co-commercialization license agreement for axatilimab. Axatilimab is being developed under an exclusive worldwide license from UCB entered into between Syndax and UCB in 2016.
About AGAVE-201
The global Phase 2 AGAVE-201 dose-ranging trial evaluated the efficacy, safety, and tolerability of axatilimab in 241 adult and pediatric patients with recurrent or refractory active chronic GVHD whose disease had progressed after two prior therapies. Patients were randomized to one of three treatment groups that investigated a distinct dose of axatilimab administered at 0.3 mg/kg every two weeks, 1 mg/kg every two weeks or 3 mg/kg every four weeks. The trial's primary endpoint is the proportion of patients in each dose group who achieved an objective response as defined by 2014 NIH Consensus Criteria for chronic GVHD by cycle 7 day 1. Secondary endpoints include duration of response, percent reduction in daily steroids dose, organ specific response rates and validated quality-of-life assessments using the Modified Lee Symptom Scale.
For more information about AGAVE-201, visit https://clinicaltrials.gov/ct2/show/NCT04710576.
About Syndax Pharmaceuticals, Inc.
Syndax Pharmaceuticals is a clinical stage biopharmaceutical company developing an innovative pipeline of cancer therapies. Highlights of the Company's pipeline include revumenib, a highly selective inhibitor of the Menin–KMT2A binding interaction, and axatilimab, a monoclonal antibody that blocks the colony stimulating factor 1 (CSF-1) receptor. For more information, please visit www.syndax.com or follow the Company on Twitter and LinkedIn.
About Incyte
Incyte is a Wilmington, Delaware-based, global biopharmaceutical company focused on finding solutions for serious unmet medical needs through the discovery, development and commercialization of proprietary therapeutics. For additional information on Incyte, please visit Incyte.com and follow @Incyte.
SOURCE Syndax Pharmaceuticals, Inc.
Syndax and Incyte gain on mid-stage win for immune disorder therapy
Jul. 24, 2023 8:28 AM ET
Syndax Pharmaceuticals, Inc. (SNDX)INCY, JNJ, SNY
By: Dulan Lokuwithana, SA News Editor
- Syndax Pharmaceuticals (NASDAQ:SNDX) and Incyte (INCY) traded higher pre-market Monday after announcing that a mid-stage trial for their candidate for the immune-mediated disorder chronic graft-versus-host disease (GVHD), axatilimab, achieved its primary endpoint.
- https://seekingalpha.com/news/3990001-syndax-stock-incyte-stock-gain-on-mid-stage-win-gvhd
- Syndax Pharmaceuticals, Inc. (SNDX)INCY,
- https://syndax.com/
- https://syndax.com/pipeline/axatilimab/
biotecHOPE™ 2023
Zilebesiran (ALN-AGT)
Zilebesiran (ALN-AGT)
Zilebesiran (ALN-AGT)
Alnylam Announces Publication of Phase 1 Study Results for Zilebesiran in the New England Journal of Medicine
Jul 19, 2023
— Dose-Dependent Reductions in Serum Angiotensinogen and 24-hour Ambulatory Blood Pressure Were Sustained for Six Months After Single Doses of Zilebesiran —
— Acceptable Safety Profile Supporting Further Development —
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Jul. 19, 2023-- Alnylam Pharmaceuticals, Inc. (Nasdaq: ALNY), the leading RNAi therapeutics company, announced today that results from its Phase 1 study of zilebesiran, an investigational RNAi therapeutic targeting liver-expressed angiotensinogen (AGT) in development for the treatment of hypertension, were published in the New England Journal of Medicine (NEJM). The full manuscript is titled, “Zilebesiran, an RNA Interference Therapeutic Agent for Hypertension,” and will appear in the July 20, 2023 issue of NEJM. The key data reported in the publication showed that in the Phase 1 study, compared to placebo, zilebesiran was associated with dose-dependent reductions in serum AGT, achieving tonic blood pressure control with consistent and durable blood pressure reduction throughout a 24-hour period, sustained up to six months after single doses of ≥200 mg of zilebesiran. Zilebesiran also demonstrated an acceptable safety profile supporting continued clinical development; the most frequent treatment-related adverse events were mild, transient injection-site reactions.
“Hypertension is the leading cause of premature death, cardiovascular disease, and chronic kidney disease worldwide, and the global prevalence is steadily increasing in parallel with population aging and secular trends in the prevalence of risk factors including obesity, physical inactivity, and unhealthy diet. Despite the availability of effective antihypertensive treatments, nearly half of patients with hypertension fail to achieve guideline-recommended blood pressure targets, leaving them at residual risk for myocardial infarction, stroke, kidney disease progression, and mortality. For clinicians, the challenge in optimizing treatment of hypertension is frequently compounded by poor adherence to prescribed medical therapy and substantial variability in blood pressure between office visits and over the 24-hour cycle,” said Akshay Desai, M.D., the lead author of the manuscript and Director of the Cardiomyopathy and Heart Failure Program in the Advanced Heart Disease Section of the Cardiovascular Division at Brigham and Women’s Hospital. “In this context, the data we have published in NEJM are exciting, suggesting the potential role for zilebesiran to treat hypertension in a novel way via a novel, subcutaneously administered gene silencing approach to hypertension. This novel approach may provide durable, tonic blood pressure control with infrequent, office-based dosing and a favorable safety profile. Additional clinical trials will provide further insights into the potential of this approach to improve clinical outcomes in the growing population of patients with hypertension.”
“The data published in NEJM suggest the potential for zilebesiran to be an effective and highly-differentiated treatment that may help people with hypertension achieve sustained blood pressure control,” said Simon Fox, Ph.D., Vice President, Zilebesiran Program Lead at Alnylam. “To that end, we are currently evaluating the safety and efficacy of zilebesiran in our KARDIA Phase 2 clinical program either as a monotherapy (KARDIA-1) or in combination with a standard-of-care antihypertensive medication (KARDIA-2), and we look forward to reporting results from these programs in mid- and late 2023, respectively.”
Summary of Published Results
The study was conducted in 107* patients (zilebesiran, N=80; placebo, N=32) with mild-to-moderate hypertension. In Part A, patients were randomized 2:1 to receive single ascending subcutaneous doses of zilebesiran (10, 25, 50, 100, 200, 400, or 800 mg) or placebo. Part B of the study assessed the effects of zilebesiran (800 mg) on blood pressure under low- and high-salt diet conditions and Part E assessed the effects of zilebesiran (800 mg) coadministration with irbesartan (an angiotensin II receptor blocker). The study primary endpoint was the frequency of adverse events (AEs). AEs were reported for 58 patients receiving zilebesiran (72 percent) and 28 receiving placebo (88 percent). The most frequent treatment-related adverse events were mild, transient injection-site reactions reported in five (6 percent) patients who received zilebesiran. No events of hypotension, hyperkalemia, or worsening renal function requiring intervention were observed. Secondary and exploratory endpoints included change from baseline in serum AGT, pharmacokinetics, and change from baseline in blood pressure. In Part A, versus placebo, zilebesiran was associated with dose-dependent reductions in serum AGT that were sustained for up to six months. Single doses of zilebesiran (≥200 mg) resulted in reductions in systolic (>10 mm Hg) and diastolic (>5 mm Hg) blood pressure by Week 8, which were consistent throughout the diurnal cycle and sustained to six months. At the 800 mg dose, zilebesiran treatment resulted in mean (± standard error) systolic and diastolic reductions of 22.5 ± 5.1 mm Hg and 10.8 ± 2.7 mm Hg at Month 6, respectively. In Parts B and E of the study, blood pressure changes following zilebesiran treatment could be attenuated through high dietary salt intake and were augmented by irbesartan coadministration.
*Five patients receiving placebo in Part A of the study re-enrolled into Part E of the study and thus transitioned from placebo to zilebesiran.
About Zilebesiran
Zilebesiran is an investigational, subcutaneously administered RNAi therapeutic targeting angiotensinogen (AGT) in Phase 2 development for the treatment of hypertension in high unmet need populations. AGT is the most upstream precursor in the Renin-Angiotensin-Aldosterone System (RAAS), a cascade which has a demonstrated role in blood pressure (BP) regulation and its inhibition has well-established anti-hypertensive effects. Zilebesiran inhibits the synthesis of AGT in the liver, potentially leading to durable reductions in AGT protein and ultimately, in the vasoconstrictor angiotensin (Ang) II. Zilebesiran utilizes Alnylam's Enhanced Stabilization Chemistry Plus (ESC+) GalNAc-conjugate technology, which enables subcutaneous dosing with increased selectivity and a wide therapeutic index. The safety and efficacy of zilebesiran have not been established or evaluated by the FDA, EMA or any other health authority.
About RNAi
RNAi (RNA interference) is a natural cellular process of gene silencing that represents one of the most promising and rapidly advancing frontiers in biology and drug development today. Its discovery has been heralded as “a major scientific breakthrough that happens once every decade or so,” and was recognized with the award of the 2006 Nobel Prize for Physiology or Medicine. By harnessing the natural biological process of RNAi occurring in our cells, a new class of medicines known as RNAi therapeutics is now a reality. Small interfering RNA (siRNA), the molecules that mediate RNAi and comprise Alnylam's RNAi therapeutic platform, function upstream of today’s medicines by potently silencing messenger RNA (mRNA) – the genetic precursors – that encode for disease-causing or disease pathway proteins, thus preventing them from being made. This is a revolutionary approach with the potential to transform the care of patients with genetic and other diseases.
About Alnylam Pharmaceuticals
Alnylam Pharmaceuticals (Nasdaq: ALNY) has led the translation of RNA interference (RNAi) into a whole new class of innovative medicines with the potential to transform the lives of people afflicted with rare and prevalent diseases with unmet need. Based on Nobel Prize-winning science, RNAi therapeutics represent a powerful, clinically validated approach yielding transformative medicines. Since its founding in 2002, Alnylam has led the RNAi Revolution and continues to deliver on a bold vision to turn scientific possibility into reality. Alnylam’s commercial RNAi therapeutic products are ONPATTRO® (patisiran), AMVUTTRA® (vutrisiran), GIVLAARI® (givosiran), OXLUMO® (lumasiran), and Leqvio® (inclisiran), which is being developed and commercialized by Alnylam’s partner, Novartis. Alnylam has a deep pipeline of investigational medicines, including multiple product candidates that are in late-stage development. Alnylam is executing on its “Alnylam P5x25” strategy to deliver transformative medicines in both rare and common diseases benefiting patients around the world through sustainable innovation and exceptional financial performance, resulting in a leading biotech profile. Alnylam is headquartered in Cambridge, MA. For more information about our people, science and pipeline, please visit www.alnylam.com and engage with us on Twitter at @Alnylam, on LinkedIn, on Instagram, or on Facebook at @AlnylamPharma.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230719155322/en/
Alnylam Pharmaceuticals, Inc.
Source: Alnylam Pharmaceuticals, Inc.
Alnylam touts phase 1 results of RNAi hypertension asset zilebesiran
Jul. 19, 2023 5:56 PM ET
Alnylam Pharmaceuticals, Inc. (ALNY)
By: Jonathan Block, SA News Editor1 Comment
- Alnylam Pharmaceuticals (NASDAQ:ALNY) said that phase 1 data on its RNAi candidate for hypertension, zilebesiran, show it led to dose-dependent reductions in serum liver-expressed anhttps://seekingalpha.com/news/3988994-alnylam-touts-phase-1-results-rnai-hypertension-asset-zilebesirangiotensinogen ("AGT").
- Alnylam Pharmaceuticals, Inc. (ALNY)
- https://www.alnylam.com/
- https://www.alnylam.com/sites/default/files/pdfs/ALN-AGT-Fact-Sheet.pdf
XPOVIO® (selinexor)
Zilebesiran (ALN-AGT)
Zilebesiran (ALN-AGT)
Karyopharm Receives FDA Fast Track Designation for Selinexor for the Treatment of Myelofibrosis
– Regulatory Designation Includes Primary Myelofibrosis, Post-Essential Thrombocythemia Myelofibrosis and Post-Polycythemia Vera Myelofibrosis –
– Pivotal Phase 3 Study of Selinexor and Ruxolitinib in Treatment-Naïve Myelofibrosis Initiated in June 2023 –
NEWTON, Mass., July 17, 2023 /PRNewswire/ -- Karyopharm Therapeutics Inc. (Nasdaq: KPTI), a commercial-stage pharmaceutical company pioneering novel cancer therapies, today announced that the United States Food and Drug Administration (FDA) has granted Fast Track Designation to the development program of selinexor for the treatment of patients with myelofibrosis, including primary myelofibrosis, post-essential thrombocythemia myelofibrosis, and post-polycythemia vera myelofibrosis.
"Fast Track Designation for selinexor highlights its potential to address the unmet medical need in myelofibrosis, an important acknowledgement as we continue our pivotal Phase 3 study," said Reshma Rangwala, MD, PhD, Chief Medical Officer of Karyopharm. "Selinexor's unique mechanism of action, XPO1 inhibition, is a novel and potentially fundamental mechanism in myelofibrosis. We have been highly encouraged by the efficacy and safety data observed to date [in our Phase 1 study] with selinexor in combination with ruxolitinib in patients with treatment-naïve myelofibrosis and believe selinexor has the potential to shift the treatment paradigm. We look forward to continued interaction with the FDA as we advance the development of this promising treatment for patients in need."
In June 2023, Karyopharm initiated a pivotal Phase 3 clinical trial (XPORT-MF-034) (NCT04562389) to assess the efficacy and safety of once-weekly selinexor 60 mg in combination with ruxolitinib in JAKi-naïve patients with myelofibrosis. Updated data from the Phase 1 study were presented at the American Association for Cancer Research Annual Meeting 2023, American Society of Clinical Oncology 2023 and European Hematology Association 2023, which showed rapid, deep and sustained spleen responses and robust symptom improvement in patients treated with selinexor 60 mg in combination with ruxolitinib as of the April 10, 2023 cut-off date. Top-line data from the Phase 3 study is expected in 2025. The Company plans to expand its clinical development program in myelofibrosis by investigating selinexor in other JAKi-naïve settings, such as novel combinations, to benefit the greatest number of patients.
Fast Track Designation is intended to facilitate development and expedite review of drugs to treat serious and life-threatening conditions so that an approved product can reach the market expeditiously. Features of Fast Track Designation include frequent interactions with the FDA review team, and if relevant criteria are met, eligibility for Priority Review and Rolling Review.
Further information about the Phase 3 study can be found at www.clinicaltrials.gov.
About Karyopharm Therapeutics
Karyopharm Therapeutics Inc. (Nasdaq: KPTI) is a commercial-stage pharmaceutical company pioneering novel cancer therapies. Since its founding, Karyopharm has been an industry leader in oral Selective Inhibitor of Nuclear Export (SINE) compound technology, which was developed to address a fundamental mechanism of oncogenesis: nuclear export dysregulation. Karyopharm's lead SINE compound and first-in-class, oral exportin 1 (XPO1) inhibitor, XPOVIO® (selinexor), is approved in the U.S. and marketed by the Company in three oncology indications and has received regulatory approvals in various indications in a growing number of ex-U.S. territories and countries, including Europe and the United Kingdom (as NEXPOVIO®) and China. Karyopharm has a focused pipeline targeting multiple high unmet need cancer indications, including in multiple myeloma, endometrial cancer, myelodysplastic neoplasms and myelofibrosis. For more information about our people, science and pipeline, please visit www.karyopharm.com, and follow us on Twitter at @Karyopharm and LinkedIn.
XPOVIO® and NEXPOVIO® are registered trademarks of Karyopharm Therapeutics Inc. Any other trademarks referred to in this release are the property of their respective owners.
SOURCE Karyopharm Therapeutics Inc.
Karyopharm granted Fast Track designation for selinexor for myelofibrosis
Jul. 17, 2023 5:13 PM ET
Karyopharm Therapeutics Inc. (KPTI)INCY
By: Jonathan Block, SA News Editor1 Comment
- The US FDA has awarded Fast Track designation to Karyopharm Therapeutics (NASDAQ:KPTI) selinexor for myelofibrosis.
- https://seekingalpha.com/news/3988199-karyopharm-granted-fast-track-designation-selinexor-myelofibrosis
- Karyopharm Therapeutics Inc. (KPTI)
- https://www.xpovio.com/
- https://www.karyopharm.com/
Donanemab
Zilebesiran (ALN-AGT)
Beyfortus™ (nirsevimab-alip)
Results from Lilly's Landmark Phase 3 Trial of Donanemab Presented at Alzheimer's Association Conference and Published in JAMA
July 17, 2023
Donanemab significantly slowed cognitive and functional decline for amyloid-positive early symptomatic Alzheimer's disease patients, lowering their risk of disease progression; nearly half of participants at earlier stage of disease on donanemab had no clinical progression at 1 year
Additional subpopulation analyses presented live showed that those study participants at earliest stage of disease had even greater benefit, with 60% slowing of decline compared to placebo
Furthermore, treatment effect continued to increase relative to placebo over the course of the trial, even though many participants completed their course of therapy at 6 or 12 months, supporting limited duration dosing
FDA submission completed in Q2; regulatory action expected by end of year
INDIANAPOLIS, July 17, 2023 /PRNewswire/ -- Eli Lilly and Company (NYSE: LLY) presented full results from the Phase 3 TRAILBLAZER-ALZ 2 study showing that donanemab significantly slowed cognitive and functional decline in people with early symptomatic Alzheimer's disease (AD). The data were shared at the 2023 Alzheimer's Association International Conference (AAIC) as a featured symposium and simultaneously published in the Journal of the American Medical Association (JAMA).
"The positive TRAILBLAZER-ALZ 2 data bring hope to people with Alzheimer's disease who urgently need new treatment options. This is the first Phase 3 study of a disease-modifying therapy to replicate the positive clinical results observed in a previous study," said Anne White, executive vice president of Eli Lilly and Company and president of Lilly Neuroscience. "If approved, we believe donanemab can provide clinically meaningful benefits for people with this disease and the possibility of completing their course of treatment as early as 6 months once their amyloid plaque is cleared. We must continue to remove any barriers in access to amyloid-targeting therapies and diagnostics in an already complex healthcare ecosystem for Alzheimer's disease."
Lilly previously announced that donanemab met the primary and all cognitive and functional secondary endpoints in the Phase 3 study. Submission to the U.S. FDA for traditional approval was completed last quarter with regulatory action expected by the end of the year. Submissions to other global regulators are currently underway, and the majority will be completed by year end.
The TRAILBLAZER-ALZ 2 results support Lilly's application for regulatory approval to treat people with amyloid-positive early symptomatic Alzheimer's disease (either mild cognitive impairment or mild dementia), regardless of their baseline level of tau. TRAILBLAZER-ALZ 2 enrolled participants with a broader range of cognitive scores and amyloid levels than other recent trials of amyloid plaque-targeting therapies. Participants in TRAILBLAZER-ALZ 2 were stratified by their level of tau, a predictive biomarker for disease progression, into either a low-medium tau group (sometimes referred to as intermediate tau) or a high tau group, which represented a later pathological stage of disease progression. All participants were then assessed over 18 months using scales that measure both cognition and function, including the integrated Alzheimer's Disease Rating Scale (iADRS) and the Clinical Dementia Rating-Sum of Boxes (CDR-SB).
As previously reported, among participants with low-medium levels of tau (n=1182), donanemab treatment significantly slowed decline by 35% on iADRS and 36% on CDR-SB. Among all amyloid-positive early symptomatic AD study participants (n=1736), treatment with donanemab significantly slowed decline by 22% on iADRS and 29% on CDR-SB. Additional data presented at AAIC reinforced that regardless of baseline clinical or pathological stage of disease, treatment with donanemab resulted in cognitive and functional benefits relative to placebo:
- A pre-specified subpopulation analysis of low-medium tau participants based on clinical stage showed greater benefit of donanemab in those at earlier stage of disease:
- In participants with mild cognitive impairment (n=214), donanemab slowed decline by 60% on iADRS and 46% on CDR-SB (for those with mild dementia due to AD, n=534, donanemab slowed decline by 30% on iADRS and 38% on CDR-SB, respectively).
- Similarly, a post-hoc subgroup analysis of low-medium tau participants based on age showed greater benefit of donanemab in patients under the age of 75:
- In participants under the age of 75 (n=542), donanemab slowed decline by 48% on iADRS and 45% on CDR-SB.
- In participants aged 75 or greater (n=551), donanemab slowed decline by 25% on iADRS and 29% on CDR-SB.
- Results were similar across other subgroups, including participants who carried or did not carry an ApoE4 allele.
- The overall treatment effect of donanemab continued to grow throughout the trial, with the largest differences versus placebo seen at 18 months.
"These results demonstrate that diagnosing and treating people earlier in the course of Alzheimer's disease may lead to greater clinical benefit," said Liana Apostolova, M.D., distinguished professor in Alzheimer's Disease research and professor in neurology, radiology, medical and molecular genetics at Indiana University School of Medicine, where she is associate dean for Alzheimer's disease research and directs the clinical core of the Alzheimer's Disease Center. "The delay of disease progression over the course of the trial is significant and will give people more time to do such things that are meaningful to them."
Donanemab specifically targets deposited amyloid plaque and has been shown to lead to plaque clearance in treated patients. Treatment with donanemab significantly reduced amyloid plaque levels regardless of baseline pathological stage of disease. Among all participants, treatment with donanemab reduced amyloid plaque on average by 84% at 18 months, compared with a 1% decrease for participants on placebo. Participants were able to stop taking donanemab once they achieved pre-defined criteria of amyloid plaque clearance.* Approximately half of participants met this threshold at 12 months and approximately seven of every ten participants reached it at 18 months.
In the earlier pathological stage of disease in participants with low-medium tau, treatment with donanemab resulted in 47% of participants with no progression at one year on the CDR-SB assessment, versus 29% on placebo. Those participants treated with donanemab also had a 39% lower risk of progressing to the next clinical stage of disease over the 18-month trial. This delay in progression meant that, on average, participants treated with donanemab had an additional 7.5 months before they reached the same level of cognitive and functional decline on CDR-SB compared to those on placebo.
"People living with early, symptomatic Alzheimer's disease are still working, enjoying trips, sharing quality time with family – they want to feel like themselves, for longer," said Mark Mintun, M.D., group vice president Neuroscience Research & Development at Lilly, and president of Avid Radiopharmaceuticals. "The results of this study reinforce the importance of diagnosing and treating disease sooner than we do today."
The incidence of amyloid-related imaging abnormalities (ARIA) and infusion-related reactions was consistent with the previous TRAILBLAZER-ALZ study. ARIA occurs across the class of amyloid plaque clearing antibody therapies. It is most commonly observed as temporary swelling in an area or areas of the brain (ARIA-E) or as microhemorrhages or superficial siderosis (ARIA-H), in either case detected by MRI, and these may be serious and even fatal in some cases. This risk should be managed with careful observation, monitoring with MRIs, and appropriate actions if ARIA is detected. Serious infusion-related reactions and anaphylaxis were also observed.
For full TRAILBLAZER-ALZ 2 results, see the publication in JAMA.
A live webcast of the scientific session at AAIC featuring the donanemab presentations can be viewed on the investor section of Lilly's web site.
Lilly will host an investor call on Monday, July 17, at 1:30 p.m. EDT (10:30 a.m. PDT) to discuss the company's presentations at the Alzheimer's Association International Conference.
About TRAILBLAZER-ALZ 2 Study and the TRAILBLAZER-ALZ program
TRAILBLAZER-ALZ 2 (NCT04437511) is a Phase 3, double-blind, placebo-controlled study to evaluate the safety and efficacy of donanemab in participants ages 60-85 years with early symptomatic Alzheimer's disease (MCI or mild dementia due to Alzheimer's disease) with the presence of confirmed Alzheimer's disease neuropathology. The trial enrolled 1736 participants, across 8 countries, selected based on cognitive assessments in conjunction with amyloid plaque imaging and tau staging by PET imaging.
Lilly previously announced and published in the New England Journal of Medicine (NEJM) results from the Phase 2 TRAILBLAZER-ALZ study in 2021. In addition, Lilly shared data from TRAILBLAZER-ALZ 4, the first active comparator study in early symptomatic Alzheimer's disease, at the 15th Clinical Trials on Alzheimer's Disease (CTAD) conference in 2022.
Lilly continues to study donanemab in multiple clinical trials, including TRAILBLAZER-ALZ 3, which is focused on preventing symptomatic Alzheimer's disease in participants with preclinical AD; TRAILBLAZER-ALZ 5, a registration trial for early symptomatic Alzheimer's disease currently enrolling in China; and TRAILBLAZER-ALZ 6, which is focused on expanding our understanding of ARIA through novel MRI sequences, blood-based biomarkers, and different dosing regimens of donanemab.
About Lilly
Lilly unites caring with discovery to create medicines that make life better for people around the world. We've been pioneering life-changing discoveries for nearly 150 years, and today our medicines help more than 51 million people across the globe. Harnessing the power of biotechnology, chemistry and genetic medicine, our scientists are urgently advancing new discoveries to solve some of the world's most significant health challenges, redefining diabetes care, treating obesity and curtailing its most devastating long-term effects, advancing the fight against Alzheimer's disease, providing solutions to some of the most debilitating immune system disorders, and transforming the most difficult-to-treat cancers into manageable diseases. With each step toward a healthier world, we're motivated by one thing: making life better for millions more people. That includes delivering innovative clinical trials that reflect the diversity of our world and working to ensure our medicines are accessible and affordable. To learn more, visit Lilly.com and Lilly.com/newsroom or follow us on Facebook, Instagram, Twitter and LinkedIn. P-LLY
* Participants completed their course of treatment with donanemab once they reached a pre-defined level of plaque clearance. Average baseline amyloid levels were ~100 Centiloids for participants with early symptomatic Alzheimer's disease.

View original content to download multimedia:https://www.prnewswire.com/news-releases/results-from-lillys-landmark-phase-3-trial-of-donanemab-presented-at-alzheimers-association-conference-and-published-in-jama-301878537.html
SOURCE Eli Lilly and Company
Eli Lilly full phase 3 data confirms benefit of Alzheimer's asset donanemab
Jul. 17, 2023 1:21 PM ET
Eli Lilly and Company (LLY)BIIB, ESALF, ESAIY
By: Jonathan Block, SA News Editor
Complete phase 3 data released on Eli Lilly's (NYSE:LLY) donanemab confirmed that the Alzheimer's biologic was effective in slowing cognitive decline in early stages of the disease compared to placebo.
LLY Dividend History
https://www.nasdaq.com/market-activity/stocks/lly/dividend-history
Beyfortus™ (nirsevimab-alip)
Beyfortus™ (nirsevimab-alip)
Beyfortus™ (nirsevimab-alip)
Beyfortus approved in the US for the prevention of RSV lower respiratory tract disease in infants
PUBLISHED17 July 2023
First preventive option specifically designed to protect the broad infant population through its first RSV season
Across all clinical endpoints, a single dose of Beyfortus delivered consistent and sustained efficacy against RSV disease vs placebo
AstraZeneca and Sanofi’s Beyfortus (nirsevimab) has been approved in the US for the prevention of respiratory syncytial virus (RSV) lower respiratory tract disease (LRTD) in newborns and infants born during or entering their first RSV season, and for children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season. Beyfortus will be available in the US ahead of the upcoming 2023-2024 RSV season.
The approval by the Food and Drug Administration (FDA) follows the unanimous vote by the Antimicrobial Drugs Advisory Committee (AMDAC) on the favourable benefit-risk profile of Beyfortus, and was based on the extensive clinical development programme for Beyfortus spanning three pivotal late-stage clinical trials. Across all clinical endpoints, a single dose of Beyfortus demonstrated consistent efficacy against RSV LRTD extending through five months, the duration of a typical RSV season.1-4
Beyfortus is the first preventive option approved to protect a broad infant population, including those born healthy at term, or preterm, or with specific health conditions that make them vulnerable to severe RSV disease. The single dose can be flexibly administered at the beginning of the RSV season or at birth for those born during the RSV season.
Iskra Reic, Executive Vice President, Vaccines and Immune Therapies, AstraZeneca, said: “Beyfortus represents an opportunity for a paradigm-shift in preventing serious respiratory disease due to RSV across a broad infant population in the US. The science that Beyfortus is built on demonstrates AstraZeneca’s continued leadership in addressing the needs of the most vulnerable populations and reducing the burden on healthcare systems.”
Thomas Triomphe, Executive Vice President, Vaccines, Sanofi, said: “Today’s approval marks an unprecedented moment for protecting infant health in the U.S., following an RSV season that took a record toll on infants, their families, and the U.S. healthcare system. Beyfortus is the only monoclonal antibody approved for passive immunisation to provide safe and effective protection for all infants during their first RSV season. I am proud that, by prioritising this potential game-changer, we are now about to bring Beyfortus to American families.”
RSV is the leading cause of hospitalisation for infants under the age of one in the US, averaging 16 times higher than the annual rate for influenza.5,6 Each year, an estimated 590,000 RSV disease cases in infants under one require medical care, including physician office, urgent care, emergency room visits and hospitalisations.7
Beyfortus was generally well tolerated with a favourable safety profile that was consistent across all clinical trials. The overall rates of adverse events were comparable between Beyfortus and placebo and the majority of adverse events were mild or moderate in severity. The most common adverse events were rash and injection site reactions.1-4
Beyfortus was approved in the European Union in October 2022 for the prevention of RSV LRTD in newborns and infants during their first RSV season. Regulatory applications are also currently under review in China, Japan and several other countries.
Notes
RSV
RSV is a very contagious virus that can lead to serious respiratory illness for infants, according to the Centers for Disease Control and Prevention (CDC). RSV symptoms can include runny nose, coughing, sneezing, fever, decrease in appetite, and wheezing.8 Two out of three infants are infected with RSV during their first year of life and almost all infants are infected by their second birthday.8,9 In the US, RSV is the leading cause of hospitalisation in infants under 12 months, averaging 16 times higher than the annual rate for influenza.5,6 Approximately 75% of infants hospitalised for RSV were born at term with no underlying conditions in a study conducted from 2014-2015.10 Each year in the US, an estimated 590,000 RSV disease cases in infants under one require medical care, including physician office, urgent care, emergency room visits and hospitalisations.7
Beyfortus
Beyfortus (nirsevimab) is a single dose long-acting antibody, developed and commercialised in partnership by AstraZeneca and Sanofi using AstraZeneca’s YTE technology. It is designed to protect infants born during or entering their first RSV season and for children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season. Beyfortus, provided directly to newborns and infants as a single dose, offers rapid protection via an antibody to help prevent LRTD caused by RSV, without requiring activation of the immune system. Beyfortus administration can be timed to the start of the RSV season.11
Beyfortus has been granted regulatory designations to facilitate expedited development by several major regulatory agencies around the world. These include Breakthrough Therapy Designation and Priority Review Designation by the China Center for Drug Evaluation under the National Medical Products Administration; Breakthrough Therapy Designation from the US Food and Drug Administration; access granted to the European Medicines Agency (EMA PRIority MEdicines (PRIME) scheme; and named “a medicine for prioritized development” under the Project for Drug Selection to Promote New Drug Development in Pediatrics by the Japan Agency for Medical Research and Development (AMED).
Pivotal clinical trials
The Phase IIb (Trial 03) study was a randomised, placebo-controlled trial designed to measure the efficacy of Beyfortus against medically attended (MA) Lower Respiratory Tract Infection (LRTI) through 150 days post-dose. Healthy preterm infants of 29 to less than 35 weeks’ gestational age were randomised (2:1) to receive a single 50mg intramuscular injection of Beyfortus or placebo regardless of weight.3,12
The Beyfortus dosing regimen was determined based on further exploration of the Phase IIb data and was used in subsequent trials as a single 50 mg dose for those who weigh less than 5 kg, or a single 100 mg dose for those who weigh 5 kg or greater.3,12
The MELODY Phase III study (Trial 04) was a randomised, double-blind, placebo- controlled trial conducted across 21 countries designed to determine efficacy of Beyfortus against medically attended LRTI due to through 150 days after dosing, versus placebo, in healthy term and late preterm infants (35 weeks gestational age or greater) entering their first RSV season.1,2,12
MEDLEY (Trial 05) was a Phase II/III, randomised, double-blind, Synagis-controlled trial with the primary objective of assessing safety and tolerability for Beyfortus in preterm infants of less than 35 weeks gestational age and infants with congenital heart disease (CHD) and/or chronic lung disease of prematurity (CLD) eligible to receive Synagis.4,12 Between July 2019 and May 2021 a total of 925 infants entering their first RSV season were randomised to receive Beyfortus or Synagis. Safety was assessed by monitoring the occurrence of adverse events through 360 days post-dose. Serum levels of Beyfortus following dosing (on day 151) in this trial were comparable with those observed in the MELODY Phase III trial, indicating similar protection in this population to that in the healthy term and late preterm infants is likely. Data were published in the New England Journal of Medicine (NEJM) in March 2022.4,12
The safety profile of Beyfortus was similar to Synagis in the MEDLEY Phase II/III trial and consistent with the safety profile in healthy term and preterm infants studied in the MELODY and Phase IIb trials. While uncommon, the most reported adverse reactions were: rash 14 days post-dose, (the majority of which were mild to moderate; non-serious injection site reactions within 7 days post-dose.1,2,4,12
The results of MELODY, MEDLEY Phase II/III and the Phase IIb trials demonstrate that a single dose of nirsevimab helps protect infants during their first RSV season against RSV disease. This broad infant population includes healthy term, late preterm and preterm infants, as well as infants with specific health conditions that make them vulnerable to severe RSV disease.1-4,12
These trials formed the basis of regulatory submissions which began in 2022.
Results from the MELODY Phase III trial (Trial 04)
The primary endpoint of the MELODY Phase III trial was met, reducing the incidence of medically attended LRTI, such as bronchiolitis or pneumonia, caused by RSV by 74.9% (95% CI 50.6, 87.3; P<0.001) compared to placebo.1,2 Observed events were 1.2% in treatment arm vs 5% in placebo arm. The efficacy of Beyfortus against the secondary endpoint of hospitalisation was 60.2% (95% CI: -14.6, 86.2). Observed events were 0.6% in treatment arm vs 1.6% in placebo arm. Between July 2019 and March 2020, 1,490 infants were randomised to receive either nirsevimab or placebo at the RSV season start Initial data from the MELODY Primary Cohort were published in NEJM in March 2022 12
Results from the Phase IIb trial (Trial 03)
The primary endpoint of the Phase IIb study was met, reducing the incidence of medically attended LRTI caused by RSV by 70.1% (95% CI: 52.3, 81.2) compared to placebo. Observed events were 2.6% in treatment arm vs 9.5% in placebo arm. Between November 2016 and December 2017, 1,453 infants were randomised (Beyfortus, n=969; placebo, n=484) at the RSV season start. Research was conducted by AstraZeneca in both hemispheres, at 164 sites in 23 countries. Data were published in NEJM in July 2020.3,12
In a prespecified secondary endpoint, Beyfortus reduced medically attended RSV LRTI with hospitalisation by 78.4% (95% CI 51.9, 90.3) versus placebo. Observed events were 0.8% in treatment arm vs 4.1% in placebo arm.3,12 A post-hoc analysis of the Phase IIb study that applied the recommended 50 mg dose in a subgroup of infants weighing less than 5 kg showed the efficacy of Beyfortus against medically attended RSV LRTI and medically attended RSV LRTI with hospitalisation was 86.2% (95% CI 68.0, 94.0) and
86.5% (95% CI 53.5, 96.1), respectively.12
Sanofi Alliance
In March 2017, AstraZeneca and Sanofi announced an agreement to develop and commercialise nirsevimab. Under the terms of the agreement, AstraZeneca leads development and manufacturing activities, and Sanofi leads commercialisation activities and records revenue. The two companies share costs and profits in all territories except the US. AstraZeneca's revenue from the agreement is reported as Alliance Revenue and Collaboration Revenue in the Company’s financial statements. Following a revision to the profit-sharing arrangement relating to the development and commercialisation of nirsevimab in the US between AstraZeneca, Sanofi and Sobi, Sobi has entered into a direct relationship with Sanofi, replacing the previous participation agreement with AstraZeneca entered into in November 2018.
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca's nirsevimab approved as RSV treatment for babies, infants
Jul. 17, 2023 2:03 PM ET
By: Jonathan Block, SA News Editor
- The US FDA has approved AstraZeneca's Beyfortus (nirsevimab) to prevent respiratory syncytial virus in babies and infants up to two years old.
- The monoclonal antibody is to be given as a single dose before the RSV season begins in the fall.
- AstraZeneca PLC (AZN)
- https://www.astrazeneca.com/
VYVGART Hytrulo
Beyfortus™ (nirsevimab-alip)
VYVGART Hytrulo
argenx Reports Positive Topline Data from ADHERE Study of VYVGART Hytrulo in Patients with Chronic Inflammatory Demyelinating Polyneuropathy
NewsJuly 17, 2023
argenx Reports Positive Topline Data from ADHERE Study of VYVGART Hytrulo in Patients with Chronic Inflammatory Demyelinating Polyneuropathy
Amsterdam, The Netherlands
- Study met primary endpoint (p=0.000039); VYVGART® Hytrulo demonstrated 61% reduction (HR: 0.39 95% CI: 0.25; 0.61) in risk of relapse versus placebo
- IgG autoantibodies shown to play significant role in underlying CIDP disease biology
- Favorable safety and tolerability profile consistent with previous clinical trials and confirmed safety profile of VYVGART®
- Conference call scheduled for today, July 17, 2023 at 8:30am ET (2:30pm CET)
argenx SE (Euronext & Nasdaq: ARGX), a global immunology company committed to improving the lives of people suffering from severe autoimmune diseases, today announced positive topline results from the ADHERE study evaluating VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) in adults with chronic inflammatory demyelinating polyneuropathy (CIDP). The study met its primary endpoint (p=0.000039), demonstrating a significantly lower risk of relapse with VYVGART Hytrulo compared to placebo. Detailed data from ADHERE will be presented at an upcoming medical meeting.
ADHERE Highlights
- Primary endpoint met (p=0.000039); VYVGART Hytrulo demonstrated 61% reduction (HR: 0.39 95% CI: 0.25; 0.61) in the risk of relapse versus placebo
- 67% of patients in open-label Stage A demonstrated evidence of clinical improvement (ECI), indicating that IgG autoantibodies play a significant role in the underlying biology of CIDP
- Safety and tolerability profile consistent with confirmed safety profile of VYVGART
- 91% (226/249) of eligible patients continued to the ADHERE-Plus open-label extension study
"CIDP is a chronic, progressive autoimmune disease that can cause substantial disability in those affected, often leading to impaired ambulation or difficulty completing normal daily tasks without help. The positive ADHERE data show that VYVGART Hytrulo may represent a new patient-forward treatment option that can prevent symptom deterioration while minimizing side effects and treatment burden,” commented Jeffrey Allen, M.D., Associate Professor, Department of Neurology, University of Minnesota. “With ADHERE, argenx has set a new standard for innovative CIDP studies that more broadly inform the neuromuscular community. The findings from the trial indicate we may have a novel weapon to combat this debilitating condition in our ongoing efforts to improve the lives of individuals affected by CIDP.”
“People living with CIDP often experience significant challenges with daily function including fatigue, numbness, tingling, pain and weakness while facing a future with limited mobility or independence. The promising ADHERE data bring hope to the CIDP community of a brighter future where they could experience more positive moments doing the things that make them most happy,” said Lisa Butler, Executive Director of the GBS-CIDP Foundation International.
“With these positive ADHERE data, we have generated strong clinical evidence that CIDP has a significant IgG-driven pathogenesis component and that VYVGART Hytrulo can meaningfully improve and stabilize disease symptoms with a favorable safety profile and a simple route of administration,” commented Luc Truyen, M.D., Ph.D., Chief Medical Officer of argenx. “We are very grateful to the patients participating in the ADHERE trial and their supporters, the investigators, our collaborators and our argenx colleagues for the success of this innovative trial. Together, we are moving one step closer to transforming the treatment of autoimmunity.”
Detailed ADHERE Results
ADHERE is the largest clinical trial of CIDP patients to date, enrolling adults who were treatment naïve (not on active treatment within the past six months) or currently on immunoglobulin therapy or corticosteroids. The trial consisted of a run-in period where current treatment was stopped followed by an open-label Stage A, after which responders to VYVGART Hytrulo advanced to a randomized, placebo- controlled Stage B.
322 patients enrolled in Stage A and received treatment with VYVGART Hytrulo
- 67% (214/322) demonstrated evidence of clinical improvement (ECI) after a run-in withdrawal period based on the Inflammatory Neuropathy Cause and Treatment (INCAT) Disability Score, the Inflammatory Rasch-built Overall Disability Scale (I-RODS) or grip strength
- 70% (214/304) demonstrated ECI excluding patients ongoing in Stage A at the time of the 88th event who did not have the full opportunity to achieve a response
- 78% (214/275) demonstrated ECI in a sensitivity analysis of patients who received at least four injections to reach the full IgG-lowering effect of VYVGART Hytrulo
- Response rates similar across all prior CIDP medication subgroups with consistent efficacy on INCAT, I-RODS and grip strength.
221 responders from Stage A entered Stage B, where the primary endpoint was the relative risk of relapse based on time to relapse on the INCAT Disability Score
- VYVGART Hytrulo significantly reduced the risk of CIDP relapse compared to placebo
- Primary endpoint was met (p=0.000039); VYVGART Hytrulo demonstrated a 61% reduction (HR: 0.39 95% CI: 0.25; 0.61) in the risk of relapse compared to placebo based on time to the first adjusted INCAT deterioration of ≥1 point
- VYVGART Hytrulo patients had a lower relapse rate compared to placebo at Week 24 (26% versus 54%) and Week 48 (34% versus 60%)
- VYVGART Hytrulo patients experienced longer time to relapse compared to those on placebo with a rapid separation of the Kaplan–Meier curves beginning at Week 4 and sustained through Week 48
- VYVGART Hytrulo patients demonstrated a clinically meaningful mean improvement of 7.7 points on I-RODS and 12.3kPa on grip strength in Stage A. This clinically meaningful benefit was maintained in Stage B by treated patients and lost in placebo patients.
- Clinical benefit observed across all efficacy scales and patient subgroups, regardless of prior therapy
VYVGART Hytrulo was well-tolerated with a safety profile that is consistent with prior clinical trials and the known profile of VYVGART. The most frequent treatment-related adverse event was injection site reactions (ISRs), which occurred in a lower percentage of patients than previous VYVGART Hytrulo trials (20% in Stage A; 10% in Stage B). All ISRs were mild to moderate and resolved over time.
About Chronic Inflammatory Demyelinating Polyneuropathy
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a rare and serious autoimmune disease of the peripheral nervous system. Although confirmation of disease pathophysiology is still emerging, there is increasing evidence that IgG antibodies play a key role in the damage to the peripheral nerves. People with CIDP experience fatigue, muscle weakness and a loss of feeling in their arms and legs that can get worse over time or may come and go. These symptoms can significantly impair a person's ability to function in their daily lives. Without treatment, one-third of people living with CIDP will need a wheelchair.
About VYVGART® Hytrulo
VYVGART Hytrulo is a subcutaneous combination of efgartigimod alfa, a human IgG1 antibody fragment marketed for intravenous use as VYVGART®, and recombinant human hyaluronidase PH20 (rHuPH20), Halozyme’s ENHANZE® drug delivery technology to facilitate subcutaneous injection delivery of biologics. In binding to the neonatal Fc receptor (FcRn), VYVGART Hytrulo results in the reduction of circulating IgG. It is the first-and-only approved FcRn blocker administered by subcutaneous injection.
VYVGART Hytrulo is the proprietary name in the U.S. for subcutaneous efgartigimod alfa and recombinant human hyaluronidase PH20. It may be marketed under different proprietary names following approval in other regions.
See Important Safety Information below and full Prescribing Information for VYVGART Hytrulo for additional information
Important Safety Information
What is VYVGART® HYTRULO (efgartigimod alfa and hyaluronidase-qvfc)?
VYVGART HYTRULO is a prescription medicine used to treat a condition called generalized myasthenia gravis, which causes muscles to tire and weaken easily throughout the body, in adults who are positive for antibodies directed toward a protein called acetylcholine receptor (anti-AChR antibody positive).
About argenx
argenx is a global immunology company committed to improving the lives of people suffering from severe autoimmune diseases. Partnering with leading academic researchers through its Immunology Innovation Program (IIP), argenx aims to translate immunology breakthroughs into a world-class portfolio of novel antibody-based medicines. argenx developed and is commercializing the first approved neonatal Fc receptor (FcRn) blocker in the U.S., Japan, Israel, the EU, the UK and China. The Company is evaluating efgartigimod in multiple serious autoimmune diseases and advancing several earlier stage experimental medicines within its therapeutic franchises. For more information, visit www.argenx.com and follow us on LinkedIn, Twitter, and Instagram.
Argenx/Zai Lab rise on phase 2 results for autoimmune disorder asset
Jul. 17, 2023 10:38 AM ET
By: Jonathan Block, SA News Editor
- Argenx (NASDAQ:ARGX) and Zai Lab (NASDAQ:ZLAB) said that the primary endpoint was met in a mid-stage study of Vyvgart Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) in adults with chronic inflammatory demyelinating polyneuropathy (CIDP).
- Zai Lab has exclusive development and commercialization rights for Vyvgart Hytrulo in China.
- argenx SE (ARGX), ZLAB
- https://www.argenx.com/products
acoramidis
Beyfortus™ (nirsevimab-alip)
VYVGART Hytrulo
bridgebio announces consistently positive results from phase 3 attribute-cm study of acoramidis for patients with transthyretin amyloid cardiomyopathy (attr-cm)
07.17.2023 at 7:00 AM EDT
- Highly statistically significant result observed on primary endpoint with a Win Ratio of 1.8 (p<0.0001)
- 58% of ties in Finkelstein-Schoenfeld (F-S) primary analysis broken by all-cause mortality and frequency of cardiovascular-related hospitalization; statistical significance also achieved on an F-S test with those two parameters alone (p=0.0182)
- Clinically meaningful and consistent separation observed on all measures of mortality, morbidity, function, and quality of life
- On-treatment survival rate of 81% versus placebo survival rate of 74% (absolute risk reduction of 6.43%; relative risk reduction of 25%)
- Highly statistically significant relative risk reduction of 50% (p<0.0001) observed on frequency of cardiovascular-related hospitalization
- Highly statistically significant and clinically meaningful treatment benefit observed at 30 months on the secondary endpoints of NT-proBNP (p<0.0001), KCCQ (p<0.0001), and 6-minute walk distance (p<0.0001)
- In comparative exploratory post hoc analyses enabled by tafamidis drop-in, albeit at low patient numbers, acoramidis showed 42% greater increase in serum TTR levels and a 92% improvement in median NT-proBNP relative to placebo + tafamidis
- No safety signals of potential clinical concern identified
- Company intends to file a New Drug Application (NDA) with the U.S. Food and Drug Administration by end of 2023; late-breaker presentation has been accepted for annual meeting of the European Society of Cardiology
PALO ALTO, Calif., July 17, 2023 (GLOBE NEWSWIRE) -- BridgeBio Pharma, Inc. (Nasdaq: BBIO) (“BridgeBio” or the “Company”), is a commercial-stage biopharmaceutical company focused on genetic diseases and cancers. Today, alongside the dedicated physicians and courageous patients who participated, the Company reports positive results from ATTRibute-CM, its Phase 3 study of acoramidis in transthyretin amyloid cardiomyopathy, or ATTR-CM. ATTRibute-CM was designed to study the efficacy and safety of acoramidis, an investigational, next-generation, orally-administered, highly potent, small molecule stabilizer of transthyretin (TTR). BridgeBio will host an investor call on July 17, 2023 at 8:00 am ET to discuss these results.
“The outstanding results of the ATTRibute-CM study provide new hope to patients living with transthyretin amyloid cardiomyopathy, or ATTR-CM”, said Dr. Daniel Judge, Professor of Medicine and Cardiology at the Medical University of South Carolina, and Co-Chair of the ATTRibute-CM Steering Committee. “The consistent and clinically meaningful benefits on survival, hospitalization, and additional measures of illness severity are truly remarkable.”
“ATTR-CM is an increasingly recognized cause of heart failure. The results from BridgeBio’s ATTRibute-CM trial are very exciting and bring much hope to amyloidosis patients and their loved ones,” said Muriel Finkel, President of Amyloidosis Support Groups, a non-profit organization dedicated to the support of amyloidosis patients and caregivers.
Key results from the clinical trial include:
- A highly statistically significant improvement in the primary endpoint (a hierarchical analysis prioritizing in order: all-cause mortality, then frequency of cardiovascular-related hospitalization, then change from baseline in NT-proBNP, then change from baseline in 6-minute walk distance) demonstrated by a Win Ratio of 1.8 (p<0.0001).
- An 81% on-treatment survival rate (versus a 74% survival rate on placebo), which begins to approach actuarial models of life expectancy absent ATTR-CM (85% in this population as has been documented). The absolute risk reduction was 6.43% and the relative risk reduction was 25%.
- A highly statistically significant relative risk reduction of 50% (p<0.0001) on frequency of cardiovascular-related hospitalization. The impact and marked magnitude of risk reduction was seen across all analytical methods employed.
- The Company consistently observed a statistically significant treatment effect at 30 months across additional measured markers of morbidity, quality of life, and function:
- Change from baseline in N-terminal prohormone of brain natriuretic peptide (NT-proBNP) (p<0.0001)
- Change from baseline in Kansas City Cardiomyopathy Questionnaire (p<0.0001)
- Change from baseline in 6-minute walk distance (p<0.0001)
- No safety signals of potential clinical concern were identified.
A key objective in the rational drug design of acoramidis was to maximize TTR stabilization at clinically achieved blood concentrations. Several lines of evidence suggest that maximizing stabilization could lead to improved benefits for ATTR patients:
- Historical ATTR genotype/phenotype data and the disease-protective properties of trans-allelic, trans-suppressor variants relative to pathogenic variants in compound heterozygotes and the general, nonvariant population
- The outperformance of 80mg tafamidis vs 20mg tafamidis in the previously published ATTR-ACT trial
- Results from ATTR-polyneuropathy clinical trials
BridgeBio’s design strategy to maximize TTR stabilization by acoramidis was to phenocopy the hyperstabilizing molecular mechanism of the T119M trans-allelic, trans-suppressor rescue mutation. Prior preclinical and clinical studies have shown that acoramidis demonstrates approximately twice the stabilization of already-marketed stabilizers.
The allowance of tafamidis drop-in after at least 12 months in both the placebo and the acoramidis arms of the ATTRibute-CM trial provided the Company an opportunity to analyze, in an exploratory post hoc fashion and albeit at low patient numbers, differences in stabilizer performance as measured by serum TTR and NT-proBNP. The findings at 30 months were that:
- Acoramidis showed a 42% greater increase in serum TTR levels versus tafamidis
- Acoramidis showed a 92% improvement in median NT-proBNP relative to placebo + tafamidis
No comparison can be made as to the potential effectiveness or safety of acoramidis and tafamidis, given that these are exploratory analyses, and the study was not prospectively designed for a head-to-head comparison.
“Our heartfelt thanks go out to the patients, their caregivers, investigators, and study staff who have actively participated in ATTRibute-CM and continue to contribute to this pivotal research," stated Jonathan Fox, M.D., Ph.D., President and Chief Medical Officer of BridgeBio Cardiorenal. "We are extremely encouraged by the robustly positive and consistent findings of the ATTRibute-CM study, which confirm our position that highly potent TTR stabilization has the potential to profoundly impact patients’ lives. We look forward to presenting the data to health authorities to bring acoramidis to patients as expeditiously as possible."
The Company intends to submit its NDA to the US FDA before the end of 2023, with regulatory filings in additional markets to follow in 2024. This activity will occur in parallel with the prosecution of the remainder of the BridgeBio portfolio, which like acoramidis consists of medicines that target well-described diseases at their source. Acoramidis has intellectual property protection out to at least 2039.
Webcast Information
BridgeBio will host an investor call and simultaneous webcast to discuss the results from the Phase 3 ATTRibute-CM study of acoramidis in patients with ATTR-CM on July 17, 2023, at 8:00 am ET. A link to the webcast may be accessed from the event calendar page of BridgeBio’s website at https://investor.bridgebio.com/. A replay of the conference call and webcast will be archived on the Company’s website and will be available for at least 30 days following the event.
About BridgeBio Pharma, Inc.
BridgeBio Pharma, Inc. (BridgeBio) is a commercial-stage biopharmaceutical company founded to discover, create, test, and deliver transformative medicines to treat patients who suffer from genetic diseases and cancers with clear genetic drivers. BridgeBio’s pipeline of development programs ranges from early science to advanced clinical trials. BridgeBio was founded in 2015 and its team of experienced drug discoverers, developers and innovators are committed to applying advances in genetic medicine to help patients as quickly as possible. For more information visit bridgebio.com and follow us on LinkedIn and Twitter.
BridgeBio stock soars 80% on Phase 3 data, filing update for heart drug
Jul. 17, 2023 12:05 PM ET
By: Val Brickates Kennedy, SA News Editor1 Comment
Shares of BridgeBio (NASDAQ:BBIO) shot up 80% in midday trading Monday after the biotech company said it plans to file for US regulatory approval of its drug acoramidis by the end of the year after releasing positive Phase 3 data for the drug in the treatment of ATTR-CM.
BridgeBio shares opened at $26.76, recently changing hands at $32.81 at around 11:55 a.m. ET.
Earlier Monday, BridgeBio said the Phase 3 study showed an on-treatment survival rate of 81% for patients who took acoramidis versus 74% for those who took a placebo. The company also reported a "highly statistically significant" relative risk reduction of 50% for frequency of cardiovascular-related hospitalizations.
Domvanalimab
Zenocutuzumab (Zeno)
Domvanalimab
Gilead and Arcus Announce Anti-TIGIT Domvanalimab Continues to Demonstrate Consistent Improvement in Progression-Free Survival in Non-Small Cell Lung Cancer Study
June 03, 2023
DOWNLOAD PDFPDF FORMAT (OPENS IN NEW WINDOW)
– Clinically Meaningful Reduction in Risk of Progression or Death Was Observed in the Domvanalimab-Containing Study Arms Compared to Zimberelimab Monotherapy in First-Line, PD-L1-High NSCLC –
– Objective Response Rate (ORR) Improved in Both Domvanalimab-Containing Study Arms Compared to Zimberelimab Monotherapy –
– Results Will Be Presented Today During the American Society of Clinical Oncology (ASCO) Annual Meeting –
FOSTER CITY, Calif., & HAYWARD, Calif.--(BUSINESS WIRE)-- Gilead Sciences, Inc. (Nasdaq: GILD) and Arcus Biosciences, Inc. (NYSE: RCUS) today announced updated results from an interim analysis of the ARC-7 study in patients with first-line, metastatic non-small cell lung cancer (NSCLC) with PD-L1 tumor proportion score (TPS) ≥50% without epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) mutations. ARC-7 is the first Phase 2, randomized, open-label study evaluating the combinations of Fc-silent anti-TIGIT monoclonal antibody domvanalimab plus anti-PD-1 monoclonal antibody zimberelimab (doublet) and domvanalimab plus zimberelimab and etrumadenant, an A2a/b adenosine receptor antagonist (triplet), versus zimberelimab monotherapy. These results will be presented today during the ASCO Plenary Series: Rapid Abstract Updates session by Melissa L. Johnson, M.D., Director, Lung Cancer Research, Sarah Cannon Research Institute, and Lead Investigator for the ARC-7 study. Arcus will post the updated ARC-7 results, which will include the data presented at Dr. Johnson’s session, as well as additional data, on its website on the corporate presentation page at 5:30pm PDT.
“Progression-free survival curves showed early separation of both domvanalimab-containing arms from the zimberelimab arm, which was consistently maintained, and supports the potential therapeutic benefit of inhibiting the TIGIT pathway,” said Melissa L. Johnson, M.D., Director, Lung Cancer Research, Sarah Cannon Research Institute, and Lead Investigator for the ARC-7 study. “I was also encouraged by the consistency of meaningful improvements across other outcome measures for the domvanalimab-containing arms. I look forward to continuing to work with Gilead and Arcus on the dom-zim combinations.”
At the time of data cutoff (DCO), February 7, 2023, safety and efficacy were evaluated in all patients randomized and treated (n=150). With a median follow-up time of approximately 18 months, both domvanalimab-containing study arms demonstrated sustained, clinically meaningful improvements in progression-free survival (PFS) compared to zimberelimab monotherapy, with a 33% reduction in risk of disease progression or death for the doublet and 28% for the triplet.
“At this analysis, the domvanalimab-containing study arms continued to show improved efficacy across multiple measures and both the doublet and triplet arms were generally well tolerated,” said Dimitry S.A. Nuyten, M.D., Ph.D., Chief Medical Officer of Arcus Biosciences. “These data reinforce our confidence in the domvanalimab program.”
“The ARC-7 proof-of-concept study has critically advanced our understanding of the activity of domvanalimab, the first Fc-silent anti-TIGIT monoclonal antibody in pivotal trials,” said Bill Grossman, M.D., Ph.D., Senior Vice President, Therapeutic Area Head, Gilead Oncology. “We look forward to quickly advancing our four ongoing Phase 3 registrational programs in NSCLC and upper GI cancers.”
No unexpected safety signals were observed across the three study arms at the time of DCO. The domvanalimab-containing study arms appeared to be generally well tolerated and showed an overall safety profile consistent with the known safety profiles of each individual molecule to date. Incidence of infusion-related reactions was low across all treatment arms: 4%, 4% and 12% for zimberelimab monotherapy and the domvanalimab-doublet and -triplet arms, respectively. The addition of domvanalimab to zimberelimab did not increase the incidence of infusion-related reactions, consistent with the Fc-silent design of domvanalimab.
Domvanalimab, zimberelimab and etrumadenant are investigational molecules. Neither Gilead nor Arcus has received approval from any regulatory authority for any use globally, and their safety and efficacy for the treatment of lung cancer have not been established.
About the ARC-7 Study
The ARC-7 study is the first Phase 2, multicenter, three-arm, randomized, open-label study evaluating the safety and efficacy of anti-TIGIT antibody domvanalimab plus anti-PD-1 antibody zimberelimab (doublet) versus domvanalimab plus zimberelimab and etrumadenant (triplet), an A2a/b adenosine receptor antagonist, versus zimberelimab monotherapy in 150 patients with first-line metastatic non-small cell lung cancer (NSCLC) with PD-L1 TPS ≥50% and no EGFR or ALK mutations. Patients are randomized 1:1:1 across the three study arms, and patients who progress on zimberelimab monotherapy may cross over to receive the triplet. At the time of this interim analysis, 150 patients had a median follow-up of 18.5 months. The co-primary endpoints are objective response rate and progression-free survival per Response Evaluation Criteria in Solid Tumors (RECIST 1.1). Secondary endpoints include duration of response, disease control rate, overall survival and safety. ARC-7 is a proof-of-concept study to assess the safety and efficacy of domvanalimab-containing study arms over zimberelimab monotherapy. More information about ARC-7 is available at: https://clinicaltrials.gov/ct2/show/NCT04262856.
About Domvanalimab
Domvanalimab is the first Fc-silent investigational monoclonal antibody in pivotal trials that is designed to block and bind to the T-cell immunoreceptor with Ig and ITIM domains (TIGIT), a protein receptor on immune cells that acts as a brake on the immune response. Cancer cells can exploit TIGIT to avoid detection by the immune system. By binding to TIGIT, domvanalimab is expected to free up immune activating pathways and activate immune cells to attack and kill cancer cells. Domvanalimab has demonstrated complete receptor coverage on all TIGIT-expressing peripheral leukocytes.
Domvanalimab is being evaluated in four registrational Phase 3 studies across lung and gastrointestinal cancers, including: (1) ARC-10, evaluating domvanalimab plus zimberelimab versus pembrolizumab in first-line locally advanced or metastatic PD-L1 ≥50% NSCLC; (2) PACIFIC-8, being operationalized by AstraZeneca, evaluating domvanalimab plus durvalumab in unresectable Stage 3 NSCLC; (3) STAR-121, evaluating domvanalimab plus zimberelimab and chemotherapy versus pembrolizumab plus chemotherapy in first-line PD-L1-unselected NSCLC; and (4) STAR-221, evaluating domvanalimab plus zimberelimab and chemotherapy versus nivolumab plus chemotherapy in first-line locally advanced, unresectable or metastatic gastric, esophageal and gastro-esophageal junction adenocarcinomas.
About Arcus Biosciences
Arcus Biosciences is a clinical-stage, global biopharmaceutical company developing differentiated molecules and combination medicines for people with cancer. In partnership with industry partners, patients and physicians around the world, Arcus is expediting the development of first- or best-in-class medicines against well-characterized biological targets and pathways and studying novel, biology-driven combinations that have the potential to help people with cancer live longer. Founded in 2015, the company has advanced multiple investigational medicines into clinical studies, including new combination approaches that target TIGIT, PD-1, the adenosine axis (CD73 and A2a/A2b receptors) and HIF-2a. For more information about Arcus Biosciences’ clinical and preclinical programs, please visit www.arcusbio.com.
About Gilead Sciences
Gilead Sciences, Inc. is a biopharmaceutical company that has pursued and achieved breakthroughs in medicine for more than three decades, with the goal of creating a healthier world for all people. The company is committed to advancing innovative medicines to prevent and treat life-threatening diseases, including HIV, viral hepatitis and cancer. Gilead operates in more than 35 countries worldwide, with headquarters in Foster City, California.
Source: Arcus Biosciences
Gilead raises stake in Arcus Biosciences
Jul. 06, 2023 1:15 PM ET
Arcus Biosciences, Inc. (RCUS), GILD
By: Dulan Lokuwithana, SA News Editor
Update 3:24PM EST: Adds comments from Arcus
According to a regulatory filing on Thursday, Gilead (NASDAQ:GILD) has increased its ownership in cancer-focused biotech Arcus Biosciences (NYSE:RCUS) with the purchase of ~1.0M additional RCUS shares for $19.26 apiece in late June.
The disclosure was made weeks after the duo expanded their oncology collaboration. The purchase consideration of $19.4M was spent from the available cash resources, Gilead (GILD) said in a regulatory filing.
https://seekingalpha.com/news/3986021-gilead-raises-stake-in-arcus-biosciences
PAXALISIB
Zenocutuzumab (Zeno)
Domvanalimab
KAZIA'S PAXALISIB RECEIVES FAST TRACK DESIGNATION FROM FDA FOR TREATMENT OF SOLID TUMOR BRAIN METASTASES HARBORING PI3K PATHWAY MUTATIONS IN COMBINATION WITH RADIATION THERAPY
NEWS PROVIDED BY
06 Jul, 2023, 07:00 ET
SYDNEY, July 6, 2023 /PRNewswire/ -- Kazia Therapeutics Limited (NASDAQ: KZIA; ASX: KZA), an oncology-focused drug development company, is pleased to announce that its lead program, paxalisib, has been awarded Fast Track Designation (FTD) by the United States Food and Drug Administration (FDA) for the treatment of solid tumor brain metastases harboring PI3K pathway mutations in combination with radiation therapy.
The FDA's decision to grant FTD was based on promising clinical data from an interim analysis of an ongoing Phase 1 clinical trial in which patients with brain metastases from a primary tumour are receiving paxalisib in combination with radiotherapy (NCT04192981). These clinical data were presented at the 2022 Annual Conference on CNS Clinical Trials and Brain Metastases, jointly organized by the Society for Neuro-Oncology (SNO) and the American Society for Clinical Oncology (ASCO), by Dr. Jonathan Yang, lead investigator in the clinical trial. All nine evaluable patients in the trial (100%) responded to the combination of paxalisib with radiotherapy. Published benchmarks suggest a typical response rate for radiotherapy alone to be around 20-40%.
Key Points
- FTD is designed to expedite development of pharmaceutical products which demonstrate the potential to address unmet medical needs in serious or life-threatening conditions.
- FTD provides Kazia with enhanced access to FDA, including opportunities for face-to-face meetings and written consultation throughout the remaining development of paxalisib. Drugs granted FTD may also be eligible for Accelerated Approval and Priority Review, which may result in faster product approval.
- Paxalisib was previously granted FTD for glioblastoma in August 2020, giving paxalisib now two largely independent opportunities to access the benefits of this designation.
"Brain metastases are rapidly emerging as a key pillar of paxalisib's clinical development," said Dr. John Friend, Chief Executive Officer of Kazia. "We have seen a high level of interest from clinicians in the emerging data from this patient population, and it is exciting to now have that interest complemented by FDA's award of Fast Track Designation. With important data read-outs expected in adult and childhood brain cancer during CY2023, we will be working with investigators and advisors to drive forward our research in brain metastases also."
Brain Metastases
Brain metastases are a common complication of many tumours, but are particularly common in breast cancer, lung cancer, and melanoma. Brain metastases are typically highly resistant to treatment and survival rates are generally low. More than 250,000 patients are diagnosed with brain metastases each year in the United States alone.
Radiotherapy is a common treatment modality for brain metastases. Despite some efficacy, patients typically become resistant over time, and repeat courses of radiotherapy can be associated with significant neurological toxicity.
Expansion of Paxalisib Brain Metastases Study
The Phase I study (NCT04192981)is evaluating the safety and efficacy of paxalisib in combination with whole brain radiotherapy (WBRT) in patients with brain metastases and leptomeningeal metastases from any primary tumour (cancer that has spread to the brain from elsewhere in the body). The study was designed and initiated by Dr. Jonathan Yang, when he was at Memorial Sloan Kettering Cancer Center in New York, NY.
The study was designed in two stages. The first stage aimed to recruit 12 patients and was intended to establish the maximum tolerated dose (MTD) for paxalisib in conjunction with WBRT. Subject to positive results in the first stage, the study includes a second stage to assess initial efficacy signals and establish whether further development is warranted.
The results of the first stage of the study were reported at the SNO / ASCO 2022 Annual Conference on CNS Trials and Brain Metastases in August 2022. The combination was reported to be generally well-tolerated, with all nine evaluable patients showing evidence of clinical response.
Recruitment of the second stage commenced in 2H CY2022. The study is now open at two additional clinical sites: Miami Cancer Institute in Miami, FL, and the Fred Hutchinson Cancer Center in Seattle, WA, where Dr. Yang is now based.
Fast Track Designation
Introduced under the FDA Modernization Act (1997), FTD may be awarded by FDA to investigational drugs which are intended to treat a serious or life-threatening condition, and which fill an unmet medical need. FTD must be requested by the sponsor company and must be accompanied by a detailed review of both preclinical and clinical data. To be awarded FTD, drugs must generally be able to show some potential advantage over existing therapies, either in terms of safety or efficacy.
The key benefits of FTD comprise enhanced access to FDA, with regular and more frequent opportunities for consultation and discussion. In addition, drugs with FTD may be eligible for Accelerated Approval, in which a new medicine is approved based on a surrogate endpoint, and Priority Review, in which the standard 12-month review process may be reduced to eight months. Drugs with FTD may also receive a 'rolling review' of their NDA submission, in which sections are submitted for review as they become available, potentially expediting the approval process.
Next Steps
Further data from the ongoing Phase 1 study is expected in 1Q CY2024. Kazia continues to hold discussions with clinicians and advisors regarding the potential design of a registrational study in this indication.
Paxalisib is also the subject of nine other ongoing clinical trials, including the pivotal GBM AGILE study in glioblastoma, which is expected to provide final data in 2H CY2023, and a phase II study in pediatric patients with diffuse midline gliomas, which is expected to provide initial data in 3Q CY2023.
About Kazia Therapeutics Limited
Kazia Therapeutics Limited (NASDAQ: KZIA; ASX: KZA) is an oncology-focused drug development company, based in Sydney, Australia.
Our lead program is paxalisib, a brain-penetrant inhibitor of the PI3K / Akt / mTOR pathway, which is being developed to treat multiple forms of brain cancer. Licensed from Genentech in late 2016, paxalisib is or has been the subject of ten clinical trials in this disease. A completed Phase II study in glioblastoma reported promising signals of clinical activity in 2021, and a pivotal study in glioblastoma, GBM AGILE, is ongoing, with final data expected in CY2023. Other clinical trials are ongoing in brain metastases, diffuse midline gliomas, and primary CNS lymphoma, with several of these having reported encouraging interim data.
Paxalisib was granted Orphan Drug Designation for glioblastoma by the FDA in February 2018, and Fast Track Designation for glioblastoma by the FDA in August 2020. In addition, paxalisib was granted Rare Pediatric Disease Designation and Orphan Drug Designation by the FDA for diffuse intrinsic pontine glioma in August 2020, and for atypical teratoid / rhabdoid tumours (AT/RT) in June 2022 and July 2022, respectively.
Kazia is also developing EVT801, a small-molecule inhibitor of VEGFR3, which was licensed from Evotec SE in April 2021. Preclinical data has shown EVT801 to be active against a broad range of tumour types and has provided compelling evidence of synergy with immuno-oncology agents. A Phase I study commenced recruitment in November 2021.
For more information, please visit www.kaziatherapeutics.com or follow us on Twitter @KaziaTx.
This document was authorized for release by John Friend, MD, Chief Executive Officer.
SOURCE Kazia Therapeutics Limited
Kazia jumps as FDA awards Fast Track tag for lead program
Jul. 06, 2023 7:29 AM ET
Kazia Therapeutics Limited (KZIA)
By: Dulan Lokuwithana, SA News Editor
Australian biotech Kazia Therapeutics (NASDAQ:KZIA) added ~29% pre-market Thursday after announcing that the FDA issued Fast Track Designation for its lead program, paxalisib, in combination with radiation therapy for certain patients with brain metastases.
https://seekingalpha.com/news/3985876-kazia-stock-jumps-fda-fast-track-tag-lead-program
Kazia Therapeutics Limited (KZIA)
https://www.kaziatherapeutics.com/site/for-researchers/paxalisib
Zenocutuzumab (Zeno)
Zenocutuzumab (Zeno)
FUJOVEE™ (Abivertinib)
Zenocutuzumab (Zeno) granted second Breakthrough Therapy Designation by the U.S. Food & Drug Administration
July 5, 2023 at 4:01 PM EDT
– Zeno granted BTD for the treatment of NRG1+ non-small cell lung cancer
UTRECHT, The Netherlands and CAMBRIDGE, Mass., July 05, 2023 (GLOBE NEWSWIRE) -- Merus N.V. (Nasdaq: MRUS), a clinical-stage oncology company developing innovative, full-length multispecific antibodies (Biclonics® and Triclonics®) for cancer, today announced that the U.S. Food and Drug Administration (FDA) has granted Breakthrough Therapy Designation (BTD) for zenocutuzumab (Zeno) for the treatment of patients with advanced unresectable or metastatic NRG1 fusion (NRG1+) non-small cell lung cancer (NSCLC), following progression with prior systemic therapy. This designation for Zeno follows BTD for the treatment of patients with NRG1+ pancreatic cancer, following progression with prior systemic therapy or in patients who have no satisfactory alternative treatment options recently announced on June 30, 2023, Fast Track Designation for the treatment of patients with metastatic solid tumors harboring NRG1 gene fusions (NRG1+ cancer) that have progressed on standard of care therapy announced in January 2021 and Orphan Drug Designation for the treatment of patients with pancreatic cancer announced in July 2020.
BTD is supported by data from the ongoing phase 1/2 eNRGy trial and Early Access Program (EAP) which are assessing the safety and anti-tumor activity of Zeno monotherapy in NRG1+ cancer (Phase 1/2: NCT02912949, EAP: NCT04100694). Data from the eNRGy trial and EAP were featured as oral presentations during the 2021 and 2022 American Society of Clinical Oncology Annual Meetings (Abstract #3003, #105 respectively). As of June 1, 2023, more than 175 patients with NRG1+ cancer have been treated with Zeno monotherapy.
BTD is intended to expedite the development and review of a medicine to treat a serious or life-threatening condition, where preliminary clinical evidence indicates that the drug may demonstrate substantial improvement on clinically significant endpoints over available therapies. BTD allows for more intensive FDA guidance on an efficient drug development program, an organizational commitment involving senior managers, and experienced review staff, as appropriate, in a collaborative, cross-disciplinary review, and eligibility for rolling review and priority review. With this BTD, Merus plans to engage in these discussions with the FDA in an expedited manner, and then provide a further update on the path and timeline to a potential Biologics License Application (BLA) submission.
Merus believes that obtaining a commercialization partnership agreement will be an essential step in bringing Zeno to patients with NRG1+ cancer, if approved.
“We are thrilled to receive the second BTD for Zeno, this time in NRG1+ lung cancer,” said Bill Lundberg, M.D., President, Chief Executive Officer of Merus. “We believe this further acknowledges Zeno’s clinically meaningful, durable response for patients with NRG1+ cancer and we aim to bring this potential first and best in class targeted agent for NRG1+ cancer to market with support from a potential commercial partner.”
Merus plans to provide a clinical update on Zeno in NRG1+ cancer at a major medical conference in 2023.
Further, Merus is evaluating Zeno in combination with androgen deprivation therapy (enzalutamide or abiraterone) in castration resistant prostate cancer (CRPC), irrespective of NRG1+ status. Merus plans to provide initial clinical data on Zeno in CRPC in the second half of 2023. Merus is also evaluating Zeno in combination with afatinib in patients with NRG1+ NSCLC.
About the eNRGy Clinical Trial
Merus is currently enrolling patients in the phase 1/2 eNRGy trial to assess the safety and anti-tumor activity of Zeno monotherapy in NRG1+ cancer. The eNRGy trial consists of three cohorts: NRG1+ pancreatic cancer; NRG1+ non-small cell lung cancer; and other NRG1+ cancer. Further details, including current trial sites, can be found at www.ClinicalTrials.gov and Merus’ trial website at www.nrg1.com or by calling 1-833-NRG-1234.
About Zeno
Zeno is an antibody-dependent cell-mediated cytotoxicity (ADCC)-enhanced Biclonics® that utilizes the Merus Dock & Block® mechanism to inhibit the neuregulin/HER3 tumor-signaling pathway in solid tumors with NRG1 fusions (NRG1+ cancer). Through its unique mechanism of binding to HER2 and potently blocking the interaction of HER3 with its ligand NRG1 or NRG1-fusion proteins, Zeno has the potential to be particularly effective against NRG1+ cancer. In preclinical studies, Zeno potently inhibits HER2/HER3 heterodimer formation thereby inhibiting oncogenic signaling pathways, leading to inhibition of tumor cell proliferation and blocking tumor cell survival.
About Merus N.V.
Merus is a clinical-stage oncology company developing innovative full-length human bispecific and trispecific antibody therapeutics, referred to as Multiclonics®. Multiclonics® are manufactured using industry standard processes and have been observed in preclinical and clinical studies to have several of the same features of conventional human monoclonal antibodies, such as long half-life and low immunogenicity. For additional information, please visit Merus’ website, Twitter and LinkedIn.
Merus' zenocutuzumab given second Breakthrough Therapy designation
Jul. 05, 2023 4:35 PM ET
By: Jonathan Block, SA News Editor1 Comment
- The US FDA has granted Breakthrough Therapy designation for the second time to Merus' (NASDAQ:MRUS) zenocutuzumab for NRG1 fusion (NRG1+) non-small cell lung cancer.
- The candidate is currently in a phase 1/2 examining the safety and anti-tumor activity of zeno monotherapy in NRG1+ cancer.
- https://seekingalpha.com/news/3985782-merus-zenocutuzumab-given-second-breakthrough-therapy-designation
- Merus N.V. (MRUS)
- https://merus.nl/
- https://merus.nl/pipeline/
FUJOVEE™ (Abivertinib)
Epcoritamab (DuoBody®-CD3xCD20)
FUJOVEE™ (Abivertinib)
Shanghai Escugen Biotechnology Co., Ltd., a partner of Levena Biopharma, a Sorrento Company, releases positive results from a first-in-human study of ESG401, a TROP2 Antibody Drug Conjugate in patients with locally advanced/metastatic solid tumors at the
June 5, 2023 at 9:00 AM EDT
CHICAGO, June 05, 2023 (GLOBE NEWSWIRE) -- Shanghai Escugen Biotechnology Co., Ltd. (“Escugen”), a partner of Levena (Suzhou) Biopharma Co., Ltd. (“Levena”), a wholly owned subsidiary of Sorrento Therapeutics, Inc. (Sorrento), today released preliminary results from a first-in-human study of ESG401, a trophoblast cell-surface antigen 2 (TROP2) antibody drug conjugate (ADC), in patients with locally advanced/metastatic solid tumors at the 2023 Annual Meeting of ASCO, the American Society of Clinical Oncology, held June 2-6 in Chicago, IL. ESG401 is an innovative ADC developed by Escugen and Levena. Escugen and Levena Biopharma jointly own the domestic and international patents of this ADC and share global rights for the product. ESG401 is composed of a humanized anti-Trop2 IgG1 monoclonal antibody (mAb) conjugated to a topoisomerase I inhibitor SN38 via a proprietary stable covalent linker with a drug antibody ratio (DAR) of 8. ESG401 has potential differentiated advantages over its competitors in terms of safety, effectiveness and process robustness. Using an innovative, highly stable and cleavable linker, this ADC demonstrated that it releases very little free toxin during circulation, which may reduce off target toxicity in a series of preclinical studies. Additionally, premature release of the mAb may compete for binding sites with the ADC to reduce its efficacy. The ADC highly enriches in tumor tissues and rapidly endocytoses, thereby effectively killing tumor cells and inhibiting tumor growth.
In the Phase I study, adult ESG401 patients with locally advanced/metastatic solid tumors refractory to or relapsed from standard treatments with measurable disease (RECIST v1.1) were eligible. ESG401 was administered by IV infusion initially in an ascending dose safety study by designated dose and regimen until unacceptable toxicity or progressive disease and followed by expansion cohorts. The Bayesian Optimal Interval (BOIN) design was used to establish the maximum tolerated dose (MTD). As of February 3, 2023, 35 heavily pretreated patients with a median age of 53 years were treated with at least one dose of ESG401 during dose escalation, 2 to 20 mg/kg administered every 3 weeks (Regimen A), or 12 to 16 mg/kg on day 1, 8, and 15 in a 4-week cycle (Regimen B). Eighty percent of the patients had an ECOG status of 1. Sixty-three percent of the patients had received at least 3 lines of prior therapy and overall the number of lines of prior therapy was a median of 4 (range 2-10).
About Escugen Biotechnology Co., Ltd.
Escugen Biotechnology Co., Ltd. is a clinical-stage biotechnology company committed to developing and commercializing innovative drugs for the treatment of cancer, autoimmune disease and other diseases with unmet medical needs. The company’s leading programs include ESG401, an anti-Trop2 antibody drug conjugate, currently in Phase Ib/II clinical trials in patients with locally advanced/metastatic solid tumors, and ESG206, an anti-BAFFR monoclonal antibody, currently in Phase I study in subjects with B-cell Lymphoid Malignancies.
About Sorrento Therapeutics, Inc.
Sorrento is a clinical and commercial stage biopharmaceutical company developing new therapies to treat cancer, pain (non-opioid treatments), autoimmune disease, and COVID-19. Sorrento's multimodal, multipronged approach to fighting cancer is made possible by its extensive immuno-oncology platforms, including key assets such as next-generation tyrosine kinase inhibitors ("TKIs"), fully human antibodies (“G-MAB™ library”), immuno-cellular therapies (“DAR-T™”), antibody-drug conjugates (“ADCs”), and oncolytic virus (“Seprehvec™”). Sorrento is also developing potential antiviral therapies and vaccines against coronaviruses, including STI-1558 and COVI-MSC™, and diagnostic test solutions, including COVIMARK™.
Sorrento's commitment to life-enhancing therapies for patients is also demonstrated by our effort to advance a TRPV1 agonist, non-opioid pain management small molecule, resiniferatoxin (“RTX”), and SP-102 (10 mg, dexamethasone sodium phosphate viscous gel) (SEMDEXA™), a novel, viscous gel formulation of a widely used corticosteroid for epidural injections to treat lumbosacral radicular pain, or sciatica, and to commercialize ZTlido® (lidocaine topical system) 1.8% for the treatment of postherpetic neuralgia (PHN). RTX has been cleared for a Phase II trial for intractable pain associated with cancer and a Phase II trial in osteoarthritis patients. Positive final results from the Phase III Pivotal Trial C.L.E.A.R. Program for SEMDEXA™, its novel, non-opioid product for the treatment of lumbosacral radicular pain (sciatica), were announced in March 2022. ZTlido® was approved by the FDA on February 28, 2018.
For more information visit www.sorrentotherapeutics.com
Sorrento sees promising phase 2 results for abivertinib for lymphoma
Jul. 05, 2023 12:02 PM ET
Sorrento Therapeutics, Inc. (SRNEQ)JNJ, ABBV
By: Jonathan Block, SA News Editor2 Comments
- New phase 2a data from China found that Sorrento Therapeutics' (OTCPK:SRNEQ) abivertinib for marginal zone lymphoma achieved an overall response rate (ORR) of ~59%.
- https://seekingalpha.com/news/3985616-sorrento-promising-phase-2-results-abivertinib-lymphoma
- Sorrento Therapeutics, Inc. (SRNEQ)
- https://sorrentotherapeutics.com/
Elafibranor (GFT505)
Epcoritamab (DuoBody®-CD3xCD20)
Epcoritamab (DuoBody®-CD3xCD20)
Ipsen and GENFIT Announce Positive Results from Phase III ELATIVE® trial of elafibranor in patients with primary biliary cholangitis, a rare cholestatic liver disease
June 30, 2023
- Trial met primary endpoint with a statistically significant higher percentage of patients achieving a clinically meaningful cholestasis response compared to placebo
- Elafibranor was well tolerated with a safety profile consistent with previous studies
- Results position elafibranor as a potentially important new treatment option, where there is still high unmet need
- Ipsen intends to submit regulatory applications for elafibranor following discussions with the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA)
- GENFIT conference call (English and French) on June 30 at 8am ET / 1pm GMT / 2pm CET
Paris (France); June 30, 2023 - Ipsen (Euronext: IPN; ADR: IPSEY) and GENFIT (Nasdaq and Euronext: GNFT) today announced positive topline data from the pivotal ELATIVE® Phase III trial. In the trial the efficacy and safety of elafibranor, an investigational dual α,δ PPAR agonist, is being assessed for the treatment of patients with the rare cholestatic liver disease, primary biliary cholangitis (PBC), who have an inadequate response or intolerance to the current standard of care therapy, ursodeoxycholic acid (UDCA).
The trial met its primary composite endpoint, with 51% of patients on elafibranor 80mg achieving a cholestasis response compared with 4% on placebo (p<0.0001). Cholestasis response is defined in the trial as alkaline phosphatase (ALP) <1.67 x upper limit of normal (ULN), an ALP decrease ≥ 15 percent and total bilirubin (TB) ≤ ULN at 52 weeks. ALP and bilirubin are important predictors of disease progression. Reductions in levels of both can indicate reduced cholestatic injury and improved liver function.
The first secondary endpoint, normalization of ALP at Week 52, was also met with statistically significant improvements for investigational elafibranor compared with placebo. For the other secondary endpoint, a trend for pruritus improvement was observed with a greater decrease from baseline in the PBC Worst Itch NRS score for patients on elafibranor compared to placebo, which did not reach statistical significance. In the study, elafibranor was generally well tolerated with a safety profile consistent with that observed in previously reported studies.
“These are encouraging results that suggest elafibranor could be an effective treatment to prevent progression of PBC in patients who have received UDCA. It has a good safety profile and was well- tolerated, and could provide an important new therapeutic option for long-term treatment of patients with this debilitating condition,” said Howard Mayer, Executive Vice President and Head of Research and Development for Ipsen. “PBC is a serious condition which, if not treated properly, can lead to progression of liver disease and ultimately liver failure. We are excited about the potential of this investigational treatment and Ipsen now intends to discuss these results with regulatory agencies and plans to move forward with regulatory submissions to the U.S. Food and Drug Administration and the European Medicines Agency.”
“We are pleased by these results because PBC remains a disease where significant unmet medical needs exist”, added Pascal Prigent, Chief Executive Officer of GENFIT. “This long-awaited trial outcome is therefore good news for patients and for healthcare professionals who need more options to improve the clinical management of patients with PBC. It is also a gratifying recognition of the quality of our team’s work and of GENFIT’s ability to innovate and deliver tangible results.”
PBC is a rare, progressive, autoimmune cholestatic liver disease1 in which bile ducts in the liver are gradually destroyed. The damage to bile ducts can inhibit the liver’s ability to rid the body of toxins, and can lead to scarring of liver tissue, known as cirrhosis.1 Common symptoms of PBC include fatigue and pruritus (itch), which can be severely debilitating.1 Untreated, PBC can lead to liver failure, or in some cases death. It is also a leading cause of liver transplantation. It primarily affects middle-aged women, with nine women diagnosed for every man. It is a disease where a significant proportion of patients are unable to benefit from existing therapies. The prevalence of people living with PBC is estimated to be between 23.9-39.2 per 100,000 in the U. S23and 22.27 per 100,000 in Europe.4
ELATIVE® is a multi-center, randomized, double-blind, placebo-controlled Phase III clinical trial, with an open-label long-term extension (NCT03124108). ELATIVE® is evaluating the efficacy and safety of elafibranor 80mg once daily versus placebo for the treatment of patients with PBC with an inadequate response or intolerance to UDCA, the existing first-line therapy for PBC. The trial enrolled 161 patients who were randomized 2:1 to receive elafibranor 80mg once daily or placebo. Patients with an inadequate response to UDCA would continue to receive UDCA in combination with elafibranor or placebo, while patients unable to tolerate UDCA would receive only elafibranor or placebo.
Full data from the ELATIVE® trial will be presented at a future scientific congress.
GENFIT will host a conference call on June 30, 2023 at 8:00am ET / 1:00pm GMT / 2:00pm CET in English and in French
Both the English and French conference calls will be accessible on the investor page of our website, under the events section at https://ir.genfit.com/ or by calling 888-394-8218 (toll-free U.S. and Canada), 0800 279 0425 (toll-free UK) or 0805 101 219 (France) five minutes prior to the start time (confirmation code: 6752821). A replay will be available shortly after the call.
ABOUT ELAFIBRANOR
Elafibranor is a novel, oral, once-daily, dual peroxisome activated receptor (PPAR) alpha/delta (α,δ) agonist, currently under investigation as a treatment for patients with PBC, a rare liver disease. In 2019, it was granted a Breakthrough Therapy designation by the FDA in adults with PBC who have an inadequate response to ursodeoxycholic acid (UDCA). Elafibranor has not received approval by regulatory authorities anywhere in the world.
ABOUT IPSEN
Ipsen is a global, mid-sized biopharmaceutical company focused on transformative medicines in Oncology, Rare Disease and Neuroscience. With total sales of €3.0bn in FY 2022, Ipsen sells medicines in over 100 countries. Alongside its external-innovation strategy, the Company’s research and development efforts are focused on its innovative and differentiated technological platforms located in the heart of leading biotechnological and life-science hubs: Paris-Saclay, France; Oxford, U.K.; Cambridge, U.S.; Shanghai, China. Ipsen has around 5,400 colleagues worldwide and is listed in Paris (Euronext: IPN) and in the U.S. through a Sponsored Level I American Depositary Receipt program (ADR: IPSEY). For more information, visit ipsen.com
ABOUT GENFIT
GENFIT is a late-stage biopharmaceutical company dedicated to improving the lives of patients with rare and severe liver diseases characterized by high unmet medical needs. GENFIT is a pioneer in liver disease research and development with a rich history and strong scientific heritage spanning more than two decades. Thanks to its expertise in bringing early-stage assets with high potential to late development and pre-commercialization stages, today GENFIT boasts a growing and diversified pipeline of innovative therapeutic and diagnostic solutions. Its R&D pipeline covers six therapeutic areas via seven programs which explore the potential of differentiated mechanisms of action, across a variety of development stages (pre-clinical, Phase 1, Phase 2, Phase 3). These diseases are acute on-chronic liver failure (ACLF), hepatic encephalopathy (HE), cholangiocarcinoma (CCA), urea cycle disorders (UCD), organic acidemias (OA) and primary biliary cholangitis (PBC). Beyond therapeutics, GENFIT’s pipeline also includes a diagnostic franchise focused on NASH and ACLF. GENFIT has facilities in Lille and Paris (France), Zurich (Switzerland) and Cambridge, MA (USA). GENFIT is a publicly traded company listed on the Nasdaq Global Select Market and on compartment B of Euronext’s regulated market in Paris (Nasdaq and Euronext: GNFT). In 2021, IPSEN became one of GENFIT’s largest shareholders and holds 8% of the company’s share capital. For more information, visit www.genfit.com
Attachment
Genfit soars 23% as Phase 3 trial for liver disease candidate succeeds
Jun. 30, 2023 6:58 AM ET
Genfit S.A. (GNFT), IPSEY, IPSEF
By: Dulan Lokuwithana, SA News Editor
French biotech Genfit S.A. (NASDAQ:GNFT) added ~23% pre-market Friday after the company and its partner Ipsen (OTCPK:IPSEY) (OTCPK:IPSEF) announced that a Phase 3 trial for elafibranor targeted at the rare liver disease primary biliary cholangitis (PBC) reached the primary endpoint.
https://seekingalpha.com/news/3984392-genfit-stock-soars-on-liver-disease-drug
Genfit S.A. (GNFT), IPSEY, IPSEF
https://www.genfit.com/pipeline/elafibranor/clinical-overview/
Epcoritamab (DuoBody®-CD3xCD20)
Epcoritamab (DuoBody®-CD3xCD20)
Epcoritamab (DuoBody®-CD3xCD20)
June 27, 2023
AbbVie and Genmab Announce Positive Topline Results from Phase 1/2 EPCORE™ NHL-1 Trial Evaluating Epcoritamab (DuoBody®-CD3xCD20) in Patients with Relapsed/Refractory Follicular Lymphoma (FL)
- Based on the topline results of epcoritamab from the EPCORE™ NHL-1 clinical trial, AbbVie and Genmab will engage global regulatory authorities to discuss next steps
- Additional data from the clinical trial will be presented at a future medical meeting
- Follicular lymphoma is a common form of non-Hodgkin's lymphoma and currently has limited treatment options, particularly in the relapsed/refractory setting
NORTH CHICAGO, Ill., June 27, 2023 /PRNewswire/ -- AbbVie (NYSE: ABBV) and Genmab (Nasdaq: GMAB) today announced topline results from the follicular lymphoma (FL) cohort of the Phase 1/2 EPCORE™ NHL-1 clinical trial evaluating epcoritamab (DuoBody®-CD3xCD20), an investigational T-cell engaging bispecific antibody administered subcutaneously. The study cohort includes 128 adult patients with relapsed or refractory (R/R) FL who received at least two or more lines of systemic therapy. 70.3 percent of patients were double refractory to an anti-CD20 monoclonal antibody and an alkylating agent. Epcoritamab is being co-developed by AbbVie and Genmab as part of the companies' oncology collaboration.
"We are encouraged by these topline results, which further support the clinical profile of epcoritamab as a potential therapeutic option for patients with relapsed or refractory follicular lymphoma," said Mariana Cota Stirner, M.D., Ph.D., vice president, therapeutic area head for hematology, AbbVie. "Together with our partner Genmab, these results may bring us one step closer to our goal of advancing a potential core therapy for patients with B-cell malignancies."
EPCORE™ NHL-1 is an open-label trial evaluating the safety and preliminary efficacy of epcoritamab and consists of three parts: a Phase 1 first-in-human, dose escalation part; a Phase 2a expansion part; and a Phase 2a optimization part. The topline results from this cohort showed an overall response rate (ORR) of 82 percent as confirmed by an independent review committee (IRC), which exceeded the protocol prespecified threshold for efficacy. The observed median duration of response (DOR) was not reached, and longer follow-up will be required. The median number of lines of prior therapy in this cohort was three (range: two to nine lines of therapy).
No new safety signals were observed with epcoritamab in this study at the time of this analysis. The most common treatment-emergent adverse event was cytokine release syndrome (CRS) with 66.4 percent (1.6 percent Grade 3 or higher). The optimization part of the trial is continuing to evaluate alternative step-up dosing regimens to help further mitigate the risk of CRS, preliminary data are encouraging.
Full results from the study will be submitted for presentation at a future medical meeting.
About the Phase 1/2 EPCORE™ NHL-1 trial
EPCORE™ NHL-1 is an open-label, multi-center safety and preliminary efficacy trial of epcoritamab that consists of three parts: a Phase 1 first-in-human, dose escalation part; a Phase 2a expansion part; and a Phase 2a dose optimization part. The trial was designed to evaluate subcutaneous epcoritamab in adult patients with relapsed, progressive or refractory CD20+ mature B-cell non-Hodgkin's lymphoma (NHL), including follicular lymphoma (FL). In the Phase 2a expansion part, additional patients are being enrolled to further explore the safety and efficacy of epcoritamab in three cohorts of patients with different types of relapsed or refractory (R/R) B-cell NHLs who have limited therapeutic options. The dose optimization part evaluates the potential for alternative step-up dosing regimens to help further minimize Grade 2 CRS and mitigate Grade ≥3 cytokine release syndrome. The primary endpoint of the expansion part was overall response rate as assessed by an independent review committee. Secondary efficacy endpoints included duration of response, complete response rate, duration of complete response, progression-free survival, and time to response as determined by the Lugano criteria. Overall survival, time to next therapy, and rate of minimal residual disease negativity were evaluated as secondary efficacy endpoints.
About Follicular Lymphoma
Follicular lymphoma (FL) is typically an indolent, or slow growing, form of NHL that arises from B-cell lymphocytes.1 FL is the second most common form of NHL overall, accounting for 20 to 30 percent of all NHL cases, and representing 10 to 20 percent of all lymphomas in the western world.2,3 Although FL is an indolent lymphoma, it is considered incurable with conventional therapy.4,5
About Epcoritamab
Epcoritamab is an investigational IgG1-bispecific antibody created using Genmab's proprietary DuoBody® technology and administered subcutaneously. Genmab's DuoBody-CD3 technology is designed to direct cytotoxic T cells selectively to elicit an immune response toward target cell types. Epcoritamab is designed to simultaneously bind to CD3 on T cells and CD20 on B-cells and induces T cell mediated killing of CD20+ cells.6
Epcoritamab-bysp (EPKINLY™) was recently approved in the United States (U.S.) and is indicated for the treatment of adult patients with R/R diffuse large B-cell lymphoma (DLBCL), not otherwise specified (NOS), including DLBCL arising from indolent lymphoma, and high-grade B-cell lymphoma (HGBL) after two or more lines of systemic therapy. This indication is approved under accelerated approval based on response rate and durability of response. Continued approval for this indication is contingent upon verification and description of clinical benefit in a confirmatory trial(s). Please see U.S. Important Safety Information below.
In October 2022, a Marketing Authorization Application was submitted for epcoritamab for the treatment of patients with R/R DLBCL after two or more lines of systemic therapy, which was validated by the European Medicines Agency. Additionally, in December 2022, a Japan new drug application was submitted to the Ministry of Health, Labor and Welfare of Japan for epcoritamab for the treatment of patients with R/R large B-cell lymphoma (LBCL) after two or more lines of systemic therapy. Epcoritamab is not approved in the European Union and Japan.
The companies will share commercial responsibilities in the United States and Japan, with AbbVie responsible for further global commercialization. AbbVie will continue to pursue regulatory submissions for epcoritamab across international markets excluding the United States and Japan throughout the year.
Genmab and AbbVie are continuing to evaluate the use of epcoritamab as a monotherapy, and in combination, across lines of therapy in a range of hematologic malignancies. This includes an ongoing Phase 3, open-label, randomized trial evaluating epcoritamab as a monotherapy in patients with R/R DLBCL (NCT: 04628494), an ongoing Phase 3, open-label, randomized trial evaluating epcoritamab in combination in adult participants with newly diagnosed DLBCL (NCT: 05578976), and a Phase 3, open-label clinical trial evaluating epcoritamab in combination in patients with R/R FL (NCT: 05409066). Epcoritamab is not approved to treat newly diagnosed patients with DLBCL or FL. The safety and efficacy of epcoritamab has not been established for these investigational uses. Please visit clinicaltrials.gov for more information.
EPKINLY™ (epcoritamab-bysp) U.S. IMPORTANT SAFETY INFORMATION
Please see the Full Prescribing Information and Medication Guide, including Important Warnings.
About AbbVie in Oncology
At AbbVie, we are committed to transforming standards of care for multiple blood cancers while advancing a dynamic pipeline of investigational therapies across a range of cancer types. Our dedicated and experienced team joins forces with innovative partners to accelerate the delivery of potential breakthrough medicines. We are evaluating more than 20 investigational medicines in over 300 clinical trials across some of the world's most widespread and debilitating cancers. As we work to have a remarkable impact on people's lives, we are committed to exploring solutions to help patients obtain access to our cancer medicines. For more information, please visit http://www.abbvie.com/oncology.
About AbbVie
AbbVie's mission is to discover and deliver innovative medicines that solve serious health issues today and address the medical challenges of tomorrow. We strive to have a remarkable impact on people's lives across several key therapeutic areas: immunology, oncology, neuroscience, eye care, virology and gastroenterology, in addition to products and services across our Allergan Aesthetics portfolio. For more information about AbbVie, please visit us at www.abbvie.com. Follow @abbvie on Twitter, Facebook, Instagram, YouTube and LinkedIn.
ABBV Dividend History
https://www.nasdaq.com/market-activity/stocks/abbv/dividend-history
biotecHOPE™ 2023
NGENLA (somatrogon-ghla)
NGENLA (somatrogon-ghla)
NGENLA (somatrogon-ghla)
FDA Approves Pfizer’s NGENLA™, a Long-Acting Once-Weekly Treatment for Pediatric Growth Hormone Deficiency
Wednesday, June 28, 2023 - 06:45am
New, longer-acting treatment offers option to reduce the frequency of injections for children with growth hormone deficiency from daily to once-weekly
NEW YORK & MIAMI--(BUSINESS WIRE)-- Pfizer Inc. (NYSE: PFE) and OPKO Health Inc. (NASDAQ: OPK) announced today that the U.S. Food and Drug Administration (FDA) has approved NGENLA (somatrogon-ghla), a once-weekly, human growth hormone analog indicated for treatment of pediatric patients aged three years and older who have growth failure due to inadequate secretion of endogenous growth hormone. NGENLA is expected to become available for U.S. prescribing in August 2023.
Growth hormone deficiency (GHD) is a rare disease characterized by the inadequate secretion of the growth hormone somatropin from the pituitary gland, affecting one in approximately 4,000 to 10,000 children.1,2 Without treatment, children will have persistent growth attenuation, a very short height in adulthood, and puberty may be delayed.1,2,3 Children living with GHD may also experience challenges in relation to their physical health and mental well-being.1,2,3
“For more than 30 years, Pfizer has been committed to supporting children and adults living with growth hormone deficiency, beginning with the delivery of a medicine that has long been a part of the standard of care,” said Angela Hwang, Chief Commercial Officer, President, Global Biopharmaceuticals Business, Pfizer. “We are excited to bring this next-generation treatment to patients in the United States, continuing our commitment to helping children living with this rare growth disorder reach their full potential.”
The FDA approval is supported by results from a multi-center, randomized, open-label, active-controlled Phase 3 study which evaluated the safety and efficacy of NGENLA when administered once-weekly compared to once-daily somatropin. The study met its primary endpoint of NGENLA non-inferiority compared to somatropin, as measured by annual height velocity at 12 months. NGENLA was generally well tolerated in the study and had a safety profile comparable to somatropin.
“The approval of NGENLA will be significant for children with growth hormone deficiency in the U.S. It holds potential to reduce the treatment burden that can come with daily growth hormone injections,” said Joel Steelman, M.D., Pediatric Endocrinologist, Cook Children’s Health Care System. “As a new, longer-acting option that has the ability to reduce treatment frequency from daily to weekly, NGENLA could become an important treatment option that can improve adherence for children being treated for growth hormone deficiency.”
“Throughout our collaboration with Pfizer, we have worked tirelessly toward our shared goal of helping children living with growth hormone disease and their families,” said Phillip Frost, M.D., Chairman and Chief Executive Officer, OPKO Health. “We are proud of the clinical development program that supported the FDA approval of NGENLA and are excited about its potential for these patients and their families as it becomes available in the United States.”
NGENLA is approved for the treatment of pediatric GHD in more than 40 markets including Canada, Australia, Japan, and EU Member States.
The full Prescribing Information can be found here. If it is not currently available via this link, it will be visible as soon as possible as we work to finalize the document. Please check back for the full information shortly.
About NGENLA(somatrogon-ghla) Injection
NGENLA (somatrogon-ghla) is a human growth hormone that works by replacing the lack of growth hormone in the body. NGENLA is taken by injection just below the skin, administered via a device that allows for titration based on patient need. Compared to the growth hormone GENOTROPIN® (somatropin), its action in the body lasts longer, enabling weekly injections instead of daily.
In 2014, Pfizer and OPKO entered into a worldwide agreement for the development and commercialization of NGENLA for the treatment of GHD. Under the agreement, OPKO is responsible for conducting the clinical program and Pfizer is responsible for registering and commercializing NGENLA for GHD.
About the NGENLA Clinical Program
The safety and efficacy of NGENLA (somatrogon-ghla) was demonstrated in a multi-center, randomized, open-label, active-controlled Phase 3 study (NCT 02968004). The Phase 3 study enrolled and treated 224 pediatric patients, treatment-naïve children with growth hormone deficiency who were randomized 1:1 into two arms: NGENLA (somatrogon-ghla) once-weekly at a dose of 0.66 mg/kg/day vs somatropin, once-daily at a dose of 0.034 mg/kg/day. The study met its primary endpoint of NGENLA non-inferiority compared to somatropin, measured by annual height velocity at 12 months.
About Growth Hormone Deficiency
Growth hormone deficiency is a rare disease characterized by the inadequate secretion of growth hormone from the pituitary gland and affects one in approximately 4,000 to 10,000 children.1,2 In children, this disease can be caused by genetic mutations or acquired after birth.1,4 Because the patient's pituitary gland secretes inadequate levels of somatropin, the hormone that causes growth, a child’s height may be affected and puberty may be delayed.1,2,5 Without treatment, affected children will have persistent growth attenuation and a very short height in adulthood.1,2 Children may also experience challenges in relation to physical health and mental well-being.1,2
Important NGENLA (somatrogon-ghla) Safety Information
- Growth hormone should not be used in children after the growth plates have closed.
- Growth hormone should not be used in children with some types of eye problems caused by diabetes (diabetic retinopathy).
- Growth hormone should not be used in children who have cancer or other tumors.
- Growth hormone should not be used in children who are critically ill because of some types of heart or stomach surgery, trauma, or breathing (respiratory) problems.
- Growth hormone should not be used in children with Prader-Willi syndrome who are very overweight or have breathing problems including sleep apnea.
- NGENLA should not be used by children who have had an allergic reaction to somatrogon-ghla or any of the ingredients in NGENLA. Look for prompt medical attention in case of an allergic reaction.
- Some children have developed diabetes mellitus while taking growth hormone. Dosages of diabetes medicines may need to be adjusted during treatment with NGENLA. Children should be watched carefully if NGENLA is given along with glucocorticoid therapy and/or other drugs that are processed by the body in the same way.
- In childhood cancer survivors, treatment with growth hormone may raise the likelihood of a new tumor, particularly some benign (non-cancerous) brain tumors. This likelihood may be higher in children who were treated with radiation to the brain or head. Your child’s health care provider will need to check your child for a return of cancer or a tumor.
- Children treated with growth hormone have had increased pressure in the brain. If your child has headaches, eye problems, nausea (feeling like you are going to be sick), or vomiting, contact your child’s health care provider.
- NGENLA may decrease thyroid hormone levels. Decreased thyroid hormone levels may change how well NGENLA works. Your child’s health care provider will do blood tests to check your child’s hormone levels.
- Children treated with growth hormone should be checked regularly for low serum cortisol levels and/or the need to increase the dose of the glucocorticoids they are taking.
- In children experiencing fast growth, curvature of the spine may develop or worsen. This is also called scoliosis. Children with scoliosis should be checked regularly to make sure their scoliosis does not get worse during their growth hormone therapy.
- Use a different area on the body for each injection. This can help to avoid skin problems such as lumpiness or soreness.
- Growth hormone treatment may cause serious and constant stomach (abdominal) pain. This could be a sign of pancreatitis. Tell your child’s health care provider if your child has any new stomach (abdominal) pain.
- In studies of NGENLA in children with GHD, side effects included injection site reactions such as pain, swelling, rash, itching, or bleeding. Other side effects were the common cold, headache, fever (high temperature), low red blood cells (anemia), cough, vomiting, decreased thyroid hormone levels, stomach pain, rash, or throat pain.
- A health care provider will help you with the first injection. He or she will also train you on how to inject NGENLA.
- Rx only
About GENOTROPIN(somatropin)
GENOTROPIN is a man-made, prescription treatment option. The indications GENOTROPIN is approved for vary by market. GENOTROPIN is approved for growth failure due to GHD and adult GHD, Prader-Willi Syndrome, Idiopathic Short Stature, Turner Syndrome, Small for Gestational Age (with no catch-up growth), and Chronic Renal Insufficiency. GENOTROPIN is taken by injection just below the skin and is available in a wide range of devices to fit a range of individual dosing needs. GENOTROPIN is just like the natural growth hormone that our bodies make and has an established safety profile.
Important GENOTROPIN (somatropin) Safety Information
- Somatropin should not be used for growth promotion in pediatric patients with closed epiphyses.
- Somatropin is contraindicated in patients with active proliferative or severe nonproliferative diabetic retinopathy.
- Somatropin is contraindicated in patients with active malignancy. Because growth hormone deficiency may be a sign of pituitary or other brain tumors, the presence of such tumors should be ruled out before treatment is initiated. Somatropin should not be used in patients with any evidence of progression or recurrence of an underlying intracranial tumor.
- Somatropin in pharmacologic doses should not be used to treat patients with acute critical illness due to complications from open heart surgery, abdominal surgery or multiple accidental traumas, or those patients with acute respiratory failure due to an increased mortality. The safety of continuing replacement somatropin treatment for approved uses in patients who develop these illnesses has not been established.
- Somatropin is contraindicated in patients with Prader-Willi syndrome who are severely obese or have respiratory impairment.
- GENOTROPIN is contraindicated in patients with a known hypersensitivity to somatropin or any of its excipients. Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropin products. Patients and caregivers should be informed that such reactions are possible and that prompt medical attention should be sought if an allergic reaction occurs.
- New-onset Type-2 diabetes mellitus has been reported. Monitor patients with glucose intolerance closely; dosage of antihyperglycemic drug may need to be adjusted. Monitor carefully if somatropin is administered in combination with glucocorticoid therapy and/or other drugs metabolized by the CP450 pathway.
- In childhood cancer survivors, an increased risk of a second neoplasm, in particular meningiomas, has been reported in patients treated with somatropin after their first neoplasm, particularly those who were treated with cranial radiation. Children with certain rare genetic causes of short stature have an increased risk of developing malignancies. Practitioners should thoroughly consider the risks and benefits of starting somatropin in these patients and if treatment is initiated, should carefully monitor these patients for development of neoplasms. Patients should be monitored carefully for any malignant transformation of skin lesions.
- Intracranial hypertension (IH) has been reported in a small number of patients treated with somatropin. If papilledema is observed during somatropin treatment, treatment should be stopped and reassessed. Patients with Turner syndrome and Prader-Willi syndrome may be at increased risk for the development of IH.
- Undiagnosed/untreated hypothyroidism may prevent an optimal response to somatropin, in particular, the growth response in children. Patients with Turner syndrome have an inherently increased risk of developing autoimmune thyroid disease and primary hypothyroidism. In patients with growth hormone deficiency, central (secondary) hypothyroidism may first become evident or worsen during somatropin treatment. Therefore, patients treated with somatropin should have periodic thyroid function tests, and thyroid hormone replacement therapy should be initiated or appropriately adjusted when indicated.
- Patients treated with somatropin who have or are at risk for pituitary hormone deficiency(s) may be at risk for reduced serum cortisol levels and/or unmasking central hypoadrenalism and should be monitored for reduced serum cortisol levels. In addition, patients treated with glucocorticoid replacement for pre-existing hypoadrenalism may require an increase in their maintenance or stress doses following initiation of somatropin treatment and should be monitored for reduced cortisol levels and/or need for glucocorticoid dose increases.
- Progression of scoliosis can occur in patients who experience rapid growth. Patients with scoliosis should be monitored for manifestation or progression during somatropin therapy.
- Slipped capital femoral epiphyses may occur more frequently in patients with endocrine disorders (including GHD and Turner syndrome) or in patients undergoing rapid growth. Any pediatric patient with the onset of a limp or complaints of hip or knee pain during somatropin therapy should be carefully evaluated.
- Somatropin should be used during pregnancy only if clearly needed and with caution in nursing mothers because it is not known whether somatropin is excreted in human milk.
- Subcutaneous injection of somatropin at the same site repeatedly may result in tissue atrophy. This can be avoided by rotating the injection site.
- Cases of pancreatitis have been reported rarely in children and adults receiving somatropin treatment, with some evidence supporting a greater risk in children compared with adults. Published literature indicates that girls who have Turner syndrome may be at greater risk than other somatropin-treated children. Pancreatitis should be considered in any somatropin-treated patient, especially a child, who develops persistent severe abdominal pain.
- In clinical trials with GENOTROPIN in pediatric GHD patients, the following events were reported infrequently: injection site reactions, including pain or burning associated with the injection, fibrosis, nodules, rash, inflammation, pigmentation, or bleeding; lipoatrophy; headache; hematuria; hypothyroidism; and mild hyperglycemia.
- In clinical studies of 273 pediatric patients born SGA treated with GENOTROPIN, the following clinically significant events were reported: mild transient hyperglycemia; 1 patient with benign intracranial hypertension; 2 patients with central precocious puberty; 2 patients with jaw prominence; and several patients with aggravation of preexisting scoliosis, injection site reactions, and self-limited progression of pigmented nevi. Anti-hGH antibodies were not detected in any of the patients treated with GENOTROPIN.
- Deaths have been reported with the use of a growth hormone in pediatric PWS patients with severe obesity, history of upper airway obstruction or sleep apnea, and/or unidentified respiratory infection. Therefore, all patients with PWS should be evaluated and monitored for signs of upper airway obstruction, sleep apnea, and respiratory infections, and have effective weight control.
- In clinical trials with GENOTROPIN in pediatric patients with PWS, the following drug-related events were reported: edema, aggressiveness, arthralgia, benign intracranial hypertension, hair loss, headache, and myalgia.
- Somatropin may increase the occurrence of otitis media in Turner syndrome patients. In 2 clinical studies with GENOTROPIN in pediatric patients with Turner syndrome, the most frequently reported adverse events were respiratory illnesses (influenza, tonsillitis, otitis, sinusitis), joint pain, and urinary tract infection. The only treatment-related adverse event that occurred in more than 1 patient was joint pain.
- In 2 clinical studies with GENOTROPIN in pediatric patients with ISS, the most commonly encountered adverse events included upper respiratory tract infections, influenza, tonsillitis, nasopharyngitis, gastroenteritis, headaches, increased appetite, pyrexia, fracture, altered mood, and arthralgia.
- In clinical trials with GENOTROPIN in adults with GHD, the majority of side effects were symptoms of fluid retention, including peripheral swelling/edema, arthralgia, pain and stiffness of the extremities, myalgia, paresthesia, and hypoesthesia. Generally, these were transient and dose-dependent.
- In women on oral estrogen replacement, a larger dose of somatropin may be required to achieve the defined treatment goal.
- Elderly patients may be more sensitive to the action of somatropin, and therefore may be more prone to develop adverse reactions.
- The cartridges of GENOTROPIN contain m-Cresol and should not be used by patients with a known sensitivity to this preservative.
- Subcutaneous injection of somatropin at the same site repeatedly may result in tissue atrophy. This can be avoided by rotating the injection site.
- Health care providers should supervise the first injection and provide appropriate training and instruction for the proper use of all devices for GENOTROPIN.
- Rx only
For the full Prescribing Information for GENOTROPIN, please visit http://labeling.pfizer.com/ShowLabeling.aspx?id=577.
Pfizer Inc.: Breakthroughs that Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety, and value in the discovery, development, and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments, and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world's premier innovative biopharmaceutical companies, we collaborate with health care providers, governments, and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.pfizer.com. In addition, to learn more, please visit us on www.pfizer.com and follow us on Twitter at @Pfizer and @Pfizer_News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
About OPKO Health
OPKO is a multinational biopharmaceutical and diagnostics company that seeks to establish industry-leading positions in large, rapidly growing markets by leveraging its discovery, development, and commercialization expertise and novel and proprietary technologies. For more information, visit www.opko.com.
Source: Pfizer Inc.
Pfizer, OPKO Health win FDA nod for dwarfism therapy
Jun. 28, 2023 7:35 AM ET
By: Dulan Lokuwithana, SA News Editor1 Comment
- Pfizer (NYSE:PFE) and OPKO Health (OPK) announced Wednesday the FDA approval of Ngenla, a once-weekly human growth hormone analog for children with growth hormone deficiency, commonly known as dwarfism.
- Specifically, the FDA approval for Ngenla (somatrogon-ghla) allows its use in children aged three years and older whose growth failure is caused by insufficient production of growth hormone. The companies expect to launch Ngenla for the U.S. market in August 2023.
- https://seekingalpha.com/news/3983563-pfizer-opko-health-win-fda-nod-dwarfism-therapy
- Pfizer Inc. (PFE)OPK
- https://www.pfizer.com/
- https://www.opko.com/what-we-do/our-research/somatrogon
ACI-24.060
NGENLA (somatrogon-ghla)
NGENLA (somatrogon-ghla)
AC Immune Receives FDA Fast Track Designation For Anti-Amyloid-Beta Active Immunotherapy, ACI-24.060, To Treat Alzheimer’s Disease
Jun 27, 2023
AC Immune Receives FDA Fast Track Designation for Anti-Amyloid-beta Active Immunotherapy, ACI-24.060, to Treat Alzheimer’s Disease
- Ongoing Phase 1b/2 ABATE study enrolling well and expanding to sites in USA with Investigational New Drug (IND) clearance for ACI-24.060
- Dosed first individual with Down syndrome (DS) in the DS cohort of ABATE
- Interim safety and immunogenicity data in Alzheimer’s disease (AD) and DS cohorts expected in H2 2023
- Initial PET data on amyloid plaque reduction in AD expected H1 2024
Lausanne, Switzerland, June 27, 2023 – AC Immune SA (NASDAQ: ACIU), a clinical-stage biopharmaceutical company pioneering precision medicine for neurodegenerative diseases, today announced that it has received Fast Track designation from the U.S. Food and Drug Administration (FDA) for its wholly-owned anti-amyloid beta (Abeta) active immunotherapy (vaccine)-candidate, ACI-24.060, for treatment of Alzheimer’s disease. This follows FDA clearance of the Investigational New Drug (IND) application enabling expansion to the USA of the ongoing Phase 1b/2 ABATE study of ACI-24.060 in patients with AD and individuals with DS. Furthermore, the first individual with DS has been dosed in ABATE.
Dr. Andrea Pfeifer, CEO of AC Immune SA, commented: “We are delighted to see the quality and importance of our ACI-24.060 program reflected in the granting of Fast Track designation, which offers opportunities for expedited development and regulatory review. This regulatory progress underscores the attraction of an active immunotherapy targeting toxic species of Abeta. By inducing a polyclonal response including antibodies against both oligomeric Abeta and pyroglutamate-Abeta, ACI-24.060 targets the same toxic species as disease modifying anti-Abeta monoclonal antibodies that slowed AD progression in Phase 3 clinical trials. As ACI-24.060, created using our SupraAntigen® platform, specifically targets the most toxic forms of Abeta, we believe it may offer best-in-class efficacy with all the potential advantages in safety, administration and distribution that can be expected from a vaccine. We look forward to showing in H1 2024 the effect of ACI-24.060 on amyloid plaque reduction, a surrogate marker for disease modification.”
ACI-24.060’s Fast Track designation and IND clearance, as well as the expansion of ABATE to include individuals with DS were supported by positive initial interim safety and immunogenicity data from ABATE’s first, low dose AD cohort. Dosing in a second, higher dose AD cohort began earlier this year.
Dr. Johannes Streffer, CMO of AC Immune SA, commented: “ABATE’s expansion into the USA will allow us to accelerate the trial’s advancement and build upon the strong momentum we’ve generated in Europe. With today’s announcement, we remain firmly on track to report additional interim safety and immunogenicity data later this year, and for the crucial interim readout of Abeta-PET imaging data in AD in the first half of next year. By benchmarking the amount of Abeta plaque reduction achieved with ACI-24.060 against those achieved with FDA-approved monoclonal antibodies, we believe we can generate early evidence of our vaccine’s therapeutic potential to support its expeditious advancement towards pivotal programs in AD and DS-related AD.”
Dr. Michael Rafii, Medical Director of the Alzheimer’s Therapeutic Research Institute, Professor of Neurology at the Keck School of Medicine, and the Principal Investigator of the trial commented: “Despite representing the world’s largest population that is genetically at high risk for AD, individuals with DS are vastly underserved and underrepresented in clinical trials. I applaud AC Immune for seeking to address the urgent needs of this population and believe ACI-24.060 holds great promise as a novel therapy that can lower Abeta plaques to delay, or perhaps even prevent, the onset of clinical dementia symptoms in AD and DS-related AD. Moreover, I believe the potential safety, efficacy, and logistical advantages of a vaccine over monoclonal antibodies strongly support the development of therapeutics such as ACI-24.060 as the next generation of anti-Abeta therapies.”
About the Phase 1b/2 ABATE Study (ClinicalTrials.gov Identifier: NCT05462106)
The ABATE study is a Phase 1b/2, multicenter, adaptive, double-blind, randomized, placebo-controlled study to assess the safety, tolerability, immunogenicity, and pharmacodynamic effects of ACI-24.060 in subjects with prodromal Alzheimer’s disease and in adults with Down syndrome. All participants in the trial must have brain Abeta pathology confirmed by a positron emission tomography (PET) scan. Recent clinical studies and FDA approvals have validated Abeta as a disease modifying therapeutic target in AD and are supportive of Abeta PET imaging as a surrogate marker of efficacy. The trial begins with a dose escalation phase in AD patients, during which various doses/dosing regimens may be evaluated, and also includes individuals with DS.
About AD in Down syndrome
Individuals with Down syndrome (DS) have a third copy of all or part of chromosome 21, which contains the gene that codes for amyloid-precursor protein (APP). Overproduction of APP is believed to cause the accumulation of Abeta plaques. Virtually all individuals with DS will develop Abeta plaques and AD1, with DS-related AD sharing a similar pathophysiology and biomarkers with other forms of genetic AD. Given the more predictable onset and progression of symptoms in DS-related AD, AC Immune believes ABATE’s results will offer crucial insights into the ability of ACI-24.060 active immunotherapy to modulate neurodegeneration at its earliest stages and offer this population a much needed therapeutic option.
About ACI-24.060
ACI-24.060, derived from AC Immune’s SupraAntigen® platform, has been shown in preclinical studies to induce a strong polyclonal antibody response that matures and is maintained against both oligomeric and pyroglutamate-Abeta species, key pathological forms of Abeta believed to drive Abeta plaque formation and disease progression. ACI-24.060 is designed to enhance the formation of broad-spectrum protective antibodies with the same safety and tolerability previously demonstrated in the ACI-24 program in Phase 1 and 2 trials. This investigational candidate has the potential to efficiently inhibit plaque formation and increase plaque clearance, and thereby may reduce or prevent disease progression.
Reference
- Lott, Ira T., and Elizabeth Head. "Dementia in Down syndrome: unique insights for Alzheimer disease research." Nature Reviews Neurology 15.3 (2019): 135-147.
About AC Immune SA
AC Immune SA is a clinical-stage biopharmaceutical company that aims to become a global leader in precision medicine for neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and NeuroOrphan indications driven by misfolded proteins. The Company’s two clinically validated technology platforms, SupraAntigen® and Morphomer®, fuel its broad and diversified pipeline of first- and best-in-class assets, which currently features ten therapeutic and three diagnostic candidates, five of which are currently in Phase 2 clinical trials and one of which is in Phase 3. AC Immune has a strong track record of securing strategic partnerships with leading global pharmaceutical companies including Genentech, a member of the Roche Group, Eli Lilly and Company, and others, resulting in substantial non-dilutive funding to advance its proprietary programs and >$3 billion in potential milestone payments.
SupraAntigen® is a registered trademark of AC Immune SA in the following territories: AU, EU, CH, GB, JP, RU, SG and USA. Morphomer® is a registered trademark of AC Immune SA in CN, CH, GB, JP, KR, NO and RU.
The information on our website and any other websites referenced herein is expressly not incorporated by reference into, and does not constitute a part of, this press release.
Attachment

![]()
Source: AC Immune SA
AC Immune gains 14% on FDA fast track tag for Alzheimer’s vaccine
Jun. 27, 2023 8:44 AM ET
By: Dulan Lokuwithana, SA News Editor
Swiss biotech AC Immune SA (NASDAQ:ACIU) added ~14% pre-market Tuesday after announcing that the FDA issued Fast Track designation for its anti-amyloid vaccine ACI-24.060 as a treatment for Alzheimer’s disease (AD).
The FDA offers the Fast Track designation to accelerate the development and review of drugs targeted at serious conditions with unmet medical needs. Companies with Fast Track Designations, subject to conditions, can secure the FDA’s Accelerated Approval and Priority Review, enabling patients to access those treatments sooner.
Previously, the FDA had cleared AC Immune’s (ACIU) Investigational New Drug (IND) application for ACI-24.060, allowing the company to expand its ongoing Phase 1b/2 ABATE study in the U.S. for patients with AD and Down syndrome.
https://seekingalpha.com/news/3983125-ac-immune-wins-fda-fast-track-tag-alzheimers-shot
Pombiliti® + Opfolda®
NGENLA (somatrogon-ghla)
Pombiliti® + Opfolda®
Amicus Therapeutics Announces Approval and Launch of New Pompe Disease Therapy in the European Union
June 27, 2023 at 7:00 AM EDT
Pombiliti® (cipaglucosidase alfa) + Opfolda® (miglustat) Now Approved in the European Union for Adults with Late-onset Pompe Disease (LOPD)
PHILADELPHIA, June 27, 2023 (GLOBE NEWSWIRE) -- Amicus Therapeutics (Nasdaq: FOLD), a patient-dedicated global biotechnology company focused on developing and commercializing novel medicines for rare diseases, today announced that the European Commission (EC) has granted approval for Opfolda® (miglustat) 65mg capsules, an enzyme stabilizer of cipaglucosidase alfa, a long-term enzyme replacement therapy for adults with late-onset Pompe disease. Pombiliti® (cipaglucosidase alfa) was previously approved by the EC in March 2023. Pompe disease is an inherited lysosomal disorder caused by deficiency of the enzyme acid α-glucosidase (GAA). Amicus plans to immediately launch Pombiliti + Opfolda in Germany and is commencing reimbursement processes with healthcare authorities in other European countries.
“Late-onset Pompe disease is a rare, neuromuscular disorder that can have devastating consequences for patients and their families. The European Commission approval for Pombiliti and Opfolda is the realization of the work of so many individuals and teams dedicated to the mission of improving the lives of people living with Pompe disease. We look forward to bringing this much needed, new treatment to all adults living in the EU with late-onset Pompe disease,” said John F. Crowley, Executive Chairman of Amicus Therapeutics, Inc.
"We are extremely pleased with the EC approval of Pombiliti and Opfolda, and are grateful to the Pompe community around the world who have helped advance this therapy. Given the strength of the label and our launch readiness, we believe Pombiliti and Opfolda has the potential to become the next standard of care in this devastating condition by showing that improvement is possible for people living with late-onset Pompe disease,” said Bradley Campbell, President and Chief Executive Officer of Amicus Therapeutics, Inc.
Pombiliti + Opfolda is a unique two-component therapy. Pombiliti (cipaglucosidase alfa), is a bis-M6P-enriched rhGAA enzyme, designed for increased uptake into muscle cells. Once in the cell, Pombiliti can be processed into its most active and mature form to break down glycogen. Opfolda (miglustat) is an enzyme stabilizer designed to stabilize the enzyme in the blood. The EC approval was based on clinical data from the Phase 3 pivotal study (PROPEL), the only trial in LOPD to study the real-world population of both ERT-naïve and ERT-experienced participants in a controlled setting.
“This significant milestone marks the beginning of broad access to Pombiliti and Opfolda for the LOPD community in Europe, where there is a high medical need for novel treatment options,” said Prof. Benedikt Schoser, Professor of Neurology at Ludwig-Maximilians-University of Munich LMU Department of Neurology. “In clinical studies, Pombiliti and Opfolda have exhibited clinically meaningful and positive changes in the key mobility and respiratory manifestations of this challenging disease. The EC approval and indication reflect the hope for the potential of this innovative therapy for people living with Pompe disease.”
“The Pompe community is greatly appreciative of Amicus’ long-standing commitment to develop a treatment option to address the continuing unmet needs of people living with late-onset disease. Each person deserves alternatives to help them best manage their condition,” said Tiffany House, President, International Pompe Association.
In the U.K., the Medicines and Healthcare products Regulatory Agency (MHRA) regulatory approval is expected in the third quarter of 2023. The U.S. Food and Drug Administration’s review is ongoing, and the Company expects approval in the third quarter of 2023. The FDA previously granted Breakthrough Therapy designation for Pombiliti + Opfolda.
About Pombiliti® + Opfolda®
Pombiliti + Opfolda, is a two-component therapy that consists of cipaglucosidase alfa, a bis-M6P-enriched rhGAA that facilitates high-affinity uptake through the M6P receptor while retaining its capacity for processing into the most active form of the enzyme, and the oral enzyme stabilizer, miglustat, that’s designed to reduce loss of enzyme activity in the blood. In clinical studies, Pombiliti + Opfolda was associated with demonstrated improvements in both musculoskeletal and respiratory measures.
About Pompe Disease
Pompe disease is an inherited lysosomal disorder caused by deficiency of the enzyme acid alpha-glucosidase (GAA). Reduced or absent levels of GAA lead to accumulation of glycogen in cells, which is believed to result in the clinical manifestations of Pompe disease. Pompe disease ranges from a rapidly deteriorating infantile form with significant impact to heart function, to a more slowly progressive, late-onset form primarily affecting skeletal muscle and progressive respiratory involvement. Late-onset Pompe disease can be severe and debilitating with progressive muscle weakness throughout the body that worsens over time, particularly skeletal muscles and muscles controlling breathing.
About Amicus Therapeutics
Amicus Therapeutics (Nasdaq: FOLD) is a global, patient-dedicated biotechnology company focused on discovering, developing and delivering novel high-quality medicines for people living with rare diseases. With extraordinary patient focus, Amicus Therapeutics is committed to advancing and expanding a pipeline of cutting-edge, first- or best-in-class medicines for rare diseases. For more information please visit the company’s website at www.amicusrx.com, and follow on Twitter and LinkedIn.
Amicus Therapeutics wins EC approval of Opfolda for Pompe disease
Jun. 26, 2023 3:24 PM ET
Amicus Therapeutics, Inc. (FOLD)
By: Jonathan Block, SA News Editor
- The European Commission has granted marketing authorization to Amicus Therapeutics' Opfolda (miglustat) for late-onset Pompe disease.
- Miglustat, an oral enzyme stabilizer, is intended to be used in combination with Pombiliti (cipaglucosidase alfa), a long-term enzyme replacement therapy that won EC approval in March.
- https://seekingalpha.com/news/3982942-amicus-therapeutics-wins-ec-approval-opfolda-pompe-disease
- Amicus Therapeutics, Inc. (FOLD)
- https://amicusrx.com/
- https://amicusrx.com/products/pombiliti-opfolda/
KT-253
VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection
Pombiliti® + Opfolda®
Kymera Therapeutics Receives FDA Orphan Drug Designation for KT-253, a Novel, Highly Potent and Selective MDM2 Degrader for the Treatment of Acute Myeloid Leukemia
Jun 22, 2023< Go BackDownload PDF
WATERTOWN, Mass., June 22, 2023 (GLOBE NEWSWIRE) -- Kymera Therapeutics, Inc. (NASDAQ: KYMR), a clinical-stage biopharmaceutical company advancing targeted protein degradation to deliver novel small molecule protein degrader medicines, today announced that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation to KT-253 for the treatment of Acute Myeloid Leukemia (AML).
KT-253 is a highly potent and selective degrader that targets MDM2, the crucial regulator of the most common tumor suppressor, p53. p53 remains intact (wild type) in close to 50% of cancers, meaning that it retains its ability to modulate cancer cell growth. While small molecule inhibitors have been developed to stabilize and upregulate p53 expression, they have been found to induce a feedback loop that increases MDM2 protein levels, which can repress p53 and limit their efficacy. In preclinical studies, KT-253 has shown the ability to overcome the MDM2 feedback loop and rapidly induce cancer cell death, even with brief exposures. Given MDM2 overexpression and amplification is implicated in AML, KT-253 is being explored in this cancer, as well as other liquid and solid tumors.
“This orphan drug designation reinforces the potential of KT-253 to advance the treatment of AML by targeting MDM2, a protein that has been challenging to effectively drug with conventional medicines,” said Nello Mainolfi, Founder, President and CEO, Kymera Therapeutics. “We have a significant opportunity to deliver an important new medicine that acts on this common cancer mechanism, and we look forward to rapidly advancing KT-253 in AML and exploring its potential in other hematological and solid tumors.”
The Phase 1 study initiated in March 2023 will evaluate the safety, tolerability, pharmacokinetics/pharmacodynamics, and clinical activity of KT-253 in patients with relapsed or refractory high grade myeloid malignancies, including AML, acute lymphocytic leukemia (ALL), lymphoma and solid tumors. Patients in the KT-253 Phase 1a dose escalation study will receive IV doses of KT-253 administered once every 3 weeks. The open-label study is intended to identify the recommended Phase 2 dose for KT-253, and is comprised of two arms, with ascending doses of KT-253 in each arm. The first arm will consist of patients with lymphomas and advanced solid tumors and the second arm will consist of patients with high grade myeloid malignancies and ALL.
The FDA's Orphan Drug Designation program provides orphan status to drugs defined as those intended for the treatment, diagnosis or prevention of rare diseases that affect fewer than 200,000 people in the United States. Orphan drug designation qualifies the sponsor of the drug for certain development incentives, including tax credits for qualified clinical testing, prescription drug user fee exemptions and seven-year marketing exclusivity upon FDA approval.
About Acute Myeloid Leukemia (AML)
AML is a rapidly growing cancer of the blood and bone marrow characterized by a broad spectrum of cytogenetic and molecular abnormalities resulting in uncontrolled clonal expansion of myeloid blasts cells. In 2019, approximately 70,000 patients had been diagnosed with AML in the United States.
About Kymera Therapeutics
Kymera is a biopharmaceutical company pioneering the field of targeted protein degradation, a transformative approach to address disease targets and pathways inaccessible with conventional therapeutics. Kymera’s Pegasus platform is a powerful drug discovery engine, advancing novel small molecule programs designed to harness the body’s innate protein recycling machinery to degrade dysregulated, disease-causing proteins. With a focus on undrugged nodes in validated pathways, Kymera is advancing a pipeline of novel therapeutic candidates designed to address the most promising targets and provide patients with more effective treatments. Kymera’s initial programs target IRAK4, IRAKIMiD, and STAT3 within the IL-1R/TLR or JAK/STAT pathways, and the MDM2 oncoprotein, providing the opportunity to treat patients with a broad range of immune-inflammatory diseases, hematologic malignancies, and solid tumors.
Founded in 2016, Kymera is headquartered in Watertown, Mass. Kymera has been named a “Fierce 15” company by Fierce Biotech and has been recognized by both the Boston Globe and the Boston Business Journal as one of Boston’s top workplaces. For more information about our people, science, and pipeline, please visit www.kymeratx.com or follow us on Twitter or LinkedIn.
FDA grants orphan drug status to Kymera blood cancer drug KT-253
Jun. 22, 2023 12:17 PM ET
Kymera Therapeutics, Inc. (KYMR)
By: Val Brickates Kennedy, SA News Editor1 Comment
Kymera Therapeutics (NASDAQ:KYMR) said that its drug candidate KT-253 has received orphan drug status from the US Food and Drug Administration for the treatment of acute myeloid leukemia.
The company initiated Phase 1 testing of the drug in March for the treatment of various blood cancers. The drug, which targets and degrades the protein MDM2, is intended to help induce cancer cell death.
ERAS-801
VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection
VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection
ERASCA GRANTED FDA ORPHAN DRUG DESIGNATION FOR CNS-PENETRANT EGFR INHIBITOR ERAS-801 FOR THE TREATMENT OF MALIGNANT GLIOMA
06.22.2023
ERAS-801 has now received ODD in addition to FDA Fast Track Designation
Initial THUNDERBBOLT-1 Phase 1 monotherapy data in patients with recurrent GBM expected in H2 2023
SAN DIEGO, June 22, 2023 (GLOBE NEWSWIRE) -- Erasca, Inc. (Nasdaq: ERAS), a clinical-stage precision oncology company singularly focused on discovering, developing, and commercializing therapies for patients with RAS/MAPK pathway-driven cancers, today announced the United States Food and Drug Administration (FDA) has granted Orphan Drug Designation (ODD) to ERAS-801 for the treatment of malignant glioma, which includes glioblastoma (GBM). ERAS-801 is an orally bioavailable, small molecule EGFR inhibitor that exhibited substantial central nervous system (CNS) penetration in preclinical animal studies.
Per FDA regulations, ODD is granted by the FDA to investigational therapies addressing rare medical diseases or conditions affecting less than 200,000 people in the United States. Orphan drug status provides benefits to drug developers, including assistance in the drug development process, tax credits for clinical costs, exemptions from certain FDA fees, and the potential for seven years of post-approval marketing exclusivity.
“GBM is an aggressive malignancy afflicting approximately 37,000 patients annually in the United States and Europe. Currently approved EGFR inhibitors are limited by insufficient CNS penetration to treat GBM and minimal activity against GBM-specific EGFR amplifications, mutations, and other molecular alterations, which contribute to high rates of relapse and a five-year survival rate below 10%,” said Jonathan E. Lim, M.D., Erasca’s chairman, CEO, and co-founder. “Receiving ODD recognizes both the importance of innovation for patients with GBM and the therapeutic potential of ERAS-801 to provide a targeted treatment option for these patients, who have a poor prognosis. This ODD follows the earlier Fast Track Designation granted to ERAS-801 by the FDA and underscores the urgency of finding new treatments for this patient population. The broad activity against both oncogenic and wildtype EGFR, high CNS penetration, and demonstrated ability to improve outcomes in over 90% of diverse EGFR-driven patient-derived glioma models support the potential for ERAS-801 to overcome current challenges with existing therapies. We anticipate reporting initial monotherapy data for ERAS-801 from the Phase 1 THUNDERBBOLT-1 trial in patients with recurrent GBM in the second half of 2023.”
ERAS-801 was designed and developed by a renowned team of cancer researchers—Michael Jung, Ph.D., Timothy Cloughesy, M.D., and David Nathanson, Ph.D.
About ERAS-801
ERAS-801 is a highly potent, selective, reversible, and orally bioavailable small molecule EGFR inhibitor with significantly enhanced CNS penetration. In animal models, ERAS-801 had a brain-to-plasma partition coefficient, Kp, of 3.7 and a corresponding unbound partition coefficient, Kp,uu, of 1.2, which was up to four times higher than approved EGFR inhibitors, suggesting that approximately 100% of the free drug in plasma is able to cross the blood-brain barrier (BBB). At clinically relevant exposures across 30 patient-derived GBM models that were intended to represent the heterogeneity of GBM, ERAS-801 demonstrated a survival benefit in 13 out of 14 (93%) EGFR mutant and/or amplified models and had statistically significantly higher brain penetrance and prolonged survival compared to approved EGFR tyrosine kinase inhibitors, including osimertinib, lapatinib, and erlotinib. ERAS-801 is currently being evaluated as a monotherapy in THUNDERBBOLT-1, an ongoing Phase 1 trial in patients with recurrent GBM (rGBM). In April 2023, the FDA granted Fast Track Designation (FTD) to ERAS-801 for the treatment of adult patients with GBM with EGFR gene alterations. In June 2023, the FDA granted ODD to ERAS-801 for the treatment of malignant glioma, which includes glioblastoma.
About THUNDERBBOLT-1
THUNDERBBOLT-1 is evaluating the safety, tolerability, and preliminary efficacy of ERAS-801 as a monotherapy in patients with rGBM. The dose escalation portion will determine the recommended dose, which will then be used during the dose expansion portion to further evaluate the efficacy and safety of ERAS-801. Future sub-studies of THUNDERBBOLT-1 may potentially explore ERAS-801 in combination with other agents and in broader patient types. Initial Phase 1 data from THUNDERBBOLT-1 are anticipated in the second half of 2023.
About Erasca
At Erasca, our name is our mission: To erase cancer. We are a clinical-stage precision oncology company singularly focused on discovering, developing, and commercializing therapies for patients with RAS/MAPK pathway-driven cancers. Our company was co-founded by leading pioneers in precision oncology and RAS targeting to create novel therapies and combination regimens designed to comprehensively shut down the RAS/MAPK pathway for the treatment of cancer. We have assembled what we believe to be the deepest RAS/MAPK pathway-focused pipeline in the industry. We believe our team’s capabilities and experience, further guided by our scientific advisory board which includes the world’s leading experts in the RAS/MAPK pathway, uniquely position us to achieve our bold mission of erasing cancer.

![]()
Source: Erasca, Inc.
FDA grants orphan drug status to Erasca brain cancer drug ERAS-801
Jun. 22, 2023 5:53 PM ET
By: Val Brickates Kennedy, SA News Editor
The US Food and Drug Administration has granted orphan drug status to Erasca's (NASDAQ:ERAS) drug candidate ERAS-801 for the treatment of malignant brain tumors, including glioblastoma.
Erasca said the designation could entitle ERAS-801 to seven years of market exclusivity if it receives FDA approval. The drug received fast track status in April.
VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection
VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection
VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection
argenx Announces U.S. Food and Drug Administration Approval of VYVGART Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection for Subcutaneous Use in Generalized Myasthenia Gravis
NewsJune 20, 2023
argenx Announces U.S. Food and Drug Administration Approval of VYVGART Hytrulo Injection for Subcutaneous Use in Generalized Myasthenia Gravis
Amsterdam, the Netherlands
- VYVGART® Hytrulo is first FDA-approved subcutaneous (SC) injectable for generalized myasthenia gravis (gMG)
- With this approval, argenx broadens innovative gMG product offering and demonstrates continued commitment to providing more choice and flexibility for patients
- Efficacy of VYVGART Hytrulo was established by demonstrating a comparable pharmacodynamic (PD) effect to VYVGART® in Phase 3 ADAPT-SC bridging study
- Management to host conference call tomorrow at 2:30pm CET (8:30 am ET)
argenx SE (Euronext & Nasdaq: ARGX), a global immunology company committed to improving the lives of people suffering from severe autoimmune diseases, today announced that the U.S. Food and Drug Administration (FDA) approved VYVGART® Hytrulo (efgartigimod alfa and hyaluronidase-qvfc). VYVGART Hytrulo is an injection for subcutaneous (SC) use for the treatment of generalized myasthenia gravis (gMG) in adult patients who are anti-acetylcholine receptor (AChR) antibody positive. These patients represent approximately 85% of the total gMG population.
VYVGART Hytrulo is a subcutaneous product combination of efgartigimod alfa, a human IgG1 antibody fragment marketed for intravenous use as VYVGART, and recombinant human hyaluronidase PH20 (rHuPH20), Halozyme’s ENHANZE® drug delivery technology to facilitate subcutaneous delivery of biologics. The product is to be administered subcutaneously by a healthcare professional as a single injection (1,008 mg fixed dose) over 30-90 seconds in cycles of once weekly injections for four weeks.
“Today’s approval of VYVGART Hytrulo is another significant milestone on our path to redefine what well-controlled means for gMG patients. The availability of a second argenx innovation in just 18 months also underscores our longstanding commitment to the gMG community by providing more choice and flexibility in how patients receive treatment,” said Luc Truyen M.D., Ph.D., Chief Medical Officer, argenx. “With our broad gMG offering of both a first-in-class infusion and SC injection, we continue to offer an individualized treatment approach and possibility of staying symptom free, while providing patients options of how and where they want to seek treatment. We want to thank the gMG patient community and their supporters, clinical investigators, our employees and all stakeholders who have collaborated with us to advance this subcutaneous option, including our partners at Halozyme.”
“The availability of another gMG treatment option from argenx, now in a subcutaneous delivery, is a meaningful advancement for the patient community. Patients now have the opportunity to receive treatment in an infusion center, at home or at a physician’s office - providing more flexibility and freedom of choice that can make daily living easier for gMG patients and their caregivers,” said Allison Foss, Executive Director of the Myasthenia Gravis Association.
Phase 3 ADAPT-SC Bridging Study
“The clinical trials of VYVGART continue to show significant benefit to patients with a favorable safety profile and clear improvements in gMG disease scores. Now with the approval of VYVGART Hytrulo, we have a broad gMG treatment offering with both IV and SC administration options and can select based on patient needs and preference without sacrificing clinical benefit or safety,” said James F. Howard Jr., M.D., Professor of Neurology (Neuromuscular Disease), Medicine and Allied Health, Department of Neurology, The University of North Carolina at Chapel Hill School of Medicine and Principal Investigator for the ADAPT-SC trial.
This FDA approval is based on positive results from the Phase 3 ADAPT-SC study, which established the efficacy of VYVGART Hytrulo by demonstrating a reduction in anti-AChR antibody levels comparable to intravenous VYVGART in adult gMG patients. ADAPT-SC was a bridging study to the Phase 3 ADAPT study, which formed the basis for approval of intravenous VYVGART in December 2021.
In the ADAPT-SC study, the primary endpoint of noninferiority was met (p< 0.0001) and VYVGART Hytrulo demonstrated mean total IgG reduction of 66.4% from baseline at day 29, compared to 62.2% with VYVGART. Additional key secondary endpoints were met, which were consistent with efficacy measures from the ADAPT study identifying the correlation between total IgG reduction and clinical benefit in gMG.
VYVGART Hytrulo has a demonstrated safety profile, consistent with the ADAPT clinical trial with the exception of injection site reactions (ISRs), which were higher with VYVGART Hytrulo. It was generally well-tolerated with ISRs being the most frequent adverse events. All ISRs, which are commonly observed with biologics administered subcutaneously, were mild to moderate, and resolved over time.
Access to VYVGART Hytrulo
VYVGART Hytrulo is expected to be available for patients in the U.S. in July 2023. argenx is committed to supporting access for patients to its medicines and has decided to price VYVGART Hytrulo at parity to VYVGART on a net annual revenue basis.
Throughout their treatment journey, patients can access VYVGART Hytrulo in the same personalized way they access VYVGART today with support from My VYVGART Path. Program resources include disease and product education, access support and benefits verification, and financial assistance programs for eligible patients. Patients and clinicians can access more information at VYVGARTHytrulo.com.
Marketing authorization applications for SC efgartigimod are under review by the European Medicines Agency with a decision expected by the end of 2023, and Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) with a decision expected by the first quarter of 2024.
What is VYVGART® HYTRULO (efgartigimod alfa and hyaluronidase-qvfc)?
VYVGART HYTRULO is a prescription medicine used to treat a condition called generalized myasthenia gravis, which causes muscles to tire and weaken easily throughout the body, in adults who are positive for antibodies directed toward a protein called acetylcholine receptor (anti-AChR antibody positive).
About Phase 3 ADAPT-SC Trial
The Phase 3 ADAPT-SC trial was a multicenter, randomized, open-label, parallel-group study evaluating the noninferiority of the pharmacodynamic (PD) effect of VYVGART Hytrulo compared with VYVGART in adult patients with gMG. The pharmacodynamic effect was measured by percent change from baseline in autoantibody (AChR) levels at day 29. Safety, clinical efficacy, immunogenicity and pharmacokinetics (PK) were also assessed. A total of 110 adult patients with gMG in North America, Europe and Japan enrolled in the ADAPT-SC trial. Patients were randomized in a 1:1 ratio to receive VYVGART Hytrulo or VYVGART for one treatment cycle consisting of four doses at once-weekly intervals. The total study duration was approximately 12 weeks, including seven weeks of follow-up after the treatment cycle. At the completion of ADAPT-SC, patients had the opportunity to roll-over to ADAPT-SC+, an open-label extension study.
About VYVGART® Hytrulo
VYVGART Hytrulo is a subcutaneous combination of efgartigimod alfa, a human IgG1 antibody fragment marketed for intravenous use as VYVGART®, and recombinant human hyaluronidase PH20 (rHuPH20), Halozyme’s ENHANZE® drug delivery technology to facilitate subcutaneous injection delivery of biologics. In binding to the neonatal Fc receptor (FcRn), VYVGART Hytruloresults in the reduction of circulating IgG. It is the first-and-only approved FcRn blocker administered by subcutaneous injection.
About Generalized Myasthenia Gravis
Generalized myasthenia gravis (gMG) is a rare and chronic autoimmune disease where IgG autoantibodies disrupt communication between nerves and muscles, causing debilitating and potentially life-threatening muscle weakness. Approximately 85% of people with MG progress to gMG within 24 months, where muscles throughout the body may be affected. Patients with confirmed AChR antibodies account for approximately 85% of the total gMG population.
About argenx
argenx is a global immunology company committed to improving the lives of people suffering from severe autoimmune diseases. Partnering with leading academic researchers through its Immunology Innovation Program (IIP), argenx aims to translate immunology breakthroughs into a world-class portfolio of novel antibody-based medicines. argenx developed and is commercializing the first-and-only approved neonatal Fc receptor (FcRn) blocker in the U.S., Japan, Israel, the EU and the UK. The Company is evaluating efgartigimod in multiple serious autoimmune diseases and advancing several earlier stage experimental medicines within its therapeutic franchises. For more information, visit www.argenx.com and follow us on LinkedIn, Twitter, and Instagram.
Argenx wins FDA nod for myasthenia gravis therapy
Jun. 21, 2023 7:02 AM ET
By: Dulan Lokuwithana, SA News Editor
- Dutch biotech argenx SE (NASDAQ:ARGX) traded higher in the pre-market Wednesday after announcing the FDA approval of Vyvgart Hytrulo as a subcutaneous injection for patients with the autoimmune condition, generalized myasthenia gravis (gMG).
- https://seekingalpha.com/news/3981285-argenx-wins-fda-nod-myasthenia-g argenx SE (ARGX), HALO ravis-therapy
- https://vyvgart.com/
- https://www.argenx.com/
lovotibeglogene autotemcel (lovo-cel)
AKEEGA™ (niraparib and abiraterone acetate)
lovotibeglogene autotemcel (lovo-cel)
bluebird bio Announces FDA Priority Review of the Biologics License Application for lovotibeglogene autotemcel (lovo-cel) for Patients with Sickle Cell Disease (SCD) 12 years and Older with a History of Vaso-Occlusive Events
BLA submission based on data from the largest and most mature clinical development program for any gene therapy in sickle cell disease
PDUFA date set for December 20, 2023
SOMERVILLE, Mass.--(BUSINESS WIRE)--Jun. 21, 2023-- bluebird bio, Inc. (Nasdaq: BLUE) today announced that the U.S. Food and Drug Administration (FDA) has accepted the Biologics License Application (BLA) for lovotibeglogene autotemcel (lovo-cel) for priority review. Lovo-cel is a potentially transformative one-time gene therapy for individuals living with sickle cell disease (SCD) ages 12 and older who have a history of vaso-occlusive events (VOEs). It is specifically designed to treat the underlying cause of SCD through the addition of a functional gene that enables production of anti-sickling adult hemoglobin and is the most deeply studied gene therapy in development for this disease. The agency has set a Prescription Drug User Fee Act (PDUFA) goal date of December 20, 2023.
“The burden that people living with SCD and their families live with today is staggering. Beyond extreme pain crises that send patients to the hospital, SCD progression is associated with grave long-term consequences,” said Andrew Obenshain, chief executive officer, bluebird bio. “The FDA’s acceptance of our BLA for lovo-cel moves us one step closer in bringing a potentially transformative therapy to the sickle cell disease community that is long overdue, and we are grateful to the patients, caregivers, researchers, clinicians, and community leaders who have enabled this exciting milestone. We look forward to working with the agency on its review.”
The BLA for lovo-cel is based on efficacy results from 36 patients in the HGB-206 study Group C cohort with a median 32 months of follow-up and two patients in the HGB-210 study with 18 months of follow-up each. The BLA submission also includes safety data from 50 patients treated across the entire lovo-cel program, including six patients with six or more years of follow-up, which is the longest follow-up of any gene therapy program for SCD.
If approved, lovo-cel will be bluebird bio’s third ex-vivo gene therapy approved by the FDA for a rare genetic disease and its second FDA approval for an inherited hemoglobin disorder, building on more than a decade of leadership in gene therapy.
The FDA’s Priority Review designation is granted to therapies that have the potential to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions, and targets a review timeline of six months from the time of filing, compared to a standard review timeline of 10 months.
The FDA previously granted lovo-cel orphan drug designation, fast track designation, regenerative medicine advanced therapy (RMAT) designation, and rare pediatric disease designation.
About sickle cell disease (SCD)
Sickle cell disease (SCD) is a complex and progressive genetic disease associated with debilitating and unpredictable pain crises, anemia, irreversible damage to vital organs, and early death. In SCD, high concentrations of sickle hemoglobin (HbS) in red blood cells (RBCs) cause RBCs to become sickled, sticky, and rigid with a shorter life span, which manifests acutely as hemolytic anemia, vasculopathy, and vaso-occlusion. Pain onset can be sudden and unpredictable, often requiring hospitalization. Fifty to sixty percent of adults with sickle cell disease have end organ damage, with 24 percent experiencing damage in multiple organs, and one in four patients have a stroke by the age of 45. The impact of SCD is pervasive and affects every aspect of life for patients and their families and caregivers – from missed work and school, decreased quality of life and mental health, and the ability to complete daily tasks. In the U.S., there are approximately 100,000 people living with SCD, and the median age of death is 45 years of age.
While SCD was the first disease to have a genetic cause identified, treatment advances have lagged – since that discovery in 1949,i only four therapies have been approved,ii none of which address the underlying genetic cause of disease.
About lovotibeglogene autotemcel (lovo-cel)
lovotibeglogene autotemcel (lovo-cel) gene therapy is an investigational one-time treatment being studied for sickle cell disease (SCD), that is designed to add functional copies of a modified form of the β-globin gene (βA-T87Q-globin gene) into a patient’s own hematopoietic (blood) stem cells (HSCs). Once patients have the βA-T87Q-globin gene, their red blood cells (RBCs) can produce anti-sickling hemoglobin (HbAT87Q) that decreases the proportion of HbS, with the goal of reducing sickled RBCs, hemolysis, and other complications. bluebird bio’s clinical development program for lovo-cel includes the completed Phase 1/2 HGB-205 and ongoing Phase 1/2 HGB-206 and Phase 3 HGB-210 studies. bluebird bio is also conducting a long-term safety and efficacy follow-up study (LTF-307) for people who have been treated with lovo-cel in bluebird bio-sponsored clinical studies.
In the BLA submission, as of August 2022, the majority of adverse events in treated patients were attributed to underlying sickle cell disease or conditioning with busulfan. Nonserious adverse events related to lovo-cel included infusion reactions (hot flush and decreased blood pressure) in two patients (2% each). Serious adverse events related to lovo-cel included anemia in two patients (4%) with concurrent alpha-thalassemia trait, and leukemia in two patients (4%), not resulting from insertional oncogenesis. Three of 50 patients (6%) died, one due to sudden cardiac death and two due to leukemia.
About bluebird bio, Inc.
bluebird bio is pursuing curative gene therapies to give patients and their families more bluebird days.
With a dedicated focus on severe genetic diseases, bluebird has industry-leading programs for sickle cell disease, β-thalassemia and cerebral adrenoleukodystrophy and is advancing research to apply new technologies to these and other diseases. We custom design each of our therapies to address the underlying cause of disease and have developed in-depth and effective analytical methods to understand the safety of our lentiviral vector technologies and drive the field of gene therapy forward.
Founded in 2010, bluebird has the largest and deepest ex-vivo gene therapy data set in the world—setting the standard for the industry. Today, bluebird continues to forge new paths, combining our real-world experience with a deep commitment to patient communities and a people-centric culture that attracts and grows a diverse flock of dedicated birds.
For more information, visit bluebirdbio.com or follow us on social media at @bluebirdbio, LinkedIn, Instagram and YouTube.
bluebird bio is a trademark of bluebird bio, Inc.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230621695509/en/
Source: bluebird bio, Inc.
bluebird bio gains on FDA priority review for new gene therapy
Jun. 21, 2023 7:24 AM ET
bluebird bio, Inc. (BLUE)VRTX, CRSP
By: Dulan Lokuwithana, SA News Editor4 Comments
- bluebird bio (NASDAQ:BLUE) added ~5% pre-market Wednesday after announcing that the FDA granted priority review for the company’s Biologics License Application (BLA) for its gene therapy lovo-cel targeted at patients with sickle cell disease (SCD).
- The agency has set December 20, 2023, as the regulatory action date for its decision.
- https://seekingalpha.com/news/3981328-bluebird-bio-wins-fda-priority-review-gene-therapy
- bluebird bio, Inc. (BLUE)
- https://www.bluebirdbio.com/our-science/pipeline
- https://www.bluebirdbio.com/
Pelabresib (CPI-0610)
AKEEGA™ (niraparib and abiraterone acetate)
lovotibeglogene autotemcel (lovo-cel)
MorphoSys to Host Virtual Investor Call with Key Opinion Leaders Focused on Pelabresib on June 21, 2023
EQS-News: MorphoSys AG / Key word(s): Miscellaneous
MorphoSys to Host Virtual Investor Call with Key Opinion Leaders Focused on Pelabresib on June 21, 2023
14.06.2023 / 08:39 CET/CEST
The issuer is solely responsible for the content of this announcement.
Media Release
Planegg/Munich, Germany, June 14, 2023
MorphoSys to Host Virtual Investor Call with Key Opinion Leaders Focused on Pelabresib on June 21, 2023
MorphoSys AG (FSE: MOR; NASDAQ: MOR) will host a virtual investor event on Wednesday, June 21, at 9:00 a.m. EDT / 3:00 p.m. CEST.
During the event, Jean-Paul Kress, M.D., MorphoSys’ Chief Executive Officer, and Tim Demuth, M.D., Ph.D., MorphoSys’ Chief Research and Development Officer, will discuss the potential of the company’s lead investigational asset, pelabresib. There will also be live presentations from – and a Q&A opportunity with – key opinion leaders John Mascarenhas, M.D., Professor of Medicine and Director of the Adult Leukemia Program at The Tisch Cancer Institute at Mount Sinai, New York, and Gabriela Hobbs, M.D., Assistant Professor of Medicine at Harvard Medical School, and Clinical Director of Leukemia Service at Massachusetts General Hospital.
Topics will include an overview of the disease burden for patients with myelofibrosis, including treatment gaps; a recap of encouraging findings in myelofibrosis from the pelabresib Phase 2 MANIFEST study in combination with ruxolitinib and background on the Phase 3 MANIFEST-2 study, which will report topline results by the end of 2023; and new proof of concept results and expansion plans for pelabresib in other myeloid diseases. The full agenda is below.
To access the live webcast, including audio, video and presentation slides, visit the Investors section of the MorphoSys website at https://www.morphosys.com/en/investors.
A replay of the webcast and presentation will be available on the company’s website after the event.
Agenda:
PresenterPresentationJean-Paul Kress, M.D.
Chief Executive Officer, MorphoSys
Welcome and opening remarksGabriela Hobbs, M.D.
Assistant Professor of Medicine at Harvard Medical School and Clinical Director of Leukemia Service at Massachusetts General Hospital
Myelofibrosis burden of disease and medical needJohn Mascarenhas, M.D.
Professor of Medicine and Director of the Adult Leukemia Program
at The Tisch Cancer Institute at Mount Sinai, New York
Pelabresib in myelofibrosis updateTim Demuth, M.D., Ph.D.
Chief Research and Development Officer, MorphoSys
Pelabresib clinical development road mapAll presentersModerated Q&A
About MorphoSys
At MorphoSys, we are driven by our mission: More life for people with cancer. As a global commercial-stage biopharmaceutical company, we develop and deliver innovative medicines, aspiring to redefine how cancer is treated. MorphoSys is headquartered in Planegg, Germany, and has its U.S. operations anchored in Boston, Massachusetts. To learn more, visit us at www.morphosys.com and follow us on Twitter and LinkedIn.
About Pelabresib
Pelabresib (CPI-0610) is an investigational selective small molecule designed to promote anti-tumor activity by inhibiting the function of bromodomain and extra-terminal domain (BET) proteins to decrease the expression of abnormally expressed genes in cancer. Pelabresib is being investigated as a treatment for myelofibrosis and has not yet been evaluated or approved by any regulatory authorities.
About MANIFEST-2
MANIFEST-2 (NCT04603495) is a global, double-blind, randomized Phase 3 clinical trial with pelabresib in combination with ruxolitinib versus placebo plus ruxolitinib in JAK inhibitor-naïve patients with myelofibrosis. The primary endpoint of the study is a 35% or greater reduction in spleen volume (SVR35) from baseline at 24 weeks. The key secondary endpoint of the study is a 50% or greater improvement in total symptom score (TSS50) from baseline at 24 weeks. Topline data from the MANIFEST-2 study will be available by the end of 2023. Constellation Pharmaceuticals, Inc., a MorphoSys company, is the MANIFEST-2 trial sponsor.
About MANIFEST
MANIFEST (NCT02158858) is an open-label Phase 2 clinical trial of pelabresib in patients with myelofibrosis. The MANIFEST trial is evaluating pelabresib in combination with ruxolitinib in JAK-inhibitor-naïve myelofibrosis patients (Arm 3), with a primary endpoint of the proportion of patients with a ≥35% spleen volume reduction from baseline (SVR35) after 24 weeks of treatment. The trial is also evaluating pelabresib either as a monotherapy in patients who are resistant to, intolerant of, or ineligible for ruxolitinib and no longer on the drug (Arm 1) or as add-on therapy in combination with ruxolitinib in patients with a suboptimal response to ruxolitinib or myelofibrosis progression (Arm 2). Patients in Arms 1 and 2 are being stratified based on transfusion-dependent (TD) status. The primary endpoint for the patients in cohorts 1A and 2A, who were TD at baseline, is conversion to transfusion independence for 12 consecutive weeks. The primary endpoint for patients in cohorts 1B and 2B, who were not TD at baseline, is the proportion of patients with a ≥35% spleen volume reduction from baseline after 24 weeks of treatment. The study is also evaluating pelabresib as a monotherapy in patients with high-risk essential thrombocythemia who are intolerant of, or refractory to, hydroxyurea (Arm 4). The primary endpoint for patients in Arm 4 is complete hematological response rate after one cycle, or 21 days, of treatment. Constellation Pharmaceuticals, Inc., a MorphoSys company, is the MANIFEST trial sponsor.
JP Morgan upgrades MorphoSys to overweight ahead of Phase 3 data
Jun. 16, 2023 7:30 PM ET
By: Val Brickates Kennedy, SA News Editor
JP Morgan has upgraded MorphoSys (NASDAQ:MOR) to overweight, citing upcoming data from a Phase 3 clinical study for its drug pelabresib in the treatment of myelofibrosis, a type of bone marrow cancer.
AKEEGA™ (niraparib and abiraterone acetate)
AKEEGA™ (niraparib and abiraterone acetate)
AKEEGA™ (niraparib and abiraterone acetate)
Health Canada Authorizes AKEEGA™ (niraparib and abiraterone acetate) Dual Action Tablets for Targeted Treatment of Patients with Metastatic Castration-Resistant Prostate Cancer (mCRPC) with BRCA (1/2) Gene Mutations
Jun. 14, 2023 8:00 AM ET
Approval for AKEEGATM is based on results from the Phase 3 MAGNITUDE study, a prospectively designed precision medicine study that includes the largest cohort to date of BRCA1/2-positive patients with untreated metastatic castration-resistant prostate cancer (mCRPC)1,2
Niraparib in combination with abiraterone acetate plus prednisone or prednisolone (AAP), showed significant improvement in radiographic progression-free survival (rPFS) compared to AAP in mCRPC patients with BRCA1/2 mutations3
TORONTO, June 5, 2023 /CNW/ - The Janssen Pharmaceutical Companies of Johnson & Johnson (JNJ) announced today that Health Canada has issued a Notice of Compliance with conditions (NOC/c) for AKEEGA™ (niraparib and abiraterone acetate) tablets, plus prednisone or prednisolone for the treatment of adult patients with deleterious or suspected deleterious BRCA mutated (germline and/or somatic) metastatic castration resistant prostate cancer (mCRPC), who are asymptomatic/mildly symptomatic, and in whom chemotherapy is not clinically indicated. Patients must have confirmation of BRCA mutation before AKEEGA™ treatment is initiated.4 The approval with conditions is based on a clinically meaningful radiographic progression-free survival (rPFS), time to symptomatic progression (TSP) and time to cytotoxic chemotherapy (TCC) with continued approval contingent upon the verification and description of clinical benefit from the final OS analyses.4

"Patients with BRCA-altered prostate cancer face an aggressive disease that can have a worse prognosis than patients whose cancers do not have these mutations," says Dr. Kim Chi*, Medical Oncologist, BC Cancer. "Thankfully, years of research have led to the development of novel targeted therapies like the combination of niraparib with abiraterone plus prednisone that can significantly improve outcomes for the right patients. Early biomarker identification paired with targeted treatment can set a new standard of care for patients and enable physicians to take a more personalized and precision medicine approach to treating this unique subset of prostate cancers."
Prostate cancer is the most common cancer (excluding non-melanoma skin cancers) and third leading cause of cancer death among Canadian men, with an estimated 4,600 deaths in 2022.5 Approximately 10 to 50 per cent of prostate cancer patients progress to mCRPC within three years of a diagnosis6 of whom an estimated 10 to 15 per cent harbour a BRCA mutation.7 Despite advancements in available therapies, the five-year survival rate for men with metastatic prostate cancer remains at 30 per cent.8
The presence of mutations in homologous recombination repair (HRR) genes, which include BRCA1/2 genes, is associated with potentially an early onset of disease, a more aggressive form of the disease, a higher rate of recurrence, and poor prognosis, demonstrating the importance of biomarker testing for timely identification of these mutations.6
"There is a significant need among those diagnosed with this form of prostate cancer who, until now, have had no treatment options targeting their disease. It is critical for these patients to get the right treatment at the right time, underscoring the importance of early genetic testing for these biomarkers," says Jackie Manthorne**, President & CEO, Canadian Cancer Survivor Network. "The approval of this new therapy represents a clear path toward better outcomes and gives patients the hope that they can have more meaningful time with those they love."
The Health Canada NOC/c is based on positive results from the randomized, double-blind, placebo-controlled multicenter Phase 3 MAGNITUDE study.4 The trial assessed whether the addition of niraparib to abiraterone acetate plus prednisone or prednisolone (AAP) compared with placebo plus AAP improved outcomes in those with mCRPC, with or without alterations in HRR- associated genes, including BRCA1/2.4,9 A total of 423 patients with HRR gene alterations were enrolled, 225 of whom had BRCA mutations, making this the largest cohort of BRCA1/2-positive patients with first line mCRPC in any clinical study to date.1,4 At the primary analysis with a median follow-up of 18.6 months, patients with BRCA mutations who received niraparib and AAP treatment experienced an improvement in rPFS, with a 47 per cent reduction in the risk of radiographic progression or death compared with the placebo group (HR = 0.533; 95% CI: [0.361, 0.789], two-sided p = 0.0014).3,4 Improvements in TCC and TSP were also observed although the significance boundary of 0.0001 was not met by either endpoint at the first interim analysis for these secondary endpoints.3
The observed safety profile of the combination of niraparib and AAP was consistent with the known safety profile of each agent, with no new safety signals identified.4 Serious adverse events occurred in 36 per cent of patients treated with niraparib plus AAP and 25 per cent of patients treated with placebo plus AAP.4 Permanent discontinuation due to an adverse event occurred in 10.8 per cent of patients treated with niraparib plus AAP and 6.2 per cent of patients treated with placebo plus AAP.4 The combination of niraparib and AAP also maintained overall quality of life in comparison with placebo and AAP.3
AKEEGA™ will be available as regular strength tablets containing 100 mg niraparib / 500 mg abiraterone (recommended starting dose) and low-strength tablets of 50 mg niraparib / 500 mg abiraterone acetate respectively.4
"For the past 30 years, Janssen has been dedicated to improving patient outcomes through delivering transformational therapies where they are needed most, especially where people face devastating forms of cancer with limited treatment options," says Berkeley Vincent, President, Janssen Inc. "The approval of AKEEGA™ further strengthens our portfolio of prostate cancer therapies and enables us to take another step toward changing the trajectory of this disease."
Janssen's legacy of innovation in prostate cancer has significantly contributed to the evolution of treatment approaches for over a decade. From the first approval for ZYTIGA® (abiraterone acetate) in 2011 followed by ERLEADA® (apalutamide tablets) in 2018, Janssen has continued to build on insights from clinical research, leading to four approved indications in prostate cancer.10,11 The authorization of AKEEGATM marks Janssen's fifth indication for the treatment of prostate cancer across the continuum of the disease.
About AKEEGATM
AKEEGATM (niraparib and abiraterone acetate) is an orally administered, tablets of niraparib, a highly selective poly (adenosine diphosphate-ribose) polymerase (PARP) inhibitor, and abiraterone prodrug, an androgen biosynthesis inhibitor which blocks enzyme 17a-hydroxylase/C17,20-lyase (CYP17).4 This combination targets two oncogenic drivers in patients with mCRPC and HRR gene alterations.4 AKEEGATM is indicated with prednisone or prednisolone for the treatment of adult patients with deleterious or suspected deleterious BRCA mutated (germline and/or somatic) mCRPC, who are asymptomatic/mildly symptomatic, and in whom chemotherapy is not clinically indicated. Patients must have confirmation of BRCA mutation before AKEEGA™ treatment is initiated.4
The overall safety profile of AKEEGA™ is based on MAGNITUDE cohort 1, which consisted of HRR positive patients who received niraparib 200 mg once daily plus AAP (n=212) or placebo plus AAP (n=211).4 The median duration of exposure to niraparib plus AAP was 13.8 months.4 Serious adverse events occurred in 36 per cent of patients treated with niraparib plus AAP and 25 per cent of patients treated with placebo plus AAP.4 Fatal adverse events occurred in 5.7 per cent of those treated with niraparib plus AAP and 3.3 per cent of patients treated with placebo plus AAP.4 The most common adverse events (all grades) in patients treated with niraparib plus AAP were anemia, hypertension, constipation, fatigue, nausea and thrombocytopenia.4 The most frequently observed adverse events greater or equal to grade 3 were anemia, hypertension, thrombocytopenia, neutropenia and blood alkaline phosphatase increased.4
Additional ongoing studies include the Phase 3 AMPLITUDE study, evaluating the combination of niraparib and AAP in a biomarker-selected patient population with metastatic castration-sensitive prostate cancer (mCSPC).12
About MAGNITUDE
MAGNITUDE (NCT03748641) is a Phase 3 randomized, double-blind, placebo-controlled, multicenter clinical study evaluating the safety and efficacy of the combination of niraparib and AAP for patients with mCRPC (n=765), with or without certain HRR gene alterations and who have not received prior therapy for mCRPC, and for patients with mCSPC who have only received standard of care, next-generation androgen receptor inhibitors and up to four months of AAP.3,4 The study includes patients with (HRR biomarker [BM] positive; ATM, BRCA1, BRCA2, BRIP1, CDK12, CHEK2, FANCA, HDAC2, PALB2) and without specified gene alterations (HRR BM negative), who were randomized 1:1 to receive niraparib 200 mg once daily plus AAP or placebo plus AAP.3 A total of 423 patients with HRR gene alterations were enrolled, 225 (53.2 per cent) of whom had BRCA mutations.1,4 The primary endpoint of the MAGNITUDE trial is rPFS assessed by blinded independent central review.4 Secondary endpoints include TCC, TSP and overall survival (OS).4
About single agents (abiraterone acetate and niraparib)
Abiraterone acetate, marketed by Janssen in Canada as ZYTIGA®, is an orally administered androgen biosynthesis inhibitor. In Canada, abiraterone acetate is indicated in combination with prednisone for the treatment of mCRPC in patients who are asymptomatic or mildly symptomatic or have received prior chemotherapy containing docetaxel after failure of androgen deprivation.10 It is also indicated in combination with prednisone and androgen deprivation therapy (ADT) for the treatment of patients with newly diagnosed hormone-sensitive high-risk metastatic prostate cancer who may have received up to 3 months of prior ADT.10
In April 2016, Janssen Biotech, Inc. entered a worldwide (except Japan) collaboration and license agreement with TESARO, Inc. (acquired by GlaxoSmithKline [GSK] in 2019) for exclusive rights to niraparib in prostate cancer.
In Canada, niraparib is currently marketed by GSK as ZEJULA®, as a monotherapy for the maintenance treatment of female adult patients with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in a complete or partial response to first-line platinum-based chemotherapy; and for the maintenance treatment of female adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in a complete or partial response to platinum-based chemotherapy.13
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we're creating a future where disease is a thing of the past. We're the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com/canada. Follow us at www.twitter.com/JanssenCanada. Janssen Inc. is one of the Janssen Pharmaceutical Companies of Johnson & Johnson.
JNJ Dividend History
https://www.nasdaq.com/market-activity/stocks/jnj/dividend-history
LEQEMBI® (lecanemab-irmb)
LEQEMBI® (lecanemab-irmb)
AKEEGA™ (niraparib and abiraterone acetate)
FDA Advisory Committee Votes Unanimously to Confirm the Clinical Benefit of LEQEMBI® (lecanemab-irmb) for the Treatment of Alzheimer’s Disease
JUNE 9, 2023 • NEWS RELEASE
Peripheral and Central Nervous System Drugs Advisory Committee voted based on data from large global confirmatory Phase 3 Clarity AD clinical trial in patients living with early Alzheimer’s disease
The PDUFA action date for traditional approval of LEQEMBI has been set for July 6, 2023, with designation of priority review
LEQEMBI received accelerated approval from the FDA for the treatment of early Alzheimer’s disease on January 6, 2023
TOKYO and CAMBRIDGE, Mass., June 09, 2023 (GLOBE NEWSWIRE) -- Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, “Eisai”) and Biogen Inc. (Nasdaq: BIIB, Corporate headquarters: Cambridge, Massachusetts, CEO: Christopher A. Viehbacher, “Biogen”) announced today that the U.S. Food and Drug Administration’s (FDA) Peripheral and Central Nervous System Drugs Advisory Committee (PCNS) voted unanimously that the data from Eisai’s Phase 3 Clarity AD clinical trial confirms the clinical benefit of LEQEMBI® (lecanemab-irmb) 100 mg/mL injection for intravenous use for the treatment of Alzheimer’s disease (AD). Additionally, the committee members confirmed the overall benefit-risk profile of LEQEMBI, the clinical meaningfulness of the data and discussed its use in specific subgroups, including Apolipoprotein E (ApoE) ε4 homozygote patients, patients requiring concomitant treatment with anticoagulant agents, and patients with cerebral amyloid angiopathy.
The unanimous decision by the panel of independent experts was based on the supplementary Biologics License Application (sBLA) which includes data from Eisai’s large global confirmatory Phase 3 Clarity AD trial. The Clarity AD trial met its prespecified primary endpoint, demonstrating a highly statistically significant slowing of cognitive and functional decline (27%, p=0.00005) compared to placebo over 18 months. Highly statistically significant treatment effects were also observed for all multiplicity-controlled secondary endpoints that examined cognition and functional changes using other validated scales. The most common adverse events (>10%) in the LEQEMBI group were infusion reactions (LEQEMBI: 26.4%; placebo: 7.4%), ARIA-H (combined cerebral microhemorrhages, cerebral macrohemorrhages, and superficial siderosis: LEQEMBI: 17.3%; placebo: 9.0%), ARIA-E (edema/effusion: LEQEMBI: 12.6%; placebo: 1.7%), headache (LEQEMBI: 11.1%; placebo: 8.1%), and fall (LEQEMBl: 10.4%; placebo: 9.6%). Infusion reactions were largely mild-to-moderate (grade 1-2: 96%) and occurred on the first dose (75%). The results of the Clarity AD study were presented at the Clinical Trials on Alzheimer's Disease (CTAD) conference and simultaneously published in the peer-reviewed medical journal, The New England Journal of Medicine [nejm.org].
LEQEMBI, a humanized immunoglobulin gamma 1 (IgG1) monoclonal antibody directed against aggregated soluble (protofibril*) and insoluble forms of amyloid beta (Aβ), received accelerated approval on January 6, 2023, and was launched in the U.S. on January 18, 2023. The accelerated approval was based on Phase 2 data that demonstrated that LEQEMBI reduced the accumulation of Aβ plaque in the brain, a defining feature of AD. Its continued approval may be contingent upon verification of LEQEMBI’s clinical benefit in the confirmatory Clarity AD trial (Study 301). The advisory committee agreed unanimously that Study 301 verified the clinical benefit. The Prescription Drug User Fee Act (PDUFA) action date for the traditional approval is July 6, 2023.
Eisai serves as the lead of lecanemab development and regulatory submissions globally with both companies co-commercializing and co-promoting the product and Eisai having final decision-making authority.
LEQEMBI has been approved under the FDA accelerated approval pathway. Click here for the Prescribing Information [leqembi.com].
INDICATION, DOSAGE AND ADMINISTRATION, AND IMPORTANT SAFETY INFORMATION IN THE U.S.
INDICATION
LEQEMBI is indicated for the treatment of Alzheimer’s disease. Treatment with LEQEMBI should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was initiated in clinical trials. There are no safety or effectiveness data on initiating treatment at earlier or later stages of the disease than were studied. This indication is approved under accelerated approval based on reduction in amyloid beta plaques observed in patients treated with LEQEMBI. Continued approval for this indication may be contingent upon verification of clinical benefit in a confirmatory trial.
IMPORTANT SAFETY INFORMATION
WARNINGS AND PRECAUTIONS
Amyloid Related Imaging Abnormalities
- LEQEMBI can cause amyloid related imaging abnormalities-edema (ARIA-E) and -hemosiderin deposition (ARIA-H). ARIA-E can be observed on MRI as brain edema or sulcal effusions, and ARIA-H as microhemorrhage and superficial siderosis. ARIA is usually asymptomatic, although serious and life-threatening events, including seizure and status epilepticus, rarely can occur. Reported symptoms associated with ARIA may include headache, confusion, visual changes, dizziness, nausea, and gait difficulty. Focal neurologic deficits may also occur. Symptoms associated with ARIA usually resolve over time.
ARIA Monitoring and Dose Management Guidelines
- Obtain recent (within one year) brain magnetic resonance imaging (MRI) prior to initiating treatment with LEQEMBI. Obtain an MRI prior to the 5th, 7th, and 14th infusions.
- Recommendations for dosing in patients with ARIA-E and ARIA-H depend on clinical symptoms and radiographic severity. Depending on ARIA severity, use clinical judgment in considering whether to continue dosing, temporarily discontinue treatment, or permanently discontinue LEQEMBI.
- Enhanced clinical vigilance for ARIA is recommended during the first 14 weeks of treatment with LEQEMBI. If a patient experiences symptoms suggestive of ARIA, clinical evaluation should be performed, including MRI if indicated. If ARIA is observed on MRI, careful clinical evaluation should be performed prior to continuing treatment.
- There is no experience in patients who continued dosing through symptomatic ARIA-E or through asymptomatic, but radiographically severe, ARIA-E. There is limited experience in patients who continued dosing through asymptomatic but radiographically mild to moderate ARIA-E. There are limited data in dosing patients who experienced recurrent ARIA-E.
Incidence of ARIA
- In Study 1 (Study 201), symptomatic ARIA occurred in 3% (5/161) of LEQEMBI-treated patients. Clinical symptoms associated with ARIA resolved in 80% of patients during the period of observation.
- Including asymptomatic cases, ARIA was observed in LEQEMBI: 12% (20/161); placebo: 5% (13/245). ARIA-E was observed in LEQEMBI: 10% (16/161); placebo: 1% (2/245). ARIA-H was observed in LEQEMBI: 6% (10/161); placebo: 5% (12/245). There was no increase in isolated ARIA-H for LEQEMBI compared to placebo.
- Intracerebral hemorrhage >1 cm in diameter was reported after one treatment in LEQEMBI: 1 patient; placebo: zero patients. Events of intracerebral hemorrhage, including fatal events, in patients taking LEQEMBI have also been reported in other studies.
Apolipoprotein E ε4 (ApoE ε4) Carrier Status and Risk of ARIA
- In Study 1, 6% (10/161) of patients in the LEQEMBI group were ApoE ε4 homozygotes, 24% (39/161) were heterozygotes, and 70% (112/161) were noncarriers.
- The incidence of ARIA was higher in ApoE ε4 homozygotes than in heterozygotes and noncarriers among patients treated with LEQEMBI. Of the 5 LEQEMBI-treated patients who had symptomatic ARIA, 4 were ApoE ε4 homozygotes, 2 of whom experienced severe symptoms. An increased incidence of symptomatic and overall ARIA in ApoE ε4 homozygotes compared to heterozygotes and noncarriers in LEQEMBI-treated patients has been reported in other studies.
- The recommendations on management of ARIA do not differ between ApoE ε4 carriers and noncarriers.
- Consider testing for ApoE ε4 status to inform the risk of developing ARIA when deciding to initiate treatment with LEQEMBI.
Radiographic Findings
- The majority of ARIA-E radiographic events occurred early in treatment (within the first 7 doses), although ARIA can occur at any time and patients can have more than 1 episode. The maximum radiographic severity of ARIA-E in patients treated with LEQEMBI was mild in 4% (7/161) of patients, moderate in 4% (7/161) of patients, and severe in 1% (2/161) of patients. Resolution on MRI occurred in 62% of ARIA-E patients by 12 weeks, 81% by 21 weeks, and 94% overall after detection. The maximum radiographic severity of ARIA-H microhemorrhage in patients treated with LEQEMBI was mild in 4% (7/161) of patients and severe in 1% (2/161) of patients; 1 of the 10 patients with ARIA-H had mild superficial siderosis.
Concomitant Antithrombotic Medication and Other Risk Factors for Intracerebral Hemorrhage
- Patients were excluded from enrollment in Study 1 for baseline use of anticoagulant medications. Antiplatelet medications such as aspirin and clopidogrel were allowed. If anticoagulant medication was used because of intercurrent medical events that required treatment for ≤4 weeks, treatment with LEQEMBI was to be temporarily suspended.
- Most exposures to antithrombotic medications were to aspirin; few patients were exposed to other antiplatelet drugs or anticoagulants, limiting any meaningful conclusions about the risk of ARIA or intracerebral hemorrhage in patients taking other antiplatelet drugs or anticoagulants. Because intracerebral hemorrhages >1 cm in diameter have been observed in patients taking LEQEMBI, additional caution should be exercised when considering the administration of antithrombotics or a thrombolytic agent (e.g., tissue plasminogen activator) to a patient already being treated with LEQEMBI.
- Patients were excluded from enrollment in Study 1 for the following risk factors for intracerebral hemorrhage: prior cerebral hemorrhage >1 cm in greatest diameter, more than 4 microhemorrhages, superficial siderosis, evidence of vasogenic edema, evidence of cerebral contusion, aneurysm, vascular malformation, infective lesions, multiple lacunar infarcts or stroke involving a major vascular territory, and severe small vessel or white matter disease. Caution should be exercised when considering the use of LEQEMBI in patients with these risk factors.
Infusion-Related Reactions
- Infusion-related reactions were observed in LEQEMBI: 20% (32/161); placebo: 3% (8/245), and the majority of cases in LEQEMBI-treated patients (88%, 28/32) occurred with the first infusion. All infusion-related reactions were mild (56%) or moderate (44%) in severity. Infusion-related reactions resulted in discontinuations in 2% (4/161) of patients treated with LEQEMBI. Symptoms of infusion-related reactions included fever and flu-like symptoms (chills, generalized aches, feeling shaky, and joint pain), nausea, vomiting, hypotension, hypertension, and oxygen desaturation.
- After the first infusion, 38% of LEQEMBI-treated patients had transient decreased lymphocyte counts to <0.9 x109/L compared to 2% on placebo, and 22% of LEQEMBI-treated patients had transient increased neutrophil counts to >7.9 x109/L compared to 1% on placebo.
- In the event of an infusion-related reaction, the infusion rate may be reduced, or the infusion may be discontinued, and appropriate therapy initiated as clinically indicated. Prophylactic treatment with antihistamines, acetaminophen, nonsteroidal anti-inflammatory drugs, or corticosteroids prior to future infusions may be considered.
1. About LEQEMBITM (lecanemab-irmb)
Lecanemab (brand name in the U.S.: LEQEMBI™) is the result of a strategic research alliance between Eisai and BioArctic. Lecanemab is a humanized immunoglobulin gamma 1 (IgG1) monoclonal antibody directed against aggregated soluble (protofibril) and insoluble forms of amyloid-beta (Aβ). In the U.S., LEQEMBI was granted accelerated approval by the U.S. Food and Drug Administration (FDA) on January 6, 2023. LEQEMBI is indicated for the treatment of Alzheimer’s disease (AD) in the U.S. Treatment with LEQEMBI should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was initiated in clinical trials. There are no safety or effectiveness data on initiating treatment at earlier or later stages of the disease than were studied. This indication is approved in the U.S. under accelerated approval based on reduction in Aβ plaques observed in patients treated with LEQEMBI. Continued approval for this indication may be contingent upon verification of clinical benefit in a confirmatory trial. In the U.S., Eisai submitted a supplemental Biologics License Application (sBLA) to the FDA for approval under the traditional pathway on January 6, 2023. On March 3, 2023, the FDA accepted Eisai’s sBLA based on the Clarity AD clinical data, and the LEQEMBI application has been granted Priority Review, with a Prescription Drug User Fee Act (PDUFA) action date of July 6, 2023.
Eisai has also submitted applications for approval of lecanemab in Japan, EU, China, Canada, Great Britain and South Korea. In Japan and China, the applications have been designated for priority review, and in Great Britain, lecanemab has been designated for the Innovative Licensing and Access Pathway (ILAP), which aims to reduce the time to market for innovative medicines.
Eisai has completed lecanemab subcutaneous bioavailability study, and subcutaneous dosing is currently being evaluated in the Clarity AD (Study 301) OLE. A maintenance dosing regimen has been evaluated as part of Study 201 as well as the Clarity AD (Study 301) OLE. Separate supplemental Biologics License Applications for subcutaneous dosing and a maintenance dosing regimen will be submitted to the FDA at the end of Eisai's fiscal year.
Since July 2020 the Phase 3 clinical study (AHEAD 3-45) for individuals with preclinical AD, meaning they are clinically normal and have intermediate or elevated levels of amyloid in their brains, is ongoing. AHEAD 3-45 is conducted as a public-private partnership between the Alzheimer’s Clinical Trial Consortium that provides the infrastructure for academic clinical trials in AD and related dementias in the U.S, funded by the National Institute on Aging, part of the National Institutes of Health, Eisai and Biogen.
Since January 2022, the Tau NexGen clinical study for Dominantly Inherited AD (DIAD), that is conducted by Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU), led by Washington University School of Medicine in St. Louis, is ongoing.
2. About the Collaboration between Eisai and Biogen for AD
Eisai and Biogen have been collaborating on the joint development and commercialization of AD treatments since 2014. Eisai serves as the lead of LEQEMBI development and regulatory submissions globally with both companies co-commercializing and co-promoting the product and Eisai having final decision-making authority.
3. About the Collaboration between Eisai and BioArctic for AD
Since 2005, Eisai and BioArctic have had a long-term collaboration regarding the development and commercialization of AD treatments. Eisai obtained the global rights to study, develop, manufacture and market LEQEMBI for the treatment of AD pursuant to an agreement with BioArctic in December 2007. The development and commercialization agreement on the antibody LEQEMBI back-up was signed in May 2015.
4. About Eisai Co., Ltd.
Eisai's Corporate Concept is "to give first thought to patients and people in the daily living domain, and to increase the benefits that health care provides." Under this Concept (also known as human health care (hhc) Concept), we aim to effectively achieve social good in the form of relieving anxiety over health and reducing health disparities. With a global network of R&D facilities, manufacturing sites and marketing subsidiaries, we strive to create and deliver innovative products to target diseases with high unmet medical needs, with a particular focus in our strategic areas of Neurology and Oncology.
In addition, we demonstrate our commitment to the elimination of neglected tropical diseases (NTDs), which is a target (3.3) of the United Nations Sustainable Development Goals (SDGs), by working on various activities together with global partners.
For more information about Eisai, please visit www.eisai.com [eisai.com] (for global headquarters: Eisai Co., Ltd.), and connect with us on Twitter @Eisai_SDGs.
5. About Biogen
Founded in 1978, Biogen is a leading global biotechnology company that has pioneered multiple breakthrough innovations including a broad portfolio of medicines to treat multiple sclerosis, the first approved treatment for spinal muscular atrophy, and two co-developed treatments to address a defining pathology of Alzheimer’s disease. Biogen is advancing a pipeline of potential novel therapies across neurology, neuropsychiatry, specialized immunology and rare diseases and remains acutely focused on its purpose of serving humanity through science while advancing a healthier, more sustainable and equitable world.
The company routinely posts information that may be important to investors on its website at www.biogen.com. Follow Biogen on social media – Twitter, LinkedIn, Facebook, YouTube.
FDA panel recommends full approval for Biogen, Eisai Alzheimer's drug
Jun. 09, 2023 4:22 PM ET
Biogen Inc. (BIIB), ESALF, ESAIY
By: Val Kennedy, SA News Editor22 Comments
An advisory panel of the US Food and Drug Administration has voted unanimously to recommend full approval of Biogen (NASDAQ:BIIB) and Eisai's (OTCPK:ESALF) (OTCPK:ESAIY) Alzheimer's disease drug Leqembi, which would boost the drug's chances of being covered by Medicare.
The panel voted 6 to 0 for the drug. While the FDA is not bound to the recommendations of its expert panels, it generally follow them.
Trading of Biogen shares was halted Friday ahead of the vote.
Nirsevimab
LEQEMBI® (lecanemab-irmb)
SAR’579, ANKET®/IPH6101
Nirsevimab unanimously recommended by FDA Advisory Committee for the prevention of RSV lower respiratory tract disease in infants
PUBLISHED 8 June 2023
If approved, nirsevimab would be the first preventive option specifically designed to protect the broad infant population through its first RSV season
Across all clinical endpoints, a single dose of nirsevimab delivered consistent and sustained efficacy against RSV disease vs placebo
The US Food and Drug Administration (FDA) Antimicrobial Drugs Advisory Committee (AMDAC) has voted unanimously 21 to 0 that AstraZeneca and Sanofi’s nirsevimab has a favourable benefit risk profile for the prevention of respiratory syncytial virus (RSV) lower respiratory tract disease (LRTD) in newborns and infants born during or entering their first RSV season. The Committee also voted 19 to 2 in support of nirsevimab’s favourable benefit risk profile for children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season.
Nirsevimab has the potential to protect the broad infant population through its first RSV season, including those born healthy at term or preterm, or with specific health conditions that make them vulnerable to RSV disease. The single dose can be flexibly administered at the beginning of the RSV season or at birth for newborns born during the RSV season.
The FDA accepted the Biologics License Application (BLA) for nirsevimab in 2022 and the agency has indicated it will work to expedite its review. The Prescription Drug User Fee Act date is in the third quarter of 2023. If approved by that time, nirsevimab will be available in the US ahead of the 2023-2024 RSV season.
Dr William Muller, Associate Professor, Pediatrics, Northwestern University Feinberg School of Medicine and Scientific Director, Clinical and Community Trials, Ann & Robert H. Lurie Children’s Hospital of Chicago, Illinois, US said: “RSV remains the most common cause of bronchiolitis and pneumonia in infants, and the inability to predict which infants will develop severe RSV disease leads to uncertainty for new parents and for physicians. The innovation of nirsevimab as a long-acting antibody that can be conveniently administered to a broad infant population with a single-dose at the time protection is most needed is a significant public health advancement that could have far-reaching impact on the well-being of our families and healthcare systems in the US.”
Iskra Reic, Executive Vice President, Vaccines and Immune Therapies, AstraZeneca, said: “We are delighted that the Antimicrobial Drugs Advisory Committee has unanimously recognised the favourable benefit risk profile of nirsevimab as the first preventative option against RSV for a broad infant population. Nirsevimab builds on AstraZeneca’s strong science, leadership in RSV and commitment to addressing the needs of the most vulnerable. We look forward to continuing to work with the FDA to complete their expedited review, and we hope to see nirsevimab available as soon as possible given the significant burden of RSV in infants.”
Thomas Triomphe, Executive Vice President, Vaccines, Sanofi, said: “Most babies hospitalised with RSV are born at term and healthy, which is why interventions specifically designed to protect all infants are likely to result in the greatest impact. We are encouraged by the Advisory Committee’s positive vote based on the compelling clinical development program supporting nirsevimab and its breakthrough potential to reduce the magnitude of annual RSV burden.”
RSV is a very contagious virus that can lead to serious respiratory illness, according to the Centers for Disease Control and Prevention (CDC).1 In the US, RSV is the leading cause of hospitalisation for babies under one.2 About 75% of infants hospitalised for RSV in the US were born at term with no underlying conditions.3
The AMDAC based its recommendation on the nirsevimab clinical development programme spanning three pivotal late-stage clinical trials, including results from the MELODY Phase III trial recently published in the New England Journal of Medicine.4-8 Across all clinical endpoints, a single dose of nirsevimab demonstrated sustained and consistent reduction in RSV LRTD requiring medical care vs placebo through the entire RSV season. Nirsevimab was generally well tolerated with a favourable safety profile that was consistent across all clinical trials. The overall rates of adverse events were comparable between nirsevimab and placebo and the majority of adverse events were mild or moderate in severity. The most common adverse events were rash, fever and injection site reactions.4-10
Notes
Antimicrobial Drugs Advisory Committee (AMDAC)
AMDAC reviews and evaluates available data concerning the safety and effectiveness of marketed and investigational human drug products for use in the treatment of infectious diseases and disorders and makes appropriate recommendations to the Commissioner of Food and Drugs. The AMDAC’s recommendation, while not binding, will be considered by the FDA during its review of the BLA for nirsevimab.
RSV
RSV is a very contagious virus that can lead to serious respiratory illness for infants, according to the CDC.1 Two out of three infants are infected with RSV during their first year of life and almost all infants are infected by their second birthday.11 In the US, RSV is the leading cause of hospitalisation in infants under 12 months.2 Approximately 75% of infants hospitalised for RSV were born healthy and at term with no underlying conditions in a study conducted from 2014-2015.3 RSV symptoms can include runny nose, coughing, sneezing, fever, decrease in appetite, and wheezing.1 Each year RSV infection leads to approximately 500,000 emergency department visits in the US by children under 5 years of age, which represents 1 in 4 of all RSV-related doctor visits, according to the CDC.12
Nirsevimab
Nirsevimab is a single dose long-acting antibody, developed and commercialised in partnership by AstraZeneca and Sanofi using AstraZeneca’s YTE technology. It is designed to protect infants born during or entering their first RSV season and for children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season. Nirsevimab, provided directly to newborns and infants as a single dose, offers RSV protection via an antibody to help prevent LRTD caused by RSV. Monoclonal antibodies do not require the activation of the immune system to help offer timely, rapid and direct protection against disease.13
Nirsevimab has been granted regulatory and other designations to facilitate expedited development by several major regulatory agencies around the world. These include Breakthrough Therapy Designation and Priority Review designation by the China Center for Drug Evaluation under the National Medical Products Administration; Breakthrough Therapy Designation from the US Food and Drug Administration; access granted to the European Medicines Agency (EMA) PRIority Medicines (PRIME) scheme; and named “a medicine for prioritized development” under the Project for Drug Selection to Promote New Drug Development in Pediatrics by the Japan Agency for Medical Research and Development (AMED). Nirsevimab was approved in the European Union in October 2022.
Pivotal clinical trials
The Phase IIb study (Trial 03) was a randomised, placebo-controlled trial designed to measure the efficacy of nirsevimab against medically attended Lower Respiratory Tract Infection (LRTI) through 150 days postdose. Healthy preterm infants of 29–35 weeks’ gestation were randomised (2:1) to receive a single 50mg intramuscular injection of nirsevimab or placebo.6
The dosing regimen was recommended based on further exploration of the Phase IIb data.6 The subsequent Phase III study, MELODY (Trial 04) applied the recommended dosing regimen.4,5
The MELODY Phase III study was a randomised, placebo-controlled trial conducted across 21 countries designed to determine efficacy of nirsevimab against medically attended LRTI due to RSV confirmed by reverse transcriptase polymerase chain reaction testing through 150 days after dosing, versus placebo, in healthy late preterm and term infants (35 weeks gestational age or greater) entering their first RSV season.4,5
MEDLEY (Trial 05) was a Phase II/III, randomised, double-blind, Synagis-controlled trial with the primary objective of assessing safety and tolerability for nirsevimab in preterm infants and infants with congenital heart disease (CHD) and/or chronic lung disease of prematurity (CLD) eligible to receive Synagis.7 Between July 2019 and May 2021 approximately 918 infants entering their first RSV season were randomised to receive a single 50mg (in infants weighing <5kg) or 100mg (in infants weighing ≥5kg) intramuscular injection of nirsevimab or Synagis. Safety was assessed by monitoring the occurrence of TEAEs and TESAEs through 360 days post-dose.7 Serum levels of nirsevimab following dosing (on day 151) in this trial were comparable with those observed in the MELODY Phase III trial, indicating similar protection in this population to that in the healthy term and late preterm infants is likely.7 Data was published in the New England Journal of Medicine (NEJM) in March 2022.
The safety profile of nirsevimab was similar to Synagis in the MEDLEY Phase II/III and consistent with the safety profile in term and preterm infants studied in the MELODY Phase III trial.4,5,7 While uncommon, the most reported adverse reactions were: rash 14 days post-dose, (the majority of which were mild to moderate); pyrexia (fever) within 7 days post-dose; non-serious injection site reactions within 7 days post-dose.
The results of MELODY, MEDLEY Phase II/III and the Phase IIb trials demonstrate that a single dose of nirsevimab helps protect infants during their first RSV season against RSV disease.4-8 This broad infant population includes preterm, healthy late preterm and term infants, as well as infants with specific conditions.
These trials formed the basis of regulatory submissions which began in 2022.
Results from the MELODY Phase III trial (Trial 04)
The primary endpoint of the MELODY Phase III trial was met, reducing the incidence of medically attended LRTI, such as bronchiolitis or pneumonia, caused by RSV by 74.5% (95% CI 49.6, 87.1; P<0.001) compared to placebo. Infants were randomised (2:1) to receive a single 50mg (in infants weighing <5kg) or 100mg (in infants weighing ≥5kg) intramuscular injection of nirsevimab or placebo. Between July 2019 and March 2020, 1,490 infants were randomised to receive either nirsevimab or placebo at the RSV season start.4,5 Data was published in NEJM in March 2022.
Following the analysis of the initial 1,490 infants within the MELODY primary cohort, additional infants continued to be enrolled. A total of 3,012 healthy late preterm and term infants (35 weeks gestational age or greater) entering their first RSV season were randomised to receive nirsevimab (n=2,009) or placebo (n=1,003). In this updated analysis of the full enrolment cohort, nirsevimab demonstrated a 76.8% (95% CI: 49.4, 89.4) reduction in hospitalisation-associated RSV LRTI vs placebo. Additionally, nirsevimab reduced very severe MA RSV LRTI by 78.6% (95% CI: 48.8, 91.0) through an RSV season, and efficacy against MA RSV LRTI was consistent with previous trials (76.4%; 95% CI: 62.3, 85.2). The safety profile of nirsevimab was similar to placebo (nirsevimab, 1.3%; placebo, 1.5%).4
Sanofi Alliance
In March 2017, AstraZeneca and Sanofi announced an agreement to develop and commercialise nirsevimab. Under the terms of the agreement, AstraZeneca leads development and manufacturing activities, and Sanofi leads commercialisation activities and records revenue. The two companies share costs and profits in all territories except in the US. AstraZeneca's revenue from the agreement is reported as Alliance Revenue and Collaboration Revenue in the Company’s financial statements. Following a revision to the profit-sharing arrangement relating to the development and commercialisation of nirsevimab in the US between AstraZeneca, Sanofi and Sobi, Sobi has entered into a direct relationship with Sanofi, replacing the previous participation agreement with AstraZeneca entered into in November 2018.
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca, Sanofi win FDA advisory committee backing for RSV therapy nirsevimab
Jun. 08, 2023 7:09 PM ET
By: Anuron Mitra, SA News Editor
A U.S. Food and Drug Administration (FDA) advisory committee on Thursday voted in favor to recommend approval of Sanofi (NASDAQ:SNY) and AstraZeneca's (NASDAQ:AZN) antibody therapy to prevent respiratory syncytial virus (RSV) infection in newborn babies and infants.
The FDA's Antimicrobial Drugs Advisory Committee unanimously voted 21 to 0 in favor of using the therapy, nirsevimab, to prevent infections in newborns or infants in their first RSV season.
SAR’579, ANKET®/IPH6101
LEQEMBI® (lecanemab-irmb)
SAR’579, ANKET®/IPH6101
SAR'579 / IPH6101 RECEIVES FDA FAST TRACK DESIGNATION IN THE US FOR THE TREATMENT OF HEMATOLOGICAL MALIGNANCIES
Thu, 06/08/2023 - 07:00
- SAR’579, ANKET® platform lead asset, is a trifunctional anti-CD123 NKp46×CD16 NK cell engager from a joint research collaboration between Innate Pharma and Sanofi, now under development by partner Sanofi.
Innate Pharma SA (Euronext Paris: IPH; Nasdaq: IPHA) (“Innate” or the “Company”) is pleased to share Sanofi’s news that the U.S. Food and Drug Administration (FDA) has granted Fast Track Designation for SAR’579 / IPH6101 for the treatment of hematological malignancies.
Fast Track Designation is an FDA process designed to facilitate the development, and expedite the review of, medicines to treat serious conditions and fill unmet medical need. The FDA created this process to help deliver important new drugs to patients earlier, and it covers a broad range of serious illnesses.
SAR’579, ANKET® platform lead asset, is a trifunctional anti-CD123 NKp46×CD16 NK cell engager from a joint research collaboration between Innate Pharma and Sanofi, now under development by partner Sanofi.
“It is promising to see SAR’579 / IPH6101 was granted Fast Track Designation in the US for the treatment of hematological malignancies, and congratulate our partner Sanofi on this milestone,” said Mondher Mahjoubi, Chief Executive Officer of Innate Pharma. “In addition to the encouraging clinical data recently presented at the 2023 ASCO Annual Meeting, this FDA Fast Track Designation further validates the potential of the ANKET® platform to treat cancer patients with NK Cell Engagers.”
About ANKET®
ANKET® (Antibody-based NK cell Engager Therapeutics) is Innate's proprietary platform for developing next-generation, multi-specific natural killer (NK) cell engagers to treat certain types of cancer.
This versatile, fit-for-purpose technology is creating an entirely new class of molecules to induce synthetic immunity against cancer.
About the Innate-Sanofi agreements:
The Company has a research collaboration and license agreement with Sanofi to apply Innate’s proprietary technology to the development of innovative multi-specific antibody formats engaging NK cells through the activating receptors NKp46 and CD16 to kill tumor cells.
Under the terms of the 2016 research collaboration and license agreement, Sanofi is responsible for the development, manufacturing and commercialization of products resulting from the research collaboration, which includes IPH6101/SAR’579 (Trifunctional anti-CD123 NKp46×CD16 NK cell engager) and IPH6401/SAR’514 (Trifunctional anti-BCMA NKp46×CD16 NK cell engager). As part of the 2016 agreement, Innate Pharma will be eligible to up to €400m in development and commercial milestone payments as well as royalties on net sales.
Another license agreement was entered in December 2022, which includes IPH62 and 2 options.
Press Release in English410.67 KBCommuniqué de presse en français239.5 KB
Sanofi, Innate Pharma win FDA Fast Track tag for blood cancer drug
Jun. 08, 2023 9:05 AM ET
Innate Pharma S.A. (IPHA), SNY, SNYNF
By: Dulan Lokuwithana, SA News Editor
- Innate Pharma (NASDAQ:IPHA) added ~8% pre-market Thursday on the news that the FDA granted Fast Track Designation for SAR’579 / IPH6101, a candidate developed by the French biotech in partnership with Sanofi (NASDAQ:SNY).
- The agency has issued Fast Track Designation for SAR’579 / IPH6101 as a treatment for hematological malignancies.
- SAR’579 / IPH6101 is an antibody-based natural killer cell engager jointly developed by the two French companies under a 2016 research collaboration. According to its terms, Innate Pharma (IPHA) will receive €400m in milestone payments and royalties on net sales from drugs under the partnership.
- Innate Pharma S.A. (IPHA), SNY, SNYNF
- https://seekingalpha.com/news/3978627-sanofi-stock-innate-win-fda-fast-track-blood-cancer-drug
- https://www.innate-pharma.com/science/our-nk-cell-engager-platform
- https://www.innate-pharma.com/
biotecHOPE™ 2023
SETRUSUMAB (UX143)
SETRUSUMAB (UX143)
SETRUSUMAB (UX143)
ULTRAGENYX AND MEREO BIOPHARMA ANNOUNCE POSITIVE DATA FROM THE ONGOING PHASE 2/3 ORBIT STUDY OF SETRUSUMAB (UX143) IN OSTEOGENESIS IMPERFECTA (OI)
Jun 05, 2023
Pediatric data show substantial induction of bone production in 1 week and a large increase in bone formation within 3 months of initiating monthly setrusumab treatment
Phase 3 sites beginning to screen patients
Conference call to discuss data planned for 5 p.m. Eastern Time
NOVATO, Calif. and LONDON, June 05, 2023 (GLOBE NEWSWIRE) -- Ultragenyx Pharmaceutical Inc. (NASDAQ: RARE) and Mereo BioPharma Group plc (NASDAQ: MREO) today announced data from the dose-selection Phase 2 portion of the Phase 2/3 Orbit study showing that setrusumab rapidly induced bone production in OI-affected patients. Across all patients evaluated setrusumab demonstrated statistically significant increases in levels of serum P1NP, a sensitive marker of bone formation, and a substantial and significant improvement in bone mineral density (BMD) by 3 months.
“The rate of increasing bone mineralization we're observing on DXA scans is striking, unlike anything I have typically seen with bisphosphonate therapy. This increase in bone mass underscores the potential to make denser and stronger bone,” said Gary Gottesman, M.D., Professor of Pediatrics and Medicine, Washington University School of Medicine.
As of the data cut off, serum P1NP levels through at least 1 month of treatment were available from all 24 patients enrolled in Orbit and demonstrated that treatment with setrusumab significantly increased serum P1NP in both dosing cohorts, peaking at one to two weeks and again, as expected, after the 2-month dosing timepoint. In the 20 mg/kg cohort, there was a mean serum P1NP increase of 57% from baseline over the first month. Because of the higher baseline P1NP level in younger patients, this represents an approximate 8-fold greater increase in serum P1NP over 1 month in pediatric and adolescent patients when compared to adult OI patients. The absolute effect of setrusumab on increasing serum P1NP over the 1-month period with the 20 mg/kg dose, was approximately 80% of the effect achieved with the 40 mg/kg dose, demonstrating a dose response. Patients on placebo at the 1-month timepoint (n=4) showed no significant change in mean serum P1NP from baseline.
The large increase in BMD observed in the Orbit patient population over the first 3 months was consistent with the rapid increase in serum P1NP levels and was similar to results that took 1 year to achieve in the ASTEROID study in adult OI patients. Lumbar spine BMD data were available in 17 of 24 Orbit patients at the 3-month timepoint. Treatment with setrusumab for 3 months resulted in an increase in lumbar spine BMD from baseline of 9.4% at 20 mg/kg (n=10), which represents a substantial mean change in Z-score of +0.65. Treatment with 40 mg/kg (n=7) resulted in a 9.8% BMD increase. Patients on placebo at the 3-month timepoint (n=2) showed no significant change in BMD or change in lumbar spine Z-score.
“The dramatic lumbar spine BMD improvements in children at 3 months show that growing bones are more dynamic, and we anticipate the potential for a greater effect on bone formation and strength in younger patients with maturing bones,” said Eric Crombez, M.D., chief medical officer at Ultragenyx. “Based on the reports from study investigators, we’re encouraged by the impact setrusumab appears to be having on bone health so far.”
As of the data cut-off, there have been no treatment-related serious adverse events observed in the study. Reported adverse events have been generally consistent with those observed in the ASTEROID study and include infusion associated events, headache and sinusitis. There have been no reported hypersensitivity reactions related to setrusumab. There were no safety-related differences observed between dosing groups or age groups.
The totality of data demonstrated meaningful response in serum P1NP and BMD across both cohorts, with the majority of the effect observed at 20 mg/kg, which is the dose planned across the setrusumab Phase 3 program. Screening has begun for the Phase 3 portion of the study, which is designed to enroll approximately 195 patients at more than 40 sites across 12 countries.
Investor Conference Call and Webcast Information
Ultragenyx will host an investor conference call today, Monday, June 5, at 2 p.m. PT / 5 p.m. ET to discuss the results. The live and replayed webcast of the call will be available through the company’s website at https://ir.ultragenyx.com/events-presentations. To participate in the live call, please register by clicking on the following link (registration link), and you will be provided with dial in details. The replay of the call will be available for one year.
The Setrusumab Phase 3 Program
Ultragenyx and Mereo are developing setrusumab in pediatric and young adult patients across OI sub-types I, III and IV with two late-stage trials: the pivotal Phase 2/3 Orbit study and Phase 3 Cosmic study.
The global, seamless Phase 2/3 Orbit study is evaluating the effect of setrusumab versus placebo on fracture rate in patients aged 5 to <26 years. In the Phase 2 portion, 24 patients were randomized 1:1 to receive setrusumab at one of two doses to determine the optimal dosing strategy for Phase 3. The Orbit study was designed to be placebo-controlled, however the placebo arm was removed from the Phase 2 portion by amendment. All of the placebo patients enrolled in Phase 2 (n=4) were subsequently rerandomized to one of the dosing cohorts.
The pivotal Phase 3 portion of the study will include approximately 195 patients, randomized 2:1 to receive setrusumab or placebo, with a primary efficacy endpoint of annualized clinical fracture rate. All patients will transition to an extension period and receive open-label setrusumab after the Phase 3 primary analysis is complete.
The Phase 3 Cosmic study is an open-label, randomized, active-controlled study in patients aged 2 to <5 years evaluating setrusumab versus intravenous bisphosphonates (IV-BP) therapy on reduction in total fracture rate, including morphometric vertebral fractures. The Cosmic study is anticipated to start in the next few months and will enroll approximately 50-66 patients.
About Osteogenesis Imperfecta (OI)
Osteogenesis Imperfecta (OI) includes a group of genetic disorders impacting bone metabolism. Approximately 85% to 90% of OI cases are caused by mutations in the COL1A1 or COL1A2 genes, leading to either reduced or abnormal collagen and changes in bone metabolism. The collagen mutations in OI can result in increased bone brittleness, which contributes to a high rate of fractures, including at atypical sites. Patients with OI also exhibit increased bone resorption (breakdown of old bone) and inadequate production of new bone, which leads to decreased bone mass, bone fragility and weakness. OI can also lead to bone deformities, abnormal spine curvature, pain, decreased mobility, and short stature. No treatments are approved for OI, which affects approximately 60,000 people in the developed world.
About Setrusumab (UX143)
Setrusumab is a fully human monoclonal antibody that inhibits sclerostin, a protein that acts on a key bone-signaling pathway that inhibits the maturation and activity of bone-forming cells. The goal of blocking inhibitory effects of sclerostin is to increase new bone formation, bone mineral density and bone strength. Sclerostin inhibition also reduces excessive bone resorption, further enhancing its impact on bone density. In mouse models of OI, the use of anti-sclerostin antibodies was shown to stimulate bone formation, improve bone mass and density, and increase bone strength against fracture force testing.
Mereo BioPharma’s Phase 2b study (ASTEROID) treatment phase of the dose-finding study of setrusumab for the treatment of OI in 112 adults was concluded in 2019. The ASTEROID study demonstrated treatment with setrusumab resulted in a clear, dose-dependent and statistically significant effect on bone formation and bone density at multiple anatomical sites among adult participants with OI.
Ultragenyx and Mereo BioPharma are collaborating on the development of setrusumab globally based on the collaboration and license agreement between the parties. The companies have developed a comprehensive late-stage program to continue development of setrusumab in pediatric and young adult patients across OI sub-types I, III and IV.
About Ultragenyx Pharmaceutical Inc.
Ultragenyx is a biopharmaceutical company committed to bringing novel products to patients for the treatment of serious rare and ultrarare genetic diseases. The company has built a diverse portfolio of approved therapies and product candidates aimed at addressing diseases with high unmet medical need and clear biology for treatment, for which there are typically no approved therapies treating the underlying disease.
The company is led by a management team experienced in the development and commercialization of rare disease therapeutics. Ultragenyx’s strategy is predicated upon time- and cost-efficient drug development, with the goal of delivering safe and effective therapies to patients with the utmost urgency.
For more information on Ultragenyx, please visit the company's website at: www.ultragenyx.com.
About Mereo BioPharma
Mereo BioPharma is a biopharmaceutical company focused on the development of innovative therapeutics for rare diseases. The Company has two rare disease product candidates, setrusumab for the treatment of Osteogenesis Imperfecta (OI) and alvelestat for the treatment of severe alpha-1-antitrypsin deficiency-associated lung disease (AATD-LD) and Bronchiolitis Obliterans Syndrome (BOS). The Company’s partner, Ultragenyx Pharmaceutical, Inc., has initiated a pivotal Phase 2/3 pediatric study in young adults (5-25 years old) for setrusumab in OI and expects to initiate a study in pediatric patients (<5 years old) in the next few months. The partnership with Ultragenyx includes potential milestone payments of up to $254 million and royalties to Mereo on commercial sales in Ultragenyx territories. Mereo has retained EU and UK commercial rights and will pay Ultragenyx royalties on commercial sales in those territories. Alvelestat has received U.S. Orphan Drug Designation for the treatment of AATD, Fast Track designation from the FDA, and positive data were reported from a Phase 2 proof-of-concept study in North America, Europe and the UK. In addition to the rare disease programs, Mereo has two oncology product candidates in clinical development. Etigilimab (anti-TIGIT) has completed enrollment in a Phase 1b/2 basket study evaluating its safety and efficacy in combination with an anti-PD-1 in a range of tumor types including three rare tumors and three gynecological carcinomas - cervical, ovarian, and endometrial; navicixizumab, for the treatment of late line ovarian cancer, has completed a Phase 1 study and has been partnered with OncXerna Therapeutics, Inc. in a global licensing agreement that includes payments of up to $300 million in milestones and royalties.
For more information on Mereo BioPharma, please visit www.mereobiopharma.com
Ultragenyx, Mereo gain on Phase 2 data for bone disorder therapy
Jun. 06, 2023 8:23 AM ET
Ultragenyx Pharmaceutical Inc. (RARE)MREO
By: Dulan Lokuwithana, SA News Editor
Shares of Ultragenyx Pharmaceutical (NASDAQ:RARE) and Mereo BioPharma (MREO) gained in the pre-market Tuesday after the biotechs announced mid-stage data for setrusumab, a monoclonal antibody targeted at the bone disorder osteogenesis imperfecta (OI).
Citing data from the dose-selection Phase 2 portion of the Phase 2/3 Orbit study, the companies said that setrusumab led to a statistically significant increase in serum P1NP, an indicator of bone formation, and a sharp rise in bone mineral density (BMD) in three months.
https://seekingalpha.com/news/3977845-ultragenyx-stock-mereo-stock-gain-bone-disorder
BNT316/ONC-392
SETRUSUMAB (UX143)
SETRUSUMAB (UX143)
BioNTech and OncoC4 Present Positive Phase 1/2 Data for Antibody Candidate BNT316/ONC-392 in Hard-to-Treat NSCLC at ASCO
2 June 2023
- BNT316/ONC-392 is a next-generation anti-CTLA-4 monoclonal antibody candidate jointly developed by BioNTech and OncoC4 as monotherapy or combination therapy in a range of solid tumor indications, including non-small cell lung cancer (NSCLC)
- Interim data of BNT316/ONC-392 from the ongoing Phase 1/2 trial to be presented at this year’s ASCO Annual Meeting demonstrate encouraging signs of clinical anti-tumor activity and a manageable safety profile in patients with metastatic, PD-(L)1-resistant NSCLC
- Initiation of a pivotal Phase 3 trial with BNT316/ONC-392 as monotherapy in immunotherapy-resistant NSCLC patients is planned in Q3 2023, following FDA’s Fast Track designation in 2022
- Lung cancer remains one of the most commonly diagnosed malignant cancer types and the leading cause of cancer deaths worldwide, with NSCLC1 making up approximately 85% of all lung cancers
MAINZ, Germany, and ROCKVILLE, Maryland, USA, June 2, 2023 (GLOBE NEWSWIRE) — BioNTech SE (Nasdaq: BNTX, “BioNTech”) and OncoC4, Inc. (“OncoC4”), today announced positive preliminary data from the ongoing Phase 1/2 trial with the companies’ anti-CTLA-4 antibody candidate, BNT316/ONC-392 (gotistobart), in a patient cohort with metastatic, PD-(L)1-resistant non-small cell lung cancer (“NSCLC”). The preliminary results show encouraging clinical anti-tumor activity for BNT316/ONC-392 as a monotherapy in a hard-to-treat patient population, as well as a manageable safety profile. The data will be presented in a poster discussion session at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting by Kai He, M.D., Ph.D., Pelotonia Institute for Immuno-Oncology, The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute, Columbus, Ohio, USA.
The results featured at the ASCO Annual Meeting include a total of 27 patients with metastatic, PD-(L)1-resistant NSCLC, available for tumor response assessment who have received at least two doses of 10 mg/kg of BNT316/ONC-392. At data cut-off, the overall response rate (“ORR”) among evaluable patients was 29.6%, with a disease control rate (“DCR”) of 70.4%, including 1 complete response, 7 partial responses and 11 patients with stable disease. BNT316/ONC-392 continues to be well tolerated with a manageable safety profile. Immune-related adverse events (irAE) of Grade 3 and 4 were observed in 10 patients (30%), which is considered lower than what was reported for similar drugs.
“Metastatic NSCLC has a very poor prognosis with a 5-year survival rate of only 9%2. These new data highlight the potential of BNT316/ONC-392 to provide a new approach to leveraging CTLA-4 as an effective target to address advanced, hard-to-treat tumors, further broadening our oncology toolkit,” said Prof. Özlem Türeci, M.D., Chief Medical Officer and Co-Founder at BioNTech. “Our goal is to accelerate the development of this program in NSCLC towards pivotal Phase 3 evaluation in line with our mission of providing the optimal therapeutic strategy for each cancer patient.”
“The clinical activity and safety profile validate the improved therapeutic index of BNT316/ONC-392,” said Pan Zheng, M.D., Ph.D. Chief Medical Officer and Co-Founder at OncoC4. “We are especially encouraged by the readouts from the PD-(L)1-resistant NSCLC. Responses were observed regardless of PD-L1 status, and among those who failed multiple lines of immunotherapy and chemotherapy, including PD-1 and CTLA-4 combination therapy.”
Lung cancer remains one of the most commonly diagnosed malignant cancer types and the leading cause of cancer deaths worldwide, with NSCLC1 making up approximately 85% of all lung cancers. The new data further support the initiation of a pivotal Phase 3 study with BNT316/ONC-392 as monotherapy for immunotherapy-resistant NSCLC, for which the candidate received Fast Track designation from the U.S. Food and Drug Administration (“FDA”) in 2022. The Phase 3 trial, PRESERVE-003 (NCT05671510), is planned to start in Q3 2023.
About BNT316/ONC-392
BNT316/ONC-392 (gotistobart) is a next-generation anti-CTLA-4 antibody candidate jointly developed by BioNTech and OncoC4. BNT316/ONC-392 is currently in late-stage clinical development as monotherapy or combination therapy in various cancer indications. The immune checkpoint receptor CTLA-4 inhibits T cell immune response and reduces the activity of T cells in recognizing and eliminating cancer cells. Blocking CTLA-4 preserves T cell activity and enhances anti-tumor activity. BNT316/ONC-392 was designed to preserve CTLA-4 recycling and thus immunosuppressive T cells (regulatory T cells, or “Tregs”) function in the peripheral tissues. This aims to give rise to fewer immune-related adverse effects and a more favorable safety profile. BNT316/ONC-392 is currently being evaluated in an ongoing Phase 1/2 trial (NCT04140526) in patients with advanced solid tumors as single agent or in combination with pembrolizumab. In addition, the candidate is also being evaluated in an additional Phase 2 trial as a combination therapy with pembrolizumab in platinum-resistant ovarian cancer (NCT05446298).
About NSCLC
Non-small cell lung cancer (NSCLC) covers all epithelial lung cancers other than small cell lung cancer and includes squamous cell carcinoma, large cell carcinoma, and adenocarcinoma. It is the most common type of lung cancer, accounting for up to 85% of cases1, with risk factors ranging from smoking to asbestos exposure and pulmonary fibrosis3. With a 5-year relative survival rate of 23% in the United States (2012-2018), NSCLC is a devastating disease with limited treatment options depending on the stage and location of the tumor.3 Current standard of care includes surgery and radiotherapy in combination with chemotherapy.3
About BioNTech
Biopharmaceutical New Technologies (BioNTech) is a next generation immunotherapy company pioneering novel therapies for cancer and other serious diseases. The Company exploits a wide array of computational discovery and therapeutic drug platforms for the rapid development of novel biopharmaceuticals. Its broad portfolio of oncology product candidates includes individualized and off-the-shelf mRNA-based therapies, innovative chimeric antigen receptor T cells, bispecific immune checkpoint modulators, targeted cancer antibodies and small molecules. Based on its deep expertise in mRNA vaccine development and in-house manufacturing capabilities, BioNTech and its collaborators are developing multiple mRNA vaccine candidates for a range of infectious diseases alongside its diverse oncology pipeline. BioNTech has established a broad set of relationships with multiple global pharmaceutical collaborators, including Genmab, Sanofi, Genentech, a member of the Roche Group, Regeneron, Genevant, Fosun Pharma and Pfizer.
For more information, please visit www.BioNTech.com.
About OncoC4
Based in Rockville, Maryland, OncoC4 is a privately held, late clinical-stage biopharmaceutical company that is actively engaged in the discovery and development of novel biologicals for cancer treatment. Its lead clinical candidate is ONC-392, a next generation anti-CTLA-4 antibody that allows CTLA-4 to recycle and maintain its protective function against autoimmune diseases while enhancing anti-tumor activity at the same time. In addition, OncoC4 has a pipeline of first-in-class preclinical product candidates focusing on the CD24-Siglecs cancer immune evasion pathway.
More information: www.oncoc4.com.
BioNTech reports promising data on BNT316, Phase 3 trial slated for Q3
Jun. 02, 2023 9:59 AM ET
By: Val Kennedy, SA News Editor3 Comments
BioNTech (NASDAQ:BNTX) reported promising data from a mid-stage clinical study for its therapy candidate BNT316/ONC-392 in the treatment of metastatic non-small cell lung cancer, or NSCLC, the most prevalent form of the disease.
The German biotech company said preliminary data from a Phase 1/2 study showed anti-tumor activity was observed in 29.6% of the patients who took the anti-CTLA-4 antibody therapy, with the drug largely well tolerated. The trial consisted of 27 patients with metastatic PD-L1-resistant NSCLC.
https://www.biontech.com/int/en/home/pipeline-and-products/pipeline.html
VCA-894A
SETRUSUMAB (UX143)
Imetelstat
Vanda Pharmaceuticals Announces Orphan Drug Designation Granted for VCA-894A, a Novel Antisense Oligonucleotide Candidate for the Treatment of Charcot-Marie-Tooth Disease, Type 2S
June 2, 2023 WASHINGTON, June 1, 2023 /PRNewswire/ -- Vanda Pharmaceuticals Inc. (Vanda) (Nasdaq: VNDA) today announced the U.S. Food and Drug Administration (FDA) has granted Orphan Drug Designation for VCA-894A for the treatment of Charcot-Marie-Tooth disease, axonal, type 2S (CMT2S), caused by cryptic splice site variants within IGHMBP2. CMT2S is a rare subtype of Charcot-Marie-Tooth disease (CMT), an inherited peripheral neuropathy for which there is no available treatment. The estimated prevalence of CMT is 1 in 2,500 individuals, with varying clinical features dependent on the various genetic variants of CMT.1,2 The prevalence of CMT2S is estimated to be less than 1 in 1,000,000 worldwide.3 Onset of CMT2S begins in early childhood.2 CMT2S is characterized by slowly progressive distal muscle weakness and atrophy, affecting the upper and lower limbs in a child's first decade of life, leaving patients with decreased reflexes and sensory impairment.1,2 Because CMT2S is a progressive disease, most patients become wheelchair bound. "This designation is an important milestone, which we believe may enable the development of individualized treatments tailored to one's genetic variants for patients with CMT2S," said Mihael H. Polymeropoulos, M.D., Vanda's President, CEO and Chairman of the Board. VCA-894A is a novel antisense oligonucleotide (ASO) with a mechanism of action that specifically targets a cryptic splice site variant within immunoglobulin mu-binding protein 2 (IGHMBP2). Mutations within IGHMBP2 play a pivotal role in the manifestation of CMT2S, likely due to alpha-motor neuron loss, and consequently peripheral nervous system deterioration.4 ASOs have the capacity to modulate gene expression, allowing for the personalized treatment of rare diseases. Delivery of ASOs to the central nervous system has been previously successful in several ASO programs, with a broad applicability in addressing a number of neurodegenerative and neuromuscular disorders.5 Orphan Drug Designation is granted by the FDA to investigational therapies addressing rare medical conditions and provides benefits to drug developers.
About Vanda Pharmaceuticals Inc. Vanda is a leading global biopharmaceutical company focused on the development and commercialization of innovative therapies to address high unmet medical needs and improve the lives of patients. For more on Vanda Pharmaceuticals Inc., please visit www.vandapharma.com and follow us on Twitter @vandapharma. About VCA-894A VCA-894A is a 2'-O-methoxyethyl (MOE) phosphorothioate oligonucleotide sodium salt. VCA-894A specifically targets a cryptic splice site variant within IGHMBP2, which causes CMT2S. ASOs may have broad applicability in addressing a number of disorders, from nervous system treatments to systemic treatments.
SOURCE Vanda Pharmaceuticals Inc.
Vanda gains on FDA orphan drug designation for nerve disorder candidate
Jun. 02, 2023 3:15 PM ET
Vanda Pharmaceuticals Inc. (VNDA)
By: Dulan Lokuwithana, SA News Editor
Vanda Pharmaceuticals (NASDAQ:VNDA) gained after three straight sessions of declines on Friday after announcing that the FDA granted Orphan Drug Designation for its experimental therapy VCA-894A as a treatment for a type of rare nerve disorder called Charcot-Marie-Tooth disease (CMT).
VCA-894A is an antisense oligonucleotide that targets immunoglobulin mu-binding protein 2 (IGHMBP2), mutations of which are thought to play a key role in causing a subtype of CMT called CMT type 2S (CMT2S).
https://seekingalpha.com/news/3977334-vanda-stock-wins-fda-orphan-drug-tag-nerve-disorder-drug
Vanda Pharmaceuticals Inc. (VNDA)
Imetelstat
Repotrectinib
Imetelstat
Geron Announces ASCO Presentation Reporting Durable Continuous Transfusion Independence with Imetelstat in IMerge Phase 3 Lower Risk MDS Patients
06/02/2023
PDF Format (opens in new window)
- Primary endpoint of 8-week transfusion independence (TI) significantly higher with imetelstat vs. placebo (P<0.001), with median TI duration approaching one year for imetelstat 8-week TI responders
- Statistically significant and clinically meaningful efficacy results achieved across key MDS subgroups: ring sideroblast (RS) status, baseline transfusion burden and IPSS risk category
- Safety results consistent with prior imetelstat clinical experience
- Reduction in variant allele frequency (VAF) of genes commonly mutated in MDS and their correlation with clinical endpoints support disease-modifying potential of imetelstat
- Data support NDA submission which is on track for June 2023 to support potential U.S. commercial launch in first half of 2024
FOSTER CITY, Calif.--(BUSINESS WIRE)-- Geron Corporation (Nasdaq: GERN), a late-stage clinical biopharmaceutical company, announced a presentation reporting durable continuous transfusion independence with imetelstat, the Company’s first-in-class telomerase inhibitor, in IMerge Phase 3 lower risk MDS patients. These data were presented today at the American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago, IL.
“The presentation at ASCO of our IMerge Phase 3 data highlighted the meaningful longer-term duration of transfusion independence with imetelstat compared to placebo, as well as significantly higher rates of TI across MDS subgroups, greater reductions in transfusion units and sustained increases in hemoglobin levels,” said Faye Feller, M.D., Executive Vice President, Chief Medical Officer of Geron. “With our U.S. New Drug Application based on these data on track to be submitted to the FDA this month, I look forward to the day when imetelstat could be available for lower risk MDS patients in the first half of 2024.”
IMerge Phase 3 enrolled lower risk MDS patients who were relapsed after, refractory to, or ineligible for erythropoiesis stimulating agent (ESA) treatment and were transfusion dependent, defined as requiring at least four units of packed red blood cells (RBCs) over an eight-week period. The ASCO presentation reported IMerge Phase 3 results with a data cut-off of October 2022, the same for top-line results reported in January 2023. The primary endpoint of 8-week transfusion independence (TI) was met with high statistical significance (P<0.001) for imetelstat-treated patients (39.8%) vs. placebo (15.0%). Of the imetelstat 8-week responders, 83% had a single continuous TI period. Highly statistically significant (P<0.001; hazard ratio 0.23) durable transfusion independence for 8-week TI responders was achieved with a median TI duration approaching one year for imetelstat, compared to approximately 13 weeks for placebo. The key secondary endpoint of 24-week TI was also met with high statistical significance (P<0.001) for imetelstat-treated patients (28.0%) vs. placebo (3.3%).
Mean hemoglobin levels in imetelstat-treated patients increased significantly (P<0.001) over time compared to placebo patients. For patients achieving 8-week TI, median increases in hemoglobin were 3.6 g/dL for imetelstat and 0.8 g/dL for placebo. Imetelstat-treated patients also experienced a statistically significant (P=0.042) and clinically meaningful mean reduction in RBC transfusion units compared to placebo. A highly statistically significant (P<0.001) hematologic improvement-erythroid (HI-E) rate was achieved for imetelstat (42.4%) versus placebo (13.3%) using the IWG 2018 criteria for HI-E.
Significantly higher 8-week TI rates were observed with imetelstat vs. placebo across key lower risk MDS subgroups, including ring sideroblast (RS) status, baseline transfusion burden and IPSS risk category, with similar 8-week TI responses seen for imetelstat within each subgroup category.
“The IMerge Phase 3 results are especially encouraging because of the significant unmet need in lower risk MDS patients with symptomatic anemia needing regular red blood cell transfusions, especially with less than half of such patients responding to frontline ESA therapy, and most of those who do respond losing that response in less than two years,” said Amer Methqal Zeidan, MBBS MHS, Associate Professor of Internal Medicine (Hematology) and director of hematology Early Therapy Research at Yale School of Medicine and Yale Cancer Center, who presented the data at ASCO and is an IMerge lead investigator. “Based on the IMerge trial results, I believe imetelstat represents an important and novel option for patients with lower risk MDS after ESA failure, particularly in terms of the high response rate, durability of response, significant and sustained hemoglobin increase in responders, the preliminary evidence of disease modification across the mutational spectrum of the disease and considering the manageable and reversible adverse event profile. This potential treatment option is especially important for patients with high transfusion burden and those without ring sideroblasts who have high unmet need.”
The safety profile observed with imetelstat in IMerge Phase 3 was consistent with prior clinical experience with no new safety signals. Non-hematologic adverse events (AEs) were generally low grade. No cases of Hy’s Law or drug-induced liver injury were observed, and the incidence of grade 3 liver function test laboratory abnormalities was similar between imetelstat and placebo groups. Grade 3-4 thrombocytopenia and neutropenia were the most frequently reported hematologic AEs and were most often reported during Cycles 1-3. These cytopenias resolved within two weeks, and over 80% of events were reversible to grade 2 or lower within 4 weeks. There were no fatal hematologic AEs or cytopenic events. Clinical consequences of grade 3-4 infection and bleeding were low and similar between imetelstat and placebo groups.
Most AEs leading to dose modifications were grade 3-4 neutropenia and thrombocytopenia. Although approximately 75% of patients treated with imetelstat had dose modifications due to AEs, less than 15% of patients discontinued treatment due to treatment-emergent adverse events (TEAE). Discontinuation of imetelstat treatment in these patients due to a TEAE generally occurred late in treatment, with a median time to treatment discontinuation of 21.1 weeks (range 2.3 to 44.0 weeks).
Reductions in variant allele frequency (VAF) of genes frequently mutated in MDS were greater for imetelstat-treated patients vs. placebo: SF3B1 (P< 0.001), TET2 (P= 0.032), DNMT3A (P= 0.019) and ASXL1 (P=0.146). SF3B1 VAF reduction correlated with a greater increase in hemoglobin (P< 0.001) and longer TI duration (P< 0.001). A greater VAF reduction in TET2, DNMT3A or ASXL1 also correlated with longer TI duration. Such correlations support the disease-modifying potential of imetelstat.
The presentation slides are available on the Publications section of Geron’s website: https://www.geron.com/research-and-development/publications/.
About IMerge Phase 3
The Phase 3 portion of the IMerge Phase 2/3 study is a double-blind, 2:1 randomized, placebo-controlled clinical trial to evaluate imetelstat in patients with IPSS Low or Intermediate-1 risk (lower risk) transfusion dependent MDS who were relapsed after, refractory to, or ineligible for, erythropoiesis stimulating agent (ESA) treatment, had not received prior treatment with either a HMA or lenalidomide and were non-del(5q). To be eligible for IMerge Phase 3, patients were required to be transfusion dependent, defined as requiring at least four units of packed red blood cells (RBCs), over an eight-week period during the 16 weeks prior to entry into the trial. The primary efficacy endpoint of IMerge Phase 3 is the rate of red blood cell transfusion independence (RBC-TI) lasting at least eight weeks, defined as the proportion of patients without any RBC transfusion for at least eight consecutive weeks since entry to the trial (8-week TI). Key secondary endpoints include the rate of RBC-TI lasting at least 24 weeks (24-week TI), the duration of TI and the rate of hematologic improvement erythroid (HI-E), which is defined under 2006 IWG criteria as a rise in hemoglobin of at least 1.5 g/dL above the pretreatment level for at least eight weeks or a reduction of at least four units of RBC transfusions over eight weeks compared with the prior RBC transfusion burden. A total of 178 patients were enrolled in IMerge Phase 3 across North America, Europe, Middle East and Asia.
About Imetelstat
Imetelstat is a novel, first-in-class telomerase inhibitor exclusively owned by Geron and being developed in hematologic malignancies. Data from non-clinical studies and clinical trials of imetelstat provide strong evidence that imetelstat targets telomerase to inhibit the uncontrolled proliferation of malignant stem and progenitor cells in myeloid hematologic malignancies resulting in malignant cell apoptosis and potential disease-modifying activity. Imetelstat has been granted Fast Track designation by the U.S. Food and Drug Administration for both the treatment of adult patients with transfusion dependent anemia due to Low or Intermediate-1 risk MDS that is not associated with del(5q) who are refractory or resistant to an erythropoiesis stimulating agent, and for adult patients with Intermediate-2 or High-risk MF whose disease has relapsed after or is refractory to janus associated kinase (JAK) inhibitor treatment. Geron plans to submit a New Drug Application (NDA) in the U.S. in June 2023 and a Marketing Authorization Application (MAA) in the EU in the second half of 2023 in the lower risk MDS indication.
About Geron
Geron is a late-stage biopharmaceutical company pursuing therapies with the potential to extend and enrich the lives of patients living with hematologic malignancies. Our first-in-class telomerase inhibitor, imetelstat, harnesses Nobel Prize-winning science in a treatment that may alter the underlying drivers of disease. Geron currently has two Phase 3 pivotal clinical trials underway evaluating imetelstat in lower risk myelodysplastic syndromes (LR MDS), and in relapsed/refractory myelofibrosis (MF). To learn more, visit www.geron.com or follow us on LinkedIn.
Source: Geron Corporation
Multimedia Files:
 Download:Download original 249 KB 1806 x 886Download thumbnail 7 KB 200 x 98Download lowres 31 KB 480 x 235Download square 11 KB 250 x 250
Download:Download original 249 KB 1806 x 886Download thumbnail 7 KB 200 x 98Download lowres 31 KB 480 x 235Download square 11 KB 250 x 250
Geron reports positive late-stage data on imetelstat in myelodysplastic syndromes
Jun. 02, 2023 4:55 PM ET
By: Jonathan Block, SA News Edito
- Geron's (NASDAQ:GERN) imetelstat for lower risk myelodysplastic syndromes led to increased transfusion independence compared to those on placebo and also increased mean hemoglobin levels in a phase 3 trial.
- Results from the IMerge study found that at week 8, transfusion independence for imetelstat-treated patients was 39.8% compared to 15% for placebo.
- https://seekingalpha.com/news/3977366-geron-positive-late-stage-data-imetelstat-myelodysplastic-syndromes
- Geron Corporation (GERN)
- https://www.geron.com/research-and-development/imetelstat/
Roxadustat
Repotrectinib
Repotrectinib
FibroGen Announces Positive Topline Results from China Pivotal Phase 3 Clinical Trial of Roxadustat for the Treatment of Chemotherapy Induced Anemia
- Met primary endpoint of noninferiority of roxadustat to erythropoietin alfa
- Plan to file supplemental New Drug Application in China
SAN FRANCISCO and BEIJING, May 18, 2023 (GLOBE NEWSWIRE) -- FibroGen, Inc. (NASDAQ: FGEN) and its subsidiary, FibroGen (China) Medical Technology Development Co., Ltd. today announced positive topline data from Company’s Phase 3 clinical study of roxadustat for treatment of anemia in patients receiving concurrent chemotherapy treatment for non-myeloid malignancies in China.
Roxadustat (爱瑞卓®) demonstrated non-inferiority compared to recombinant erythropoietin alfa (SEPO®) on the primary endpoint of change in hemoglobin (Hb) level from baseline to the average level during weeks 9-13.
In the preliminary safety analysis, the adverse event profile of roxadustat was generally consistent with previous findings and supportive of a positive benefit risk in this patient population.
“Roxadustat is a promising potential new oral drug for treating chemotherapy-induced anemia, which complicates the treatment of many cancer patients,” said Mark D. Eisner, MD, MPH, Chief Medical Officer, FibroGen. “Chemotherapy-induced anemia remains an unmet medical need in China, and we believe that roxadustat has potential to improve the lives of these patients.”
A total of one-hundred fifty-nine (159) patients with non-myeloid malignancy (solid tumor) with a baseline hemoglobin level at or below 10 g/dL were enrolled into this Phase 3, randomized, open-label, active-controlled study investigating the efficacy and safety of roxadustat for treatment of chemotherapy-induced anemia (CIA). Patients were randomly assigned roxadustat or erythropoietin alfa three times per week (TIW), during a treatment period of 12 weeks, with an additional 4-week follow-up period. The primary endpoint of the study was change in hemoglobin level from baseline to the average level during weeks 9-13. For more information regarding this study, please visit www.clinicaltrials.gov (NCT05301517).
Detailed results from the study will be submitted for presentation at an upcoming medical conference.
This Phase 3 study is sponsored and conducted by FibroGen and is part of the collaboration with AstraZeneca. FibroGen will work with AstraZeneca and the China Health Authority to file the supplemental New Drug Application.
About Chemotherapy-Induced Anemia
Although chemotherapy-induced anemia is one of the most common side effects of chemotherapy, it is often not recognized and is frequently undertreated. CIA can adversely affect long-term patient outcomes, as anemia limits both quality of life and efficacy of chemotherapy treatment. The incidence and severity of CIA depends on a variety of factors. This includes the type of cancer and the treatment, including the type of chemotherapy, schedule, and intensity of therapy. It also depends on whether the patient has received prior myelosuppressive chemotherapy, radiation therapy, or both. An estimated 30% to 90% of cancer patients receiving chemotherapy develop anemia; and in China the figure approaches 80%1. Approximately 650,000 cancer patients undergo chemotherapy every year in the United States. In China, over 3 million cancer patients undergo chemotherapy2.
About Roxadustat
Roxadustat, an oral medication, is the first in a new class of medicines comprising HIF-PH inhibitors that promote erythropoiesis, or red blood cell production, through increased endogenous production of erythropoietin, improved iron absorption and mobilization, and downregulation of hepcidin. Roxadustat is in clinical development for chemotherapy-induced anemia (CIA) in China.
Roxadustat is approved in China, Europe, Japan, and numerous other countries for the treatment of anemia of CKD in adult patients on dialysis (DD) and not on dialysis (NDD). Several other licensing applications for roxadustat have been submitted by partners, Astellas and AstraZeneca to regulatory authorities across the globe, and are currently under review. Astellas and FibroGen are collaborating on the development and commercialization of roxadustat for the potential treatment of anemia in territories including Japan, Europe, Turkey, Russia and the Commonwealth of Independent States, the Middle East, and South Africa. FibroGen and AstraZeneca are collaborating on the development and commercialization of roxadustat for the potential treatment of anemia in the U.S., China, and other markets not licensed to Astellas.
About FibroGen
FibroGen, Inc. is a biopharmaceutical company committed to discovering, developing, and commercializing a pipeline of first-in-class therapeutics. The Company applies its pioneering expertise in connective tissue growth factor (CTGF) biology and hypoxia-inducible factor (HIF) to advance innovative medicines for the treatment of unmet needs. Pamrevlumab, an anti-CTGF human monoclonal antibody, is in clinical development for the treatment of idiopathic pulmonary fibrosis (IPF), locally advanced unresectable pancreatic cancer (LAPC), metastatic pancreatic cancer, and Duchenne muscular dystrophy (DMD). Roxadustat (爱瑞卓®, EVRENZOTM) is currently approved in China, Europe, Japan, and numerous other countries for the treatment of anemia in CKD patients on dialysis and not on dialysis. Roxadustat is in clinical development for chemotherapy-induced anemia (CIA) in China. FibroGen recently expanded its research and development portfolio to include product candidates in the immuno-oncology space. For more information, please visit www.fibrogen.com.
![]()
Source: FibroGen, Inc.
Redefining How to Treat Anemia in Chronic Kidney Disease
We are advancing roxadustat, our first-in-class, oral small molecule product candidate for the treatment of anemia associated with chronic kidney disease (CKD), through global Phase 3 clinical development.
Roxadustat, a hypoxia-inducible factor prolyl hydroxylase (HIF-PH) inhibitor, promotes coordinated erythropoiesis through increasing endogenous erythropoietin, improving iron availability, and reducing hepcidin. Administration of roxadustat has been shown to increase red blood cell production while maintaining plasma erythropoietin levels within or near normal physiologic range in multiple subpopulations of CKD patients, including in the presence of inflammation, and without a need for supplemental intravenous iron.
Roxadustat is approved in China, Europe, Japan, and numerous other countries for the treatment of anemia in chronic kidney disease (CKD) patients on dialysis and patients not on dialysis. Several other licensing applications for roxadustat have been submitted by partners, Astellas and AstraZeneca to regulatory authorities across the globe, and are currently under review. The U.S. Food and Drug Administration issued a complete response letter for the roxadustat NDA filing for the treatment of CKD anemia in August 2021. Roxadustat is in Phase 3 clinical development in China for treatment of chemotherapy-induced anemia (CIA).
Additional information about roxadustat trials currently recruiting patients can be found at
https://www.fibrogen.com/roxadustat
Repotrectinib
Repotrectinib
Repotrectinib
U.S. Food and Drug Administration Accepts for Priority Review Bristol Myers Squibb’s Application for Repotrectinib for the Treatment of Patients with Locally Advanced or Metastatic ROS1-Positive Non-Small Cell Lung Cancer
05/30/2023
CATEGORY:
Application based on results from the registrational TRIDENT-1 trial, in which repotrectinib demonstrated high response rates and durable responses in patients with ROS1-positive locally advanced or metastatic non-small cell lung cancer
If approved, repotrectinib will provide a potential best-in-class option for patients with ROS1-positive NSCLC who are TKI-naïve and a potential first-in-class treatment for patients who have been treated with prior TKI
The U.S. Food and Drug Administration assigned a target action date of November 27, 2023
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE: BMY) today announced that the U.S. Food and Drug Administration (FDA) has accepted the New Drug Application (NDA) for repotrectinib, a next-generation tyrosine kinase inhibitor (TKI), for the treatment of patients with ROS1-positive locally advanced or metastatic non-small cell lung cancer (NSCLC), based on results from the TRIDENT-1 trial. The FDA granted the application Priority Review and assigned a Prescription Drug User Fee Act (PDUFA) goal date of November 27, 2023.
“Patients with ROS1-positive non-small cell lung cancer face a rare disease with a significant unmet medical need given the limited durability of benefit and emergence of resistance to approved therapies,” said Jonathan Cheng, M.D., senior vice president and head of oncology development, Bristol Myers Squibb. “The FDA’s acceptance of this application marks an exciting milestone on our journey to bring this next-generation tyrosine kinase inhibitor to patients. If approved, this would represent a potential best-in-class option for TKI-naïve patients and a potential first-in-class option for patients with ROS1-positive NSCLC who have been previously treated with TKI, and for whom there are currently no approved targeted therapies available. We are eager to continue working closely with the FDA on the review of this precision medicine, which has shown unprecedented level of durability of responses and robust intracranial responses in patients with ROS1-positive NSCLC.”
The filing was based on results from the registrational TRIDENT-1 study. In the trial, repotrectinib demonstrated high response rates and clinically meaningful durability of benefit in both TKI-naïve and TKI-pretreated patients, including those with ROS1 resistance mutations. The safety profile of repotrectinib was well characterized and manageable. Results from TRIDENT-1 were most recently presented at the 2022 EORTC-NCI-AACR (ENA) Symposium. The study remains ongoing to assess long-term outcomes and additional endpoints across patient populations with ROS1-positive locally advanced or metastatic NSCLC and NTRK-positive advanced solid tumors. Bristol Myers Squibb thanks the patients and investigators involved with the TRIDENT-1 clinical trial.
Turning Point Therapeutics is a wholly owned subsidiary of the Bristol-Myers Squibb Company. As of August 2022, Bristol Myers Squibb acquired the leading clinical stage precision oncology company and its pipeline of investigational drugs across precision oncology and advanced solid tumors, including repotrectinib.
About TRIDENT-1
TRIDENT-1 is a Phase 1/2 open-label, global, multi-center, first-in-human clinical trial evaluating the safety, tolerability, pharmacokinetics and anti-tumor activity of repotrectinib (TPX-0005, BMS-986472) in patients with advanced solid tumors, including non-small cell lung cancer (NSCLC).Phase 1 of the trial includes several primary and secondary safety and pharmacokinetics endpoints. Phase 2 of the trial has a primary endpoint of overall response rate (ORR) as assessed by Blinded Independent Central Review (BICR) using RECIST v1.1 and key secondary endpoints including duration of response (DOR), time to response (TTR), progression-free survival (PFS), overall survival (OS) and clinical benefit rate (CBR) in six distinct expansion cohorts, including tyrosine kinase inhibitor (TKI)-naïve and TKI-pretreated patients with ROS1-positive locally advanced or metastatic NSCLC and NTRK-positive advanced solid tumors.
About Lung Cancer
Lung cancer is the leading cause of cancer deaths globally. Non-small cell lung cancer (NSCLC) is one of the most common types of lung cancer, representing up to 84% of diagnoses. Survival rates vary depending on the stage and type of the cancer when diagnosed. ROS1 fusions are rare and occur in about 1-2% of patients with NSCLC. Patients with tumors that are ROS1-positive tend to be younger than the average patient with lung cancer, more often female and may have little to no smoking history. Per international treatment guidelines, ROS1 targeted agents are preferred in patients with a tumor harboring this alteration.
Bristol Myers Squibb: Creating a Better Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision — transforming patients’ lives through science. The goal of the company’s cancer research is to deliver medicines that offer each patient a better, healthier life and to make cure a possibility. Building on a legacy across a broad range of cancers that have changed survival expectations for many, Bristol Myers Squibb researchers are exploring new frontiers in personalized medicine, and through innovative digital platforms, are turning data into insights that sharpen their focus. Deep scientific expertise, cutting-edge capabilities and discovery platforms enable the company to look at cancer from every angle. Cancer can have a relentless grasp on many parts of a patient’s life, and Bristol Myers Squibb is committed to taking actions to address all aspects of care, from diagnosis to survivorship. Because as a leader in cancer care, Bristol Myers Squibb is working to empower all people with cancer to have a better future.
About Repotrectinib
Repotrectinib (TPX-0005, BMS-986472) is a next-generation, potential best-in-class tyrosine kinase inhibitor (TKI) targeting ROS1- or NTRK-positive locally advanced or metastatic solid tumors, including non-small cell lung cancer (NSCLC), where there remain significant unmet medical needs for patients. Repotrectinib was designed to improve durability of response and with favorable properties for human brain penetration to enhance intracranial activity. It is being studied in a registrational Phase 1/2 trial primarily in adults and a Phase 1/2 trial in pediatric patients.
In June 2017, repotrectinib was granted an Orphan Drug designation by the U.S. Food and Drug Administration (FDA). Since then, repotrectinib has demonstrated clinically meaningful results and was granted three Breakthrough Therapy Designations (BTDs) by the FDA for the treatment of patients with: ROS1-positive metastatic NSCLC who have not been treated with a ROS1 TKI; ROS1-positive metastatic NSCLC who have been previously treated with one ROS1 TKI and who have not received prior platinum-based chemotherapy; and advanced solid tumors that have an NTRK gene fusion who have progressed following treatment with one or two prior tropomyosin receptor kinase (TRK) TKIs (with or without prior chemotherapy) and have no satisfactory alternative treatments.
Repotrectinib was also previously granted four fast-track designations in patients with: ROS1-positive advanced NSCLC who have been treated with disease progression following one prior line of platinum-based chemotherapy and one prior line of a ROS1 TKI; ROS1-positive advanced NSCLC who have not been treated with a ROS1 TKI; ROS1-positive advanced NSCLC who have been previously treated with one ROS1 TKI and who have not received prior platinum-based chemotherapy; and advanced solid tumors that have an NTRK gene fusion who have progressed following treatment with at least one prior line of chemotherapy and one or two prior TRK TKIs and have no satisfactory alternative treatments.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
Multimedia Files:
 Download:Download original 99 KB 1505 x 211Download thumbnail 5 KB 200 x 28Download lowres 15 KB 480 x 67Download square 7 KB 250 x 250
Download:Download original 99 KB 1505 x 211Download thumbnail 5 KB 200 x 28Download lowres 15 KB 480 x 67Download square 7 KB 250 x 250
Bristol Myers granted FDA priority review for lung cancer therapy
May 30, 2023 7:42 AM ET
Bristol-Myers Squibb Company (BMY)
By: Dulan Lokuwithana, SA News Editor
- Bristol Myers Squibb (NYSE:BMY) announced Tuesday that the FDA accepted its New Drug Application (NDA) for repotrectinib, a tyrosine kinase inhibitor (TKI) for lung cancer, granting the priority review for its marketing application.
- The agency has assigned a Prescription Drug User Fee Act (PDUFA) goal date of November 27, 2023, to finalize its decision.
- https://seekingalpha.com/news/3975738-bristol-myers-stock-wins-fda-review-lung-cancer-drug
- Bristol-Myers Squibb Company (BMY)
- https://www.bms.com/
- https://www.bms.com/researchers-and-partners/in-the-pipeline.html
Lifileucel
Eftilagimod Alpha (Efti)
Lifileucel
Iovance Biotherapeutics Announces U.S. Food and Drug Administration Acceptance of the Biologics License Application of Lifileucel for the Treatment of Advanced Melanoma
Priority Review Granted with
Prescription Drug User Fee Act (PDUFA) Action Date of November 25, 2023
First Potential Approval of an Individualized, One-Time Cell Therapy
for Patients with Advanced Melanoma
SAN CARLOS, Calif., May 26, 2023 (GLOBE NEWSWIRE) -- Iovance Biotherapeutics, Inc. (NASDAQ: IOVA), a biotechnology company focused on innovating, developing, and delivering novel polyclonal tumor infiltrating lymphocyte (TIL) therapies for patients with cancer, today announced that the U.S. Food and Drug Administration (FDA) accepted its Biologics License Application (BLA) for lifileucel for patients with advanced melanoma. The FDA granted lifileucel Priority Review and assigned November 25, 2023 as the target action date for a decision under the Prescription Drug User Fee Act (PDUFA). The FDA is not currently planning to hold an advisory committee meeting to discuss this application and, after a preliminary review, has not at this time identified any potential review issues.
Lifileucel is a TIL therapy intended for patients with advanced melanoma who progressed on or after prior anti-PD-1/L1 therapy and targeted therapy, where applicable. There are no FDA approved therapies in this treatment setting. Under the FDA’s guidance, Priority Review allows for an six-month review from the time of BLA acceptance for treatments that, if approved, are substantially safer or more effective than standard of care therapies. The FDA also previously granted a Regenerative Medicine Advanced Therapy (RMAT) designation for lifileucel in advanced melanoma.
Frederick Vogt, Ph.D., J.D., Interim President and Chief Executive Officer of Iovance, stated, “The BLA acceptance is a significant milestone in our mission to deliver lifileucel as the first individualized, one-time cell therapy for a solid tumor. The FDA’s commitment to a six-month Priority Review validates the unmet need and urgency for new treatment options for patients with advanced melanoma who have progressed on or after standard of care therapies. I am grateful for the patients and physicians who took part in all our clinical trials, as well as the Iovance team for their outstanding work on our first BLA filing. We look forward to continuing our collaboration with the FDA during the BLA review cycle, while continuing to execute our pre-commercialization activities and advancing our robust TIL pipeline.”
The BLA submission for lifileucel is supported by positive data from the C-144-01 clinical trial in patients with advanced melanoma who progressed on or after prior anti-PD-1/L1 therapy and targeted therapy, where applicable. If lifileucel receives accelerated approval, the randomized Phase 3 TILVANCE-301 trial in frontline advanced melanoma can serve as the confirmatory study to support full approval. TILVANCE-301 is expected to be well underway at the time of approval.
About Iovance Biotherapeutics, Inc.
Iovance Biotherapeutics aims to be the global leader in innovating, developing and delivering tumor infiltrating lymphocyte (TIL) therapies for patients with cancer. We are pioneering a transformational approach to cure cancer by harnessing the human immune system’s ability to recognize and destroy diverse cancer cells in each patient. Our lead late-stage TIL product candidate, lifileucel for metastatic melanoma, has the potential to become the first approved one-time cell therapy for a solid tumor cancer. The Iovance TIL platform has demonstrated promising clinical data across multiple solid tumors. We are committed to continuous innovation in cell therapy, including gene-edited cell therapy, that may extend and improve life for patients with cancer. For more information, please visit www.iovance.com.
![]()
Source: Iovance Biotherapeutics, Inc.
Iovance up 15% on FDA acceptance of lifileucel application for melanoma
May 26, 2023 6:25 PM ET
Iovance Biotherapeutics, Inc. (IOVA)
By: Jonathan Block, SA News Editor22 Comments
- The US FDA has accepted Iovance Biotherapeutics' (NASDAQ:IOVA) Biologics License Application for lifileucel for advanced melanoma, sending shares up ~15% in after-hours trading Friday.
- The candidate has an FDA action date of Nov. 25 as it was granted Priority Review. In addition, the agency is not planning to hold an advisory committee meeting on the application.
- https://seekingalpha.com/news/3975576-iovance-up-15-fda-acceptance-lifileucel-application-melanoma
- Iovance Biotherapeutics, Inc. (IOVA)
- https://www.iovance.com/uploads/Iovance_ASCO-2021_COM-202-Coh1A.pdf
- https://www.iovance.com/
Imetelstat
Eftilagimod Alpha (Efti)
Lifileucel
Geron Oral Presentation at Upcoming ASCO Annual Meeting to Highlight Meaningful Continuous Transfusion Independence Observed in Imetelstat-Treated Lower Risk MDS Patients in IMerge Phase 3
05/25/2023
Download this Press ReleasePDF Format (opens in new window)
- Data support NDA submission which is on track for June 2023 to support potential U.S. commercial launch in first half of 2024
FOSTER CITY, Calif.--(BUSINESS WIRE)-- Geron Corporation (Nasdaq: GERN), a late-stage clinical biopharmaceutical company, today announced acceptance of its IMerge Phase 3 abstract as an oral presentation at the upcoming 2023 American Society of Clinical Oncology (ASCO) Annual Meeting. This abstract describes statistically significant positive efficacy and safety data from the pivotal IMerge Phase 3 clinical trial evaluating the Company’s first-in-class telomerase inhibitor, imetelstat, in lower risk myelodysplastic syndromes (MDS). These data support the Company’s planned New Drug Application (NDA) submission to the U.S. FDA which is on track for June 2023, to support a potential U.S. commercial launch of imetelstat in lower risk MDS in the first half of 2024.
“We believe that imetelstat has the potential to be practice-changing in lower risk MDS based on the unprecedented durability of transfusion independence, as well as broad activity across a range of disease subtypes in IMerge Phase 3,” said Faye Feller, M.D., Executive Vice President, Chief Medical Officer of Geron. “We are thrilled that these data will be featured in an oral presentation at ASCO, where we will have a significant medical affairs presence to bring more awareness to the continuing unmet need in lower risk MDS and very much look forward to meaningful engagement with the medical community.”
Details for the oral presentation are as follows:
Abstract #:7004
Title:IMerge: “Results from a Phase 3, Randomized, Double-Blind, Placebo-Controlled Study of Imetelstat in Patients (pts) With Heavily Transfusion Dependent (TD) Non-Del(5q) Lower-Risk Myelodysplastic Syndromes (LR-MDS) Relapsed/Refractory (R/R) to Erythropoiesis Stimulating Agents (ESA).”
Date/Time:June 2, 2023 at 2:12 p.m. CT
Session:“Hematologic Malignancies—Leukemia, Myelodysplastic Syndromes, and Allotransplant”
Presenter:Amer Methqal Zeidan, Yale School of Medicine
The abstract recaps top-line results from IMerge Phase 3 with a data cut-off of October 2022. As reported in January 2023, the primary endpoint of 8-week transfusion independence (TI) was met with high statistical significance (P<0.001) for imetelstat-treated patients (39.8%) vs. placebo (15.0%). Key secondary endpoint of 24-week TI and hematologic improvement erythroid (HI-E) under 2018 IWG criteria were also met with high statistical significance (P<0.001 for each) for imetelstat-treated patients vs. placebo.
In addition, the rate of 8-week TI was significantly higher with imetelstat vs. placebo across subgroups, including ring sideroblast (RS) negative patients. Median TI duration was significantly longer for imetelstat-treated patients vs. those on placebo (51.6 vs 13.3 weeks, P< 0.001). Patients receiving imetelstat had significantly higher mean hemoglobin (P < 0.001) and fewer transfusions (P = 0.042) over time than those on placebo.
In three of four genes frequently mutated in MDS, variant allele frequency (VAF) reduction was significantly greater in patients treated with imetelstat than placebo: SF3B1 (P< 0.001), TET2 (P= 0.032), DNMT3A (P= 0.019) and ASXL1 (P= NS). SF3B1 VAF reduction correlated with longer TI duration (P< 0.001).
No new safety signals were identified. The most common Grade 3/4 adverse events (AEs) were thrombocytopenia and neutropenia, with similar rates of Grade ≥3 bleeding and infections on imetelstat and placebo. In patients treated with imetelstat, cytopenias were manageable, of short duration, and > 80% were reversible to Grade ≤2 within 4 weeks.
The abstract concludes that for this lower risk MDS patient population: imetelstat demonstrated statistically significant and clinically meaningful efficacy with high 8- and 24-week TI rates, prolonged TI duration and increased hemoglobin. Also, VAF reduction and its correlation to clinical endpoints support imetelstat’s disease-modifying potential, and safety results were consistent with prior reported experience.
Full text of the abstract is available at www.asco.org.
About IMerge Phase 3
The Phase 3 portion of the IMerge Phase 2/3 study is a double-blind, 2:1 randomized, placebo-controlled clinical trial to evaluate imetelstat in patients with IPSS Low or Intermediate-1 risk (lower risk) transfusion dependent MDS who were relapsed after, refractory to, or ineligible for, erythropoiesis stimulating agent (ESA) treatment, had not received prior treatment with either a HMA or lenalidomide and were non-del(5q). To be eligible for IMerge Phase 3, patients were required to be transfusion dependent, defined as requiring at least four units of packed red blood cells (RBCs), over an eight-week period during the 16 weeks prior to entry into the trial. The primary efficacy endpoint of IMerge Phase 3 is the rate of red blood cell transfusion independence (RBC-TI) lasting at least eight weeks, defined as the proportion of patients without any RBC transfusion for at least eight consecutive weeks since entry to the trial (8-week TI). Key secondary endpoints include the rate of RBC-TI lasting at least 24 weeks (24-week TI), the duration of TI and the rate of hematologic improvement erythroid (HI-E), which is defined under 2006 IWG criteria as a rise in hemoglobin of at least 1.5 g/dL above the pretreatment level for at least eight weeks or a reduction of at least four units of RBC transfusions over eight weeks compared with the prior RBC transfusion burden. A total of 178 patients were enrolled in IMerge Phase 3 across North America, Europe, Middle East and Asia.
About Imetelstat
Imetelstat is a novel, first-in-class telomerase inhibitor exclusively owned by Geron and being developed in hematologic malignancies. Data from non-clinical studies and clinical trials of imetelstat provide strong evidence that imetelstat targets telomerase to inhibit the uncontrolled proliferation of malignant stem and progenitor cells in myeloid hematologic malignancies resulting in malignant cell apoptosis and potential disease-modifying activity. Imetelstat has been granted Fast Track designation by the U.S. Food and Drug Administration for both the treatment of adult patients with transfusion dependent anemia due to Low or Intermediate-1 risk MDS that is not associated with del(5q) who are refractory or resistant to an erythropoiesis stimulating agent, and for adult patients with Intermediate-2 or High-risk MF whose disease has relapsed after or is refractory to janus associated kinase (JAK) inhibitor treatment. Geron plans to submit a New Drug Application (NDA) in the U.S. in June 2023 and a Marketing Authorization Application (MAA) in the EU in the second half of 2023 in the lower risk MDS indication.
About Geron
Geron is a late-stage biopharmaceutical company pursuing therapies with the potential to extend and enrich the lives of patients living with hematologic malignancies. Our first-in-class telomerase inhibitor, imetelstat, harnesses Nobel Prize-winning science in a treatment that may alter the underlying drivers of disease. Geron currently has two Phase 3 pivotal clinical trials underway evaluating imetelstat in lower risk myelodysplastic syndromes (LR MDS), and in relapsed/refractory myelofibrosis (MF). To learn more, visit www.geron.com or follow us on LinkedIn.
Source: Geron Corporation
Multimedia Files:
 Download:Download original 249 KB 1806 x 886Download thumbnail 7 KB 200 x 98Download lowres 31 KB 480 x 235Download square 11 KB 250 x 250
Download:Download original 249 KB 1806 x 886Download thumbnail 7 KB 200 x 98Download lowres 31 KB 480 x 235Download square 11 KB 250 x 250
Geron on track for imetelstat myelodysplastic syndromes NDA submission in June
May 25, 2023 5:56 PM ET
By: Jonathan Block, SA News Editor5 Comments
- Geron (NASDAQ:GERN) said that its planned New Drug Application for imetelstat for lower risk myelodysplastic syndromes is on track for submission in June.
- The company noted that an abstract of phase 3 data that is supporting the application was accepted for an oral presentation at the American Society of Clinical Oncology Annual Meeting next month.
- Geron (GERN) is eying a potential US launch in H1 2024.
- https://seekingalpha.com/news/3975291-geron-imetelstat-myelodysplastic-syndromes-nda-submission-june
- Geron Corporation (GERN)
- https://www.geron.com/
Eftilagimod Alpha (Efti)
Eftilagimod Alpha (Efti)
Eftilagimod Alpha (Efti)
Immutep Doses First Patient in AIPAC-003 Phase II/III Trial for Metastatic Breast Cancer
May 25th 2023
Print / PDF
Media Release
SYDNEY, AUSTRALIA, May 25, 2023 -- Immutep Limited (ASX: IMM; NASDAQ: IMMP) ("Immutep” or “the Company”), a clinical-stage biotechnology company developing novel LAG-3 immunotherapies for cancer and autoimmune disease, today announces the first patient has been enrolled and safely dosed at a European clinical site for its integrated Phase II/III AIPAC-003 trial in metastatic breast cancer.
AIPAC-003 is evaluating eftilagimod alpha (“efti”), Immutep’s soluble LAG-3 protein and first-in-class MHC Class II agonist, in combination with standard-of-care paclitaxel for the treatment of metastatic HER2-neg/low breast cancer and triple-negative breast cancer. It will take place at approximately 17 clinical sites across Europe and the United States of America. Patients will receive same-day administration of efti + paclitaxel that can continue until disease progression.
Immutep CSO, Prof Frédéric Triebel said: “Commencing patient dosing for our AIPAC-003 trial of efti is a significant milestone for Immutep. Our aim is to improve clinical outcomes, focusing on a robust primary endpoint later in the phase III, overall survival, for patients with standard-of-care chemotherapy. Our previous trial, AIPAC, showed encouraging efficacy and safety results, including a 2.9-month median overall survival benefit and statistically significant median overall survival improvements of between 4.2 to 19.6 months across three pre-specified subgroups. We look forward to seeing how 90mg efti dosing, along with same-day administration of efti plus paclitaxel until disease progression, may build upon these prior results.”
AIPAC-003 includes an open-label lead-in of up to 12 patients dosed at 90mg efti, which will be followed by a randomized (1:1) portion of the Phase II consisting of up to 58 evaluable patients who will receive 30mg efti or 90mg efti to determine the optimal biological dose in combination with paclitaxel. Depending on the Phase II results, potential regulatory actions and resources, a randomized, double-blinded, placebo-controlled Phase III portion will then follow. The Phase III will have overall survival as the primary objective and may include a specific patient population.
About Eftilagimod Alpha (Efti)
Efti is Immutep’s proprietary soluble LAG-3 protein and MHC Class II agonist that stimulates both innate and adaptive immunity for the treatment of cancer. As a first-in-class antigen presenting cell (APC) activator, efti binds to MHC (major histocompatibility complex) Class II molecules on APC leading to activation and proliferation of CD8+ cytotoxic T cells, CD4+ helper T cells, dendritic cells, NK cells, and monocytes. It also upregulates the expression of key biological molecules like IFN-ƴ and CXCL10 that further boost the immune system’s ability to fight cancer.
Efti is under evaluation for a variety of solid tumours including non-small cell lung cancer (NSCLC), head and neck squamous cell carcinoma (HNSCC), and metastatic breast cancer. Its favourable safety profile enables various combinations, including with anti-PD-[L]1 immunotherapy and/or chemotherapy. Efti has received Fast Track Designation in 1st line HNSCC and in 1st line NSCLC from the United States Food and Drug Administration (FDA).
About Immutep
Immutep is a clinical stage biotechnology company developing novel LAG-3 immunotherapy for cancer and autoimmune disease. We are pioneers in the understanding and advancement of therapeutics related to Lymphocyte Activation Gene-3 (LAG-3), and our diversified product portfolio harnesses its unique ability to stimulate or suppress the immune response. Immutep is dedicated to leveraging its expertise to bring innovative treatment options to patients in need and to maximise value for shareholders. For more information, please visit www.immutep.com.
Immutep rises ~15% as eftilagimod combo shows promise in phase 1 lung cancer trial
May 24, 2023 9:22 AM ET
By: Ravikash, SA News Editor1 Comment
Immutep (NASDAQ:IMMP) said its drug eftilagimod alpha plus standard-of-care anti-PD-1 therapy and doublet chemotherapy in first line non-small cell lung cancer (NSCLC) was well tolerated and showed promising initial signals of efficacy in a phase 1 trial.
INO-3107
Toripalimab in Combination with Chemotherapy
Eftilagimod Alpha (Efti)
INOVIO Announces Orphan Drug Designation for INO-3107 for the Treatment of Recurrent Respiratory Papillomatosis from the European Commission
May 23, 2023
DownloadPDF Format (opens in new window)
PLYMOUTH MEETING, Pa., May 23, 2023 /PRNewswire/ -- INOVIO (NASDAQ:INO), a biotechnology company focused on developing and commercializing DNA medicines to help treat and protect people from HPV-related diseases, cancer, and infectious diseases, today announced that the European Commission (EC) has granted orphan drug designation for INO-3107, the company's product candidate for the treatment of Recurrent Respiratory Papillomatosis (RRP). INO-3107 is an investigational DNA medicine candidate designed to elicit a targeted T cell response against HPV-6 and HPV-11, the HPV types that cause RRP and other HPV-related diseases.
INOVIO previously announced that the European Committee for Orphan Medicinal Products (COMP) had provided a positive opinion on INOVIO's application for orphan drug designation in the European Union (EU) for INO-3107. The adoption of this decision by the EC formalizes INO-3107 as a designated orphan drug in the EU. INO-3107 received orphan drug designation from the U.S. Food and Drug Administration (FDA) in July 2020, making it the first RRP product candidate to receive designations from both U.S. and EU regulatory bodies.
"By granting orphan drug designation, U.S. and EU regulators are acknowledging the high unmet medical need of those suffering from this debilitating disease," said INOVIO's Senior Vice President of Regulatory Affairs, Dr. Cheryl Elder. "This is yet another important step forward for our development process and for the RRP patients around the world who could benefit from a potentially game-changing therapy."
Orphan drug designation is granted for the treatment, prevention, or diagnosis of diseases that are life-threatening or chronically debilitating and affect no more than five in 10,000 people across the European Union (EU). Medicines that are granted orphan drug designation by the EC qualify for financial and regulatory incentives including protocol assistance at reduced charges, access to centralized marketing authorization, and up to 10 years of market exclusivity in the EU after product approval.
About RRP
RRP is a debilitating and rare disease caused primarily by HPV-6 and/or HPV-11. RRP is characterized by the development of small, wart-like growths, or papillomas, in the respiratory tract. While papillomas are generally benign, they can cause severe, life-threatening airway obstruction and respiratory complications. RRP can also significantly affect quality of life for patients by affecting the voice box, limiting the ability to speak effectively. Surgery to remove papillomas is the standard of care for RRP; however, the papillomas often grow back because the underlying HPV infection has not been eradicated.
About INO-3107
INO-3107 is INOVIO's clinical-stage DNA medicine product candidate being developed as a potential treatment for RRP. INO-3107 is designed to elicit a targeted T cell response against HPV-6 and HPV-11, the HPV types responsible for causing RRP among other HPV-related diseases. These targeted T cells are designed to seek out and kill infected cells, with the aim of potentially preventing or slowing the growth of new papillomas. INO-3107 received orphan drug designation from the U.S. Food and Drug Administration (FDA) in July 2020. For more information about INOVIO's HPV franchise, please visit https://ir.inovio.com/events-and-presentations/default.aspx
About INOVIO
INOVIO is a biotechnology company focused on developing and commercializing DNA medicines to help treat and protect people from HPV-related diseases, cancer, and infectious diseases. INOVIO's DNA medicines in development are delivered using its investigational proprietary smart device, CELLECTRA®, to produce immune responses against targeted pathogens and cancers. For more information, visit www.inovio.com.
View original content:https://www.prnewswire.com/news-releases/inovio-announces-orphan-drug-designation-for-ino-3107-for-the-treatment-of-recurrent-respiratory-papillomatosis-from-the-european-commission-301832688.html
SOURCE INOVIO Pharmaceuticals, Inc.
Inovio wins orphan drug status for HPV-related candidate in Europe
May 23, 2023 4:34 PM ET
Inovio Pharmaceuticals, Inc. (INO)
By: Jonathan Block, SA News Editor
- The European Commission has granted Orphan Drug designation to Inovio Pharmaceuticals' (NASDAQ:INO) INO-3107 for recurrent respiratory papillomatosis.
- The monoclonal antibody is designed to provoke a targeted T cell response against HPV-6 and HPV-11, the HPV types that cause the disease.
- https://seekingalpha.com/news/3974367-inovio-wins-orphan-drug-status-hpv-related-candidate-europe
- Inovio Pharmaceuticals, Inc. (INO)
- https://inovio.com/dna-medicines-pipeline/
RGX-121 Gene Therapy
Toripalimab in Combination with Chemotherapy
Toripalimab in Combination with Chemotherapy
REGENXBIO Receives FDA Regenerative Medicine Advanced Therapy (RMAT) Designation for RGX-121 Gene Therapy for Hunter Syndrome
May 23, 2023 at 7:05 AM EDT
- RMAT recognizes that the preliminary clinical evidence from RGX-121, a potential one-time AAV Therapeutic, indicates the potential to address unmet medical needs for MPS II
- RMAT designation is for gene therapies intended to treat or cure serious condition in order to expedite the drug development and review processes
- CAMPSIITE™ trial is enrolling MPS II patients as part of a pivotal program that incorporates material from the NAVXpress™ platform process manufactured at the REGENXBIO Manufacturing Innovation Center and continues to support plan to file Biologics License Application in 2024 using the accelerated approval pathway
ROCKVILLE, Md., May 23, 2023 /PRNewswire/ -- REGENXBIO Inc. (Nasdaq: RGNX) today announced that the U.S. Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation for RGX-121, an investigational one-time AAV Therapeutic for the treatment of Mucopolysaccharidosis Type II (MPS II), also known as Hunter syndrome. RMAT designation is designed to expedite the drug development and review processes for promising new treatments, including gene therapies, and recognizes that the preliminary clinical evidence from RGX-121 indicates its potential to address unmet medical needs for MPS II. RGX-121 is currently being studied in the CAMPSIITE™ trial that is enrolling MPS II patients as part of a pivotal program that incorporates material from the NAVXpress™ platform process manufactured at the REGENXBIO Manufacturing Innovation Center and continues to support plans to file Biologics License Application (BLA) in 2024 using the accelerated approval pathway.
"We are pleased that the FDA has granted RMAT designation for RGX-121 for its potential to address the neurological manifestations of MPS II and prevent or stabilize cognitive decline, which remains a significant unmet need for this community," said Steve Pakola, M.D., Chief Medical Officer of REGENXBIO. "This is an important regulatory milestone, and we remain on track to complete enrollment of CAMPSIITE in the first half of 2023 to support a BLA filing in 2024 using the accelerated approval pathway."
Established under the 21st Century Cures Act, a drug is eligible for RMAT designation if it is intended to treat, modify, reverse or cure a serious or life-threatening disease or condition, and preliminary clinical evidence indicates that the drug or therapy has the potential to address unmet medical needs for such disease or condition.
RMAT designation includes the benefits of early FDA interactions to discuss surrogate or intermediate endpoints, potential ways to support accelerated approval and satisfy post-approval requirements, potential priority review of the BLA and other opportunities to expedite development and review. In addition, sponsors of products that have been granted RMAT designation and which received accelerated approval may be able to fulfill the post-approval requirements from clinical evidence obtained from sources other than the traditional confirmatory clinical trials.
"Severe Hunter syndrome is a progressively debilitating disorder that affects a child's physical and mental development and leads to a shortened lifespan, and I applaud the FDA for granting RMAT designation to RGX-121," said Joseph Muenzer, M.D., Ph.D., Director, Muenzer MPS Research and Treatment Center, Bryson Distinguished Professor in Pediatrics Genetics, University of North Carolina at Chapel Hill. "I am encouraged by the FDA's recognition of the potential of a gene therapy like RGX-121 to improve the quality of life for boys with severe Hunter syndrome and the urgent need for new treatment options."
"We know that families are waiting for new treatment options for this serious disease and that every day matters," said Terri Klein, President and Chief Executive Officer, National MPS Society. "The expedited development of new treatment options like RGX-121 are critical to families facing this devastating diagnosis."
RGX-121 Program Highlights
The Phase I/II/III CAMPSIITE™ trial of RGX-121 for MPS II patients aged 4 months up to 5 years is ongoing and in February 2023, REGENXBIO announced additional interim data from the Phase I/II part of the trial, demonstrating that RGX-121 continued to be well-tolerated across 15 patients. Patients receiving the pivotal program dose level continued to demonstrate the largest reductions in CSF GAGs, including Heparin Sulfate (HS) and HS D2S6, which approached normal levels at 48 weeks. CSF GAGs have the potential to be considered a surrogate biomarker that is reasonably likely to predict clinical benefit in MPS II disease under the accelerated approval pathway, as buildup of GAGs in the CSF of MPS II patients correlates with clinical manifestations, including neurodevelopmental deficits. In addition, improvements in neurodevelopmental and daily activity skill acquisition were observed up to three years after RGX-121 administration.
A Phase I/II trial of RGX-121 for the treatment of pediatric patients with MPS II over the age of five years old is also ongoing.
About RGX-121
RGX-121 is designed to use the NAV® AAV9 vector to deliver the human iduronate-2-sulfatase gene (IDS) which encodes the iduronate-2-sulfatase (I2S) enzyme to the central nervous system (CNS). Delivery of the IDS gene within cells in the CNS could provide a permanent source of secreted I2S beyond the blood-brain barrier, allowing for long-term cross correction of cells throughout the CNS. RGX-121 has received Orphan Drug Product, Rare Pediatric Disease, Fast Track and Regenerative Medicine Advanced Therapy designations from the U.S. Food and Drug Administration.
About Mucopolysaccharidosis Type II (MPS II)
MPS II, or Hunter Syndrome, is a rare, X-linked recessive disease caused by a deficiency in the lysosomal enzyme iduronate-2-sulfatase (I2S) leading to an accumulation of glycosaminoglycans (GAGs), including heparan sulfate (HS) in tissues which ultimately results in cell, tissue, and organ dysfunction, including in the central nervous system (CNS). MPS II is estimated to occur in 1 in 100,000 to 170,000 births. In severe forms of the disease, early developmental milestones may be met, but developmental delay is readily apparent by 18 to 24 months. Specific treatment to address the neurological manifestations of MPS II remains a significant unmet medical need. Key biomarkers of I2S enzymatic activity in MPS II patients include its substrate heparan sulfate (HS) D2S6, which has been shown to correlate with neurocognitive manifestations of the disorder.
About REGENXBIO Inc.
REGENXBIO is a leading clinical-stage biotechnology company seeking to improve lives through the curative potential of gene therapy. REGENXBIO's NAV Technology Platform, a proprietary adeno-associated virus (AAV) gene delivery platform, consists of exclusive rights to more than 100 novel AAV vectors, including AAV7, AAV8 and AAV9. REGENXBIO and its third-party NAV Technology Platform Licensees are applying the NAV Technology Platform in the development of a broad pipeline of candidates, including late-stage and commercial programs, in multiple therapeutic areas. REGENXBIO is committed to a "5x'25" strategy to progress five AAV Therapeutics from our internal pipeline and licensed programs into pivotal-stage or commercial products by 2025.

View original content to download multimedia:HTTPS://WWW.PRNEWSWIRE.COM/NEWS-RELEASES/REGENXBIO-RECEIVES-FDA-REGENERATIVE-MEDICINE-ADVANCED-THERAPY-RMAT-DESIGNATION-FOR-RGX-121-GENE-THERAPY-FOR-HUNTER-SYNDROME-301831944.HTML
SOURCE REGENXBIO Inc.
Regenxbio's gene therapy for Hunter syndrome gets FDA regenerative medicine status
May 23, 2023 8:00 AM ET
By: Ravikash, SA News Editor
The U.S. Food and Drug Administration (FDA) granted Regenerative Medicine Advanced Therapy (RMAT) designation to Regenxbio's (NASDAQ:RGNX) one-time gene therapy RGX-121 to treat Mucopolysaccharidosis Type II (MPS II), also known as Hunter syndrome.
Toripalimab in Combination with Chemotherapy
Toripalimab in Combination with Chemotherapy
Toripalimab in Combination with Chemotherapy
Junshi Biosciences Announces Acceptance of the Supplemental NDA for Toripalimab in Combination with Chemotherapy for Advanced Triple-negative Breast Cancer
May 23, 2023 1:53 AM ET
SHANGHAI, China, May 23, 2023 (GLOBE NEWSWIRE) -- Shanghai Junshi Biosciences Co., Ltd (“Junshi Biosciences”, HKEX: 1877; SSE: 688180), a leading innovation-driven biopharmaceutical company dedicated to the discovery, development, and commercialization of novel therapies, announced that the National Medical Products Administration (“NMPA”) has accepted the supplemental new drug application ("sNDA”) for the company’s anti-PD-1 monoclonal antibody, toripalimab, used in combination with albumin-bound paclitaxel for the treatment of PD-L1 positive (CPS ≥ 1) untreated metastatic or recurrent metastatic triple-negative breast cancer (“TNBC”).
According to GLOBOCAN 2020, breast cancer exhibited the highest incidence rates worldwide, with 2.26 million new cases and 0.68 million deaths in 2020. In China, 0.42 million new cases and 0.12 million deaths due to breast cancer were reported in 2020, accounting for 18.4% and 17.1% of global cases, respectively. Amongst these breast cancer cases, approximately 10% to 15% were classified as TNBC. TNBC is a more aggressive type of cancer with a higher risk of recurrence and a poor prognosis. Unfortunately, advanced TNBC does not respond well to targeted therapy and endocrine therapy, and there are currently no specific treatment methods available.
In recent years, clinical studies have shown that immunotherapy in combination with chemotherapy for the treatment of advanced TNBC can achieve better efficacy and tolerability. To this day, however, no immunotherapy drugs have been approved for advanced TNBC in China, and chemotherapy remains the primary treatment option. Alternative drugs include anthracyclines, taxanes, platinum-based drugs, etc. Both mono-chemotherapy and combination chemotherapy have poor efficacy, with a median survival time of about 9 to 12 months and a 5-year survival rate of less than 30%.
The supplemental new drug application is based on the TORCHLIGHT study (NCT04085276), which is a randomized, double-blind, placebo-controlled, multi-center Phase III clinical study jointly conducted across 56 centers nationwide, with Professor Zefei JIANG from the Department of Oncology of the Chinese People’s Liberation Army General Hospital and Vice President and Secretary General of the Chinese Society of Clinical Oncology (CSCO), serving as the principal investigator. The study was designed to compare the efficacy and safety of toripalimab combined with albumin-bound paclitaxel versus placebo combined with albumin-bound paclitaxel in patients with an initial diagnosis of stage IV or recurrent metastatic TNBC. In February 2023, the Independent Data Monitoring Committee (IDMC) determined in an interim analysis that the primary endpoint of the TORCHLIGHT study had met its pre-defined efficacy boundary.
TORCHLIGHT study is the first domestic Phase III registered study to achieve positive results in advanced TNBC immunotherapy. The study results showed that, compared with albumin-bound paclitaxel alone, toripalimab in combination with albumin-bound paclitaxel in patients with an initial diagnosis of stage IV or recurrent metastatic triple-negative breast cancer could significantly prolong the progression-free survival (“PFS”) of PD-L1 positive patients. Meanwhile, the overall survival (“OS”), one of the secondary endpoints, also showed a clear trend of improvement in PD-1 positive patients as well as in all patients, regardless of PD-1 status. The safety profile of toripalimab is consistent with known checkpoint inhibitor-related risks, and no new safety signals were identified.
Details of the TORCHLIGHT results will be published in the form of a “Late-breaking Abstract (LBA)” (#LBA1013) oral presentation during the rapid abstract session at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting.
“Over 2 million breast cancer cases occur annually, making it the most prevalent cancer worldwide,” said Professor Zefei JIANG from the Department of Oncology of the Chinese People’s Liberation Army General Hospital. “While advancements in breast cancer treatment have continued to improve patient prognosis, TNBC remains a challenging subtype characterized by its aggressive nature and poor prognosis. Effective treatment methods for TNBC are still lacking, and the 5-year survival rate for advanced TNBC patients falls below 30%. In our TORCHLIGHT study, we combined chemotherapy with an immune checkpoint inhibitor, which resulted in significantly prolonged PFS in TNBC patients, along with other significant survival benefits. I am delighted to see the acceptance of the NDA for toripalimab in combination with chemotherapy for the treatment of advanced TNBC. I eagerly anticipate its approval as it will provide better treatment options for TNBC patients in China!”
“For a very long time, the treatment of advanced TNBC has been incredibly challenging, and TNBC has posed a constant threat to patients’ lives,” said Dr. Jianjun ZOU, the Global Research and Development President of Junshi Biosciences. “We at Junshi Biosciences have remained steadfast in our patient-centric approach and successfully collaborated with researchers on the TORCHLIGHT study, which has demonstrated significant improvements in PFS and OS. We plan to work closely with regulatory authorities to expedite the approval process and address the unmet needs of countless TNBC patients in China as soon as possible.”
About Toripalimab
Toripalimab is an anti-PD-1 monoclonal antibody developed for its ability to block PD-1 interactions with its ligands, PD-L1 and PD-L2, and for enhanced receptor internalization (endocytosis function). Blocking PD-1 interactions with PD-L1 and PD-L2 promotes the immune system’s ability to attack and kill tumor cells.
More than forty company-sponsored toripalimab clinical studies covering more than fifteen indications have been conducted globally by Junshi Biosciences, including in China, the United States, Southeast Asia, and Europe. Ongoing or completed pivotal clinical trials evaluating the safety and efficacy of toripalimab cover a broad range of tumor types, including cancers of the lung, nasopharynx, esophagus, stomach, bladder, breast, liver, kidney and skin.
In China, toripalimab was the first domestic anti-PD-1 monoclonal antibody approved for marketing (approved in China as TUOYI®). Currently, there are six approved indications for toripalimab in China:
- unresectable or metastatic melanoma after failure of standard systemic therapy;
- recurrent or metastatic nasopharyngeal carcinoma (“NPC”) after failure of at least two lines of prior systemic therapy;
- locally advanced or metastatic urothelial carcinoma that failed platinum-containing chemotherapy or progressed within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy;
- in combination with cisplatin and gemcitabine as the first-line treatment for patients with locally recurrent or metastatic NPC;
- in combination with paclitaxel and cisplatin in first-line treatment of patients with unresectable locally advanced/recurrent or distant metastatic esophageal squamous cell carcinoma ("ESCC");
- in combination with pemetrexed and platinum as the first-line treatment in EGFR mutation-negative and ALK mutation-negative, unresectable, locally advanced or metastatic non-squamous non-small cell lung cancer (NSCLC).
The first three indications have been included in the National Reimbursement Drug List (NRDL) (2022 Edition). Toripalimab is the only anti-PD-1 monoclonal antibody included in the NRDL for the treatment of melanoma.
In the United States, the Biologics License Application (BLA) for toripalimab in combination with gemcitabine/cisplatin for the first-line treatment of patients with advanced recurrent or metastatic NPC and toripalimab monotherapy for the second-line or later treatment of recurrent or metastatic NPC after platinum-containing chemotherapy is under review by the U.S. Food and Drug Administration (“FDA”). The FDA has granted Breakthrough Therapy designations for toripalimab in combination with chemotherapy for the first-line treatment of recurrent or metastatic NPC as well as for toripalimab monotherapy in the second or third-line treatment of recurrent or metastatic NPC. Additionally, the FDA has granted Fast Track designation for toripalimab for the treatment of mucosal melanoma and Orphan Drug designations for the treatment of esophageal cancer, NPC, mucosal melanoma, soft tissue sarcoma, and small cell lung cancer (SCLC).
In Europe, marketing authorization applications (MAA) were accepted by the European Medicines Agency (EMA) and the United Kingdom’s Medicines and Healthcare products Regulatory Agency (MHRA) for 1) toripalimab combined with cisplatin and gemcitabine for the first-line treatment of patients with locally recurrent or metastatic NPC and 2) toripalimab combined with paclitaxel and cisplatin for the first-line treatment of patients with unresectable locally advanced/recurrent or metastatic ESCC, in December 2022 and February 2023.
About Junshi Biosciences
Founded in December 2012, Junshi Biosciences (HKEX: 1877; SSE: 688180) is an innovation-driven biopharmaceutical company dedicated to the discovery, development, and commercialization of innovative therapeutics. The company has established a diversified R&D pipeline comprising over 50 drug candidates, with five therapeutic focus areas covering cancer, autoimmune, metabolic, neurological, and infectious diseases. Junshi Biosciences was the first Chinese pharmaceutical company that obtained marketing approval for an anti-PD-1 monoclonal antibody in China. Its first-in-human anti-BTLA monoclonal antibody for the treatment of various cancers was the first in the world to be approved for clinical trials by the FDA and NMPA and has since entered Phase Ib/II trials in both China and the US. Its anti-PCSK9 monoclonal antibody was the first in China to be approved for clinical trials by the NMPA.
In the face of the pandemic, Junshi Biosciences’ response was strong and immediate, joining forces with Chinese and international scientific research institutions and enterprises to develop an arsenal of drug candidates to combat COVID-19, taking the initiative to shoulder the social responsibility of Chinese pharmaceutical companies by prioritizing and accelerating COVID-19 R&D. In 2021, JS016 (etesevimab), China’s first neutralizing fully human monoclonal antibody against SARS-CoV-2 administered with bamlanivimab, was granted Emergency Use Authorizations (EUA) in over 15 countries and regions worldwide. Meanwhile, VV116 (deuremidevir hydrobromide), a novel oral nucleoside analog anti-SARS-CoV-2 drug designed to hinder virus replication, has been approved for marketing in China and Uzbekistan. The JS016 and VV116 programs are a part of the company’s continuous efforts towards innovation for disease control and prevention of the global pandemic.
Junshi Biosciences has about 3,000 employees in the United States (San Francisco and Maryland) and China (Shanghai, Suzhou, Beijing, Guangzhou, etc.). For more information, please visit: http://junshipharma.com.
Junshi Biosciences Contact Information
IR Team:
Junshi Biosciences
Shanghai Junshi Biosciences Co., Ltd. (SHJBF)
https://www.junshipharma.com/en/
Science and Therapeutic Area
R&D Pipeline
https://www.junshipharma.com/en/rd-pipeline/
biotecHOPE™ 2023
BMS-986278
Isaralgagene Civaparvovec
Isaralgagene Civaparvovec
Bristol Myers Squibb’s Investigational LPA1 Antagonist Reduces the Rate of Lung Function Decline in Patients with Idiopathic Pulmonary Fibrosis
05/22/2023CATEGORY:
Phase 2 study shows 26 weeks of treatment with twice-daily 60 mg dose of BMS-986278 resulted in a 62% relative reduction in the rate of decline in percent predicted forced vital capacity (ppFVC) versus placebo
BMS-986278 was well tolerated with rates of adverse events and treatment discontinuation comparable to placebo
Data demonstrate potential of BMS-986278 in pulmonary fibrosis and support progression into Phase 3
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE: BMY) today announced results from a Phase 2 study evaluating BMS-986278, a potential first-in-class, oral, lysophosphatidic acid receptor 1 (LPA1) antagonist, in patients with idiopathic pulmonary fibrosis. The study showed twice-daily administration of 60 mg of BMS-986278 over 26 weeks reduced the rate of decline in percent predicted forced vital capacity (ppFVC) by 62% compared to placebo. Pulmonary fibrosis is a devastating, life-threatening illness, with daily symptoms including coughing, labored breathing and extreme fatigue. These data were presented today at the American Thoracic Society 2023 International Conference held May 19-24, 2023, in Washington, D.C.
“As a treating physician, I am acutely aware of the urgent need for new pulmonary fibrosis treatment options that can improve symptoms, address the underlying cause of disease and are well tolerated by patients,” said Tamera J. Corte, clinical trial investigator and Consultant Respiratory Physician and Director of Interstitial Lung Disease, Department of Respiratory Medicine, Royal Prince Alfred Hospital. “These Phase 2 data for this potential first-in-class oral LPA1 antagonist represent important progress for patients and physicians alike, who are eager for a new standard of care that can mitigate the decline of lung function.”
In this Phase 2 study, patients were randomized (1:1:1) to placebo, 30 mg or 60 mg BMS-986278 twice-daily for 26 weeks. Two-thirds of patients were on background antifibrotic therapy during the trial. Patients who met prespecified blood pressure reduction criteria were to receive a dose reduction to 10 mg of BMS-986278 or matching placebo twice-daily. Dose reductions due to blood pressure criteria were implemented in 5% (placebo), 8% (30 mg) and 6% (60 mg) of patients. The primary endpoint was rate of change in ppFVC from baseline through 26 weeks as assessed based on two prespecified estimands:
- The treatment policy estimand (similar to an Intention-to-Treat [ITT] analysis) included all observed data regardless of dose reduction and provides an estimate of efficacy with dose reduction as part of the treatment regimen.
- The while-on-treatment estimand included all observed data prior to dose reduction and provides an estimate of efficacy without dose reduction as part of the treatment regimen. A similar number of patients received dose reduction across the placebo (n=5), 30 mg (n=7) and 60 mg (n=6) treatment arms.
A prespecified Bayesian analysis was utilized to provide the probability of a positive treatment difference for BMS-986278 compared to placebo.
Treatment with 60 mg of BMS-986278 led to a 62% relative reduction in the rate of change in ppFVC versus placebo in the while-on-treatment analysis (1.8% mean difference in the rate of change in ppFVC versus placebo [95% CI; 0.2, 3.4]), and a 54% reduction versus placebo in the treatment policy analysis (1.4% mean difference in the rate of change in ppFVC versus placebo [95% CI; −0.1, 3.0]). The Bayesian analysis showed a greater than 95% probability that 60 mg of BMS-986278 was superior compared to placebo in reducing the rate of decline in ppFVC over 26 weeks in both the while-on-treatment and treatment policy estimands. The 30 mg dose was not effective compared to placebo.
BMS-986278 was well tolerated in both treatment arms with rates of adverse events, including rates of gastrointestinal side effects, and treatment discontinuation comparable to placebo. In the placebo, 30 mg and 60 mg arms, adverse events (AEs) occurred in 80%, 76% and 74% of patients, respectively, while serious AEs occurred in 17%, 11% and 11% of patients, respectively. The most frequent AEs in the placebo, 30 mg and 60 mg arms included diarrhea (12%, 11%, 11%), cough (5%, 8%, 11%) and orthostatic hypotension (10%, 8%, 5%). Treatment discontinuation rates due to AEs were comparable to placebo, occurring in 10%, 10% and 7% of patients in the placebo, 30 mg and 60 mg arms, respectively.
“The in-house development of BMS-986278 and progress of our pulmonary fibrosis program are a direct result of our industry-leading drug discovery and development capabilities, underscoring our expertise in disease biology and medicinal chemistry,” said Samit Hirawat, MD, chief medical officer, Bristol Myers Squibb. “These Phase 2 data give us the confidence to initiate our global Phase 3 clinical trial program where we will continue exploring BMS-986278 as a potentially new and meaningful therapeutic option for people with pulmonary fibrosis.”
Bristol Myers Squibb would like to thank the patients and investigators who were involved in this study.
About BMS-986278
BMS-986278 is a potential first-in-class, oral, small molecule lysophosphatidic acid receptor 1 (LPA1) antagonist currently being evaluated as a novel antifibrotic treatment for patients with idiopathic pulmonary fibrosis and progressive pulmonary fibrosis. Increased LPA levels and activation of LPA1 have been implicated in the pathogenesis of pulmonary fibrosis. A preclinical in vitro and in vivo study found that antagonizing LPA1 may be beneficial in treating lung injury and fibrosis.
About the BMS-986278 Phase 2 Trial
This Phase 2 trial was a global, randomized study in which patients with idiopathic pulmonary fibrosis received 30 mg or 60 mg of BMS-986278 or matched placebo orally twice-daily. Overall, 278 patients were randomized and 276 received treatment. The study consisted of a 26-week placebo-controlled treatment period, an optional 26-week active treatment extension period and a 4-week post-treatment follow-up period. Patients were permitted to take background antifibrotic treatment. The primary endpoint was rate of change in percent predicted forced vital capacity (ppFVC) from baseline to week 26. ppFVC compares the observed FVC to that which is expected for a healthy person of the same age, gender, race and height. Patients who met prespecified blood pressure reduction criteria were to receive a dose reduction to 10 mg of BMS-986278 or matching placebo twice-daily. A separate cohort of patients with progressive pulmonary fibrosis is ongoing.
More information can be found on www.clinicaltrials.gov (NCT04308681).
About Pulmonary Fibrosis
Pulmonary fibrosis is a chronic, life-threatening interstitial lung disease (ILD) that occurs when lung tissue becomes damaged and scarred, impacting how lungs function. Progressive pulmonary fibrosis is the preferred term to describe patients who have an ILD with a progressive fibrotic phenotype. Idiopathic pulmonary fibrosis is the most common type of progressive fibrosing ILD. As an idiopathic disease, there is no identifiable cause, and as of 2021, more than 700,000 adults are living with IPF globally.
Many people living with PPF and IPF are physically impaired, experience a progressive decline in lung function, have difficulty performing simple daily activities due to breathlessness and require continuous supplemental oxygen to ease the burden of normal breathing.
IPF is a fatal disease with a median survival time of 3-5 years following diagnosis and 5-year survival rate of approximately 45%. Innovation in treatment has been limited with few new therapies approved in nearly 10 years.
Bristol Myers Squibb: Pioneering Paths Forward in Immunology to Transform Patients’ Lives
Bristol Myers Squibb is inspired by a single vision – transforming patients’ lives through science. For people living with immune-mediated diseases, the debilitating reality of enduring chronic symptoms and disease progression can take a toll on their physical, emotional and social well-being, making simple tasks and daily life a challenge. Driven by our deep understanding of the immune system that spans over 20 years of experience, and our passion to help patients, the company continues to pursue pathbreaking science with the goal of delivering meaningful solutions that address unmet needs in rheumatology, gastroenterology, dermatology and pulmonology. We follow the science, aiming to tailor therapies to individual needs, improve outcomes and expand treatment options by working to identify mechanisms with the potential to achieve long-term remission – and perhaps even cures – in the future. By building partnerships with researchers, patients and caregivers to deliver innovative treatments, Bristol Myers Squibb strives to elevate patient care to new standards and deliver what matters most – the promise of living a better life.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
BMY Dividend History
https://www.nasdaq.com/market-activity/stocks/bmy/dividend-history
https://www.bms.com/researchers-and-partners/in-the-pipeline.html
Isaralgagene Civaparvovec
Isaralgagene Civaparvovec
Isaralgagene Civaparvovec
News Release Details
Sangamo Therapeutics Receives U.S. FDA Fast Track Designation for Isaralgagene Civaparvovec for the Treatment of Fabry Disease
May 22, 2023 at 8:05 AM EDT
BRISBANE, Calif.--(BUSINESS WIRE)--May 22, 2023-- Sangamo Therapeutics, Inc. (Nasdaq: SGMO), a genomic medicine company, today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track Designation to isaralgagene civaparvovec, or ST-920, a wholly owned gene therapy product candidate for the treatment of Fabry disease.
Fast Track designation aims to facilitate the development and expedite the review of new therapeutics that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs. Companies granted this designation are given the opportunity for more frequent interactions with the FDA. These clinical programs may also be eligible to apply for Accelerated Approval and Priority Review if relevant criteria are met. The FDA has previously granted ST-920 Orphan Drug Designation.
“We are thrilled with the FDA’s decision to grant Fast Track Designation for ST-920. Fabry is a debilitating disease with life-long impact,” said Nathalie Dubois-Stringfellow, Ph.D, Sangamo’s Senior Vice President, Chief Development Officer. “This decision from the FDA underscores the potential for ST-920 to address a serious unmet need and serve as a meaningful therapeutic option for patients with Fabry disease. We are highly encouraged by this promising development and look forward to our expected meeting with the FDA on Phase 3 trial design in the summer.”
ST-920 is currently being evaluated in the Phase 1/2 STAAR study, with a total of 20 patients dosed to date. In February 2023, Sangamo announced promising results from the STAAR study via an oral presentation at the 19th Annual WORLDSymposium, showing sustained, elevated expression of alpha-galactosidase A (α-Gal A) activity in the 13 dosed patients as of the data cutoff, 78% globotriaosylceramide (Gb3) substrate clearance at 6-months and 77% reduction in urine podocyte loss in one of the first kidney biopsies, and a clinically meaningful and statistically significant increase in mean general health scores, as measured by the SF-36 General Health survey. A copy of the presentation is available in the Presentations section of the Sangamo website. Sangamo is currently preparing for a potential Phase 3 trial and plans to meet with the FDA on the proposed Phase 3 study design in the summer, with a trial start anticipated by the end of 2023, depending on regulatory interactions.
About the STAAR Study
The Phase 1/2 STAAR study is a global open-label, single-dose, dose-ranging, multicenter clinical study designed to evaluate the safety and tolerability of isaralgagene civaparvovec, or ST-920, a gene therapy product candidate in patients with Fabry disease. Isaralgagene civaparvovec requires a one-time infusion without preconditioning. The STAAR study is enrolling patients who are on ERT, are ERT pseudo-naïve (defined as having been off ERT for six or more months), or who are ERT-naïve. The U.S. Food and Drug Administration has granted Orphan Drug and Fast Track designation to isaralgagene civaparvovec, which has also received Orphan Medicinal Product designation from the European Medicines Agency.
About Fabry Disease
Fabry disease is a lysosomal storage disorder caused by mutations in the galactosidase alpha gene (GLA), which leads to deficient alpha-galactosidase A (α-Gal A) enzyme activity, which is necessary for metabolizing globotriaosylceramide (Gb3). The buildup of Gb3 in the cells can cause serious damage to vital organs, including the kidney, heart, nerves, eyes, gut and skin. Symptoms of Fabry disease can include decreased or absent sweat production, heat intolerance, angiokeratoma (skin blemishes), vision problems, kidney disease, heart failure, gastrointestinal disturbance, mood disorders, neuropathic pain and tingling in the extremities.
About Sangamo Therapeutics
Sangamo Therapeutics is a clinical-stage biopharmaceutical company with a robust genomic medicines pipeline. Using ground-breaking science, including our proprietary zinc finger genome engineering technology and manufacturing expertise, Sangamo aims to create new genomic medicines for patients suffering from diseases for which existing treatment options are inadequate or currently don’t exist.
To learn more, visit www.sangamo.com and connect with us on LinkedIn and Twitter.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230522005108/en/
Source: Sangamo Therapeutics, Inc.
Sangamo nabs Fast Track designation for Fabry disease candidate
May 22, 2023 8:22 AM ET
Sangamo Therapeutics, Inc. (SGMO)
By: Jonathan Block, SA News Editor
- The US FDA has granted Fast Track status to Sangamo Therapeutics' (NASDAQ:SGMO) gene therapy isaralgagene civaparvovec for Fabry disease.
- https://seekingalpha.com/news/3973744-sangamo-nabs-fast-track-designation-fabry-disease-candidate
- Sangamo Therapeutics, Inc. (SGMO)
- https://www.sangamo.com/
- https://www.sangamo.com/programs/#pipeline
efanesoctocog alfa
Isaralgagene Civaparvovec
efanesoctocog alfa
EMA validates marketing authorisation application for efanesoctocog alfa for treatment of haemophilia A
19 May, 2023 07:00
Sobi today announced that the European Medicines Agency (EMA) has accepted and validated a marketing authorisation application for efanesoctocog alfa, a new class of high-sustained FVIII developed for the treatment of people with haemophilia A of all age groups. The application is based on data from the pivotal XTEND-1 phase 3 study in adults and adolescents and the XTEND-Kids paediatric study in patients <12 years of age.Efanesoctocog alfa was approved by the US Food and Drug Administration (FDA) as ALTUVIIIO earlier this year.
“Sobi aims to raise the standard of care for rare disease patients around the globe,” said Tony Hoos, MD, PhD, Head of Research & Development and Chief Medical Officer. “Today’s announcement may represent a crucial step towards improving the lives of people with haemophilia A through a potential new treatment option. We look forward to working closely with EMA during their review of our dossier to allow timely access for the haemophilia community in Europe.”
Haemophilia A is a rare, genetic disorder in which the ability of a person's blood to clot is impaired due to a lack of factor VIII. Haemophilia A occurs in about one in 5,000 male births annually, and more rarely in females. People with haemophilia can experience bleeding episodes including life-threatening haemorrhages, acute and chronic pain, irreversible joint damage with disability and negative impacts on quality of life. Despite advancements in treatment made in recent years, a large unmet medical need still exists and requires further improvement in the standard of care.
About XTEND-1
XTEND-1 was an open-label, non-randomized interventional study with two parallel assignment arms. Participants in the prophylaxis arm received a weekly prophylactic dose of efanesoctocog alfa for 52 weeks. Participants in on-demand arm received efanesoctocog alfa on demand for 26 weeks followed by a switch to weekly prophylaxis for another 26 weeks. XTEND-1 evaluated efficacy, safety and pharmacokinetics in 159 previously treated patients ≥12 years of age with severe haemophilia A.
About XTEND-Kids
XTEND-Kids was an open-label, non-randomised interventional, single-arm study. Participants received a weekly prophylactic dose of efanesoctocog alfa for 52 weeks. XTEND-Kids evaluates efficacy, safety, and pharmacokinetics in 74 previously treated patients <12 years of age with severe haemophilia A.
About efanesoctocog alfa
Efanesoctocog alfa [Antihemophilic Factor (Recombinant), Fc-VWF-XTEN Fusion Protein] (formerly BIVV001) is a novel and investigational recombinant factor VIII therapy with the potential to deliver near-normal factor activity levels for a significant parts of the week, improving bleed protection in a once-weekly dose for people with haemophilia A. Efanesoctocog alfa builds on the innovative Fc fusion technology by adding a region of von Willebrand factor and XTEN® polypeptides to extend its time in circulation. It is the only therapy that has been shown to break through the von Willebrand factor ceiling, which imposes a half-life limitation on current factor VIII therapies. It was approved as ALTUVIIIO [Antihemophilic Factor (Recombinant), Fc-VWF-XTEN Fusion Protein-ehtl] by Sanofi in the US in February 2023. It is not approved in any country outside the US.
About the Sanofi and Sobi collaboration
Sobi and Sanofi collaborate on the development and commercialization of Alprolix® and Elocta®/Eloctate®. The companies also collaborate on the development and commercialisation of efanesoctocog alfa or ALTUVIIIO in the US. Sobi has final development and commercialisation rights in the Sobi territory (essentially Europe, North Africa, Russia, and most Middle Eastern markets). Sanofi has final development and commercialisation rights in North America and all other regions in the world excluding the Sobi territory.
Sanofi®
Sanofi are an innovative global healthcare company, driven by one purpose: to chase the miracles of science to improve people's lives. Their team, across some 100 countries, is dedicated to transforming the practice of medicine by working to turn the impossible into the possible. Sanofi provide potentially life-changing treatment options and life-saving vaccine protection to millions of people globally, while putting sustainability and social responsibility at the centre of our ambitions. Sanofi is listed on EURONEXT: SAN and NASDAQ: SNY.
Sobi®
Sobi is a specialised international biopharmaceutical company transforming the lives of people with rare and debilitating diseases. Providing reliable access to innovative medicines in the areas of haematology, immunology and specialty care, Sobi has approximately 1,600 employees across Europe, North America, the Middle East, Asia and Australia. In 2022, revenue amounted to SEK 18.8 billion. Sobi’s share (STO:SOBI) is listed on Nasdaq Stockholm. More about Sobi at sobi.com, LinkedIn and YouTube.
https://www.sobi.com/en/pipeline
Sobi's hemophilia A therapy gets review in EU
May 19, 2023 5:13 AM ET
Sanofi (SNY), BIOVFRHHBY, NVO, BAYRY, BAYZF, NONOF, RHHBF, TAK
By: Ravikash, SA News Editor
The European Medicines Agency (EMA) has accepted and validated Swedish Orphan Biovitrum's (Sobi) (OTCPK:BIOVF) application seeking approval of hemophilia A therapy efanesoctocog alfa.
Sobi and Sanofi (NASDAQ:SNY) have a collaboration for efanesoctocog alfa, which was approved under the name Altuviiio in the U.S. in February for as a once-weekly routine prevention, on-demand treatment and control of bleeding episodes, and perioperative management of bleeding in adults and children with hemophilia A.
Hemophilia A is a genetic bleeding disorder caused by insufficient levels of a blood protein called factor VIII, which helps in clotting of blood.
https://seekingalpha.com/news/3973362-sobis-hemophilia-a-therapy-gets-review-in-eu
https://www.sobi.com/en/pipeline
Repotrectinib
Rucosopasem manganese (GC4711)
efanesoctocog alfa
May 18, 2023
Zai Lab Announces That Repotrectinib Granted Priority Review by China’s NMPA
SHANGHAI, China and CAMBRIDGE, Mass., May 18, 2023 (GLOBE NEWSWIRE) -- Zai Lab Limited (NASDAQ: ZLAB; HKEX: 9688) today announced that the Center for Drug Evaluation (CDE) of China’s National Medical Products Administration (NMPA) has granted priority review to repotrectinib for the treatment of adult patients with locally advanced or metastatic ROS1-positive non-small-cell lung cancer (NSCLC).
“The CDE’s decision to grant priority review to repotrectinib underscores repotrectinib as a potential next-generation best-in-class treatment for ROS1-positive NSCLC in both TKI-naïve and pretreated patients in China,” said Rafael G. Amado, M.D., President, Head of Global Oncology Research and Development at Zai Lab. “We thank the agency for their commitment and continued support to patients in need, and we look forward to our continued partnership with regulatory authorities in China to bring this important medicine to patients in need as soon as possible.”
Priority review was established in China to encourage innovative drug development with significant clinical value and urgent clinical need. It is implemented under the Drug Registration Regulation (Bureau Order 27) and the Working Procedure for Priority Review and Approval of Drug Marketing Authorization (Interim, NMPA 2020 No. 82) effective on July 1, 2020, and July 7, 2020, respectively. According to the regulation and guidance, the regulatory authority will prioritize the evaluation resources for applications under priority review to expedite the review and approval timelines.
About Repotrectinib
Repotrectinib is a next-generation tyrosine kinase inhibitor targeting the ROS1 and NTRK oncogenic drivers of advanced solid tumors, including NSCLC. Patients with tumor harboring ROS1 and NTRK gene fusions treated with approved targeted therapies often develop resistance mutations, limiting binding of these drugs to their target, eventually leading to tumor progression. Repotrectinib is the first next-generation TKI for ROS1-positive metastatic NSCLC, uniquely designed to address key drivers of disease progression. Zai Lab and Turning Point Therapeutics, Inc. (Turning Point Therapeutics, acquired by Bristol Myers Squibb) are studying repotrectinib in TRIDENT-1, a registrational Phase 1/2 study in adults, and CARE, a Phase 1/2 study in pediatric patients. Repotrectinib has shown robust antitumor activity and durable responses among TKI-naïve and pre-treated patients. Zai Lab is enrolling patients in the registrational TRIDENT-1 study in Greater China (Mainland China, Hong Kong, Taiwan, and Macau), while Turning Point Therapeutics is enrolling patients in other regions of the world.
Repotrectinib has been granted three Breakthrough Therapy Designations from the U.S. Food and Drug Administration in: ROS1-positive metastatic NSCLC patients who have not been treated with a ROS1 TKI; ROS1-positive metastatic NSCLC patients who have previously been treated with a ROS1 TKI and who have not received prior platinum-based chemotherapy; and patients with advanced solid tumors that have an NTRK gene fusion who have progressed following treatment with one or two prior TRK TKIs, with or without prior chemotherapy, and have not had satisfactory alternative treatments. Additionally, repotrectinib was previously granted four Fast-Track designations in ROS1-positive advanced NSCLC patients who are ROS1 TKI naïve; ROS1-positive advanced NSCLC patients who have been previously treated with one prior line of platinum-based chemotherapy and one prior ROS1 TKI; ROS1-positive advanced NSCLC patients pretreated with one prior ROS1 TKI without prior platinum-based chemotherapy; and NTRK-positive patients with advanced solid tumors who have progressed following treatment with at least one prior line of chemotherapy and one or two prior TRK TKIs and have not had satisfactory alternative treatments. Repotrectinib was also granted an Orphan Drug designation in 2017.
Repotrectinib has been granted three Breakthrough Therapy Designations from the CDE of China’s NMPA in ROS1-positive metastatic NSCLC patients who have not been treated with a ROS1 TKI; ROS1-positive metastatic NSCLC patients who have previously been treated with a ROS1 TKI and who have not received prior platinum-based chemotherapy; and ROS1-positive metastatic NSCLC patients who have previously been treated with a ROS1 TKI and one prior line of platinum-based chemotherapy.
Zai Lab has an exclusive license agreement with Turning Point Therapeutics to develop and commercialize repotrectinib in Greater China.
About Non-Small Cell Lung Cancer in China
Lung cancer is both the most commonly diagnosed cancer type and the leading cause of cancer death in China. The incidence of lung cancer in China in 2020 was 815,563 cases, with 714,699 deaths.1 NSCLC accounts for approximately 85% of lung cancer, and about 70% of NSCLC is locally advanced or metastatic at initial diagnosis. In China, ROS1 rearrangements occur in 2-3% of patients with advanced NSCLC.
1Globocan 2020.
About Zai Lab
Zai Lab (NASDAQ: ZLAB; HKEX: 9688) is an innovative, research-based, commercial-stage biopharmaceutical company based in China and the United States. We are focused on discovering, developing, and commercializing innovative products that address medical conditions with significant unmet needs in the areas of oncology, autoimmune disorders, infectious diseases, and neuroscience. Our goal is to leverage our competencies and resources to positively impact human health in China and worldwide.
For additional information about Zai Lab, including our products, business activities and partnerships, research, and other events or developments, please visit www.zailaboratory.com or follow us at www.twitter.com/ZaiLab_Global.

Source: Zai Lab Limited
Zai Lab gets priority review for lung cancer dug repotrectinib in China
May 18, 2023 8:50 AM ET
By: Ravikash, SA News Editor
- China's National Medical Products Administration (NMPA) granted priority review to Zai Lab's (NASDAQ:ZLAB) repotrectinib to treat adult patients with locally advanced or metastatic ROS1-positive non-small-cell lung cancer (NSCLC).
- https://seekingalpha.com/news/3972983-zai-lab-gets-priority-review-for-lung-cancer-dug-repotrectinib-in-china
- Zai Lab Limited (ZLAB)BMY
- https://www.zailaboratory.com/
Rucosopasem manganese (GC4711)
Rucosopasem manganese (GC4711)
Rucosopasem manganese (GC4711)
Galera Announces FDA Orphan Drug Designation Granted to Rucosopasem for Pancreatic Cancer
May 18, 2023 at 8:00 AM EDT
Rucosopasem in clinical development to augment the anti-cancer efficacy of stereotactic body radiation therapy
MALVERN, Pa., May 18, 2023 (GLOBE NEWSWIRE) -- Galera Therapeutics, Inc. (Nasdaq: GRTX), a clinical-stage biopharmaceutical company focused on developing and commercializing a pipeline of novel, proprietary therapeutics that have the potential to transform radiotherapy in cancer, today announced that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation to Galera’s second product candidate, rucosopasem manganese (rucosopasem), for the treatment of pancreatic cancer.
Rucosopasem is a next-generation selective dismutase mimetic in clinical development to augment the anti-cancer efficacy of stereotactic body radiation therapy (SBRT) in patients with pancreatic cancer and lung cancer. The Company is currently conducting the GRECO-2 Phase 2b randomized, double-blind, placebo-controlled 220-patient trial of rucosopasem in combination with SBRT in patients with locally advanced pancreatic cancer (LAPC).
“Orphan drug designation for rucosopasem highlights the urgent need for more treatment options to extend survival in patients with pancreatic cancer, which is the fourth leading cause of cancer death in the U.S.,” said Mel Sorensen, M.D., Galera’s President and CEO. “Following our announcement of encouraging survival results from our pilot proof-of-concept trial in patients with LAPC in 2021, we initiated the GRECO-2 trial, which is currently enrolling. We believe rucosopasem has the potential to improve the efficacy of SBRT for pancreatic cancer, and we anticipate topline data from GRECO-2 by the end of next year.”
About Orphan Drug Designation
The U.S. Food and Drug Administration (FDA)’s orphan drug product program is designed to support the development of new drug candidates for the treatment of rare diseases (a condition with a prevalence of less than 200,000 in the U.S.). The FDA has authority to grant orphan drug status to a drug product intended to treat, diagnose or prevent a rare disease or condition. Orphan drug designation provides certain benefits, including market exclusivity upon regulatory approval, exemption of FDA application fees, and tax credits for qualified clinical trials.
About Galera Therapeutics
Galera Therapeutics, Inc. is a clinical-stage biopharmaceutical company focused on developing and commercializing a pipeline of novel, proprietary therapeutic candidates that have the potential to transform radiotherapy in cancer. Galera’s selective dismutase mimetic product candidate avasopasem manganese (avasopasem, or GC4419) is being developed for radiation-induced toxicities. A New Drug Application (NDA) for avasopasem is currently under priority review by the U.S. Food and Drug Administration (FDA) with a Prescription Drug User Fee (PDUFA) date of August 9, 2023 for radiotherapy-induced severe oral mucositis in patients with head and neck cancer undergoing standard-of-care treatment. The Company’s second product candidate, rucosopasem manganese (rucosopasem, or GC4711), is in clinical-stage development to augment the anti-cancer efficacy of stereotactic body radiation therapy in patients with non-small cell lung cancer and locally advanced pancreatic cancer. Rucosopasem was granted Orphan Drug Designation by the U.S. FDA for the treatment of pancreatic cancer. Galera is headquartered in Malvern, PA.
Galera wins FDA’s orphan drug status for pancreatic cancer therapy
May 18, 2023 6:51 AM ET
Galera Therapeutics, Inc. (GRTX)
By: Dulan Lokuwithana, SA News Editor1 Comment
- Galera Therapeutics (NASDAQ:GRTX), a biotech focused on radiotherapy for cancer, added ~4% pre-market Thursday after announcing that the FDA granted Orphan Drug Designation for its pancreatic cancer therapy rucosopasem manganese.
- https://seekingalpha.com/news/3972902-galera-stock-wins-fda-orphan-drug-status-ancer-drug
- Galera Therapeutics, Inc. (GRTX)
- https://www.galeratx.com/
- https://www.galeratx.com/our-pipeline/rucosopasem/
GTX-102
Rucosopasem manganese (GC4711)
Rucosopasem manganese (GC4711)
ULTRAGENYX RECEIVES FDA AGREEMENT TO EXPAND ONGOING GLOBAL PHASE 1/2 TRIAL EVALUATING GTX-102 IN PATIENTS WITH ANGELMAN SYNDROME IN THE U.S.
May 17, 2023
AMENDED U.S. PROTOCOL INCREASES LOADING AND MAINTENANCE DOSES TO SIMILAR RANGE AS EX-U.S. EXPANSION COHORTS
NOVATO, Calif., May 17, 2023 (GLOBE NEWSWIRE) -- Ultragenyx Pharmaceutical Inc. (NASDAQ: RARE) today announced that the U.S. Food and Drug Administration (FDA) has reviewed and agreed to a protocol amendment to the Phase 1/2 study of GTX-102 in pediatric patients with Angelman syndrome that enables the company to harmonize dose ranges in the U.S. with those being used in ex-U.S. cohorts of the study. Outside of the U.S., the Phase 1/2 study has been actively enrolling and dosing patients in the expansion cohorts to verify the GTX-102 dose and treatment regimen that will be used in the Phase 3 program.
“Agreement on the protocol amendment enables comparable dose ranges across all geographies and allows us to move forward rapidly to complete the study. We have begun working urgently to activate multiple study sites in the U.S. and plan to begin enrollment as quickly as possible,” said Scott Stromatt, M.D., SVP and chief medical officer of neurology clinical development at Ultragenyx. “We are eager to expand the study in the U.S. to build on the encouraging data, which demonstrate important clinical activity across multiple functional domains impacted by Angelman syndrome with an acceptable safety profile.”
About the Phase 1/2 study
The Phase 1/2, open-label, dose-escalating study is evaluating the safety and tolerability of GTX-102 in pediatric patients with Angelman syndrome with a genetically confirmed diagnosis of full maternal UBE3A gene deletion. The study is also looking at clinical response as measured by a panel of efficacy assessments for the functional domains impacted in Angelman syndrome. Patients in the earlier dose-escalation cohorts of the study have moved into long-term maintenance dosing, and the study is now enrolling the new expansion cohorts to verify the GTX-102 dose range and treatment regimen that will be used in the Phase 3 program. As of May 4, 2023, 13 patients have had more than 12 months of exposure to GTX-102, with the longest more than 18 months.
The ex-U.S. portion of the study, which includes sites in Europe, Canada and Australia, is currently enrolling patients in expansion cohorts. As additional investigator sites open in the U.S., the study will begin enrolling expansion cohorts using similar dose ranges to the ex-U.S. study. The study will enroll approximately 40 patients across the expansion cohorts. U.S. patients that initiated the study on the 2 mg dose or in the comparator group will begin dosing under the amended protocol.
About Angelman Syndrome
Angelman syndrome is a rare, neurogenetic disorder caused by loss-of-function of the maternally inherited allele of the UBE3A gene. The maternal-specific inheritance pattern of Angelman syndrome is due to genomic imprinting of UBE3A in neurons of the central nervous system (CNS), a naturally occurring phenomenon in which the maternal UBE3A allele is expressed and the paternal UBE3A is not. Silencing of the paternal UBE3A allele is regulated by the UBE3A antisense transcript (UBE3A-AS), the intended target of GTX-102. In almost all cases of Angelman syndrome, the maternal UBE3A allele is either missing or mutated, resulting in limited to no protein expression. This condition is generally not inherited but instead occurs spontaneously. It is estimated to affect 1 in 12,000 to 1 in 20,000 people globally.
Individuals with Angelman syndrome have developmental delay, balance issues, motor impairment, and debilitating seizures. Some individuals with Angelman syndrome are unable to walk and most do not speak. Anxiety and disturbed sleep can be serious challenges in individuals with Angelman syndrome. While individuals with Angelman syndrome have a normal lifespan, they require continuous care and are unable to live independently. Angelman syndrome is not a degenerative disorder, but the loss of the UBE3A protein expression in neurons results in abnormal communications between neurons. Angelman syndrome is often misdiagnosed as autism or cerebral palsy. There are no currently approved therapies for Angelman syndrome; however, several symptoms of this disorder can be reversed in adult animal models of Angelman syndrome suggesting that improvement of symptoms can potentially be achieved at any age.
About GTX-102
GTX-102 is an investigational antisense oligonucleotide delivered via intrathecal administration and designed to target and inhibit expression of UBE3A-AS. Nonclinical studies show that GTX-102 reduces the levels of UBE3A-AS and reactivates expression of the paternal UBE3A allele in neurons of the CNS. Reactivation of paternal UBE3A expression in animal models of Angelman syndrome has been associated with improvements in some of the neurological symptoms associated with the condition. GTX-102 has been granted Orphan Drug Designation, Rare Pediatric Disease Designation, and Fast Track Designation from the FDA.
About Ultragenyx Pharmaceutical Inc.
Ultragenyx is a biopharmaceutical company committed to bringing novel products to patients for the treatment of serious rare and ultrarare genetic diseases. The company has built a diverse portfolio of approved therapies and product candidates aimed at addressing diseases with high unmet medical need and clear biology for treatment, for which there are typically no approved therapies treating the underlying disease.
The company is led by a management team experienced in the development and commercialization of rare disease therapeutics. Ultragenyx’s strategy is predicated upon time- and cost-efficient drug development, with the goal of delivering safe and effective therapies to patients with the utmost urgency.
For more information on Ultragenyx, please visit the company's website at: www.ultragenyx.com.
Ultragenyx gets FDA nod to amend dosing ranges in trial of neuro disorder drug
May 17, 2023 8:46 AM ET
Ultragenyx Pharmaceutical Inc. (RARE)
By: Ravikash, SA News Editor
- Ultragenyx Pharmaceutical (NASDAQ:RARE) said the U.S. Food and Drug Administration (FDA) agreed to a protocol amendment to a phase 1/2 trial of GTX-102 in children with Angelman syndrome.
- The amendment allows the company to harmonize dose ranges in the U.S. with those being used in ex-U.S. groups of the trial.
- https://seekingalpha.com/news/3972532-ultragenyx-gets-fda-nod-to-amend-trial-of-neuro-disorder-drug
- Ultragenyx Pharmaceutical Inc. (RARE)
- https://www.ultragenyx.com/
OCA-Bezafibrate
SRP-9001 Gene Therapy
SRP-9001 Gene Therapy
INTERCEPT PHARMACEUTICALS RECEIVES FDA ORPHAN DRUG DESIGNATION FOR THE FIXED-DOSE COMBINATION OF OCA AND BEZAFIBRATE FOR THE TREATMENT OF PRIMARY BILIARY CHOLANGITIS (PBC)
May 16, 2023 at 5:00 PM EDT
Company on track to complete planned interim analyses from two ongoing Phase 2 studies of the OCA-bezafibrate combination in 2023
Results from planned interim analysis of Phase 2 study evaluating the effects of OCA and bezafibrate on serum biomarkers in PBC to be presented at EASL Congress 2023
MORRISTOWN, N.J., May 16, 2023 (GLOBE NEWSWIRE) -- Intercept Pharmaceuticals, Inc. (Nasdaq: ICPT), a biopharmaceutical company focused on the development and commercialization of novel therapeutics to treat progressive non-viral liver diseases, today announced that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation for the fixed-dose combination of obeticholic acid (OCA) and bezafibrate, a peroxisome proliferator-activated receptor (PPAR) agonist, for the potential treatment of individuals with primary biliary cholangitis (PBC).
“We are pleased that the FDA has granted orphan drug designation for the fixed-dose combination of OCA-bezafibrate, an important component of our long-term strategy and ongoing commitment to people living with PBC,” said M. Michelle Berrey, MD, MPH, President of Research & Development and Chief Medical Officer of Intercept. “This designation represents a milestone in the development of the OCA-bezafibrate fixed-dose combination, which we believe provides the potential to establish best-in-class clinical benefits and further improve the treatment of PBC.”
Intercept has two ongoing Phase 2 studies (747-213 / NCT04594694, 747-214 / NCT05239468) that are designed to explore a range of therapeutic doses for the combination of OCA and bezafibrate. The company expects to complete planned interim analyses from both ongoing Phase 2 studies in 2023, with the first data being presented at the 2023 European Association for the Study of the Liver (EASL) Congress, which will be held from June 21-24, 2023, in Vienna, Austria. The planned interim analyses from these Phase 2 studies, in addition to Phase 1 and preclinical data, will serve as the basis of a potential end-of-phase 2 meeting with the FDA.
FDA's Office of Orphan Drug Products grants orphan status to support the development of medicines for rare disorders that affect fewer than 200,000 people in the U.S. Orphan drug designation provides certain benefits, including market exclusivity upon regulatory approval, exemption of FDA application fees, and tax credits for qualified clinical trials.
About the Investigational OCA-Bezafibrate Fixed-Dose Combination
Intercept is investigating a fixed-dose combination of OCA and bezafibrate for the potential treatment of individuals with PBC. The OCA-bezafibrate combination is investigational; safety and efficacy have not been established. OCA, a farnesoid X receptor (FXR) agonist, is marketed by Intercept as Ocaliva in the United States for the treatment of PBC. Bezafibrate, a pan-peroxisome proliferator-activated receptor (pan-PPAR) agonist, is not approved in the United States for any indication.
FXR and PPAR are distinct pathways that each play a role in PBC. Simultaneously targeting both pathways may offer the greatest potential to impact bile acid synthesis, metabolism, and clearance that underlie cholestatic liver diseases. Published studies establish a clinical proof-of-concept that suggests that the combination of OCA and bezafibrate may provide additive clinical efficacy and tolerability benefits in the treatment of PBC.
About Primary Biliary Cholangitis
Primary biliary cholangitis (PBC) is a rare, progressive, and chronic autoimmune disease that affects the bile ducts in the liver and is most prevalent (approximately 1 in 10,000) in women over the age of 40. PBC causes bile acid to build up in the liver, resulting in inflammation and scarring (fibrosis), which, if left untreated, can lead to cirrhosis, a liver transplant, or death.
About Intercept
Intercept is a biopharmaceutical company focused on the development and commercialization of novel therapeutics to treat progressive non-viral liver diseases, including primary biliary cholangitis (PBC), nonalcoholic steatohepatitis (NASH), and severe alcohol-associated hepatitis (sAH). For more information, please visit www.interceptpharma.com or connect with the Company on Twitter and LinkedIn.
![]()
Source: Intercept Pharmaceuticals, Inc.
Intercept receives Orphan Drug status for rare autoimmune disease candidate
May 16, 2023 5:50 PM ET
Intercept Pharmaceuticals, Inc. (ICPT)
By: Jonathan Block, SA News Editor
- The US FDA granted Orphan Drug designation to Intercept Pharmaceuticals' (NASDAQ:ICPT) combination of obeticholic acid (OCA) and bezafibrate for primary biliary cholangitis (PBC).
- https://seekingalpha.com/news/3972376-intercept-receives-orphan-drug-status-rare-autoimmune-disease-candidate
- Intercept Pharmaceuticals, Inc. (ICPT)
- https://www.interceptpharma.com/
- https://www.interceptpharma.com/our-research/pipeline/
SRP-9001 Gene Therapy
SRP-9001 Gene Therapy
SRP-9001 Gene Therapy
Sarepta Therapeutics Announces Positive Vote from U.S. FDA Advisory Committee Meeting for SRP-9001 Gene Therapy to Treat Duchenne Muscular Dystrophy
05/12/23 7:02 PM EDT
– Advisory committee voted 8-6 in support of accelerated approval of SRP-9001
– Regulatory action date is May 29, 2023
CAMBRIDGE, Mass.--(BUSINESS WIRE)--May 12, 2023-- Sarepta Therapeutics, Inc. (NASDAQ: SRPT), the leader in precision genetic medicine for rare diseases, today announced that the U.S. Food and Drug Administration (FDA) Cellular, Tissue and Gene Therapies Advisory Committee (CTGTAC) voted 8 to 6 in support of accelerated approval of SRP-9001 (delandistrogene moxeparvovec) for the treatment of ambulatory patients with Duchenne muscular dystrophy with a confirmed mutation in the DMD gene.
“Today’s advisory committee outcome is extremely important to the patient community, who are in urgent need of new therapies,” said Doug Ingram, president and chief executive officer, Sarepta. “With the May 29 action date our top priority, we will work collaboratively with the FDA to complete the review of our BLA for SRP 9001. We extend our sincere appreciation to the families, clinicians, FDA presenters and committee members who participated in today’s panel and to all those who provided input and comments both in the written record and in the open public hearing.”
SRP-9001 is intended to treat the underlying cause of Duchenne, which is characterized by mutations in the dystrophin gene that results in the lack of dystrophin protein. In the absence of dystrophin, which is required to strengthen and protect muscles, muscles become weakened and damaged. SRP-9001 is intended to deliver a gene that codes for a shortened, functional form of dystrophin to muscle cells. The committee’s positive vote is based on the evaluation of the totality of evidence including the SRP-9001 product design as well as biological and empirical data. SRP-9001 is supported by non-clinical evidence in addition to efficacy and safety data from studies 101, 102 and 103 as well as an integrated analysis across these three clinical studies comparing functional results to a propensity-score-weighted external control (EC).
The CTGTAC’s vote, while not binding, will be considered by the FDA when making its decision regarding the potential accelerated approval of SRP-9001. The Biologics License Application (BLA) for SRP-9001 is currently under priority review by the FDA with a regulatory action date of May 29, 2023.
About SRP-9001 (delandistrogene moxeparvovec)
SRP-9001 (delandistrogene moxeparvovec) is an investigational gene transfer therapy designed to address the underlying cause of DMD through the targeted production of functional components of dystrophin in muscle tissue. Sarepta is responsible for global development and manufacturing for SRP-9001 and plans to commercialize SRP-9001 in the United States upon receiving FDA approval. In December 2019, Roche partnered with Sarepta to combine Roche’s global reach, commercial presence and regulatory expertise with Sarepta’s gene therapy candidate for Duchenne to accelerate access to SRP-9001 for patients outside the United States.
About Duchenne Muscular Dystrophy
Duchenne muscular dystrophy (DMD) is a rare, fatal neuromuscular genetic disease that occurs in approximately one in every 3,500-5,000 newborn males worldwide. DMD is caused by a change or mutation in the gene that encodes instructions for dystrophin. Symptoms of DMD usually appear in infants and toddlers. Affected children may experience developmental delays such as difficulty in walking, climbing stairs or standing from a sitting position. As the disease progresses, muscle weakness in the lower limbs spreads to the arms and other areas. Most patients require full-time use of a wheelchair in their early teens, and then progressively lose the ability to independently perform activities of daily living such as using the restroom, bathing and feeding. Eventually, increasing difficulty in breathing due to respiratory muscle dysfunction requires ventilation support, and cardiac dysfunction can lead to heart failure. The condition is universally fatal, and patients usually succumb to the disease in their twenties.
About Sarepta Therapeutics
Sarepta is on an urgent mission: engineer precision genetic medicine for rare diseases that devastate lives and cut futures short. We hold leadership positions in Duchenne muscular dystrophy (DMD) and limb-girdle muscular dystrophies (LGMDs), and we currently have more than 40 programs in various stages of development. Our vast pipeline is driven by our multi-platform Precision Genetic Medicine Engine in gene therapy, RNA and gene editing. For more information, please visit www.sarepta.com or follow us on Twitter, LinkedIn, Instagram and Facebook.
Internet Posting of Information
We routinely post information that may be important to investors in the 'For Investors' section of our website at www.sarepta.com. We encourage investors and potential investors to consult our website regularly for important information about us.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230512005452/en/
Source: Sarepta Therapeutics, Inc.
Sarepta muscular dystrophy drug SRP-9001 endorsed by FDA advisors
May 12, 2023 6:31 PM ET
Sarepta Therapeutics, Inc. (SRPT)RHHBY, CTLT
By: Jonathan Block, SA News Editor4 Comments
- A panel of advisors to the US FDA has voted that the benefits of Sarepta Therapeutics' (NASDAQ:SRPT) gene therapy SRP-9001 for Duchenne muscular dystrophy outweigh the risks.
- https://seekingalpha.com/news/3971083-sarepta-muscular-dystrophy-drug-srp-9001-endorsed-fda-advisors
- Sarepta Therapeutics, Inc. (SRPT)
- https://www.sarepta.com/
- https://www.sarepta.com/products-pipeline/pipeline
HyBryte™
SRP-9001 Gene Therapy
HyBryte™
Soligenix Announces Scheduling of Type A Meeting with the U.S. FDA to Review Proposed Study Design for a Second Phase 3 Study Evaluating HyBryte™ in the Treatment of Cutaneous T-Cell Lymphoma
Update on FDA Meeting Outcome Expected Next Month
PRINCETON, N.J., May 11, 2023 /PRNewswire/ -- Soligenix, Inc. (Nasdaq: SNGX) (Soligenix or the Company), a late-stage biopharmaceutical company focused on developing and commercializing products to treat rare diseases where there is an unmet medical need, announced today that the United States (U.S.) Food and Drug Administration (FDA) has granted a Type A meeting to discuss the design of a second, Phase 3 pivotal study evaluating HyBryte™ (hypericin sodium) in the treatment of early stage cutaneous T-cell lymphoma (CTCL), a rare cancer, where it has successfully demonstrated statistically significant results in the first Phase 3 clinical trial. The Type A Meeting is the highest priority classification of meeting the FDA grants companies.
"Responding to FDA feedback, Soligenix has submitted a confirmatory Phase 3 draft study protocol retaining the key aspects of the first Phase 3 trial," stated Christopher J. Schaber, PhD, President and Chief Executive Officer of Soligenix. "We look forward to discussing the protocol in detail with FDA. We intend to provide a further update once we have received the minutes from the meeting or when we have more clarity on next steps, which we anticipate having by or before the end of June."
About HyBryte™
HyBryte™ (research name SGX301) is a novel, first-in-class, photodynamic therapy utilizing safe, visible light for activation. The active ingredient in HyBryte™ is synthetic hypericin, a potent photosensitizer that is topically applied to skin lesions that is taken up by the malignant T-cells, and then activated by visible light approximately 24 hours later. The use of visible light in the red-yellow spectrum has the advantage of penetrating more deeply into the skin (much more so than ultraviolet light) and therefore potentially treating deeper skin disease and thicker plaques and lesions. This treatment approach avoids the risk of secondary malignancies (including melanoma) inherent with the frequently employed DNA-damaging drugs and other phototherapy that are dependent on ultraviolet exposure. Combined with photoactivation, hypericin has demonstrated significant anti-proliferative effects on activated normal human lymphoid cells and inhibited growth of malignant T-cells isolated from CTCL patients. In a published Phase 2 clinical study in CTCL, patients experienced a statistically significant (p=0.04) improvement with topical hypericin treatment whereas the placebo was ineffective. HyBryte™ has received orphan drug and fast track designations from the FDA, as well as orphan designation from the European Medicines Agency (EMA).
The recently published Phase 3 FLASH trial enrolled a total of 169 patients (166 evaluable) with Stage IA, IB or IIA CTCL. The trial consisted of three treatment cycles. Treatments were administered twice weekly for the first 6 weeks and treatment response was determined at the end of the 8th week of each cycle. In the first double-blind treatment cycle, 116 patients received HyBryte™ treatment (0.25% synthetic hypericin) and 50 received placebo treatment of their index lesions. A total of 16% of the patients receiving HyBryte™ achieved at least a 50% reduction in their lesions (graded using a standard measurement of dermatologic lesions, the CAILS score) compared to only 4% of patients in the placebo group at 8 weeks (p=0.04) during the first treatment cycle (primary endpoint). HyBryte™ treatment in the first cycle was safe and well tolerated.
In the second open-label treatment cycle (Cycle 2), all patients received HyBryte™ treatment of their index lesions. Evaluation of 155 patients in this cycle (110 receiving 12 weeks of HyBryte™ treatment and 45 receiving 6 weeks of placebo treatment followed by 6 weeks of HyBryte™ treatment), demonstrated that the response rate among the 12-week treatment group was 40% (p<0.0001 vs the placebo treatment rate in Cycle 1). Comparison of the 12-week and 6-week treatment groups also revealed a statistically significant improvement (p<0.0001) between the two groups, indicating that continued treatment results in better outcomes. HyBryte™ continued to be safe and well tolerated. Additional analyses also indicated that HyBryte™ is equally effective in treating both plaque (response 42%, p<0.0001 relative to placebo treatment in Cycle 1) and patch (response 37%, p=0.0009 relative to placebo treatment in Cycle 1) lesions of CTCL, a particularly relevant finding given the historical difficulty in treating plaque lesions in particular.
The third (optional) treatment cycle (Cycle 3) was focused on safety and all patients could elect to receive HyBryte™ treatment of all their lesions. Of note, 66% of patients elected to continue with this optional compassionate use / safety cycle of the study. Of the subset of patients that received HyBryte™ throughout all 3 cycles of treatment, 49% of them demonstrated a positive treatment response (p<0.0001 vs patients receiving placebo in Cycle 1). Moreover, in a subset of patients evaluated in this cycle, it was demonstrated that HyBryte™ is not systemically available, consistent with the general safety of this topical product observed to date. At the end of Cycle 3, HyBryte™ continued to be well tolerated despite extended and increased use of the product to treat multiple lesions.
Overall safety of HyBryte™ is a critical attribute of this treatment and was monitored throughout the three treatment cycles (Cycles 1, 2 and 3) and the 6-month follow-up period. HyBryte's™ mechanism of action is not associated with DNA damage, making it a safer alternative than currently available therapies, all of which are associated with significant and sometimes fatal, side effects. Predominantly these include the risk of melanoma and other malignancies, as well as the risk of significant skin damage and premature skin aging. Currently available treatments are only approved in the context of previous treatment failure with other modalities and there is no approved front-line therapy available. Within this landscape, treatment of CTCL is strongly motivated by the safety risk of each product. HyBryte™ potentially represents the safest available efficacious treatment for CTCL. With very limited systemic absorption, a compound that is not mutagenic and a light source that is not carcinogenic, there is no evidence to date of any potential safety issues.
The Phase 3 CTCL clinical study was partially funded by the National Cancer Institute via a Phase II SBIR grant (#1R44CA210848-01A1) awarded to Soligenix, Inc. In addition, the FDA awarded an Orphan Products Development grant to support the evaluation of HyBryte™ for expanded treatment in patients with early-stage CTCL, including in the home use setting. The grant, totaling $2.6 million over 4 years, was awarded to a prestigious academic institution that was a leading enroller in the Phase 3 FLASH study.
About Cutaneous T-Cell Lymphoma (CTCL)
CTCL is a class of non-Hodgkin's lymphoma (NHL), a type of cancer of the white blood cells that are an integral part of the immune system. Unlike most NHLs which generally involve B-cell lymphocytes (involved in producing antibodies), CTCL is caused by an expansion of malignant T-cell lymphocytes (involved in cell-mediated immunity) normally programmed to migrate to the skin. These malignant cells migrate to the skin where they form various lesions, typically beginning as patches and may progress to raised plaques and tumors. Mortality is related to the stage of CTCL, with median survival generally ranging from about 12 years in the early stages to only 2.5 years when the disease has advanced. There is currently no cure for CTCL. Typically, CTCL lesions are treated and regress but usually return either in the same part of the body or in new areas.
CTCL constitutes a rare group of NHLs, occurring in about 4% of the approximate 700,000 individuals living with the disease. It is estimated, based upon review of historic published studies and reports and an interpolation of data on the incidence of CTCL that it affects over 25,000 individuals in the U.S., with approximately 3,000 new cases seen annually.
About Soligenix, Inc.
Soligenix is a late-stage biopharmaceutical company focused on developing and commercializing products to treat rare diseases where there is an unmet medical need. Our Specialized BioTherapeutics business segment is developing and moving toward potential commercialization of HyBryte™ (SGX301 or synthetic hypericin) as a novel photodynamic therapy utilizing safe visible light for the treatment of cutaneous T-cell lymphoma (CTCL). With a successful Phase 3 study completed, regulatory approval is being sought and commercialization activities for this product candidate are being advanced initially in the U.S. Development programs in this business segment also include expansion of synthetic hypericin (SGX302) into psoriasis, our first-in-class innate defense regulator (IDR) technology, dusquetide (SGX942) for the treatment of inflammatory diseases, including oral mucositis in head and neck cancer, and proprietary formulations of oral beclomethasone 17,21-dipropionate (BDP) for the prevention/treatment of gastrointestinal (GI) disorders characterized by severe inflammation including pediatric Crohn's disease (SGX203).
Our Public Health Solutions business segment includes active development programs for RiVax®, our ricin toxin vaccine candidate, and SGX943, our therapeutic candidate for antibiotic resistant and emerging infectious disease, and our vaccine programs targeting filoviruses (such as Marburg and Ebola) and CiVax™, our vaccine candidate for the prevention of COVID-19 (caused by SARS-CoV-2). The development of our vaccine programs incorporates the use of our proprietary heat stabilization platform technology, known as ThermoVax®. To date, this business segment has been supported with government grant and contract funding from the National Institute of Allergy and Infectious Diseases (NIAID), the Defense Threat Reduction Agency (DTRA) and the Biomedical Advanced Research and Development Authority (BARDA).
For further information regarding Soligenix, Inc., please visit the Company's website at https://www.soligenix.com and follow us on LinkedIn and Twitter at @Soligenix_Inc.
SOURCE Soligenix, Inc.
Soligenix gets FDA meeting to discuss phase 3 trial design of photodynamic therapy HyBryte
May 11, 2023 9:24 AM ET
By: Ravikash, SA News Editor
- Soligenix (NASDAQ:SNGX) said the U.S. Food and Drug Administration (FDA) has granted a Type A meeting to discuss the design of a second phase 3 trial of photodynamic therapy HyBryte ointment to treat cutaneous T-cell lymphoma (CTCL)
- The company expects update on the meeting outcome in June.
- "Responding to FDA feedback, Soligenix has submitted a confirmatory Phase 3 draft study protocol retaining the key aspects of the first Phase 3 trial," said President and CEO Christopher Schaber.
- https://seekingalpha.com/news/3970041-soligenix-gets-fda-meeting-to-discuss-phase-3-trial-design-of-hybryte
- Soligenix, Inc. (SNGX)
- https://www.soligenix.com/
- https://www.hybryte.com/
Donanemab
Proprietary Pulmonary TRiM™ Platform
HyBryte™
Lilly's Donanemab Significantly Slowed Cognitive and Functional Decline in Phase 3 Study of Early Alzheimer's Disease
May 3, 2023
Nearly half (47%) of the participants on donanemab (compared to 29% on placebo) had no clinical progression at 1 year (defined as no decline in CDR-SB)
Phase 3 trial met primary endpoint and all secondary endpoints measuring cognitive and functional decline
Donanemab treatment slowed clinical decline by 35% compared to placebo, and resulted in 40% less decline on the ability to perform activities of daily living
Over half of all participants completed their course of treatment by 12 months
INDIANAPOLIS, May 3, 2023 /PRNewswire/ -- Eli Lilly and Company (NYSE: LLY) announced today positive results of the TRAILBLAZER-ALZ 2 Phase 3 study showing that donanemab significantly slowed cognitive and functional decline in people with early symptomatic Alzheimer's disease. Donanemab met the primary endpoint of change from baseline until 18 months on the integrated Alzheimer's Disease Rating Scale (iADRS). The primary endpoint of iADRS measures cognition and activities of daily living such as managing finances, driving, engaging in hobbies, and conversing about current events. All secondary endpoints of cognitive and functional decline were also met and showed highly statistically significant clinical benefits with similar magnitude. Based on these results, Lilly will proceed with global regulatory submissions as quickly as possible and anticipates making a submission to the U.S. Food and Drug Administration (FDA) yet this quarter. Lilly will work with the FDA and other global regulators to achieve the fastest path to traditional approvals.
TRAILBLAZER-ALZ 2, a randomized, double-blind, placebo-controlled study, evaluated the safety and efficacy of donanemab, an investigational amyloid plaque targeting therapy. The study enrolled people with early symptomatic Alzheimer's disease (AD), which includes mild cognitive impairment (MCI) and the mild dementia stage of disease, with the confirmed presence of AD neuropathology, and participants completed their course of treatment with donanemab once they reached a prespecified level of amyloid plaque clearance.
Participants in TRAILBLAZER-ALZ 2 were stratified by their level of the brain protein tau, a predictive biomarker for Alzheimer's disease progression. The primary analysis population (n=1182) for which the study was powered was comprised of people with an intermediate level of tau and clinical symptoms of Alzheimer's disease. In this population, the primary endpoint (iADRS) showed 35% slowing of decline (p<0.0001), and an important key secondary endpoint (Clinical Dementia Rating-Sum of Boxes, or CDR-SB) showed 36% slowing of decline (p<0.0001) over 18 months. Additional prespecified secondary analyses showed:
- 47% of participants on donanemab showed no decline on CDR-SB, a key measure of disease severity at 1 year (compared to 29% of participants on placebo, p<0.001).
- 52% of participants completed their course of treatment by 1 year and 72% completed by 18 months as a result of achieving plaque clearance.
- Participants on donanemab had 40% less decline in ability to perform activities of daily living at 18 months [as measured by Alzheimer's Disease Cooperative Study – instrumental Activities of Daily Living Inventory (ADCS-iADL), p<0.0001].
- Participants on donanemab experienced a 39% lower risk of progressing to the next stage of disease compared to placebo (CDR-Global Score, HR=0.61; p<0.001).
"Over the last 20 years, Lilly scientists have blazed new trails in the fight against Alzheimer's disease by elucidating basic mechanisms of AD pathology and discovering imaging and blood biomarker tools to track the pathology," said Daniel Skovronsky, M.D., Ph.D., Lilly's chief scientific and medical officer, and president of Lilly Research Laboratories. "We are extremely pleased that donanemab yielded positive clinical results with compelling statistical significance for people with Alzheimer's disease in this trial. This is the first Phase 3 trial of any investigational medicine for Alzheimer's disease to deliver 35% slowing of clinical and functional decline."
The study also enrolled a smaller number of people with high levels of tau at baseline (n=552), representing a later stage of disease progression. Because these participants were predicted to progress more quickly and be less responsive to therapy, the target population for the study was the intermediate tau population. The high tau participants were combined with the intermediate tau population in an additional primary analysis of all participants enrolled (n=1736). In this combined population, donanemab also demonstrated meaningful positive results across all clinical endpoints (p<0.001), with CDR-SB and iADRS showing 29% and 22% slowing of decline, respectively.
The incidence of amyloid-related imaging abnormalities (ARIA) was consistent with the TRAILBLAZER-ALZ Phase 2 study. ARIA is observed with the amyloid plaque clearing antibody class of therapies and is most commonly observed as temporary swelling in an area or areas of the brain (ARIA-E) or as microhemorrhages or superficial siderosis (ARIA-H), in either case detected by MRI. In the overall donanemab treatment group, ARIA-E occurred in 24.0% of treated participants, with 6.1% experiencing symptomatic ARIA-E. ARIA-H occurred in 31.4% in the donanemab group and 13.6% in the placebo group. The majority of ARIA cases were mild to moderate and resolved or stabilized with appropriate management. ARIA is usually asymptomatic, although serious and life-threatening events can occur. In this study, the incidence of serious ARIA was 1.6%, including two participants whose death was attributed to ARIA and a third participant who died after an incident of serious ARIA. Infusion-related reactions occurred in 8.7% of participants with most cases mild to moderate in severity.
"We are encouraged by the potential clinical benefits that donanemab may provide, although like many effective treatments for debilitating and fatal diseases, there are associated risks that may be serious and life-threatening," said Mark Mintun, M.D., group vice president Neuroscience Research & Development at Lilly, and president of Avid Radiopharmaceuticals. "We note that these results suggest that people in the early pathological stage of disease could be the most responsive to therapeutics targeting amyloid. We thank the participants in the clinical trial and their loved ones for their time and commitment to finding solutions for this disease."
In addition to slowing cognitive and functional decline in TRAILBLAZER-ALZ 2, donanemab produced significant reductions in brain amyloid plaque levels as early as 6 months after initiating treatment, as observed using amyloid positron emission tomography (PET) brain scan, with many patients reaching amyloid levels considered negative for pathology1 (34% of participants in the intermediate tau population achieved amyloid clearance at 6 months and 71% achieved clearance at 12 months).
"Amyloid plaque is a defining pathophysiological feature of Alzheimer's disease," said Dr. Eric Reiman, CEO of Banner Research, one of the research sites for the TRAILBLAZER-ALZ 2 trial. "This study's topline results provide compelling support for the relationship between amyloid plaque removal and a clinical benefit in people with this disease."
"These Phase 3 data confirm the benefit observed in our TRAILBLAZER-ALZ study and show that donanemab, if approved, may represent a significant step forward for people with early symptomatic Alzheimer's disease, and allow them to continue to participate in activities that are meaningful to them," said Anne White, executive vice president of Eli Lilly and Company and president of Lilly Neuroscience. "We believe our data meets the 'high level of evidence' the Centers for Medicare & Medicaid Services (CMS) has described as the trigger for reconsideration of its National Coverage Determination. People with early Alzheimer's disease need and deserve full coverage and access for approved therapies."
Topline study results:
In the intermediate tau population, the baseline characteristics were similar to other contemporary early symptomatic AD studies (e.g., MMSE score was 22.9). Accordingly, the placebo arm progressed as expected (decline on iADRS and CDR-SB of 9.3 and 1.9 points respectively over 18 months). Prespecified analyses used standard statistical methods including the mixed model for repeated measures (MMRM) and natural cubic spline (NCS) analyses, with similar results across both methods. The following efficacy measures were obtained at 18 months comparing decline in donanemab to placebo treated participants:
About TRAILBLAZER-ALZ 2 Study and the TRAILBLAZER-ALZ program
TRAILBLAZER-ALZ 2 (NCT04437511) is a Phase 3, double-blind, placebo-controlled study to evaluate the safety and efficacy of donanemab in participants ages 60-85 years with early symptomatic Alzheimer's disease (MCI or mild dementia due to Alzheimer's disease) with the presence of confirmed Alzheimer's disease neuropathology. The trial enrolled 1736 participants selected based on cognitive assessments in conjunction with amyloid plaque imaging and tau staging by PET imaging.
Lilly previously announced and published in the New England Journal of Medicine (NEJM) results from the Phase 2 TRAILBLAZER-ALZ study in 2021. In addition, Lilly shared data from TRAILBLAZER-ALZ 4, the first active comparator study in early symptomatic Alzheimer's disease, at the 15th Clinical Trials on Alzheimer's Disease (CTAD) conference in 2022.
Lilly continues to study donanemab in multiple clinical trials, including TRAILBLAZER-ALZ 3, which is focused on preventing symptomatic Alzheimer's disease in participants with preclinical AD; TRAILBLAZER-ALZ 5, a registration trial for early symptomatic Alzheimer's disease currently enrolling in China; and TRAILBLAZER-ALZ 6, which is focused on expanding our understanding of ARIA through novel MRI sequences, blood-based biomarkers and different dosing regimens of donanemab.
About Lilly
Lilly unites caring with discovery to create medicines that make life better for people around the world. We've been pioneering life-changing discoveries for nearly 150 years, and today our medicines help more than 51 million people across the globe. Harnessing the power of biotechnology, chemistry and genetic medicine, our scientists are urgently advancing new discoveries to solve some of the world's most significant health challenges, redefining diabetes care, treating obesity and curtailing its most devastating long-term effects, advancing the fight against Alzheimer's disease, providing solutions to some of the most debilitating immune system disorders, and transforming the most difficult-to-treat cancers into manageable diseases. With each step toward a healthier world, we're motivated by one thing: making life better for millions more people. That includes delivering innovative clinical trials that reflect the diversity of our world and working to ensure our medicines are accessible and affordable. To learn more, visit Lilly.com and Lilly.com/newsroom or follow us on Facebook, Instagram, Twitter and LinkedIn. P-LLY
© Lilly USA, LLC 2023. ALL RIGHTS RESERVED.

View original content to download multimedia:https://www.prnewswire.com/news-releases/lillys-donanemab-significantly-slowed-cognitive-and-functional-decline-in-phase-3-study-of-early-alzheimers-disease-301814001.html
SOURCE Eli Lilly and Company
QALSODY™ (tofersen)
Proprietary Pulmonary TRiM™ Platform
Proprietary Pulmonary TRiM™ Platform
FDA Grants Accelerated Approval for QALSODY™ (tofersen) for SOD1-ALS, a Major Scientific Advancement as the First Treatment to Target a Genetic Cause of ALS
APRIL 25, 2023 • NEWS RELEASE
- FDA granted accelerated approval of QALSODY based on a reduction of neurofilament, a marker of neurodegeneration1
- Superoxide dismutase 1 (SOD1)-amyotrophic lateral sclerosis (ALS) is a devastating, uniformly fatal,2 and ultra-rare genetic form of ALS3-4 with approximately 330 people in the U.S. living with the disease5
CAMBRIDGE, Mass., April 25, 2023 (GLOBE NEWSWIRE) -- Biogen Inc. (Nasdaq: BIIB) announced today that the U.S. Food and Drug Administration (FDA) has approved QALSODY™ (tofersen) 100 mg/15mL injection for the treatment of amyotrophic lateral sclerosis (ALS) in adults who have a mutation in the superoxide dismutase 1 (SOD1) gene. This indication is approved under accelerated approval based on reduction in plasma neurofilament light chain (NfL) observed in patients treated with QALSODY. Continued approval for this indication may be contingent upon verification of clinical benefit in confirmatory trial(s).1 The ongoing Phase 3 ATLAS study of tofersen in people with presymptomatic SOD1-ALS will serve as the confirmatory trial.1
Neurofilaments are proteins that are released from neurons when they are damaged, making them a marker of neurodegeneration.6
“For more than a decade, Biogen has been steadfast in our commitment to pursuing treatments for ALS, and I want to thank the scientists as well as the entire ALS community who have all worked tirelessly to bring this first-of-its-kind treatment to people with SOD1-ALS,” said Christopher A. Viehbacher, President and Chief Executive Officer of Biogen. “Today also marks a pivotal moment in ALS research as we gained, for the first time, consensus that neurofilament can be used as a surrogate marker reasonably likely to predict clinical benefit in SOD1-ALS. We believe this important scientific advancement will further accelerate innovative drug development for ALS.”
QALSODY is the first approved treatment to target a genetic cause of ALS.1 Biogen collaborated with Ionis Pharmaceuticals on the early development of tofersen.
Warnings and precautions associated with QALSODY were serious neurologic events, including myelitis and/or radiculitis; papilledema and elevated intracranial pressure; and aseptic meningitis. If symptoms consistent with myelitis, radiculitis papilledema, elevated intracranial, or aseptic meningitis develop, diagnostic workup and treatment should be initiated according to the standard of care. Management may require interruption or discontinuation of QALSODY. The most common adverse reactions that occurred in ≥10% of QALSODY treated participants and more than the placebo arm were pain, fatigue, arthralgia, cerebrospinal (CSF) white blood cell increased, and myalgia.1
“Since SOD1 mutations were first identified as a cause of ALS 30 years ago, the familial ALS community has been searching for genetically targeted treatments. QALSODY offers families who have lost generation after generation in the prime of their life to this devastating disease a therapy targeting the underlying cause of SOD1-ALS. Today marks an important moment in ALS research as QALSODY is the first ALS treatment approved based on a biomarker,” said Jean Swidler, chair of Genetic ALS & FTD: End the Legacy. “We are excited to see what future therapies are developed now that it is understood that lowering levels of neurofilament provides important evidence that a treatment is affecting the neurodegenerative process.”
The efficacy of QALSODY was assessed in a 28-week randomized, double-blind, placebo-controlled clinical study in patients 23 to 78 years of age with weakness attributable to ALS and a SOD1 mutation confirmed by a central laboratory. One hundred eight (108) patients were randomized 2:1 to receive treatment with either QALSODY 100 mg (n=72) or placebo (n=36) for 24 weeks (3 loading doses followed by 5 maintenance doses). Concomitant riluzole and/or edaravone use was permitted for patients and at baseline 62% of patients were taking riluzone, and 8% of patients were taking edaravone.1
Over 28 weeks in VALOR, participants in the primary analysis population (n=60) treated with QALSODY experienced less decline from baseline as measured by the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R) compared to placebo, though the results were not statistically significant (QALSODY-placebo adjusted mean difference [95% CI]: 1.2 [-3.2, 5.5]). In the overall intent-to-treat population (n=108), QALSODY-treated participants experienced a 55% reduction in plasma NfL compared to a 12% increase in placebo-treated participants (difference in geometric mean ratios for QALSODY to placebo: 60%; nominal p<0.0001). Additionally, levels of CSF SOD1 protein, an indirect measure of target engagement, were reduced by 35% in the QALSODY-treated group compared to 2% in the corresponding placebo group (difference in geometric mean ratios for QALSODY to placebo: 34%; nominal p<0.0001).1
At an interim analysis at 52 weeks of participants who had completed VALOR and enrolled in an open-label extension (OLE) study, reductions in NfL were seen in participants previously receiving placebo and who initiated QALSODY in the OLE, similar to the reductions seen in participants treated with QALSODY in VALOR. Earlier initiation of QALSODY compared to placebo/delayed-start of QALSODY was associated with trends for reduction in decline on measures of clinical function (ALSFRS-R), respiratory strength (slow vital capacity percent-predicted), and muscle strength (hand-held dynamometry megascore), though they were not statistically significant. QALSODY was also associated with a non-statistically significant trend towards reduction of the risk of death or permanent ventilation. These exploratory analyses should be interpreted with caution given the limitations of data collected outside of controlled study, which may be subject to confounding.1
The approval of QALSODY was supported by 12-month integrated results from VALOR and its OLE comparing earlier initiation of tofersen (at the start of VALOR) to delayed initiation of tofersen (six months later, in the OLE), that were published in The New England Journal of Medicine.7
“I have observed the positive impact QALSODY has on slowing the progression of ALS in people with SOD1 mutations,” said Timothy M. Miller, MD, PhD, principal investigator of the QALSODY clinical trials and co-director of the ALS Center at Washington University School of Medicine in St. Louis. “The FDA’s approval of QALSODY gives me hope that people living with this rare form of ALS could experience a reduction in decline in strength, clinical function, and respiratory function.”
QALSODY will be made available for shipment in the U.S. to healthcare providers in approximately one week. Biogen anticipates there may be variation in time to treatment as institutions and treatment centers learn about QALSODY.
What is QALSODY?
QALSODYTM (tofersen) is a prescription medicine used to treat amyotrophic lateral sclerosis (ALS) in adults who have a mutation in the superoxide dismutase 1 (SOD1) gene. This indication is approved under accelerated approval based on reduction in plasma neurofilament light chain (NfL) observed in patients treated with QALSODY. Continued approval for this indication may be contingent upon verification of clinical benefit in confirmatory trial(s).
Please see full Prescribing Information.
For more details on QALSODY, visit www.QALSODY.com.
About QALSODY™ (tofersen)
QALSODY is an antisense oligonucleotide (ASO) designed to bind to SOD1 mRNA to reduce SOD1 protein production. QALSODY is indicated for the treatment of ALS in adults who have a mutation in the SOD1 gene in the U.S. This indication is approved under accelerated approval based on reduction in plasma NfL observed in patients treated with QALSODY. Continued approval for this indication may be contingent upon verification of clinical benefit in confirmatory trial(s). QALSODY is administered intrathecally as three loading doses administered at 14-day intervals followed by maintenance doses administered once every 28 days thereafter.1 In people with SOD1-ALS, mutations in their SOD1 gene cause their bodies to create a toxic misfolded form of SOD1 protein. This toxic protein causes motor neurons to degenerate, resulting in progressive muscle weakness, loss of function, and eventually, death.8
Biogen licensed tofersen from Ionis Pharmaceuticals, Inc. under a collaborative development and license agreement. Tofersen was discovered by Ionis.
In addition to the ongoing OLE of VALOR, QALSODY is being studied in the Phase 3, randomized, placebo-controlled ATLAS study to evaluate whether QALSODY can delay clinical onset when initiated in presymptomatic individuals with a SOD1 genetic mutation and biomarker evidence of disease activity (elevated plasma NfL). The primary efficacy endpoint is the proportion of participants with emergence of clinically manifest ALS. ATLAS is currently more than 50 percent enrolled with clinical trial sites in 14 countries worldwide with an estimated primary completion date in 2026. More details about ATLAS (NCT04856982) can be found at clinicaltrials.gov.
Financial Assistance Programs and Access to QALSODY
Biogen provides comprehensive support services which includes insurance couseling and financial assistance for eligible individuals. Support Coordinators are available to help with understanding insurance coverage, navigating the access landscape, and exploring financial assistance options including the QALSODY (tofersen) Copay Program, which may lower the out-of-pocket costs for eligible commercially insured patients to as low as $0. They can be reached at 1-877-725-7639 between the hours of 8:30 AM – 8:00 PM ET, Monday to Friday.
ALS Identified™ Program
Up to 15 percent of people living with ALS are thought to have a genetic form of the disease, whether or not they have a known family history. As genetic testing is not broadly available, Biogen sponsors a genetic testing program, ALS Identified™, for people living with ALS and their families in the U.S.
Sponsored by Biogen and offered through Invitae, the ALS Identified™ program facilitates access to genetic counseling and testing for all individuals 18 years or older within the U.S. and Puerto Rico with a clinical diagnosis of ALS, or a family history of ALS at no charge. More information about ALS Identified is available at insideALS.com, a website designed in collaboration with outside medical experts and the ALS community that offers continuous updates on the emerging science that provides insights and information to the ALS community. Interested people with ALS should talk to their doctor about genetic testing options and can learn more at insideALS.com.
About Amyotrophic Lateral Sclerosis and SOD1-ALS
Amyotrophic lateral sclerosis (ALS) is a rare, progressive and fatal neurodegenerative disease that results in the loss of motor neurons in the brain and the spinal cord that are responsible for controlling voluntary muscle movement. People with ALS experience muscle weakness and atrophy, causing them to lose independence as they steadily lose the ability to move, speak, eat, and eventually breathe. Average life expectancy for people with ALS is three to five years from time of symptom onset.2
Multiple genes have been implicated in ALS. Genetic testing helps determine if a person’s ALS is associated with a genetic mutation, even in individuals without a known family history of the disease. SOD1-ALS is diagnosed in approximately 2 percent of all ALS cases, with about 330 people in the United States living with the disease.5 More than 15 percent of people with ALS are thought to have a genetic form of the disease;8 however, they may not have a known family history of the disease.5
Biogen’s Continuous Commitment to ALS
For over a decade, Biogen has been committed to advancing ALS research to provide a deeper understanding of all forms of the disease. The company has continued to invest in and pioneer research despite making the difficult decision to discontinue a late-stage ALS asset in 2013. Biogen has applied important learnings to its portfolio of assets for genetic and other forms of ALS, with the goal of increasing the probability of bringing a potential therapy to patients in need. These applied learnings include evaluating genetically validated targets in defined patient populations, pursuing the most appropriate modality for each target and employing sensitive clinical endpoints. In addition to QALSODY, the company has a pipeline of investigational drugs being evaluated in ALS, including BIIB105.
About Biogen
Founded in 1978, Biogen is a leading global biotechnology company that has pioneered multiple breakthrough innovations including a broad portfolio of medicines to treat multiple sclerosis, the first approved treatment for spinal muscular atrophy, and two co-developed treatments to address a defining pathology of Alzheimer’s disease. Biogen is advancing a pipeline of potential novel therapies across neurology, neuropsychiatry, specialized immunology and rare diseases and remains acutely focused on its purpose of serving humanity through science while advancing a healthier, more sustainable and equitable world.
Biogen, Ionis win FDA nod for ALS therapy Qalsody
Apr. 25, 2023 3:11 PM ET
By: Dulan Lokuwithana, SA News Editor2 Comments
Update 03:11 PM EST: Adds comments from Biogen (NASDAQ:BIIB)
The FDA announced Tuesday the approval of Qalsody (tofersen) developed by Biogen (BIIB) and Ionis Pharmaceuticals (NASDAQ:IONS) for certain patients with neurodegenerative disease amyotrophic lateral sclerosis (ALS).
Specifically, the FDA has cleared Qalsody for ALS linked to a mutation in the superoxide dismutase 1 (SOD1) gene, which accounts for about 2% of ALS cases.
https://seekingalpha.com/news/3959949-biogen-stock-ionis-stock-win-fda-nod-als-therapy-qalsody
Proprietary Pulmonary TRiM™ Platform
Proprietary Pulmonary TRiM™ Platform
Proprietary Pulmonary TRiM™ Platform
Arrowhead Pharmaceuticals’ Proprietary Pulmonary TRiM™ Platform Achieves High Levels of Target Gene Knockdown and Long Duration of Effect
Apr 25, 2023 at 7:30 AM EDT
- Interim Results from Ongoing ARO-RAGE Phase 1/2 Study Demonstrate up to 90% Serum sRAGE Reduction with Mean Maximum Reduction of 80% after Two Doses
- Further Data to be Presented at Upcoming R&D Day
PASADENA, Calif.--(BUSINESS WIRE)--Apr. 25, 2023-- Arrowhead Pharmaceuticals Inc. (NASDAQ: ARWR) today announced interim results from an ongoing Phase 1/2 clinical study of ARO-RAGE, the company’s investigational RNA interference (RNAi) therapeutic designed to reduce production of the receptor for advanced glycation end products (RAGE) as a potential treatment for inflammatory pulmonary diseases, such as asthma. These data represent the first clinical demonstration of the potential utility of Arrowhead’s proprietary Targeted RNAi Molecule (TRiMTM) platform optimized for delivery to the lungs.
Matthias Salathe, M.D., Professor, Pulmonary, Critical Care and Sleep Medicine, and Vice Chancellor for Research at the University of Kansas Medical Center, said: “These interim ARO-RAGE Phase 1/2 data are highly encouraging. Unmet need continues to exist for many patients with severe asthma who suffer from persistent symptoms and exacerbations, despite current therapies. Reducing expression of the RAGE protein in pulmonary epithelial cells to the degree that ARO-RAGE has demonstrated to date in this study has the potential to treat patients with asthma and other inflammatory lung diseases in a fundamentally new way. RAGE represents a promising target for intervention as its activation has been implicated as a proximal regulator of the inflammatory cascade in the asthmatic airway, and thus RAGE silencing may result in potent anti-inflammatory effects. I look forward to the availability of additional results from this important trial.”
Interim results from ARO-RAGE administration in Part 1 of the ongoing Phase 1/2 study in normal healthy volunteers include:
- Reductions in soluble RAGE (sRAGE) as measured in serum after two doses on Day 1 and Day 29
- Mean maximum reduction at 92 mg dose was 80% with a maximum reduction of 90%
- Mean maximum reductions at 10 to 44 mg dose levels showed a dose response ranging from 31% to 59%
- Duration of pharmacologic effect persisted for at least 6 weeks after the second administration of the 92 mg dose with further follow up ongoing
- Interim results for this cohort are only available through Day 71
- Reductions in sRAGE as measured in bronchoalveolar lavage fluid (BALF) at Day 31 after a single dose
- Mean reduction at 92 mg dose was 75% with a maximum reduction of 92%
- Mean reductions at 10 to 44 mg doses ranged from 44% to 52%
- Reductions in serum sRAGE were also observed after a single dose
- Mean maximum reduction at 92 mg dose was 56% with a maximum reduction of 68%
- Mean maximum reductions at 10 to 44 mg dose levels showed a dose response and ranged from 23% to 53%
- The pooled placebo groups experienced a mean sRAGE increase of 8% in BALF and a mean decrease of 1% in serum
- Safety and tolerability
- Overall, no patterns of adverse changes in any clinical safety parameters
- No reported serious or severe adverse events
- No dropouts related to drug or related to adverse events
- These results include 4 of 5 escalating dose levels. Data are not yet available for single or multiple dose cohorts at 184 mg, the highest dose being tested
Christopher Anzalone, Ph.D., President and CEO at Arrowhead, said: “We think these interim data with ARO-RAGE represent clinical validation of Arrowhead’s inhaled pulmonary TRiMTM platform and, specifically, of ARO-RAGE as a potential new therapy to treat patients with inflammatory lung diseases. The high level of target gene knockdown, the long duration of effect, and the promising safety and tolerability results are all very encouraging signs for our growing pipeline of RNAi therapeutic candidates that leverage this same platform. We look forward to providing additional data at our upcoming R&D Day on June 1, 2023, and at future medical meetings.”
About the Phase 1/2 Study
ARORAGE-1001 (NCT05276570) is a Phase 1/2a, randomized, double-blinded, placebo-controlled study in normal healthy volunteers (NHV), Part 1, and patients with mild-to-moderate asthma, Part 2. The single ascending dose portion of the study includes 5 sequentially enrolled NHV cohorts with escalating single-dose levels. The multiple ascending dose portion of the study includes 5 NHV cohorts and 3 asthma patient cohorts. The objectives of the study include the assessment of safety and tolerability, pharmacokinetics, and pharmacodynamics of ARO-RAGE in NHVs and patients with asthma.
About RAGE
RAGE is implicated in the pathogenesis of numerous inflammatory diseases, including asthma. Reduction of RAGE expression via RNAi is designed to reduce the amount of RAGE protein expressed on pulmonary epithelial cells. Reduced RAGE expression in the pulmonary epithelium may result in reduction of RAGE-dependent inflammatory pathways, leading to decreased exacerbation frequency and improved airflow in patients with asthma
About Arrowhead Pharmaceuticals
Arrowhead Pharmaceuticals develops medicines that treat intractable diseases by silencing the genes that cause them. Using a broad portfolio of RNA chemistries and efficient modes of delivery, Arrowhead therapies trigger the RNA interference mechanism to induce rapid, deep, and durable knockdown of target genes. RNA interference, or RNAi, is a mechanism present in living cells that inhibits the expression of a specific gene, thereby affecting the production of a specific protein. Arrowhead’s RNAi-based therapeutics leverage this natural pathway of gene silencing.
For more information, please visit www.arrowheadpharma.com, or follow us on Twitter @ArrowheadPharma. To be added to the Company's email list and receive news directly, please visit http://ir.arrowheadpharma.com/email-alerts.
Source: Arrowhead Pharmaceuticals, Inc.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230425005446/en/
Arrowhead rises 17% after early data for asthma candidate
Apr. 25, 2023 11:04 AM ET
Arrowhead Pharmaceuticals, Inc. (ARWR)
By: Dulan Lokuwithana, SA News Editor
- Arrowhead Pharmaceuticals (NASDAQ:ARWR) added ~17% in the morning hours Tuesday after the clinical-stage biotech posted interim data from a Phase 1/2 trial for its investigational RNA interference (RNAi) therapeutic ARO-RAGE targeted at patients with asthma.
- https://seekingalpha.com/news/3959783-arrowhead-stock-rises-early-data-asthma-candidate
- Arrowhead Pharmaceuticals, Inc. (ARWR)
- https://arrowheadpharma.com/
biotecHOPE™ 2023
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen halted ATTRv-PN disease progression and improved neuropathy impairment and quality of life in Phase 3 study through 66 weeks
April 24, 2023 at 7:00 AM EDT
- NEURO-TTRansform study met all co-primary and secondary endpoints
- Positive results to be presented today at AAN 2023 demonstrate eplontersen efficacy, safety and administration profile may provide an important new treatment option in this fatal disease with significant unmet need
- Ionis to host webcast on Tuesday, April 25 at 1 p.m. ET
CARLSBAD, Calif., April 24, 2023 /PRNewswire/ -- Ionis Pharmaceuticals, Inc. (Nasdaq: IONS) today announced that the Phase 3 NEURO-TTRansform study for AstraZeneca and Ionis' eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN) met all co-primary endpoints and secondary endpoints at 66 weeks versus an external placebo group. The positive results are being presented today in an Emerging Science Session at the American Academy of Neurology (AAN) 2023 Annual Meeting in Boston. ATTRv-PN is a debilitating disease driven by the progressive accumulation of TTR amyloid deposits, which causes progressive nerve damage and leads to organ failure and eventually death.
At 66 weeks, patients treated with eplontersen demonstrated consistent and sustained benefit on the three co-primary endpoints measuring serum transthyretin (TTR) concentration, neuropathy impairment and quality of life:
- Eplontersen achieved a least squares (LS) mean reduction of 82% in serum TTR concentration from baseline, compared to an 11% reduction from baseline in the external placebo group (p<0.0001).
- Eplontersen halted disease progression as measured by modified Neuropathy Impairment Score +7 (mNIS+7), resulting in a 0.28 point LS mean increase compared to a 25.06 point increase for the external placebo group from baseline (24.8 point LS mean improvement; p<0.0001).
- Overall, 47% of treated patients showed improvements in neuropathy at 66 weeks compared to baseline versus 17% in the external placebo group. Among study completers, 53% of treated patients showed improvements in neuropathy at 66 weeks compared to baseline versus 19% in the external placebo group.
- Eplontersen improved quality of life demonstrating a 5.5 point LS mean decrease (improvement) on the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy (Norfolk QoL-DN), compared to a 14.2 point increase (worsening) in the external placebo group (19.7 point LS mean improvement; p<0.0001).
- Overall, 58% of treated patients showed improvements in QoL at 66 weeks compared to baseline versus 20% in the external placebo group. Among study completers, 65% of treated patients showed improvements in QoL at 66 weeks compared to baseline versus 23% in the external placebo group.
- Eplontersen demonstrated statistically significant benefits on both mNIS+7 and Norfolk QoL-DN at 35 weeks versus the external placebo, which were further improved at 66 weeks.
Eplontersen achieved statistically significant improvements in all secondary endpoints versus the external placebo group.
Eplontersen continued to demonstrate a favorable safety and tolerability profile. The rate of treatment emergent adverse events in the eplontersen group was comparable to the external placebo group across all major categories. There were no adverse events of special interest that led to study drug discontinuation.
"In the past, patients with hereditary transthyretin amyloid polyneuropathy usually deteriorated given the limited available treatments. This new study shows eplontersen can halt progression of neuropathy and improve quality of life at 66 weeks when compared to placebo," said Sami Khella, M.D., chief, department of neurology at Penn Presbyterian Medical Center, professor of clinical neurology at the Perelman School of Medicine at the University of Pennsylvania School of Medicine and a principal investigator on the NEURO-TTRansform study. "Today's important results demonstrate that eplontersen has a consistent and sustained treatment effect and reinforces its potential as an important medicine for the thousands of patients living with this debilitating and fatal disease."
"In the NEURO-TTRansform study, we were encouraged to see a substantial number of patients treated with eplontersen improved in measures of neuropathy impairment and quality of life at both the interim and final analyses," said Eugene Schneider, M.D., executive vice president and chief clinical development officer for Ionis. "We and our partners at AstraZeneca are especially grateful to the patients who participated in this study. With our potential approval in the U.S. in December and plans to file for regulatory approval in the EU and other countries, we are looking forward to potentially bringing eplontersen to ATTRv-PN patients in this largely underrecognized global patient population."
The NEURO-TTRansform Emerging Science presentation and poster at AAN can be found on Ionis' website after today's AAN presentation at 11:57 a.m. ET.
As part of a global development and commercialization agreement, Ionis and AstraZeneca are seeking regulatory approval for eplontersen for the treatment of ATTRv-PN in the U.S. and plan to seek regulatory approval in Europe and other parts of the world. The U.S. Food and Drug Administration accepted the New Drug Application for eplontersen for the treatment of ATTRv-PN with a PDUFA action date of December 22, 2023. Eplontersen was granted Orphan Drug Designation in the U.S.
Eplontersen is currently being evaluated in the Phase 3 CARDIO-TTRansform study for transthyretin-mediated amyloid cardiomyopathy (ATTR-CM), a systemic, progressive and fatal condition that typically leads to progressive heart failure and often death within three to five years from disease onset.
Webcast
Ionis will host a webcast to discuss the detailed 66-week results from the NEURO-TTRansform study on Tuesday, April 25 at 1 p.m. ET. Interested parties may access the webcast here. A webcast replay will be available for a limited time.
About Eplontersen
Eplontersen is an investigational LIgand-Conjugated Antisense (LICA) medicine designed to inhibit the production of TTR protein. Eplontersen is being developed as a monthly self-administered subcutaneous injection to treat all types of ATTR. ATTR amyloidosis is a systemic, progressive and fatal disease in which patients experience multiple overlapping clinical manifestations caused by the inappropriate formation and aggregation of TTR amyloid deposits in various tissues and organs, including peripheral nerves, heart, intestinal tract, eyes, kidneys, central nervous system, thyroid and bone marrow. The progressive accumulation of TTR amyloid deposits in these tissues and organs leads to organ failure and eventually death.
About Hereditary Transthyretin-Mediated Amyloid Polyneuropathy (ATTRv-PN)
Hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN) is caused by the accumulation of misfolded mutated TTR protein in the peripheral nerves. Patients with ATTRv-PN experience ongoing debilitating nerve damage throughout their body resulting in the progressive loss of motor functions, such as walking. These patients also accumulate TTR in other major organs, which progressively compromises their function. The damage from misfolded TTR protein accumulation leads to disability within five years of diagnosis and is generally fatal within a decade.
About the NEURO-TTRansform Study
NEURO-TTRansform is a global, open-label, randomized trial evaluating the efficacy and safety of eplontersen in patients with ATTRv-PN. The trial enrolled 168 adult patients with ATTRv-PN Stage 1 or Stage 2 and up to week 66 eplontersen is being compared to the external placebo group from the NEURO-TTR registrational trial for inotersen that Ionis completed in 2017. The final analysis comparing eplontersen to external placebo was completed at week 66 and all patients will be followed on treatment until week 85, when they will have the option to transition into an open-label extension study. For more information on the NEURO-TTRansform study, please visit: https://clinicaltrials.gov/ct2/show/NCT04136184
About Ionis Pharmaceuticals, Inc.
For more than 30 years, Ionis has been a leader in RNA-targeted therapy, pioneering new markets and changing standards of care with its novel antisense technology. Ionis currently has three marketed medicines and a promising late-stage pipeline highlighted by cardiovascular and neurological franchises. Our scientific innovation began and continues with the knowledge that sick people depend on us, which fuels our vision to become the leader in genetic medicine, utilizing a multi-platform approach to discover, develop and deliver life-transforming therapies.
To learn more about Ionis visit www.ionispharma.com and follow us on Twitter @ionispharma.
Cision View original content to download multimedia:https://www.prnewswire.com/news-releases/eplontersen-halted-attrv-pn-disease-progression-and-improved-neuropathy-impairment-and-quality-of-life-in-phase-3-study-through-66-weeks-301804971.html
SOURCE Ionis Pharmaceuticals, Inc.
Ionis, AstraZeneca's eplontersen meets goals in phase 3 ATTRv-PN trial
Apr. 24, 2023 8:12 AM ETIonis Pharmaceuticals, Inc. (IONS), AZNBy: Jonathan Block, SA News Editor4 Comments
Eplontersen, a late-stage candidate from Ionis Pharmaceuticals (NASDAQ:IONS) and AstraZeneca (NASDAQ:AZN) for hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN), met all primary and secondary endpoints in a phase 3 trial at 66 weeks.
Resmetirom
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Madrigal Receives Breakthrough Therapy Designation from FDA for Resmetirom and Completes Enrollment of the Phase 3 MAESTRO-NASH Biopsy Trial
CONSHOHOCKEN, Pa., April 18, 2023 (GLOBE NEWSWIRE) -- Madrigal Pharmaceuticals, Inc. (NASDAQ:MDGL), a clinical-stage biopharmaceutical company pursuing novel therapeutics for nonalcoholic steatohepatitis (NASH), today announced that resmetirom has received Breakthrough Therapy designation from the U.S. Food and Drug Administration (FDA) for the treatment of patients with NASH with liver fibrosis. The Company also announced that the outcomes portion of the Phase 3 MAESTRO-NASH biopsy trial has completed enrollment.
Paul Friedman, M.D., Chief Executive Officer of Madrigal, stated, “The Breakthrough Therapy designation for resmetirom reflects the FDA’s recognition of resmetirom's potential in the treatment of NASH as a serious, life-threatening condition and an important area of investigational drug development. It also reinforces our confidence in our regulatory strategy as we approach the new drug application (NDA) filing for resmetirom, which remains on track for Q2 2023. The filing is supported by the positive outcomes on reduction of liver fibrosis and resolution of NASH from the 52-week serial liver biopsy portion of MAESTRO-NASH.”
Becky Taub, M.D., Chief Medical Officer and President of Research & Development of Madrigal, stated, "We are also pleased to announce that the MAESTRO-NASH trial in noncirrhotic NASH is now fully enrolled. Enrollment of the MAESTRO-NASH study was closed at approximately 1,750 patients based on the enrollment target of the 54-month long-term clinical outcome portion of the study. Patient recruitment remains focused on MAESTRO-NASH-OUTCOMES, a Phase 3 clinical outcome trial evaluating resmetirom in patients with well-compensated NASH cirrhosis that provides a second and potentially earlier opportunity to support full approval for both noncirrhotic and cirrhotic NASH. Madrigal’s two Phase 3 outcomes studies are central to our regulatory strategy and underscore our commitment to verifying clinical benefit of resmetirom. On behalf of the Madrigal team, I’d like to thank all the patients, investigators and study sites that are participating in our ongoing trials.”
Breakthrough Therapy designation is a process intended to expedite the development and review of drugs for serious or life-threatening conditions. The criteria for breakthrough therapy designation require preliminary clinical evidence that demonstrates the drug may have substantial improvement on at least one clinically significant endpoint over available therapy, or over placebo if there is no available therapy. A drug that receives Breakthrough Therapy designation is eligible for more intensive guidance on an efficient drug development program and organizational commitment involving senior managers from FDA.
About the Resmetirom Phase 3 Registration Program for the Treatment of NASH
Madrigal is currently conducting four Phase 3 clinical trials to demonstrate the safety and efficacy of resmetirom for the treatment of NASH: MAESTRO-NASH, MAESTRO-NAFLD-1, MAESTRO-NAFLD-OLE, and MAESTRO-NASH-OUTCOMES.
MAESTRO-NASH is a multicenter, randomized, double-blind, placebo-controlled Phase 3 study of resmetirom in patients with liver biopsy-confirmed NASH and was initiated in March 2019. The subpart H portion of the study enrolled more than 1,000 patients with biopsy-proven NASH (at least half with F3 (advanced) fibrosis, the remainder F2 or F1B (moderate fibrosis) with a few earlier F1 patients, randomized 1:1:1 to receive once-daily resmetirom 80 mg, resmetirom 100 mg, or placebo. After 52 weeks of treatment, a second liver biopsy is performed. The dual primary surrogate endpoints on biopsy were NASH resolution with ≥2-point reduction in NAS (NAFLD Activity Score), and with no worsening of fibrosis OR a 1-point decrease in fibrosis with no worsening of NAS. Achievement of either primary endpoint was considered a successful trial outcome. A key secondary endpoint was lowering of LDL-C.
Patients enrolled in the MAESTRO-NASH study (approximately 1,750) continue on therapy after the initial 52-week treatment period for up to 54 months to accrue and measure hepatic clinical outcome events including progression to cirrhosis on biopsy (52 weeks and 54 months) and hepatic decompensation events, as well as all-cause mortality.
MAESTRO-NAFLD-1 was initiated in December 2019 and the 52-week multicenter, randomized, placebo-controlled Phase 3 study of resmetirom in over 1,200 patients with NAFLD, presumed NASH, has completed the double-blind arms and an open-label 100 mg arm. An additional open-label active treatment arm in patients with early (well-compensated) NASH cirrhosis is ongoing. The primary endpoint was to evaluate the safety and tolerability of resmetirom. A separate 52 week Phase 3 clinical trial, an open-label extension study of MAESTRO-NAFLD-1 (MAESTRO-NAFLD-OLE), is ongoing.
Patients in the 52-week Phase 3 MAESTRO-NAFLD-1 study were randomized 1:1:1:1 to receive once-daily resmetirom 80 mg, resmetirom 100 mg, placebo in double-blind arms or resmetirom 100 mg in an open-label arm. MAESTRO-NAFLD-1 (unlike MAESTRO-NASH), did not include a liver biopsy and represents a “real-life” NASH study. Patients with 3 metabolic risk factors were documented with NASH or NAFLD by historical liver biopsy or noninvasive techniques. Using noninvasive measures, MAESTRO-NAFLD-1 was designed to provide incremental safety information to support the NASH indication as well as provide additional data regarding clinically relevant key secondary efficacy endpoints to better characterize the potential clinical benefits of resmetirom on cardiovascular- and liver-related endpoints. The primary safety endpoint and several key secondary endpoints were met, including LDL-C, apolipoprotein B, and triglyceride lowering and reduction of liver fat as determined by MRI-PDFF. Additional secondary and exploratory endpoints were assessed including reduction in liver enzymes, FibroScan, and MRE scores, and other NASH biomarkers.
Data from the 52-week first 1,000 patient portion of MAESTRO-NASH, together with data from MAESTRO-NAFLD-1, MAESTRO-NAFLD-OLE, Phase 2 and Phase 1 data, including safety parameters, will form the basis for a planned subpart H submission to FDA for accelerated approval of resmetirom for treatment of NASH.
In August 2022, Madrigal initiated MAESTRO-NASH-OUTCOMES, a randomized double-blind placebo-controlled study in approximately 700 patients with early NASH cirrhosis to allow for noninvasive monitoring of progression to liver decompensation events. A positive outcome is expected to support the full approval of resmetirom for noncirrhotic NASH, potentially accelerating the timeline to full approval. In addition, this study has the potential to support an additional indication for resmetirom in patients with well-compensated NASH cirrhosis.
About NASH
Nonalcoholic steatohepatitis (NASH) is a more advanced form of nonalcoholic fatty liver disease (NAFLD). NAFLD is estimated to afflict more than 20% of adults globally, about 30% in the United States. Of that population, 20% may have NASH.
NASH is a leading cause of liver related mortality and an increasing burden on healthcare systems globally. Additionally, patients with NASH, especially those with more advanced metabolic risk factors (hypertension, concomitant type 2 diabetes), are at increased risk for adverse cardiovascular events and increased morbidity and mortality.
Once NASH progresses to significant liver fibrosis (stages F2 and F3) the risk of adverse liver outcomes increases dramatically. NASH is rapidly becoming the leading cause of liver transplantation in the U.S. There are currently no FDA-approved therapies available for the treatment of NASH.
About Madrigal Pharmaceuticals
Madrigal Pharmaceuticals, Inc. (Nasdaq: MDGL) is a clinical-stage biopharmaceutical company pursuing novel therapeutics for nonalcoholic steatohepatitis (NASH), a liver disease with high unmet medical need. Madrigal’s lead candidate, resmetirom, is a once daily, oral, thyroid hormone receptor (THR)-β selective agonist designed to target key underlying causes of NASH in the liver. For more information, visit www.madrigalpharma.com.
Source: Madrigal Pharmaceuticals, Inc.
Madrigal rises on FDA breakthrough therapy tag for liver disease drug resmetirom
Apr. 18, 2023 8:31 AM ET
Madrigal Pharmaceuticals, Inc. (MDGL)
By: Ravikash, SA News Editor13 Comments
- The U.S. Food and Drug Administration (FDA) granted breakthrough therapy designation to Madrigal Pharmaceuticals' (NASDAQ:MDGL) resmetirom to treat patients with nonalcoholic steatohepatitis (NASH) with liver fibrosis.
- https://seekingalpha.com/news/3957291-madrigal-stock-rises-on-fda-breakthrough-tag-for-liver-drug-resmetirom
- Madrigal Pharmaceuticals, Inc. (MDGL)
- https://www.madrigalpharma.com/our-programs/resmetirom/
- https://www.madrigalpharma.com/
botensilimab (AGEN1181) and balstilimab (AGEN2034)
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
botensilimab (AGEN1181) and balstilimab (AGEN2034)
Agenus Receives Fast Track Designation for Botensilimab and Balstilimab in Colorectal Cancer
April 17, 2023
LEXINGTON, Mass.--(BUSINESS WIRE)--Apr. 17, 2023-- Agenus Inc. (Nasdaq: AGEN), a leading immuno-oncology company specializing in immunological agents for cancer and infectious diseases, has been granted Fast Track Designation from the US Food and Drug Administration (FDA) for the investigation of the combination of botensilimab (AGEN1181) and balstilimab (AGEN2034). The designation is for patients with non-microsatellite instability-high (MSI-H)/deficient mismatch repair (dMMR) metastatic colorectal cancer with no active liver involvement. Patients targeted with this designation are heavily pretreated are resistant or intolerant to a fluoropyrimidine, oxaliplatin, and irinotecan, and who have also received a VEGF inhibitor, an EGFR inhibitor and/or a BRAF inhibitor, if indicated. The company is conducting a global, randomized Phase 2 trial of botensilimab in combination with balstilimab compared to standard of care in non-microsatellite instability-high (non-MSI-H) colorectal cancer patients.
"We are pleased that the FDA has granted Fast Track designation for the combination of botensilimab with balstilimab in patients with non-MSI-H colorectal cancer, recognizing the high unmet medical need in this population," said Dr. Steven O’Day, Chief Medical Officer of Agenus. "The Fast Track designation offers important benefits, including the potential eligibility for a Priority Review, and we will be working with the FDA and all key stakeholders to rapidly advance the botensilimab/balstilimab combination in colorectal cancer as well as other solid tumor indications.”
During the American Society of Clinical Oncology – Gastrointestinal Cancers Symposium in January 2023, Agenus presented positive results from its ongoing clinical trials of the botensilimab/balstilimab combination in patients with non-MSI-H colorectal cancer. The combination therapy showed an overall response rate of 23% and a 12-month survival rate of 63%, which compares to very limited activity of 1-2% overall response rate and ~25% 12-month survival rate reported for the standard of care. Responses to the botensilimab/balstilimab therapy have been durable, with 69% ongoing at data cut-off, and median overall survival not reached.
About Botensilimab
Botensilimab is a novel, multifunctional CTLA-4 investigational antibody that has been designed to extend clinical benefits to “cold” tumors that have not historically responded to standard of care or investigational therapies. In addition to binding to the CTLA-4 receptor, its Fc-enhanced structure induces a memory immune response, downregulates regulatory T cells, and delivers better priming and activation of T cells, thereby amplifying immune responses.
In a Phase 1b clinical study of more than 350 patients, botensilimab has demonstrated clinical responses in nine, previously IO unresponsive, solid tumor cancers, either alone or in combination with Agenus’ PD-1 antibody, balstilimab (data presented at ASCO GI 2023, SGO 2023, CTOS 2022, SITC 2022). Agenus is conducting global, randomized Phase 2 trials in non-MSI-H colorectal cancer, pancreatic cancer, and melanoma as part of its ACTIVATE trial programs. Additional information about these botensilimab trials can be found at www.clinicaltrials.gov under the identifiers NCT05608044, NCT05630183, and NCT05529316, respectively. A global Phase 3 trial in non-MSI-H CRC is expected to launch in 2023.
About Agenus
Agenus is a clinical-stage immuno-oncology company focused on the discovery and development of therapies that engage the body's immune system to fight cancer and infections. The Company's vision is to expand the patient populations benefiting from cancer immunotherapy by pursuing combination approaches that leverage a broad repertoire of antibody therapeutics, adoptive cell therapies (through its subsidiary MiNK Therapeutics), and adjuvants (through its subsidiary SaponiQx). The Company is equipped with a suite of antibody discovery platforms and a state-of-the-art GMP manufacturing facility with the capacity to support clinical programs. Agenus is headquartered in Lexington, MA. For more information, please visit www.agenusbio.com and our Twitter handle @agenus_bio. Information that may be important to investors will be routinely posted on our website and Twitter.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230417005330/en/
Source: Agenus Inc.
Agenus wins FDA fast track tag for colorectal cancer therapy
Apr. 17, 2023 8:21 AM ET
By: Dulan Lokuwithana, SA News Editor1 Comment
Agenus (NASDAQ:AGEN) announced Monday that the FDA granted Fast Track Designation for a combination therapy containing its anti-CTLA-4 compound botensilimab (AGEN1181) and anti-PD-1 molecule balstilimab (AGEN2034) as a treatment for certain colorectal cancer.
RGX-202
LUPKYNIS® (voclosporin) capsules
botensilimab (AGEN1181) and balstilimab (AGEN2034)
REGENXBIO Receives FDA Fast Track Designation for RGX-202, a Novel Gene Therapy Candidate for the Treatment of Duchenne Muscular Dystrophy
Apr 11, 2023 at 7:05 AM EDT
- RGX-202 is a potential one-time AAV Therapeutic for the treatment of Duchenne and includes an optimized transgene for a novel microdystrophin and REGENXBIO's proprietary NAV® AAV8 vector
- Commercial-scale cGMP material from the REGENXBIO Manufacturing Innovation Center to be used in the clinical trial
- AFFINITY DUCHENNE™ Phase I/II trial of RGX-202 is active and recruiting patients; anticipated to report initial trial data in the second half of 2023
ROCKVILLE, Md., April 11, 2023 /PRNewswire/ -- REGENXBIO Inc. (Nasdaq: RGNX) today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation for RGX-202, a potential one-time gene therapy for the treatment of Duchenne muscular dystrophy (Duchenne).
Fast Track designation aims to facilitate the development and expedite the review of new therapeutics that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs. Therapies granted this designation are given the opportunity for more frequent interactions with the FDA and may qualify for priority review. The FDA has granted RGX-202 Orphan Drug Designation and Rare Pediatric Disease Designation.
"Fast Track designation, along with our capabilities to conduct our clinical trials using commercial-scale cGMP material, will further support the efficient development of RGX-202 from clinic to commercial readiness," said Kenneth T. Mills, President, and Chief Executive Officer of REGENXBIO. "RGX-202 is a key part of our '5x25' strategy, and we look forward to continuing to work closely with the FDA and the Duchenne community as we advance a highly differentiated product candidate developed with the potential to make a meaningful difference for patients. We look forward to reporting initial data from our clinical trial of RGX-202 in the second half of this year."
"We are pleased that the FDA has granted Fast Track designation for RGX-202," said Debra Miller, Founder and CEO of CureDuchenne. "Accelerating the development of medicines for Duchenne, especially potential one-time gene therapies like RGX-202, is critical for this community."
RGX-202 Clinical Program
In January, REGENXBIO announced that the Phase I/II AFFINITY DUCHENNE™ trial of RGX-202 for the treatment of Duchenne is now active and recruiting patients. AFFINITY DUCHENNE is a multicenter, open-label dose evaluation and dose expansion clinical study to evaluate the safety, tolerability and clinical efficacy of a one-time intravenous (IV) dose of RGX-202 in patients with Duchenne. Six ambulatory, pediatric patients (ages 4 to 11 years old) with Duchenne are expected to enroll in two cohorts with doses of 1x1014 genome copies (GC)/kg body weight (n=3) and 2x1014 GC/kg body weight (n=3). After an independent safety data review for each cohort, a dose expansion phase of the trial may allow for up to six additional patients to be enrolled at each dose level (for a total of up to nine patients in each dose cohort).
Additionally, REGENXBIO is recruiting patients in the AFFINITY BEYOND™ trial, an observational screening study to evaluate the prevalence of AAV8 antibodies in patients with Duchenne up to 12 years of age. Information collected in this study may be used to identify potential participants for the AFFINITY DUCHENNE trial and potential future trials of RGX-202.
REGENXBIO Gene Therapy Manufacturing
REGENXBIO has manufactured additional clinical supply of RGX-202 in its in-house Manufacturing Innovation Center using the NAVXpress™ platform process. Located in REGENXBIO's headquarters in Rockville, MD, the Manufacturing Innovation Center is designed to meet global clinical and commercial regulatory standards, and includes two independent bulk drug substance production suites, a final drug product suite and integrated quality control labs. REGENXBIO is one of only a few gene therapy companies worldwide with a cGMP facility capable of production at scales up to 2,000 liters.
About RGX-202
RGX-202 is designed to deliver a transgene for a novel microdystrophin that includes the functional elements of the C-Terminal (CT) domain found in naturally occurring dystrophin. Presence of the CT domain has been shown in preclinical studies to recruit several key proteins to the muscle cell membrane, leading to improved muscle resistance to contraction-induced muscle damage in dystrophic mice. Additional design features, including codon optimization and reduction of CpG content, may potentially improve gene expression, increase translational efficiency and reduce immunogenicity. RGX-202 is designed to support the delivery and targeted expression of genes throughout skeletal and heart muscle using the NAV AAV8 vector, a vector used in numerous clinical trials, and a well-characterized muscle-specific promoter (Spc5-12). RGX-202 has been granted Fast Track, Orphan Drug and Rare Pediatric Disease designations by the FDA.
About Duchenne Muscular Dystrophy
Duchenne muscular dystrophy (Duchenne) is a rare genetic disorder, caused by mutations in the gene responsible for making dystrophin, a protein of central importance for muscle cell structure and function. Duchenne primarily affects males with approximately 1 in 3,500 to 1 in 5,000 males affected worldwide. The absence of functional dystrophin protein in individuals with Duchenne results in cell damage during muscle contraction, leading to cell death, inflammation, and fibrosis in muscle tissues. Initial symptoms of Duchenne include muscle weakness that is often noticeable at an early age, with diagnosis typically occurring by 5 years of age. Over time, individuals with Duchenne experience progressive muscle weakness and eventually lose the ability to walk. Respiratory and heart muscles are also affected, leading to difficulty breathing and the need for ventilator assistance, along with the development of cardiomyopathy. There is presently no cure for Duchenne.
About REGENXBIO Inc.
REGENXBIO is a leading clinical-stage biotechnology company seeking to improve lives through the curative potential of gene therapy. REGENXBIO's NAV Technology Platform, a proprietary adeno-associated virus (AAV) gene delivery platform, consists of exclusive rights to more than 100 novel AAV vectors, including AAV7, AAV8 and AAV9. REGENXBIO and its third-party NAV Technology Platform Licensees are applying the NAV Technology Platform in the development of a broad pipeline of candidates, including late-stage and commercial programs, in multiple therapeutic areas. REGENXBIO is committed to a "5x'25" strategy to progress five AAV Therapeutics from our internal pipeline and licensed programs into pivotal-stage or commercial products by 2025.
Cision View original content to download multimedia:
SOURCE REGENXBIO Inc.
Regenxbio stock pops on FDA fast track tag for Duchenne gene therapy RGX-202
Apr. 11, 2023 9:14 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted fast track designation to Regenxbio's (NASDAQ:RGNX) one-time gene therapy RGX-202 to treat Duchenne muscular dystrophy (DMD).
- https://seekingalpha.com/news/3955625-regenxbio-stock-pops-fda-fast-track-tag-duchenne-gene-therapy-rgx-202
- REGENXBIO Inc. (RGNX)
- https://www.regenxbio.com/therapeutic-programs/rgx-202/
- https://www.regenxbio.com/home/
LUPKYNIS® (voclosporin) capsules
LUPKYNIS® (voclosporin) capsules
LUPKYNIS® (voclosporin) capsules
Aurinia Pharmaceuticals Announces Promising Topline Data from Renal Biopsy Sub-study of the AURORA Trial
APRIL 05, 2023
LUPKYNIS® treated patients showed histologic activity improvement with stable chronicity scores similar to active control arm of mycophenolate mofetil (MMF) and low dose steroids alone
Data further reinforces differentiation of LUPKYNIS from first generation calcineurin inhibitors (CNIs)
Conference call to be hosted today at 8:30 a.m. EDT
EDMONTON, Alberta--(BUSINESS WIRE)-- Aurinia Pharmaceuticals Inc. (NASDAQ: AUPH) (Aurinia or the Company) today announced promising results from the AURORA Renal Biopsy Sub-Study. LUPKYNIS is a novel agent approved for the treatment of adults with active lupus nephritis (LN). The addition of LUPKYNIS on top of the then current standard of care MMF and low-dose steroids in Aurinia’s Phase 3 AURORA 1 and AURORA 2 studies led to significantly earlier and greater reductions in proteinuria while maintaining stable renal function, as evidenced by a stable estimated glomerular filtration rate (eGFR) slope over time. To further characterize the long-term impact of LUPKYNIS on the kidney at the histologic level, repeat biopsies were collected from selected patients in both treatment arms (the active control arm with patients treated with only MMF and steroids, and the study arm of voclosporin in combination with MMF and steroids). The patients in the voclosporin treatment arm demonstrated histologic activity improvement with stable chronicity scores similar to the active control arm of MMF and low dose steroids alone over the 18-months average treatment period at the time of repeat biopsy.
“We are encouraged by these results,” said Dr. Greg Keenan, recently appointed Chief Medical Officer of Aurinia. “Seeing similar improvement in the activity scores and absence of change in the chronicity scores with the LUPKYNIS treated patients as compared to those on MMF and low dose steroids alone strengthens the totality of the evidence supporting the long-term efficacy and safety of LUPKYNIS and further differentiates the safety of this second-generation treatment from the legacy, first generation CNIs.”
Repeat renal biopsies were obtained from 16 patients in the voclosporin arm and 10 patients in the active control arm over 18 months from study entry. Baseline and follow-up activity scores, a measure of active inflammation in LN, and chronicity scores, a measure of irreversible kidney injury, were obtained using a validated assessment tool. Compared to baseline, the activity scores for both LUPKYNIS and active control populations improved to a similar degree, while the chronicity scores remained stable over time in both arms.
Dr. Brad Rovin, Professor of Nephrology and Director, Division of Nephrology at the Ohio State University Wexner Medical Center said, “The lack of histologic evidence of CNI nephrotoxicity and the absence of progression of chronic kidney damage after approximately 18 months of treatment further strengthen the overall evidence supporting the long-term safety of LUPKYNIS in LN patients.”
Further data will be presented at the upcoming Congress of Clinical Rheumatology meeting, May 4-7, 2023. Aurinia will host a conference call/webcast at 8:30 am EDT to review these results. Interested participants can dial 877-407-9170 / +1 201-493-6756 (Toll-free U.S. & Canada). The audio and webcast can also be accessed under "News/Events” through the “Investors” section of the Aurinia corporate website at www.auriniapharma.com.
About Lupus Nephritis
Lupus Nephritis is a serious manifestation of systemic lupus erythematosus (SLE), a chronic and complex autoimmune disease. About 200,000-300,000 people live with SLE in the U.S. and about one-third of these people are diagnosed with lupus nephritis at the time of their SLE diagnosis. About 50 percent of all people with SLE may develop lupus nephritis. If poorly controlled, lupus nephritis can lead to permanent and irreversible tissue damage within the kidney. Black and Asian people with SLE are four times more likely to develop lupus nephritis and Hispanic people are approximately twice as likely to develop the disease compared to White people with SLE. Black and Hispanic people with SLE also tend to develop lupus nephritis earlier and have poorer outcomes, compared to White people with SLE.
About LUPKYNIS
LUPKYNIS® is the first U.S. FDA- and EC-approved oral medicine for the treatment of adult patients with active LN. LUPKYNIS is a novel, structurally modified calcineurin inhibitor (CNI) with a dual mechanism of action, acting as an immunosuppressant through inhibition of T-cell activation and cytokine production and promoting podocyte stability in the kidney. The recommended starting dose of LUPKYNIS is three capsules twice daily with no requirement for serum drug monitoring. Dose modifications can be made based on Aurinia’s proprietary personalized eGFR-based dosing protocol. Boxed Warning, warnings, and precautions for LUPKYNIS are consistent with those of other CNI-immunosuppressive treatments.
About Aurinia
Aurinia Pharmaceuticals is a fully integrated biopharmaceutical company focused on delivering therapies to treat targeted patient populations with a high unmet medical need that are impacted by autoimmune, kidney and rare diseases. In January 2021, the Company introduced LUPKYNIS® (voclosporin), the first FDA-approved oral therapy dedicated to the treatment of adult patients with active lupus nephritis. The Company’s head office is in Edmonton, Alberta, its U.S. commercial office is in Rockville, Maryland. The Company focuses its development efforts globally.
INDICATION AND IMPORTANT SAFETY INFORMATION
INDICATIONS
LUPKYNIS is indicated in combination with a background immunosuppressive therapy regimen for the treatment of adult patients with active LN. Limitations of Use: Safety and efficacy of LUPKYNIS have not been established in combination with cyclophosphamide. Use of LUPKYNIS is not recommended in this situation.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230405005355/en/
Source: Aurinia Pharmaceuticals Inc.
Released April 5, 2023
Aurinia's Lupkynis shows promise in 18-month kidney biopsy data
Apr. 05, 2023 7:07 AM ET
Aurinia Pharmaceuticals Inc. (AUPH)
By: Ravikash, SA News Editor1 Comment
Aurinia Pharmaceuticals (NASDAQ:AUPH) said biopsy data collected from its phase 3 program AURORA showed promising long term results for its oral drug Lupkynis to treat adults with active lupus nephritis (LN).
LN is a type of kidney disease caused by systemic lupus erythematosus (SLE) or lupus an autoimmune disease.
The company said repeat biopsies were collected from selected patients in both treatment groups — the active control group wherein patients were given only mycophenolate mofetil (MMF) and steroids; and the study group, in which patients were on Lupkynis (voclosporin) in combination with MMF and steroids. The phase 3 program included the AURORA 1 and AURORA 2 studies.
https://seekingalpha.com/news/3954599-aurinia-lupkynis-shows-promise-18-month-kidney-biopsy-data
Aurinia Pharmaceuticals Inc. (AUPH)
Please see Prescribing Information, including Boxed Warning, and Medication Guide for LUPKYNIS.
ANAVEX®2-73 (Blarcamesine)
LUPKYNIS® (voclosporin) capsules
LUPKYNIS® (voclosporin) capsules
ANAVEX®2-73 (Blarcamesine) Shows Clinical Benefit in Long-Term 48Week Phase 2 Extension Study in PDD
Study successfully achieved both primary and secondary objectives
ANAVEX®2-73 treatment resulted in improvements of all efficacy endpoints over 48 Weeks
Anavex plans to proceed to ANAVEX®2-73 pivotal trial for Parkinson’s disease
NEW YORK – March 30, 2023
Anavex Life Sciences Corp. (“Anavex” or the “Company”) (Nasdaq: AVXL), a clinical-stage biopharmaceutical company developing differentiated therapeutics for the treatment of neurodegenerative and neurodevelopmental disorders including Alzheimer’s disease, Parkinson’s disease, Rett syndrome, and other Central Nervous System (CNS) disorders, reports preliminary 48-week open-label extension Parkinson’s disease dementia ANAVEX®2-73-PDD-EP-001 Phase 2 study data which demonstrated longitudinal beneficial effects of ANAVEX®2-73 on the prespecified primary and secondary objectives, as well as planned primary and key secondary endpoints which will be utilized in a forthcoming pivotal study of ANAVEX®2-73 in Parkinson’s disease.
ANAVEX®2-73 (blarcamesine) is an oral small-molecule activator of the sigma-1 receptor (SIGMAR1), which data suggests is pivotal to restoring neural cell homeostasis and promoting neuroplasticity.[1]
Parkinson’s disease (PD) is a chronic, debilitating CNS disease and the second largest age-related disorder after Alzheimer’s disease.[2] This study demonstrates for the first-time that patients’ clinical symptoms consistently improve longitudinally during the 48-week ANAVEX2-73-PDD-EP-001 Phase 2 study under active ANAVEX®2-73 treatment in Parkinson’s disease.
The 48-week ANAVEX2-73-PDD-EP-001 (NCT04575259) Phase 2 study assessed safety, tolerability and efficacy, measuring among others, Movement Disorder Society-Unified Parkinson's Disease Rating Scale (MDS-UPDRS)[3]Parts I, II, III, REM Sleep Behavior Disorder Screening Questionnaire (RBDSQ), Clinical Global Impression – Improvement (CGI-I), as well as cognitive efficacy endpoint Montreal Cognitive Assessment (MoCA) over a 48-week period.
Preliminary analysis reveals that ANAVEX®2-73 (blarcamesine) was found to be generally safe and well tolerated; and safety findings in this study are consistent with the known safety profile of ANAVEX®2-73. In respect to efficacy, across all efficacy endpoints, patients performed better while on ANAVEX®2-73.
The 48-week Open Label Extension (OLE) ANAVEX2-73-PDD-EP-001 Phase 2 study was offered to participants after completion of the double-blind placebo-controlled ANAVEX2-73-PDD-001 Phase 2 study. Study participants were allowed to stay on a stable regimen of anti-Parkinson's disease medications (including levodopa, dopamine agonists, MAO-B inhibitors, or entacapone).
Previously, in the double-blind ANAVEX2-73-PDD-001 Phase 2 study, ANAVEX®2-73 treatment demonstrated statistically significant improvements compared to placebo (ITT population) for MDS-UPDRS Total score. From baseline to the end of the trial at 14 weeks, the MDS-UPDRS Total score improved by -10.98 points in the ANAVEX®2-73 high dose group and worsened by 3.53 points in the placebo group, an adjusted mean difference of -14.51 points (p = 0.034). This corresponds to a relative improvement of 18.9% over 14 weeks.[4] This data was also consistent with expression levels of pathological dysregulated neurodegenerative genes, including Parkinson’s disease genes, which were significantly restored by the therapeutic effect of ANAVEX®2-73 (p<0.005).[5]
Due to the COVID-19 pandemic, the start of the extension phase was delayed, on average, by approximately 41 weeks at the end of the preceding double-blind placebo-controlled study (DB). This led to a reduced enrollment rate for the extension phase. The period between the end of the double-blind phase to the start of the extension phase, where patients were not on ANAVEX®2-73 treatment, is known as a ‘drug holiday’. The drug holiday period of treatment separation provided an opportunity to compare the trajectory of clinical scores between no ANAVEX®2-73 treatment (drug holiday) and ANAVEX®2-73 treatment in the extension phase.
All efficacy endpoints, which includes the MDS-UPDRS Part II + III and Clinical Global Impression – Improvement (CGI-I) measured at the end of trial of the double-blind study (DB EOT), the OLE Baseline, OLE Week 24, and OLE Week 48, showed a worsening during the drug holiday. However, a consistent improvement was observed during the extension phase when patients resumed ANAVEX®2-73 treatment. These results are consistent with the pattern observed for all efficacy measures in the extension phase (see Chart and Table).[6]
The two endpoints, MDS-UPDRS Part II + III and Clinical Global Impression – Improvement (CGI-I) measured in this study are the planned primary and key secondary endpoints in Anavex’s forthcoming pivotal 6-month Parkinson’s disease study.
“It is encouraging that the patients’ clinical symptoms consistently improved longitudinally over time during the extension phase under active ANAVEX®2-73 treatment,” said Christopher U Missling, PhD, President & CEO of Anavex. “This data suggests ANAVEX®2-73’s potential capability to slow and potentially reverse the life altering symptoms of Parkinson’s disease, an urgent unmet global need.”
Moreover, at the request of the participants completing the 48-week open-label extension study, patient requested treatment with ANAVEX®2-73 is continuing beyond the open-label 48-weeks through the compassionate use Special Access Scheme. Currently, participants in the compassionate use program for ANAVEX®2-73 have been on average, for over 2 years and counting.
The Michael J. Fox Foundation (MJFF) awarded Anavex a research grant for an imaging-focused Parkinson’s disease clinical trial with ANAVEX®2-73.[7]MJFF previously awarded Anavex a research grant, which fully funded a preclinical study that established ANAVEX®2-73 as a potentially disease-modifying treatment for Parkinson’s disease.[8]
Anavex Life Sciences’ therapeutic product platform includes orally available small molecule lead drug candidate ANAVEX®2-73 for the treatment of Alzheimer’s disease, Parkinson’s disease and Rett syndrome and ANAVEX®3-71 for schizophrenia, Alzheimer’s disease, and frontotemporal dementia.
About Parkinson’s Disease (PD)
Parkinson’s disease is a chronic and progressive neurological disorder that is characterized by well-known motor symptoms including tremors, stiffness of limbs, slowness of movements, and difficulties with posture and balance, as well as by non-motor symptoms. It is the second most common neurological disorder and approximately one million people in the United States, and more that 10 million people worldwide, live with this disease. Parkinson’s disease is more common in people over 60 years of age and its prevalence is expected to increase significantly as the average age of the population increases. Current Parkinson’s treatments are only effective in managing symptoms of the disease, mainly through the use of levodopa and dopamine agonists. As the disease progresses and dopaminergic neurons continue to be lost, these drugs eventually become less effective at treating the symptoms.
About Anavex Life Sciences Corp.
Anavex Life Sciences Corp. (Nasdaq: AVXL) is a publicly traded biopharmaceutical company dedicated to the development of novel therapeutics for the treatment of neurodegenerative and neurodevelopmental disorders, including Alzheimer's disease, Parkinson's disease, Rett syndrome, and other central nervous system (CNS) diseases, pain, and various types of cancer. Anavex's lead drug candidate, ANAVEX®2-73 (blarcamesine), has successfully completed a Phase 2a and recently a Phase 2b/3 clinical trial for Alzheimer's disease, a Phase 2 proof-of-concept study in Parkinson's disease dementia, and both a Phase 2 and a Phase 3 study in adult patients with Rett syndrome. ANAVEX®2-73 is an orally available drug candidate that restores cellular homeostasis by targeting sigma-1 and muscarinic receptors. Preclinical studies demonstrated its potential to halt and/or reverse the course of Alzheimer's disease. ANAVEX®2-73 also exhibited anticonvulsant, anti-amnesic, neuroprotective, and anti-depressant properties in animal models, indicating its potential to treat additional CNS disorders, including epilepsy. The Michael J. Fox Foundation for Parkinson's Research previously awarded Anavex a research grant, which fully funded a preclinical study to develop ANAVEX®2-73 for the treatment of Parkinson's disease. ANAVEX®3-71, which targets sigma-1 and M1 muscarinic receptors, is a promising clinical stage drug candidate demonstrating disease-modifying activity against the major hallmarks of Alzheimer's disease in transgenic (3xTg-AD) mice, including cognitive deficits, amyloid, and tau pathologies. In preclinical trials, ANAVEX®3-71 has shown beneficial effects on mitochondrial dysfunction and neuroinflammation. Further information is available at www.anavex.com. You can also connect with the company on Twitter, Facebook, Instagram and LinkedIn.
Anavex gains on long-term data for Parkinson’s disease therapy
Mar. 30, 2023 8:10 AM ET
Anavex Life Sciences Corp. (AVXL)
By: Dulan Lokuwithana, SA News Editor
Anavex Life Sciences (NASDAQ:AVXL) inched ~5% higher in the pre-market Thursday after announcing initial data from an open-label extension phase from its mid-stage trial for lead asset ANAVEX 2-73 in Parkinson's disease (PD) dementi
https://seekingalpha.com/news/3952659-anavex-stock-gains-on-parkinsons-disease-data
Anavex Life Sciences Corp. (AVXL)
Eplontersen
DAYBUE™ (trofinetide)
DAYBUE™ (trofinetide)
Ionis reports positive topline 66-week results of eplontersen Phase 3 study for patients with ATTRv-PN
March 27, 2023 at 2:00 AM EDT
- Eplontersen met co-primary endpoints demonstrating sustained reduction in TTR and benefits in neuropathy and quality of life through 66 weeks
- 35 and 66-week data to be presented at the American Academy of Neurology (AAN) Annual Meeting in April
CARLSBAD, Calif., March 27, 2023 /PRNewswire/ -- Ionis Pharmaceuticals, Inc. (Nasdaq: IONS) today announced positive topline results from the 66-week analysis of the Phase 3 NEURO-TTRansform study of Ionis and AstraZeneca's eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN), a debilitating and potentially fatal disease that leads to peripheral nerve damage and motor disability.
At 66 weeks, patients treated with eplontersen continued to demonstrate a statistically significant and clinically meaningful change from baseline versus an external placebo group on the co-primary endpoints of modified Neuropathy Impairment Score +7 (mNIS+7), a measure of neuropathic disease progression, and Norfolk Quality of Life Questionnaire-Diabetic Neuropathy (Norfolk QoL-DN). The study also met its third co-primary endpoint demonstrating a statistically significant reduction in serum TTR concentration versus an external placebo group. TTR reductions were consistent with those reported at week 35. Eplontersen continued to demonstrate a safety and tolerability profile consistent with that observed at 35 weeks.
"The positive results from the 66-week analysis of the Phase 3 NEURO-TTRansform trial show that eplontersen provided consistent and sustained transthyretin protein reduction and that a substantial number of patients improved in measures of both neuropathy progression and quality of life," said Sami Khella, M.D., chief, department of neurology, Penn Presbyterian Medical Center and professor of clinical neurology, University of Pennsylvania School of Medicine. "This builds on the favorable 35-week results, which first demonstrated eplontersen's potential to significantly improve outcomes in this underserved population."
"These latest results from our NEURO-TTRansform study represent an important step towards delivering a potential new therapy for ATTRv-PN patients living with this debilitating and fatal disease. We are encouraged by the sustained benefit demonstrated by eplontersen and what a self-administered treatment could mean for patients and families affected by ATTRv-PN," said Eugene Schneider, M.D., executive vice president and chief clinical development officer for Ionis. "Together with our partner AstraZeneca, we look forward to sharing detailed results from this study at the upcoming American Academy of Neurology Annual Meeting."
"These results further underscore eplontersen's potential to be a best-in-class treatment across all forms of transthyretin-mediated amyloidosis, including polyneuropathy and cardiomyopathy which can lead to heart failure," said Mene Pangalos, executive vice president, BioPharmaceuticals R&D, AstraZeneca. "With limited treatment options currently available, there is an urgent unmet medical need for new therapies and earlier, accurate diagnosis across the different types of this systemic, progressive and fatal condition."
Data from both the 35 and 66-week analyses will be presented as an Emerging Science presentation at the American Academy of Neurology (AAN) Annual Meeting in April. The initial results from the 35-week analysis were presented at the International Symposium on Amyloidosis meeting in September 2022.
As part of a global development and commercialization agreement, Ionis and AstraZeneca are seeking regulatory approval for eplontersen for the treatment of ATTRv-PN in the U.S. and plan to seek regulatory approval in Europe and other parts of the world. Earlier this month, the U.S. Food and Drug Administration accepted a New Drug Application for eplontersen for the treatment of ATTRv-PN with a PDUFA action date of Dec. 22, 2023. Eplontersen was granted Orphan Drug Designation in the U.S.
Eplontersen is currently being evaluated in the Phase 3 CARDIO-TTRansform study for transthyretin amyloid cardiomyopathy (ATTR-CM), a systemic, progressive and fatal condition that typically leads to progressive heart failure and often death within three to five years from disease onset.
About the NEURO-TTRansform Study
NEURO-TTRansform is a global, open-label, randomized trial evaluating the efficacy and safety of eplontersen in patients with ATTRv-PN. The trial enrolled adult patients with ATTRv-PN Stage 1 or Stage 2 and up to week 66 eplontersen is being compared to the external placebo group from the NEURO-TTR registrational trial for inotersen that Ionis completed in 2017. The final analysis comparing eplontersen to external placebo was completed at week 66 and all patients will be followed on treatment until week 85, when they will have the option to transition into an open-label extension study. For more information on the NEURO-TTRansform study, please visit: https://clinicaltrials.gov/ct2/show/NCT04136184
About Hereditary Transthyretin-Mediated Amyloid Polyneuropathy (ATTRv-PN)
Hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN) is caused by the accumulation of misfolded mutated TTR protein in the peripheral nerves. Patients with ATTRv-PN experience ongoing debilitating nerve damage throughout their body resulting in the progressive loss of motor functions, such as walking. These patients also accumulate TTR in other major organs, which progressively compromises their function. The damage from misfolded TTR protein accumulation leads to disability within five years of diagnosis and is generally fatal within a decade.
About Eplontersen
Eplontersen is an investigational LIgand-Conjugated Antisense (LICA) medicine designed to inhibit the production of TTR protein. Eplontersen is being developed as a monthly self-administered subcutaneous injection to treat all types of ATTR. ATTR amyloidosis is a systemic, progressive and fatal disease in which patients experience multiple overlapping clinical manifestations caused by the inappropriate formation and aggregation of TTR amyloid deposits in various tissues and organs, including peripheral nerves, heart, intestinal tract, eyes, kidneys, central nervous system, thyroid and bone marrow. The progressive accumulation of TTR amyloid deposits in these tissues and organs leads to organ failure and eventually death.
About Ionis Pharmaceuticals, Inc.
For more than 30 years, Ionis has been a leader in RNA-targeted therapy, pioneering new markets and changing standards of care with its novel antisense technology. Ionis currently has three marketed medicines and a promising late-stage pipeline highlighted by cardiovascular and neurological franchises. Our scientific innovation began and continues with the knowledge that sick people depend on us, which fuels our vision to become the leader in genetic medicine, utilizing a multi-platform approach to discover, develop and deliver life-transforming therapies.
To learn more about Ionis visit www.ionispharma.com and follow us on Twitter @ionispharma.
View original content to download multimedia:https://www.prnewswire.com/news-releases/ionis-reports-positive-topline-66-week-results-of-eplontersen-phase-3-study-for-patients-with-attrv-pn-301781634.html
SOURCE Ionis Pharmaceuticals, Inc.
Ionis, AstraZeneca report positive outcomes from eplontersen trial
Mar. 27, 2023 7:34 AM ET
By: Preeti Singh, SA News Editor1 Comment
Ionis Pharmaceuticals (NASDAQ:IONS) on Monday reported positive topline results from the 66-week analysis of the Phase 3 NEURO-TTRansform study of eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN).
Eplontersen is an investigational medicine designed to reduce the production of transthyretin protein to treat both hereditary and non-hereditary forms of ATTR amyloidosis. Ionis (IONS) is partnered with AstraZeneca (NASDAQ:AZN) on the candidate.
DAYBUE™ (trofinetide)
DAYBUE™ (trofinetide)
DAYBUE™ (trofinetide)
March 10, 2023
General
Acadia Pharmaceuticals Announces U.S. FDA Approval of DAYBUE™ (trofinetide) for the Treatment of Rett Syndrome in Adult and Pediatric Patients Two Years of Age and Older
— First and only approved therapy for Rett syndrome, a rare, neurodevelopmental disorder, which affects 6,000 to 9,000 patients in the U.S.1
— Company expects DAYBUE to be available by the end of April, 2023
— Rare Pediatric Disease Priority Review Voucher granted in connection with approval
— Conference call and webcast to be held March 13, 2023 at 8:30 a.m. Eastern Time
SAN DIEGO–(BUSINESS WIRE)–Mar. 10, 2023– Acadia Pharmaceuticals Inc. (Nasdaq: ACAD) today announced that the U.S. Food and Drug Administration (FDA) has approved DAYBUE™ (trofinetide) for the treatment of Rett syndrome in adult and pediatric patients two years of age and older. DAYBUE is the first and only drug approved for the treatment of Rett syndrome.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20230303005382/en/
(Graphic: Business Wire)
“Today marks an important milestone for the Rett community and Acadia. As the first FDA-approved drug for the treatment of Rett syndrome, DAYBUE now offers the potential to make meaningful differences in the lives of patients and their families who have lacked options to treat the diverse and debilitating array of symptoms caused by Rett syndrome,” said Steve Davis, Acadia’s Chief Executive Officer. “We are grateful to all of the Rett syndrome patients, caregivers, clinical investigators and our employees who have contributed to making today a reality and look forward to getting DAYBUE to patients as quickly as possible.”
“Rett syndrome is a profoundly debilitating and complex, rare, neurodevelopmental disorder that presents differently across patients and can lead to an array of unpredictable symptoms throughout the course of a patient’s life,” said Jeffrey L. Neul, M.D., Ph.D., Annette Schaffer Eskind Chair and Director, Vanderbilt Kennedy Center, Professor of Pediatrics, Division of Neurology, Pharmacology, and Special Education, Vanderbilt University Medical Center and Phase 3 LAVENDER™ study investigator. “Now, for the first time after decades of clinical research, healthcare providers finally have a treatment option to address a range of core behavioral, communication and physical symptoms for their patients living with Rett syndrome.”
Rett syndrome is a complex, rare, neurodevelopmental disorder typically caused by a genetic mutation on the MECP2 gene.2,3 It is characterized by a period of normal development until six to 18 months of age, followed by significant developmental regression with loss of acquired communication skills and purposeful hand use.4 Symptoms of Rett syndrome may also include development of hand stereotypies, such as hand wringing and clapping, and gait abnormalities.5 Rett syndrome is believed to affect 6,000 to 9,000 patients in the U.S., with a diagnosed population of approximately 4,500 U.S. patients.1,6
The FDA approval of DAYBUE was supported by results from the pivotal Phase 3 LAVENDER study evaluating the efficacy and safety of trofinetide versus placebo in 187 female patients with Rett syndrome five to 20 years of age. In the study, treatment with DAYBUE demonstrated statistically significant improvement compared to placebo on both co-primary efficacy endpoints, as measured by the change from baseline in Rett Syndrome Behaviour Questionnaire (RSBQ) total score (p=0.018) and the Clinical Global Impression-Improvement (CGI-I) scale score (p=0.003) at week 12. The RSBQ is a caregiver assessment that evaluates a range of symptoms of Rett syndrome including vocalizations, facial expressions, eye gaze, hand movements (or stereotypies), repetitive behaviors, breathing, night-time behaviors and mood. The CGI-I is a global physician assessment of whether a patient has improved or worsened. In the study, the most common side effects were diarrhea (82%) and vomiting (29%).
“This is a historic day for the Rett syndrome community and a meaningful moment for the patients and caregivers who have eagerly awaited the arrival of an approved treatment for this condition,” said Melissa Kennedy, Chief Executive Officer of the International Rett Syndrome Foundation. “Rett syndrome is a complicated, devastating disease that affects not only the individual patient, but whole families. With today’s FDA decision, those impacted by Rett have a promising new treatment option that has demonstrated benefit across a variety of Rett symptoms, including those that impact the daily lives of those living with Rett and their loved ones.”
DAYBUE is expected to be available in the U.S. by the end of April, 2023.
In 2018, Acadia entered into an exclusive license agreement with Neuren Pharmaceuticals Limited (ASX: NEU) for the development and commercialization of trofinetide for the treatment of Rett syndrome and other indications in North America.
With the FDA approval of DAYBUE, Acadia has received a Rare Pediatric Disease Priority Review Voucher, which can be used to obtain priority review for a subsequent application.
Acadia Connect® Offers Dedicated Patient and Family Support and Resources
Acadia Connect® is a multi-faceted support program that will offer personal assistance, financial resources and prescription support to patients and caregivers starting and continuing appropriate DAYBUE therapy. Each dedicated support team includes a nurse care coordinator, a family access manager and 24/7 clinical pharmacist support. For more information, visit AcadiaConnect.com or call 1-844-737-2223, Monday to Friday, 8 a.m. to 8 p.m. Eastern Time.
Please read the accompanying full Prescribing Information, also available at DAYBUE.com
About Rett Syndrome
Rett syndrome is a rare, complex, neurodevelopmental disorder that may occur over four stages and affects approximately 6,000 to 9,000 patients in the U.S., with approximately 4,500 patients currently diagnosed according to an analysis of healthcare claims data.1,2,4,6 A child with Rett syndrome exhibits an early period of apparently normal development until six to 18 months, when their skills seem to slow down or stagnate. This is typically followed by a duration of regression when the child loses acquired communication skills and purposeful hand use. The child may then experience a plateau period in which they show mild recovery in cognitive interests, but body movements remain severely diminished. As they age, those living with Rett may continue to experience a stage of motor deterioration which can last the rest of the patient’s life.4 Rett syndrome is typically caused by a genetic mutation on the MECP2 gene.3 In preclinical studies, deficiency in MeCP2 function has been shown to lead to impairment in synaptic communication, and the deficits in synaptic function may be associated with Rett manifestations.3,7,8
Symptoms of Rett syndrome may also include development of hand stereotypies, such as hand wringing and clapping, and gait abnormalities.5 Most Rett patients typically live into adulthood and require round-the-clock care.2,9
About DAYBUE ™ (trofinetide)
Trofinetide is a synthetic version of a naturally occurring molecule known as the tripeptide glycine-proline-glutamate (GPE). The mechanism by which trofinetide exerts therapeutic effects in patients with Rett syndrome is unknown. In animal studies, trofinetide has been shown to increase branching of dendrites and synaptic plasticity signals.10,11
About Acadia Pharmaceuticals
Acadia is advancing breakthroughs in neuroscience to elevate life. For almost 30 years we have been working at the forefront of healthcare to bring vital solutions to people who need them most. We developed and commercialized the first and only approved therapies for hallucinations and delusions associated with Parkinson’s disease psychosis and for the treatment of Rett syndrome. Our clinical-stage development efforts are focused on treating the negative symptoms of schizophrenia, Alzheimer’s disease psychosis and neuropsychiatric symptoms in central nervous system disorders. For more information, visit us at www.acadia.com and follow us on LinkedIn and Twitter.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230303005382/en/
Acadia wins FDA nod for Rett syndrome therapy
Mar. 10, 2023 10:20 PM ET
ACADIA Pharmaceuticals Inc. (ACAD), NURPF
By: Dulan Lokuwithana, SA News Editor
Acadia Pharmaceuticals (NASDAQ:ACAD) announced late Friday that the FDA greenlighted trofinetide under the brand name Daybue to treat the rare genetic neurodevelopmental disorder Rett syndrome in those aged two years and older.
https://seekingalpha.com/news/3946547-acadia-wins-fda-nod-for-rett-syndrome-therapy
Eplontersen
DAYBUE™ (trofinetide)
Eplontersen
Ionis announces FDA acceptance of New Drug Application for eplontersen for the treatment of hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN)
March 7, 2023 at 7:05 AM EST
- 35-week data included in the filing demonstrated a statistically significant and clinically meaningful change from baseline for co-primary and secondary endpoints compared to external placebo group
- Eplontersen previously granted Orphan Drug Designation for transthyretin-mediated amyloidosis
- FDA assigns PDUFA action date of Dec. 22, 2023
CARLSBAD, Calif., March 7, 2023 /PRNewswire/ -- Ionis Pharmaceuticals (Nasdaq: IONS) today announced that the U.S. Food and Drug Administration (FDA) has accepted for review a New Drug Application (NDA) for eplontersen, an investigational antisense medicine for the treatment of people living with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN). The application has been given a Prescription Drug User Fee Act (PDUFA) action date of Dec. 22, 2023.
In its acceptance letter, the FDA stated that it has not identified any review issues and did not make any additional data requests. The FDA also noted that it is not planning to hold an advisory committee meeting to discuss the application.
Patients with ATTRv-PN experience ongoing debilitating nerve damage throughout their body resulting in the progressive loss of motor function. These patients accumulate TTR in other major organs, which progressively compromises their function and eventually leads to death within five to fifteen years of disease onset.
"We are excited by today's FDA acceptance of our NDA filing as it brings Ionis and our partner, AstraZeneca, one step closer to making eplontersen available to patients with ATTR polyneuropathy," said Eugene Schneider, M.D., executive vice president and chief clinical development officer at Ionis. "Significant reductions in TTR protein levels were observed during the NEURO-TTRansform 35-week interim analysis. Overall, the interim analysis demonstrated eplontersen has the potential to make a positive impact on disease progression and improve quality of life in a substantial number of patients."
The NDA is based on results from the global Phase 3 NEURO-TTRansform study presented at the International Symposium on Amyloidosis (ISA). In the 35-week interim analysis, eplontersen demonstrated a statistically significant and clinically meaningful change from baseline for its co-primary and key secondary endpoints compared to the external placebo group. In the study, eplontersen achieved a significant mean reduction (p<0.0001) in the co-primary endpoint of serum transthyretin (TTR) concentration compared to baseline. Eplontersen also demonstrated a significant treatment effect on the co-primary endpoint of modified Neuropathy Impairment Score +7 (mNIS+7), a measure of neuropathic disease progression, with a statistically significant difference in mean change from baseline versus the external placebo group (p<0.0001). The study met its key secondary endpoint of change from baseline in the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy (Norfolk QoL-DN), showing that treatment with eplontersen significantly improved patient-reported quality of life compared to the external placebo group (p<0.0001). Eplontersen also demonstrated a favorable safety and tolerability profile.
Eplontersen is an investigational medicine designed to reduce the production of transthyretin (TTR) protein to treat both hereditary and non-hereditary forms of ATTR amyloidosis (ATTR). In December 2021, Ionis and AstraZeneca entered into a strategic collaboration to develop and commercialize eplontersen. Eplontersen is being jointly developed and commercialized by both companies in the U.S. and will be developed and commercialized in the rest of the world by AstraZeneca, with the exception of Latin America. In January 2022, eplontersen was granted Orphan Drug Designation in the U.S. by the FDA.
In addition to the NEURO-TTRansform study, eplontersen is also currently being evaluated in the global Phase 3 CARDIO-TTRansform study for transthyretin amyloid cardiomyopathy (ATTR-CM), a systemic, progressive and fatal condition that leads to progressive heart failure and death within three to five years from disease onset.
About Eplontersen
Eplontersen is an investigational LIgand-Conjugated Antisense (LICA) medicine designed to inhibit the production of TTR protein. Eplontersen is being developed as a monthly self-administered subcutaneous injection to treat all types of ATTR. ATTR amyloidosis is a systemic, progressive and fatal disease in which patients experience multiple overlapping clinical manifestations caused by the inappropriate formation and aggregation of TTR amyloid deposits in various tissues and organs, including peripheral nerves, heart, intestinal tract, eyes, kidneys, central nervous system, thyroid and bone marrow. The progressive accumulation of TTR amyloid deposits in these tissues and organs leads to organ failure and eventually death.
About Ionis Pharmaceuticals, Inc.
For more than 30 years, Ionis has been a leader in RNA-targeted therapy, pioneering new markets and changing standards of care with its novel antisense technology. Ionis currently has three marketed medicines and a promising late-stage pipeline highlighted by cardiovascular and neurological franchises. Our scientific innovation began and continues with the knowledge that sick people depend on us, which fuels our vision to become the leader in genetic medicine, utilizing a multi-platform approach to discover, develop and deliver life-transforming therapies.
To learn more about Ionis visit www.ionispharma.com and follow us on Twitter @ionispharma.
View original content to download multimedia:https://www.prnewswire.com/news-releases/ionis-announces-fda-acceptance-of-new-drug-application-for-eplontersen-for-the-treatment-of-hereditary-transthyretin-mediated-amyloid-polyneuropathy-attrv-pn-301764027.html
SOURCE Ionis Pharmaceuticals, Inc.
Ionis, AstraZeneca eplontersen application accepted by FDA for nerve damage disorder
Mar. 07, 2023 12:59 PM ET
By: Jonathan Block, SA News Editor2 Comments
- The US FDA has accepted a New Drug Application submitted by Ionis Pharmaceuticals (NASDAQ:IONS) for eplontersen for hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN).
- The FDA action date is Dec. 22.
- The agency said it does not plan on holding an advisory committee meeting for the application.
- Ionis (IONS) is partnered with AstraZeneca (NASDAQ:AZN) on the candidate.
- https://seekingalpha.com/news/3944994-ionis-astrazeneca-eplontersen-application-accepted-by-fda-for-nerve-damage-disorder
- AstraZeneca PLC (AZN), IONS
- https://www.astrazeneca.com/
- https://www.ionispharma.com/ionis-antisense-technology/antisense-pipeline/
Sotatercept
OPSUMIT® (macitentan) & Tadalafil combo
Eplontersen
Merck’s Investigational Activin Signaling Inhibitor Sotatercept Improved Six-Minute Walk Distance by 40.8 Meters at Week 24 Versus Placebo in Adults with Pulmonary Arterial Hypertension on Background Therapy
March 6, 2023 12:01 pm ET
Sotatercept demonstrated statistically significant improvements in 8 of 9 secondary measures, including reduction in risk of clinical worsening or death
Results presented today at ACC.23/WCC and published in The New England Journal of Medicine
RAHWAY, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced full results from the Phase 3 STELLAR trial, which evaluated sotatercept, Merck’s novel investigational activin signaling inhibitor biologic, in combination with stable background therapy for the treatment of adult patients with pulmonary arterial hypertension (PAH) (WHO Group 1). Sotatercept significantly improved exercise capacity, increasing 6-minute walk distance (6MWD) by 40.8 meters (95% CI, 27.5-54.1; p<0.001) from baseline at week 24, the study’s primary endpoint.
In addition, sotatercept demonstrated statistically significant and clinically meaningful improvements in eight of nine secondary outcome measures, including improvements in WHO functional class (WHO FC) and pulmonary vascular resistance (PVR). Sotatercept reduced the risk of clinical worsening or death by 84% compared to placebo with a median follow-up of 32.7 weeks (HR=0.16 [95% CI, 0.08-0.35]; p<0.001). The safety profile of sotatercept was generally consistent with that observed in previous studies with sotatercept. These data were presented today at the American College of Cardiology’s 72nd Annual Scientific Session together with World Heart Federation’s World Congress of Cardiology and simultaneously published in The New England Journal of Medicine.
“PAH is a rare, rapidly progressive, debilitating and ultimately life-threatening condition with a five-year mortality rate of 43 percent,” said Dr. Marius Hoeper, Hannover Medical School, Germany, and lead investigator. “Sotatercept demonstrated profound improvements across the primary endpoint of six-minute walk distance and multiple secondary endpoints, including improvements in WHO functional class and pulmonary vascular resistance. These landmark results show the potential of sotatercept and the approach of targeting cellular signaling associated with vascular hyperproliferation and pathological remodeling for the treatment of PAH.”
“The results from the Phase 3 STELLAR trial are immensely important to physicians and patients and highlight the critical role sotatercept may play in improving exercise capacity and other meaningful clinical outcome measures for patients with PAH,” said Dr. Dean Y. Li, president, Merck Research Laboratories. “These findings are compelling given the profound reduction in the risk of clinical worsening or death in patients treated with sotatercept on top of background therapy. We look forward to discussing these pivotal data with health authorities and are working with urgency to bring this potential new treatment option to patients.”
STELLAR is the first Phase 3 study to evaluate the efficacy of an activin signaling inhibitor added to background therapy in adults with PAH. Key findings from secondary endpoints included:
- The proportion of patients who achieved multicomponent improvement at week 24 (defined as improvement in 6MWD, improvement in N-terminal pro-B-type natriuretic peptide (NT-proBNP) level, and either improvement in WHO FC or maintenance of WHO FC II) was significantly greater with sotatercept versus placebo (38.9% [n=63/163] versus 10.1% [n=16/160]; p<0.001).
- Sotatercept demonstrated a statistically significant reduction of -234.6 dyn·sec·cm−5 (95% CI, -288.4 to -180.8; p<0.001) from baseline at week 24 in PVR – a calculation of pulmonary artery pressure, pulmonary artery wedge pressure and cardiac output – versus placebo.
- Sotatercept demonstrated a statistically significant reduction of -441.6 (95% CI, -573.5 to -309.6; p<0.001) from baseline at week 24 in NT-proBNP levels versus placebo.
- Patients receiving sotatercept were significantly more likely to improve and maintain WHO FC at week 24 versus placebo. 29.4% (n=48/163) of patients in the sotatercept group improved in WHO FC compared to 13.8% (n=22/160) in the placebo group (p<0.001).
- Sotatercept significantly reduced events associated with clinical worsening (defined by death of any cause or specified non-fatal clinical worsening events). With a median follow-up of 32.7 weeks, 9 of 163 patients in the sotatercept group died or experienced a clinical worsening event versus 42 of 160 patients in the placebo group (HR=0.16 [95% CI, 0.08 to 0.35]; p<0.001).
- A significantly greater proportion of patients treated with sotatercept achieved or maintained a low French risk score (attaining or maintaining all three low-risk criteria: WHO functional class I or II, 6-minute walk distance > 440 meters, and NT-proBNP level < 300 pg per milliliter) versus placebo (39.5% [n=64/163] versus 18.2% [n=29/160]; p<0.001).
- In patient-reported outcomes using the PAH-SYMPACT® questionnaire, the average scores for Physical Impacts (change from baseline: -0.26 [95% CI, -0.49 to -0.04]; p=0.010) and Cardiopulmonary Symptoms (change from baseline: -0.13 [95% CI, -0.26 to -0.01]; p=0.028) were significantly reduced in patients treated with sotatercept versus placebo. PAH-SYMPACT® is a disease-specific patient-reported outcome instrument. Domain scores range from 0 to 4 with higher scores indicating greater severity of symptoms.
- The average score for Cognitive/Emotional Impacts using PAH-SYMPACT® was not significantly different between patients treated with sotatercept versus placebo (p=0.156).
Treatment-emergent adverse events (TEAEs) occurred in 90.8% of patients who received sotatercept versus 91.9% of patients who received placebo, while severe TEAEs were observed in 12.9% versus 18.1% of patients, respectively. Adverse events that occurred more frequently with sotatercept versus placebo were bleeding events, telangiectasia, increased hemoglobin levels, thrombocytopenia, increased blood pressure, and dizziness.
Study design and additional data from the STELLAR trial
STELLAR (NCT04576988) was a pivotal Phase 3, randomized, double-blind, placebo-controlled, multicenter, parallel-group study to evaluate the safety and efficacy of sotatercept in adult patients with PAH (WHO Group 1) being treated with background therapy with WHO Functional Class (FC) II or III. The primary endpoint of the study was exercise capacity, as measured by change from baseline in week 24 6MWD. Nine secondary endpoints, tested hierarchically in the following order, were multicomponent improvement, change in PVR, NT-proBNP level, improvement in WHO FC, time to clinical worsening or death, French risk score, and the PAH-SYMPACT® Physical Impacts, Cardiopulmonary Symptoms and Cognitive/Emotional Impacts domain scores; all assessed at week 24 except clinical worsening, which was assessed when the last patient completed the week 24 visit.
The study enrolled a total of 323 participants who were randomized to receive either sotatercept (n=163) once every 3 weeks at a dose of 0.3 mg/kg at visit 1 and a dose of 0.7 mg/kg thereafter or placebo (n=160) added to stable background PAH therapy. The study population characteristics were: mean [±SD] 47.9 ± 14.8 years of age; 89% white; 79% female; and average length of time since PAH diagnosis of 8.8 years. In total,198 of the randomized patients (61.3%) were receiving triple therapy and 129 patients (39.9%) were receiving prostacyclin infusion therapy. Demographic and baseline characteristics were similar between the sotatercept and placebo groups.
The safety profile of sotatercept was generally consistent with that observed in the Phase 2 PULSAR trial. Seven patients (4.4%) in the placebo group and two patients (1.2%) in the sotatercept group died during the study through the data cutoff date.
About pulmonary arterial hypertension (PAH)
Pulmonary arterial hypertension (PAH) is a rare, progressive and life-threatening blood vessel disorder characterized by the constriction of small pulmonary arteries and elevated blood pressure in the pulmonary circulation. Approximately 40,000 people in the U.S. are living with PAH. The disease progresses rapidly for many patients. PAH results in significant strain on the heart, leading to limited physical activity, heart failure and reduced life expectancy. The five-year mortality rate for patients with PAH is approximately 43%.
About sotatercept
Sotatercept is an investigational, potential first-in-class activin signaling inhibitor biologic being studied for the treatment of PAH (WHO Group 1). PAH is a rare disease caused, in part, by hyperproliferation of cells in the arterial walls in the lung, leading to narrowing and abnormal constriction. In pre-clinical models, sotatercept has been shown to modulate vascular cell proliferation, reversing vascular and right ventricle remodeling.
Sotatercept has been granted Breakthrough Therapy Designation and Orphan Drug designation by the U.S. Food and Drug Administration (FDA), as well as Priority Medicines designation and Orphan Drug designation by the European Medicines Agency for the treatment of PAH. Merck acquired exclusive rights to sotatercept in the pulmonary hypertension field through the acquisition of Acceleron Pharma Inc. Sotatercept is the subject of a licensing agreement with Bristol Myers Squibb.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on Twitter, Facebook, Instagram, YouTube and LinkedIn.
Source: Merck & Co., Inc.
Merck posts full Phase 3 data for sotatercept in pulmonary arterial hypertension
Mar. 07, 2023 5:30 AM ET
By: Dulan Lokuwithana, SA News Editor
Merck (NYSE:MRK) closed ~4% higher Monday, marking the biggest one-day gain since June 2022 after disclosing complete Phase 3 results for biologic sotatercept, which is targeted at blood vessel disorder pulmonary arterial hypertension (PAH).
MK-0616
OPSUMIT® (macitentan) & Tadalafil combo
OPSUMIT® (macitentan) & Tadalafil combo
Merck’s MK-0616, an Investigational Oral PCSK9 Inhibitor, Significantly Reduced LDL-C in Patients with Hypercholesterolemia in Phase 2b Study
March 6, 2023 12:00 pm ET
MK-0616 was generally well tolerated and reduced LDL-C across all dose levels compared to placebo
Merck plans to start Phase 3 pivotal study in the second half of 2023
RAHWAY, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced results from the Phase 2b clinical trial evaluating MK-0616, an investigational, once-daily oral proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor in adults with hypercholesterolemia. The primary objective of the study was to evaluate the percent change in low density lipoprotein cholesterol (LDL-C) from baseline to week 8 for 4 doses of MK-0616 (6, 12, 18 and 30 mg) versus placebo. At week 8, all doses of MK-0616 significantly reduced LDL-C compared to placebo and the placebo-adjusted reduction from baseline ranged from 41.2% (6 mg, CI 95%, -47.8 to -34.7; p <0.001) to 60.9% (30 mg, 95% CI, -67.6 to -54.3; p<0.001). MK-0616 was generally well-tolerated at all 4 doses studied. These data were presented today at the American College of Cardiology’s 72nd Annual Scientific Session together with World Congress of Cardiology (ACC.23/WCC) and simultaneously published in the Journal of The American College of Cardiology.
Inhibition of PCSK9 increases the removal of LDL-C from the bloodstream. MK-0616 is a macrocyclic peptide and is designed to lower LDL-C via the same biological mechanism as currently approved injectable PCSK9 inhibitors, but in a daily pill form. High LDL-C, if left untreated, can lead to a high risk of atherosclerotic cardiovascular disease (ASCVD) events, such as heart attacks and strokes.
“Despite widely available statin treatments, millions of patients are still not able to lower their cholesterol to the guideline-recommended levels and as a result are at increased risk for serious cardiovascular complications associated with atherosclerosis,” said Dr. Christie M. Ballantyne, principal investigator of the study and Professor of Medicine at Baylor College of Medicine. “Currently available PCSK9 inhibitors are effective tools to treat hypercholesterolemia but must be administered by injection. With these promising data showing that MK-0616 reduced LDL-C levels by up to 60.9%, MK-0616 should be further studied for its potential as a daily oral medicine.”
“These data reinforce our confidence that MK-0616 could become the first oral PCSK9 inhibitor, with the potential to change the way patients with hypercholesterolemia who need additional LDL-C reduction are treated. This may allow many more patients to reach their LDL-C treatment goals,” said Dr. Joerg Koglin, vice president, global clinical development, Merck Research Laboratories. “We look forward to advancing this program into Phase 3 development in the second half of this year.”
Additional data from the Phase 2b Study for MK-0616 (MK-0616-008)
MK-0616-008(NCT05261126) was a randomized, double-blind, placebo-controlled, multi-center Phase 2b trial designed to evaluate the efficacy and safety of MK-0616 administered daily compared to placebo in adult participants with hypercholesterolemia and a broad spectrum of ASCVD risk. Participants were receiving a range of lipid-lowering therapies from no statin to high-intensity statin. The primary efficacy endpoint was the percent change in LDL-C from baseline to week 8. Supportive secondary endpoints (not multiplicity controlled) were percent change in apolipoprotein B-100 (ApoB) and in non-high-density lipoprotein-C (non-HDL-C) from baseline to week 8, and the proportion of participants who achieved protocol-defined LDL-C goals at week 8.
In total, 381 participants from age 18-80 with hypercholesterolemia with a moderate to high risk of atherosclerotic cardiovascular disease were randomized 1:1:1:1:1 to receive MK-0616 at a dose of 6 mg (n=77), 12 mg (n=76), 18 mg (n=76), or 30 mg (n=76) or placebo (n=76) once daily. The study population consisted of 49% female, 66% White, 17% Asian and 6% Black/African American, and 40% Latino or Hispanic.
At week 8, all doses of MK-0616 significantly reduced LDL-C compared to placebo and the results were generally consistent across the prespecified subgroups. The LDL-C placebo-adjusted reduction from baseline were as follows for each of the four doses studied (p<0.001 for all doses): 6 mg, 41.2% (95% CI, -47.8, -34.7), 12 mg, 55.7% (95% CI, -62.3, -49.1), 18 mg, 59.1% (95% CI, -65.7, -52.5), and 30 mg, 60.9% (95% CI, -67.6, -54.3). Near-complete efficacy was achieved by week 2, with the effect persisting over the eight-week treatment period. At week 8, improvements in secondary endpoints were also observed for all MK-0616 dose arms: ApoB levels were reduced by 32.8% (6 mg) to 51.8% (30 mg), non-HDL-C levels were reduced by 35.9% (6 mg) to 55.8% (30 mg), and protocol-defined LDL-C goals were achieved by 80.5% (6 mg) to 90.8% of participants (30 mg) versus 9.3% on placebo.
MK-0616 was generally well-tolerated with no overall trends across treatment groups in discontinuation rates or adverse events at week 16. No serious adverse events that were considered by the investigator to be related to treatment with MK-0616 were reported.
About PCSK9 and MK-0616
PCSK9 plays a key role in cholesterol homeostasis by regulating levels of LDL receptors, which are responsible for the uptake of cholesterol into cells. Inhibition of PCSK9 prevents the interaction of PCSK9 with LDL receptors. This results in greater numbers of LDL receptors available on the cell surface to remove LDL cholesterol from the blood.
Discovered and developed by Merck, MK-0616 is an investigational, potentially first oral PCSK9 inhibitor designed to lower low density lipoprotein (LDL) cholesterol. MK-0616 is a macrocyclic peptide that binds to PCSK9 and inhibits the interaction of PCSK9 with LDL receptors.
About Hypercholesterolemia
Hypercholesterolemia, a disorder in which there are elevated LDL-C levels in the blood, affects approximately 73 million adults in the U.S. It is a major risk factor associated with ASCVD, which is the leading cause of death in the U.S. and globally. Despite adjusting diet and taking statin therapies, many patients with hypercholesterolemia are still not reaching their LDL-C lowering goals as recommended by guidelines.
Merck’s Focus on Cardiovascular and Pulmonary Disease
Merck has a long history of developing treatments for cardiovascular disease. More than 60 years ago, we introduced our first cardiovascular therapy – and our scientific efforts to understand and treat cardiovascular-related disorders have continued. Cardiovascular disease continues to be one of the most serious health challenges of the 21st century. Approximately 18 million people across the globe die every year, and in the United States, one person dies every 36 seconds from cardiovascular disease.
Advancements in the treatment of cardiovascular disease can make a critical difference for patients around the world. At Merck, we strive for scientific excellence and innovation in all stages of research, from discovery through approval and life cycle management. We work with experts throughout the cardiovascular and pulmonary community to advance research that can help improve the lives of patients globally.
Information for other currently enrolling cardiovascular studies can be found by visiting: https://www.merckclinicaltrials.com/cardiovascular.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on Twitter, Facebook, Instagram, YouTube and LinkedIn.
Source: Merck & Co., Inc.
Merck to start phase 3 of oral PCSK9 inhibitor for cholesterol following mid-stage results
Mar. 06, 2023 1:45 PM ET
Merck & Co., Inc. (MRK)AMGN, NVS, REGN
By: Jonathan Block, SA News Editor
- Phase 2b data for Merck's (NYSE:MRK) oral PCSK9 inhibitor MK-0616 has prompted the drugmaker to begin a phase 3 program in the second half of the year.
- https://seekingalpha.com/news/3944574-merck-to-start-phase-3-of-oral-pcsk9-inhibitor-for-cholesterol-following-mid-stage-results
- Merck & Co., Inc. (MRK)
OPSUMIT® (macitentan) & Tadalafil combo
OPSUMIT® (macitentan) & Tadalafil combo
OPSUMIT® (macitentan) & Tadalafil combo
Late-Breaking Phase 3 A DUE Data Show Investigational Single Tablet Combination Therapy of Macitentan and Tadalafil Significantly Improves Pulmonary Hemodynamics versus Monotherapy in Patients with Pulmonary Arterial Hypertension (PAH)
Mar 06, 2023United States
Study findings presented during the American College of Cardiology’s 72nd Annual Scientific Session & Expo Together With World Heart Federation’s World Congress of Cardiology
European Society of Cardiology/European Respiratory Society (ESC/ERS) PH guidelines recommend initial dual combination therapy with macitentan and tadalafil for PAH patients without cardiopulmonary comorbidities
RARITAN, NJ, March 6, 2023 – The Janssen Pharmaceutical Companies of Johnson & Johnson today announced results from the Phase 3 A DUE study (NCT03904693), which showed an investigational once-daily, single tablet combination therapy, also known as fixed dose combination, of macitentan 10 mg and tadalafil 40 mg (M/T STCT), significantly improved pulmonary hemodynamics (blood flow through pulmonary blood vessels) versus macitentan and tadalafil monotherapies in pulmonary arterial hypertension (PAH) patients with World Health Organization (WHO) functional class (FC) II or III.[1] The data were presented today as a Late-Breaking Clinical Trial presentation during the American College of Cardiology’s 72nd Annual Scientific Session & Expo Together With World Heart Federation’s World Congress of Cardiology.
PAH is a rare, progressive and life-threatening blood vessel disorder characterized by the constriction of small pulmonary arteries and elevated blood pressure in the pulmonary circulation that eventually leads to right heart failure.[2] Recently updated European Society of Cardiology/European Respiratory Society (ESC/ERS) PH guidelines[i] have recommended initial dual combination therapy with macitentan and tadalafil for PAH patients without cardiopulmonary comorbidities. Currently, this requires patients to take multiple pills as no single tablet that combines two or more PAH-specific pathways is available for these patients.[3]
“Targeting different pathways in the treatment of PAH has demonstrated clear clinical benefits, yet current treatment regimens are cumbersome and create a significant pill burden for patients, many of whom take a large number of pills each day to treat their PAH and various co-morbidities,[ii],[iii]” said Kelly Chin, M.D., Professor of Internal Medicine and Director of the Pulmonary Hypertension Program at UT Southwestern Medical Center, and an investigator in the A DUE study.[4] “The results from this study demonstrate that a single tablet combination has the potential to support initial dual combination therapy and rapid escalation from monotherapy, which may improve functional outcomes and help close the gap from guideline recommendations to clinical practice.”
The A DUE study is a double-blind, randomized, active-controlled, multi-center, adaptive parallel-group study designed to compare the efficacy and safety of investigational M/T STCT versus macitentan and tadalafil monotherapies in patients with PAH. A total of 187 adult PAH patients from across 148 sites in 19 countries worldwide in WHO FC II or III who were treatment naïve or on a stable dose of an endothelin receptor antagonist (ERA) or a phosphodiesterase type 5 inhibitor (PDE5i) for at least three months, were enrolled in the study. The primary endpoint is pulmonary vascular resistance (PVR) measured 16 weeks following initiation of treatment expressed as the ratio of geometric means to baseline.
Secondary efficacy outcome measures included change from baseline in exercise capacity as measured by change in 6-minute walk distance (6MWD) at the end of double-blind treatment at week 16 compared to baseline.
Following the double-blind treatment period, patients transitioned to the open-label treatment period for 24 months. Baseline characteristics were balanced across treatment arms except for a higher proportion of WHO FC II patients in the M/T STCT arm and a greater time from diagnosis of PAH in the macitentan arm.
“The guiding light of our PH research is the goal of transforming PAH into a manageable condition, so we’re constantly looking for ways to improve both clinical outcomes and the treatment experience,” said James List, M.D., Ph.D., Global Therapeutic Area Head, Cardiovascular, Metabolism, Retina & Pulmonary Hypertension, Janssen Research & Development, LLC. “A single tablet combination has the potential to be an important new option for helping physicians optimize disease management with the potential to enhance convenience and help improve adherence and outcomes.”
Key A DUE Study Findings
The A DUE study met its co-primary endpoint, demonstrating marked pulmonary hemodynamic improvement as shown by the highly statistically significant, consistent and robust PVR reduction in participants treated with M/T STCT compared to both monotherapies. PVR change with M/T STCT was significantly greater versus macitentan (treatment effect: 29%; 95% confidence limit [CL]: -18%, -39%, p<0.0001). PVR change with M/T STCT was also significantly greater versus tadalafil (treatment effect: 28%; 95% CL: -20%, -36%, p<0.0001).
Although the A DUE study was not powered to demonstrate a benefit on exercise capacity, there was a clinically relevant improvement in 6MWD.
- At week 16, treatment effect was not statistically significant; however, a clinically relevant improvement in 6MWD in favor of M/T STCT versus monotherapies was observed. Adjusted treatment effect in 6MWD, change from baseline, in the M/T STCT versus macitentan group was 16.04m (CL: -17.0, 49.08, p=0.380) and 25.37m in the M/T STCT versus tadalafil group (CL: -0.93, 51.59, p =0.059).
- The safety profile of M/T STCT was consistent with the known safety profiles of macitentan and tadalafil monotherapies and no new safety observations were made.
About macitentan/tadalafil STCT
Macitentan 10 mg and tadalafil 40 mg STCT is an investigational therapy that combines the ERA, macitentan, and the PDE5i, tadalafil.
About OPSUMIT® (macitentan)
OPSUMIT® is indicated for the treatment of PAH (WHO Group I) to reduce the risks of disease progression and hospitalization for PAH. The use of OPSUMIT® in patients with PAH (WHO Group I), a type of PH, was demonstrated in the pivotal SERAPHIN trial, the largest (n=742) long-term (average treatment duration=2 years) outcomes-based trial of an ERA in PAH.
About tadalafil
Tadalafil is indicated for the treatment of PAH (WHO Group 1) to improve exercise ability. Studies establishing effectiveness included predominately patients with NYHA Functional Class II – III symptoms and etiologies of idiopathic or heritable PAH (61%) or PAH associated with connective tissue diseases (23%).
OPSUMIT® INDICATION AND IMPORTANT SAFETY INFORMATION
INDICATION
OPSUMIT® (macitentan) is an endothelin receptor antagonist (ERA) indicated for the treatment of pulmonary arterial hypertension (PAH, WHO Group I) to reduce the risks of disease progression and hospitalization for PAH.
Effectiveness was established in a long-term study in PAH patients with predominantly WHO Functional Class II-III symptoms treated for an average of 2 years. Patients had idiopathic and heritable PAH (57%), PAH caused by connective tissue disorders (31%), and PAH caused by congenital heart disease with repaired shunts (8%).
Please see full Prescribing Information, including BOXED WARNING.
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we’re creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com. Follow us at @JanssenGlobal and @JanssenUS. Janssen Research & Development, LLC is part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
Janssen's macitentan, tadalafil combo improves pulmonary hemodynamics vs. monotherapies
Mar. 06, 2023 10:00 AM ET
By: Mamta Mayani, SA News Editor
- The Janssen Pharmaceutical Companies of Johnson & Johnson <<JNJ>> announces results from the Phase 3 A DUE study, which showed an investigational once-daily, single tablet combination therapy, also known as fixed dose combination, of macitentan 10 mg and tadalafil 40 mg (M/T STCT), significantly improved pulmonary hemodynamics (blood flow through pulmonary blood vessels) versus macitentan and tadalafil monotherapies in pulmonary arterial hypertension (PAH) patients with WHO functional class (FC) II or III.
- https://seekingalpha.com/news/3944464-janssens-macitentan-tadalafil-combo-improves-pulmonary-hemodynamics-vs-monotherapies
- JNJ
- https://www.janssen.com/
biotecHOPE™ 2023
IK-175
TRUSELTIQ (high-dose infigratinib)
LEQEMBI™ (lecanemab-irmb)
Ikena Oncology Receives FDA Fast Track Designation for Novel AHR Antagonist IK-175 in Combination with Immune Checkpoint Inhibitors to Treat Urothelial Carcinoma
Mar 06, 2023
BOSTON, March 06, 2023 (GLOBE NEWSWIRE) -- Ikena Oncology, Inc. (Nasdaq: IKNA, “Ikena”), a targeted oncology company forging new territory in patient-directed cancer treatment, today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation for IK-175, the Company’s novel aryl hydrocarbon receptor (AHR) antagonist, in combination with immune checkpoint inhibitors in patients with advanced urothelial carcinoma who have progressed on or within three months of receiving the last dose of checkpoint inhibitors.
Fast Track designation is reserved for therapies that represent potential best-in-class therapeutic options for diseases with high unmet need. Therapies that receive Fast Track designation often have the opportunity to communicate more frequently with the FDA on trial design and data and may also be eligible for priority review and accelerated approval. IK-175 is the second of Ikena’s candidates to receive Fast Track designation; the FDA has also granted the designation to IK-930, the Company’s novel TEAD inhibitor, in patients with unresectable NF2-deficient malignant pleural mesothelioma.
“There is an urgent need for new treatment options for urothelial carcinoma patients, many of whom find themselves out of options after progressing on checkpoint inhibitors. The Fast Track designation for IK-175 reflects the FDA’s interest in the potential role of our AHR antagonist to overcome the development of resistance to checkpoint inhibitors and supports our strategy of combining IK-175 with nivolumab to expand the number of cancer patients that can benefit from immunotherapy,” said Sergio Santillana, MD, Chief Medical Officer at Ikena.
IK-175 targets AHR, a compelling cancer-driving transcription factor that prevents immune recognition in a multitude of cancers by modulation of innate and adaptive immunity. Patients with urothelial carcinoma are generally treated through a combination of standard-of-care options, including surgery, chemotherapy, radiation and immunotherapies, including checkpoint inhibitors.
IK-175 is currently being studied in a Phase 1a/b clinical trial as a monotherapy and in combination with nivolumab in patients with advanced or metastatic solid tumors including urothelial carcinoma for which standard therapy is no longer effective or is intolerable (NCT04200963, or IK-175-001). Initial clinical data presented at the Society for Immunotherapy of Cancer (SITC) 2022 Annual Meeting demonstrated that IK-175 is well tolerated and showed encouraging, durable, anti-tumor activity in stage 1 of the trial’s monotherapy and combination arms in urothelial carcinoma patients. The IK-175 program is being developed in collaboration with Bristol Myers Squibb and they have an option to exclusively license the program through early 2024.
About Ikena Oncology
Ikena Oncology™ is focused on developing differentiated therapies for patients in need that target nodes of cancer growth, spread, and therapeutic resistance in the Hippo and RAS onco-signaling network. The Company’s lead targeted oncology program, IK-930, is a paralog-selective TEAD inhibitor addressing the Hippo signaling pathway, a known tumor suppressor pathway that also drives resistance to multiple targeted therapies. The Company’s additional research spans other targets in the Hippo pathway as well as the RAS signaling pathway, including developing IK-595, a novel MEK-RAF inhibitor. Additionally, IK-175, an AHR antagonist, is being developed in collaboration with Bristol Myers Squibb. Ikena aims to utilize their depth of institutional knowledge and breadth of tools to efficiently develop the right drug using the right modality for the right patient. To learn more, visit www.ikenaoncology.com or follow us on Twitter and LinkedIn.
Ikena gains on FDA’s fast track status for bladder cancer candidate
Mar. 06, 2023 8:42 AM ET
Ikena Oncology, Inc. (IKNA)BMY
By: Dulan Lokuwithana, SA News Editor
- Ikena Oncology (NASDAQ:IKNA) added ~9% pre-market Monday after the cancer-focused pharma company announced the FDA’s Fast Track designation for IK-175, a candidate targeted at urothelial carcinoma.
- https://seekingalpha.com/news/3944409-ikna-stock-gains-fdas-fast-track-status-bladder-cancer-candidate
- Ikena Oncology, Inc. (IKNA)
- https://ikenaoncology.com/pipeline/
LEQEMBI™ (lecanemab-irmb)
TRUSELTIQ (high-dose infigratinib)
LEQEMBI™ (lecanemab-irmb)
FDA Accepts Eisai’s Filing of a Supplemental Biologics License Application and Grants Priority Review for Traditional Approval of LEQEMBI™ (lecanemab-irmb) for the Treatment of Alzheimer’s Disease
MARCH 5, 2023 • NEWS RELEASE
Confirmatory Phase 3 Clarity AD data to be evaluated by FDA in determining whether to convert accelerated approval of LEQEMBI to a traditional approval
Priority Review accelerates FDA review time with a Prescription Drug User Fee Act (PDUFA) target action on July 6, 2023
TOKYO and CAMBRIDGE, Mass., March 05, 2023 (GLOBE NEWSWIRE) -- Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, "Eisai") and Biogen Inc. (Nasdaq: BIIB, Corporate headquarters: Cambridge, Massachusetts, CEO: Christopher A. Viehbacher, "Biogen") announced today that the U.S. Food and Drug Administration (FDA) has accepted Eisai’s supplemental Biologics License Application (sBLA) for LEQEMBI™ (lecanemab-irmb) 100 mg/mL injection for intravenous use, supporting the conversion of the accelerated approval of LEQEMBI to a traditional approval. The LEQEMBI application has been granted Priority Review, with a Prescription Drug User Fee Act (PDUFA) action date of July 6, 2023. The FDA is currently planning to hold an Advisory Committee to discuss this application but has not yet publicly announced the date of the meeting.
LEQEMBI is a humanized immunoglobulin gamma 1 (IgG1) monoclonal antibody directed against aggregated soluble (protofibrils*) and insoluble forms of amyloid beta (Aβ), approved under the Accelerated Approval Pathway for the treatment of Alzheimer's Disease (AD) on January 6, 2023. Treatment with LEQEMBI should only be initiated in patients with the mild cognitive impairment or mild dementia stage of disease and confirmed presence of Aβ pathology. On the same day that LEQEMBI received its accelerated approval, Eisai submitted the sBLA to the FDA for approval under the traditional pathway.
The sBLA is based on the findings from Eisai’s recently published large, global confirmatory Phase 3 clinical trial, Clarity AD. LEQEMBI met the primary endpoint and all key secondary endpoints with highly statistically significant results. In November 2022, results of the Clarity AD study were presented at the Clinical Trials on Alzheimer's Disease (CTAD) conference and simultaneously published in the peer-reviewed medical journal, The New England Journal of Medicine.
LEQEMBI was approved under accelerated approval in the U.S. and was launched in the U.S. on January 18, 2023. The accelerated approval was based on Phase 2 data that demonstrated that LEQEMBI reduced the accumulation of Aβ plaque in the brain, a defining feature of AD, and its continued approval may be contingent upon verification of LEQEMBI’s clinical benefit in a confirmatory trial. The FDA has determined that the results of Clarity AD can serve as the confirmatory study to verify the clinical benefit of lecanemab.
Eisai serves as the lead of LEQEMBI development and regulatory submissions globally with both Eisai and Biogen co-commercializing and co-promoting the product and Eisai having final decision-making authority.
* Protofibrils are large Aβ aggregated soluble species of 75-500 Kd.1
To learn more, visit www.LEQEMBI.com.
INDICATION, DOSAGE AND ADMINISTRATION, AND IMPORTANT SAFETY INFORMATION IN THE U.S.
INDICATION
LEQEMBI is indicated for the treatment of Alzheimer’s disease. Treatment with LEQEMBI should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was initiated in clinical trials. There are no safety or effectiveness data on initiating treatment at earlier or later stages of the disease than were studied. This indication is approved under accelerated approval based on reduction in amyloid beta plaques observed in patients treated with LEQEMBI. Continued approval for this indication may be contingent upon verification of clinical benefit in a confirmatory trial.
Please see full Prescribing Information in the U. S.
About LEQEMBITM (lecanemab-irmb)
LEQEMBITM (lecanemab-irmb) is the result of a strategic research alliance between Eisai and BioArctic. LEQEMBI is a humanized immunoglobulin gamma 1 (IgG1) monoclonal antibody directed against aggregated soluble (protofibril) and insoluble forms of amyloid-beta (Aβ). In the U.S., LEQEMBI was granted accelerated approval by the U.S. Food and Drug Administration (FDA) on January 6, 2023. LEQEMBI is indicated for the treatment of Alzheimer’s disease (AD) in the U.S. Treatment with LEQEMBI should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was initiated in clinical trials. There are no safety or effectiveness data on initiating treatment at earlier or later stages of the disease than were studied. This indication is approved under accelerated approval based on reduction in Aβ plaques observed in patients treated with LEQEMBI. Continued approval for this indication may be contingent upon verification of clinical benefit in a confirmatory trial.
In the U.S., Eisai submitted a supplemental Biologics License Application (sBLA) to the FDA for approval under the traditional pathway on January 6, 2023. The Clarity AD study of lecanemab met its primary endpoint and all key secondary endpoints with highly statistically significant results. Eisai submitted an application for manufacturing and marketing approval to the Pharmaceuticals and Medical Devices Agency (PMDA) on January 16, 2023, in Japan. The Priority Review was granted by the Ministry of Health, Labour and Welfare (MHLW) on January 26, 2023. Eisai utilized the prior assessment consultation system of PMDA, with the aim of shortening the review period for lecanemab. In Europe, Eisai submitted a marketing authorization application (MAA) to the European Medicines Agency (EMA) on January 9, 2023, and accepted on January 26, 2023. In China, Eisai initiated submission of data for a BLA to the National Medical Products Administration (NMPA) of China in December 2022, and the Priority Review was granted on February 27, 2023.
Eisai has completed lecanemab subcutaneous bioavailability study, and subcutaneous dosing is currently being evaluated in the Clarity AD OLE.
Since July 2020, Eisai's Phase 3 clinical study (AHEAD 3-45) for individuals with preclinical AD, meaning they are clinically normal and have intermediate or elevated levels of amyloid in their brains, is ongoing. AHEAD 3-45 is conducted as a public-private partnership between the Alzheimer's Clinical Trial Consortium (ACTC) that provides the infrastructure for academic clinical trials in AD and related dementias in the U.S., funded by the National Institute on Aging, part of the National Institutes of Health, Eisai and Biogen. The Tau NexGen clinical study for Dominantly Inherited AD (DIAD), that is conducted by Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU), led by Washington University School of Medicine in St. Louis, has been ongoing since January 2022.
2. About the Collaboration between Eisai and Biogen for AD
Eisai and Biogen have been collaborating on the joint development and commercialization of AD treatments since 2014. Eisai serves as the lead of lecanemab development and regulatory submissions globally with both companies co-commercializing and co-promoting the product and Eisai having final decision-making authority.
3. About the Collaboration between Eisai and BioArctic for AD
Since 2005, Eisai and BioArctic have had a long-term collaboration regarding the development and commercialization of AD treatments. Eisai obtained the global rights to study, develop, manufacture and market LEQEMBI for the treatment of AD pursuant to an agreement with BioArctic in December 2007. The development and commercialization agreement on the antibody LEQEMBI back-up was signed in May 2015.
4. About Eisai Co., Ltd.
Eisai's Corporate Concept is "to give first thought to patients and people in the daily living domain, and to increase the benefits that health care provides." Under this concept (also known as the human health care [hhc] concept), we aim to effectively achieve social good in the form of relieving anxiety over health and reducing health disparities. With a global network of R&D facilities, manufacturing sites and marketing subsidiaries, we strive to create and deliver innovative products to target diseases with high unmet medical needs, with a particular focus in our strategic areas of neurology and oncology.
In addition, we demonstrate our commitment to the elimination of neglected tropical diseases (NTDs), which is a target (3.3) of the United Nations Sustainable Development Goals (SDGs), by working on various activities together with global partners.
For more information about Eisai, please visit www.eisai.com (for global headquarters: Eisai Co., Ltd.), and connect with us on Twitter @Eisai_SDGs.
5. About Biogen
Founded in 1978, Biogen is a leading global biotechnology company that has pioneered multiple breakthrough innovations including a broad portfolio of medicines to treat multiple sclerosis, the first approved treatment for spinal muscular atrophy, and two co-developed treatments to address a defining pathology of Alzheimer’s disease. Biogen is advancing a pipeline of potential novel therapies across neurology, neuropsychiatry, specialized immunology and rare diseases and remains acutely focused on its purpose of serving humanity through science while advancing a healthier, more sustainable and equitable world.
The company routinely posts information that may be important to investors on its website at www.biogen.com. Follow Biogen on social media – Twitter, LinkedIn, Facebook, YouTube.
Biogen, Eisai's Alzheimer's drug Leqembi gets FDA priority review for traditional approval
Mar. 06, 2023 4:34 AM ET
Biogen Inc. (BIIB)ESALF, BRCTF, ESAIY
By: Ravikash, SA News Editor
The U.S. Food and Drug Administration (FDA) granted priority review to Biogen's (NASDAQ:BIIB) application seeking traditional approval of Alzheimer's disease (AD) therapy Leqembi (lecanemab) from its current status of accelerated approval.
TRUSELTIQ (high-dose infigratinib)
TRUSELTIQ (high-dose infigratinib)
MMRV Family of Vaccines -ProQuad, M-M-R®II, and VARIVAX
BridgeBio Announces Positive Phase 2 Cohort 5 Results of Infigratinib in Achondroplasia Demonstrating Mean Increase in Annualized Height Velocity of 3.03 cm/year with No Treatment-related Adverse Events
– In the highest dose level (Cohort 5, 0.25 mg/kg once daily), the mean change from baseline in annualized height velocity (AHV) at six months was +3.03 cm/yr (p = 0.0022) for the first 10 children with at least six months of follow-up in Cohort 5. The two remaining children who have not yet had six months of follow-up have a mean change from baseline in AHV of +8.8 cm/yr based on three months data
– 80% of children at six months were responders, as defined by an increase from baseline AHV of at least 25%. The mean change from baseline in AHV of responders was 3.81 cm/yr
– As a result of treatment, the median absolute AHV reached 7.6 cm/yr, which is beyond the 99th percentile of growth for children living with achondroplasia
– Infigratinib demonstrated clear dose-responsiveness as a single daily oral therapy and was well-tolerated with no adverse events (AEs) assessed as treatment-related in Cohort 5
– Based on the positive Phase 2 results, BridgeBio has started to enroll children for a pivotal Phase 3 trial
– BridgeBio expects to initiate clinical development of infigratinib for hypochondroplasia, a skeletal dysplasia closely related to achondroplasia and driven by fibroblast growth factor receptor 3 (FGFR3) gain-of-function variants, and will continue to explore the impact on the medical and functional complications of achondroplasia in future studies of infigratinib
PALO ALTO, Calif., March 06, 2023 (GLOBE NEWSWIRE) — BridgeBio Pharma, Inc. (Nasdaq: BBIO) (BridgeBio), a commercial-stage biopharmaceutical company focused on genetic diseases and cancers, today announced positive results from PROPEL2, a Phase 2 trial of the investigational therapy infigratinib in children with achondroplasia, demonstrating potential best-in-class efficacy and a clean safety profile. Infigratinib is an oral small molecule designed to inhibit FGFR3 and target achondroplasia at its source. BridgeBio will also host an investor call on March 6, 2023, at 7:30 am ET to discuss the results from the Phase 2 study.
To date, key results from the clinical trial include:
- At the highest dose level evaluated to date (Cohort 5, 0.25 mg/kg once daily), the mean increase from baseline in annualized height velocity (AHV) for the 10 children that have had six-month visits was +3.03 cm/yr (p = 0.0022). Individual data can be found in Figure 1 below
- The baseline AHV for the 10 children with six-month visits was in the expected range for children with achondroplasia at 3.73 cm/yr, rising to 6.77 cm/yr after treatment
- The two remaining children who have not yet had six months of follow-up have a mean change from baseline in AHV of +8.8 cm/yr at three months. The mean age for the cohort was 7.24 years
- 80% of the 10 children with six-month visits were responders, with a change from baseline AHV of at least 25%. Among the responders, the average change from baseline in AHV was +3.81 cm/yr
- Preliminary analysis of Collagen X (CXM) levels also saw a statistically significant increase from baseline in Cohort 5 (p=.03). CXM is the gold-standard biomarker of chondrocyte-driven growth and further validates the robust response to infigratinib
- Combined with the previously reported Cohort 4 change from baseline in AHV value of +1.52 cm/yr, the Cohort 5 data demonstrate a strong dose response for infigratinib
- Median follow-up across all cohorts is 71.1 weeks. To date, the study has shown a well-tolerated safety profile, with no study drug related treatment emergent adverse events (TEAEs) in Cohort 5. No serious adverse events (SAEs) or discontinuations due to AEs were reported in any cohort
Figure 1
“The data from Cohort 5 has shown a major impact on annualized height velocity for children with achondroplasia and an excellent safety profile to date. We are thrilled to see these promising results and consider that AHV increases of this magnitude will translate to improvements in the medical and functional complications of achondroplasia. We are excited about taking the next steps towards initiating a Phase 3, pivotal clinical trial,” said Professor Ravi Savarirayan, M.D., Ph.D., clinical geneticist and group leader of molecular therapies research at the Murdoch Children’s Research Institute in Australia, the lead investigator for PROPEL2.
“I am encouraged by these efficacy and safety results and thankful for our partnership with the physicians, community advocates, children, and families in this study. These results reach a new tier of efficacy, and coupled with our differentiated safety and convenience profile, provide us the opportunity to serve children with achondroplasia and other skeletal dysplasias. We look forward to exploring the potential of infigratinib on the wider medical and functional impacts of achondroplasia, hypochondroplasia and other skeletal dysplasias, which hold significant unmet needs for families,” said Neil Kumar, Ph.D., founder and CEO of BridgeBio.
Based on the positive results to date, BridgeBio has started enrolling children in the run-in for a Phase 3 trial. Additionally, BridgeBio expects to initiate clinical development for infigratinib in hypochondroplasia, a skeletal dysplasia closely related to achondroplasia and similarly driven by FGFR3 gain-of-function variants. BridgeBio has previously presented promising preclinical data for hypochondroplasia at ENDO 2022 and ASHG 2022.
“Achondroplasia can have broad impact that affects the whole person. People can experience a range of medical complications, including foramen magnum stenosis, spinal stenosis, cardiovascular complications, sleep-disordered breathing, obesity, and sometimes, individuals may need surgical intervention. In addition to the potential medical and physical complications, people with achondroplasia may also experience social and emotional impacts as a result of living with the condition. We are encouraged by BridgeBio’s mission to develop a therapy with the potential to address this as a whole-person condition that affects the overall health, independent function, and quality of life of those with achondroplasia,” said Dianne Kremidas, executive director of The MAGIC Foundation.
Infigratinib has IP protection out to at least 2041.
Webcast Information
BridgeBio will host an investor call and simultaneous webcast to discuss the Phase 2 data from Cohort 5 of infigratinib in children with achondroplasia on March 6, 2023 at 7:30 am ET. A link to the webcast may be accessed from the event calendar page of BridgeBio’s website at https://investor.bridgebio.com/.
A replay of the conference call and webcast will be archived on the Company’s website and will be available for at least 30 days following the event.
About Achondroplasia
Achondroplasia is the most common cause of disproportionate short stature, affecting approximately 55,000 people in the United States (US) and European Union (EU), including up to 10,000 children and adolescents with open growth plates. Achondroplasia impacts overall health and quality of life, leading to medical complications such as obstructive sleep apnea, middle ear dysfunction, kyphosis, and spinal stenosis. The condition is uniformly caused by an activating mutation in FGFR3.
About BridgeBio Pharma, Inc.
BridgeBio Pharma (BridgeBio) is a commercial-stage biopharmaceutical company founded to discover, create, test and deliver transformative medicines to treat patients who suffer from genetic diseases and cancers with clear genetic drivers. BridgeBio’s pipeline of development programs ranges from early science to advanced clinical trials. BridgeBio was founded in 2015 and its team of experienced drug discoverers, developers and innovators are committed to applying advances in genetic medicine to help patients as quickly as possible. For more information visit bridgebio.com and follow us on LinkedIn and Twitter.
BridgeBio soars 55% after Phase 2 data for achondroplasia candidate
Mar. 06, 2023 8:21 AM ET
By: Dulan Lokuwithana, SA News Editor
BridgeBio Pharma (NASDAQ:BBIO) jumped ~55% pre-market Monday after announcing Phase 2 data for infigratinib, which is an investigational therapy for children with achondroplasia, the most common cause of disproportionate short stature.
MMRV Family of Vaccines -ProQuad, M-M-R®II, and VARIVAX
MMRV Family of Vaccines -ProQuad, M-M-R®II, and VARIVAX
MMRV Family of Vaccines -ProQuad, M-M-R®II, and VARIVAX
US FDA Approves Intramuscular Administration for Merck’s MMRV Family of Vaccines: M-M-RII (Measles, Mumps, and Rubella Virus Vaccine Live), VARIVAX (Varicella Virus Vaccine Live), and ProQuad (Measles, Mumps, Rubella and Varicella Virus Vaccine Live)
March 6, 2023 6:45 am ET
With this additional route of administration, the MMRV Family now joins other routinely recommended vaccines that can be administered intramuscularly
RAHWAY, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, announced today that the U.S. Food and Drug Administration (FDA) has approved the addition of the intramuscular (IM) route of administration to the United States Product Insert (USPI) for Merck’s MMRV family of vaccines: M-M-R®II, VARIVAX®, and ProQuad®.
While these vaccines have a long history in the U.S., until now they have only been administered via subcutaneous (SC) injection.
“Building on our history of innovation in the world of vaccines, we’re proud to introduce another method of administration for M-M-R®II, VARIVAX®, and ProQuad® vaccines, which have been important in the fight against measles, mumps, rubella, and varicella in the U.S.,” said Dr. Eliav Barr, senior vice president, head of global clinical development and chief medical officer, Merck Research Laboratories.
With these approvals, healthcare professionals now have the option to choose to administer all routinely recommended injectable pediatric vaccinations included in the CDC immunization schedule, via the same IM route. In the U.S., the only measles, mumps, rubella, and varicella vaccines that can be administered IM are M-M-R®II, VARIVAX®, and ProQuad®. Additionally, the MMRV family of vaccines has already been licensed for IM administration in the European Union.
“As a pediatrician who routinely vaccinates children, I am excited to now have the option to administer these vaccines intramuscularly,” said Dr. Todd Wolynn, co-founding pediatrician of Kids Plus Pediatrics. “This approval provides our practice with an additional route of administration.”
About the MMRV Family of Vaccines
ProQuad® is a vaccine indicated for active immunization for the prevention of measles, mumps, rubella, and varicella in children 12 months through 12 years of age. It was approved by the FDA in 2005. VARIVAX® is a vaccine indicated for active immunization for the prevention of varicella in individuals 12 months of age or older. It received FDA approval in 1995 and remains the only varicella vaccine available for use in the U.S. M-M-R®II is indicated for active immunization for the prevention of measles, mumps, and rubella in individuals 12 months of age or older and received FDA approval in 1978.
Indications and Usage
ProQuad is a vaccine indicated for active immunization for the prevention of measles, mumps, rubella, and varicella in children 12 months through 12 years of age.
VARIVAX is a vaccine indicated for active immunization for the prevention of varicella in individuals 12 months of age or older.
M-M-R®II is indicated for active immunization for the prevention of measles, mumps, and rubella in individuals 12 months of age or older.
Dosage and Administration
ProQuad:
Each dose of ProQuad is approximately 0.5 mL and is administered intramuscularly or subcutaneously.
At least 1 month should elapse between a dose of a measles-containing vaccine such as M-M-R®II and a dose of ProQuad. At least 3 months should elapse between a dose of varicella-containing vaccine and ProQuad.
VARIVAX:
Each dose is approximately 0.5 mL and is administered intramuscularly or subcutaneously.
The first dose is administered at 12 to 15 months of age. The second dose is administered at 4 to 6 years of age. There should be a minimum interval of 3 months between doses. 12 months to 12 years of age: If a second dose is administered, there should be a minimum interval of 3 months between doses. Adolescents (≥13 years of age) and Adults: 2 doses, to be administered with a minimum interval of 4 weeks between doses.
M-M-R®II:
The dose for any age is approximately 0.5 mL administered intramuscularly or subcutaneously.
The recommended age for primary vaccination is 12 to 15 months and the second dose should be given at 4 to 6 years of age.
Before administrating VARIVAX® (Varicella Virus Vaccine Live), M-M-R®II (Measles, Mumps, and Rubella Virus Vaccine Live), or ProQuad® (Measles, Mumps, Rubella and Varicella Virus Vaccine Live), please read the Prescribing Information. The Patient Information also is available for VARIVAX, M-M-R®II, and ProQuad.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on Twitter, Facebook, Instagram, YouTube and LinkedIn.
Source: Merck & Co., Inc.
FDA approves intramuscular administration for Merck’s MMRV family of vaccines
Mar. 06, 2023 6:56 AM ET
By: Mamta Mayani, SA News Editor
- Merck (NYSE:MRK) announces that the FDA has approved the addition of the intramuscular (IM) route of administration to the United States Product Insert (USPI) for Merck’s MMRV family of vaccines: M-M-RII, VARIVAX, and ProQuad.
- Until now these vaccines have only been administ
- https://seekingalpha.com/news/3944331-fda-approves-intramuscular-administration-for-mercks-mmrv-family-of-vaccines
- Merck & Co., Inc. (MRK)
- https://www.merckvaccines.com/
Temferon
MMRV Family of Vaccines -ProQuad, M-M-R®II, and VARIVAX
Temferon
FDA Grants Orphan Drug Designation to Temferon for Treatment of Glioblastoma Multiforme
Mar 02, 2023
MILAN and NEW YORK, March 02, 2023 (GLOBE NEWSWIRE) -- Genenta Science (NASDAQ: GNTA), a clinical-stage immuno-oncology company developing a cell-based platform harnessing the power of hematopoietic stem cells to provide durable and safe treatments for solid tumors, today announced that the U.S. Food and Drug Administration (FDA) has granted Orphan Drug Designation (ODD) to Temferon™ for the treatment of glioblastoma multiforme (GBM).
"We expect that the FDA’s decision to grant Orphan Drug Designation to Temferon will enhance the development of our cell therapy, which we believe has the potential to address the unmet medical need of patients and strengthen our clinical program," said Pierluigi Paracchi, Chief Executive Officer of Genenta. "The Orphan Drug Designation program highlights the significant need for an efficacious therapy for patients suffering from glioblastoma multiforme."
Temferon is a proprietary cell therapy designed to reprogram the tumor microenvironment by delivering immunomodulatory molecules directly to tumors. Genenta is testing Temferon in an ongoing Phase 1/2a clinical trial in newly diagnosed patients with GBM who have an unmethylated MGMT gene promoter (uMGMT-GBM).
GBM is the most common malignant primary brain tumor and the most aggressive diffuse glioma, with unmethylated MGMT promoter status identified in approximately 60% of the GBM population.
The ODD program supports the development of treatments that address diseases affecting fewer than 200,000 people in the United States (which equates to approximately 6 cases per 10,000 population). Incentives that come with the designation include eligibility for federal grants, tax credits for qualified clinical trials, prescription drug user fee exemptions, and a seven-year marketing exclusivity period upon FDA approval.
About Genenta Science
Genenta (www.genenta.com) is a clinical-stage biotechnology company engaged in the development of a proprietary hematopoietic stem cell gene therapy for the treatment of a variety of solid tumor cancers. Temferon™ is based on ex-vivo gene transfer into autologous Tie2+ hematopoietic stem/progenitor cells (HSPCs) to deliver immunomodulatory molecules directly via tumor-infiltrating monocytes/macrophages (Tie2 Expressing Monocytes - TEMs). Temferon™, which is under investigation in a phase 1/2a clinical trial in newly diagnosed Glioblastoma Multiforme patients who have an unmethylated MGMT gene promoter (uMGMT-GBM), is designed to reach solid tumors, induce a durable immune response not restricted to pre-selected tumor antigens nor type, and avoid systemic toxicity, which are some of the main unresolved challenges in immuno-oncology.
Source: Genenta Science
Genenta's brain cancer cell therapy gets FDA orphan drug status
Mar. 02, 2023 7:04 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted orphan drug designation (ODD) to Genenta Science's (NASDAQ:GNTA) to Temferon to treat glioblastoma multiforme (GBM), a type of brain cancer.
- https://seekingalpha.com/news/3943156-genenta-brain-cancer-cell-therapy-gets-fda-orphan-drug-status
- Genenta Science S.p.A. (GNTA)
- https://www.genenta.com/our-pipeline/
ADX-2191
MMRV Family of Vaccines -ProQuad, M-M-R®II, and VARIVAX
Temferon
FDA Accepts for Priority Review ADX-2191 New Drug Application for the Treatment of Primary Vitreoretinal Lymphoma
March 2, 2023
PDUFA Date is June 21, 2023
Planned U.S. Launch of ADX-2191 in Second Half of 2023, Pending Approval by the FDA
ADX-2191 with Potential to be the First FDA-Approved Drug Available for Patients Suffering from Primary Vitreoretinal Lymphoma
LEXINGTON, Mass.--(BUSINESS WIRE)--Mar. 2, 2023-- Aldeyra Therapeutics, Inc. (Nasdaq: ALDX) (Aldeyra) today announced that the U.S. Food and Drug Administration (FDA) accepted for Priority Review the New Drug Application (NDA) for ADX-2191 (methotrexate injection, USP), an investigational drug candidate, for the treatment of primary vitreoretinal lymphoma. The FDA assigned a Prescription Drug User Fee Act (PDUFA) date of June 21, 2023. The FDA noted that no potential filing review issues have been identified.
“The FDA’s decision to grant Priority Review with a PDUFA date four months from NDA acceptance underscores the significant need for an FDA-approved treatment of primary vitreoretinal lymphoma, a rare but potentially fatal cancer,” stated Todd C. Brady, M.D., Ph.D., Aldeyra’s President and Chief Executive Officer. “We are working closely with the FDA during the review process to bring ADX‑2191 to patients as quickly as possible, and plan to launch ADX-2191 in the United States in the second half of this year, pending approval by the FDA.”
The NDA submission is supported by a combination of more than three decades of published literature on the safety and efficacy of methotrexate, the active ingredient of ADX‑2191, for the treatment of primary vitreoretinal lymphoma, in addition to safety data from the recently completed Phase 3 GUARD Trial of ADX-2191 in patients with proliferative vitreoretinopathy. During the Phase 3 GUARD Trial, no safety signals were observed, and ADX-2191 was well tolerated; there were no observed treatment-emergent serious adverse events. The most common adverse event associated with ADX‑2191 treatment was punctate keratitis, a frequently observed side effect of intravitreal methotrexate, that was most commonly mild in severity.
About ADX-2191
ADX-2191 (methotrexate injection, USP) is a sterile, non-compounded intravitreal formulation of methotrexate for the potential prevention or treatment of specific rare retinal diseases, including primary vitreoretinal lymphoma, proliferative vitreoretinopathy, and retinitis pigmentosa. The ADX-2191 intravitreal formulation is preservative-free, is designed to be vitreous-compatible, and is optimized for excipient composition, viscosity, density, tonicity, pH, concentration, and volume of administration. ADX-2191 has received FDA Orphan Drug Designation for the prevention of proliferative vitreoretinopathy, and for the treatment of primary vitreoretinal lymphoma and retinitis pigmentosa.
About Primary Vitreoretinal Lymphoma
Primary vitreoretinal lymphoma is a rare, aggressive, and potentially fatal retinal cancer that is diagnosed in approximately 300 to 600 patients in the United States per year. The median survival for newly diagnosed patients is less than five years. No approved treatments are currently available, though intravitreal injection of compounded methotrexate represents the current standard of care.
About Aldeyra
Aldeyra Therapeutics is a clinical-stage biotechnology company developing innovative therapies designed to treat immune-mediated diseases. Our approach is to discover and develop pharmaceuticals that modulate immunological systems, instead of directly inhibiting or activating single protein targets, with the goal of optimizing multiple pathways at once while minimizing toxicity. Our product candidates include RASP (reactive aldehyde species) modulators ADX-629, ADX-246, ADX-248, and chemically related molecules for the potential treatment of systemic and retinal immune-mediated diseases. Our pre-commercial product candidates are reproxalap, a RASP modulator for the potential treatment of dry eye disease (under U.S. Food and Drug Administration New Drug Application review) and allergic conjunctivitis, and ADX-2191, a novel formulation of intravitreal methotrexate for the potential treatment of primary vitreoretinal lymphoma (under U.S. Food and Drug Administration New Drug Application review), proliferative vitreoretinopathy, and other rare sight-threatening retinal diseases. For more information, visit https://www.aldeyra.com/ and follow us on LinkedIn, Facebook, and Twitter.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230301005873/en/
Source: Aldeyra Therapeutics, Inc.
FDA accepts for priority review Aldeyra's ADX-2191 application in retinal cancer
Mar. 02, 2023 7:27 AM ET
Aldeyra Therapeutics, Inc. (ALDX)
By: Mamta Mayani, SA News Editor
- Under Priority Review, the FDA has accepted Aldeyra Therapeutics' (NASDAQ:ALDX) New Drug Application (NDA) for ADX-2191 (methotrexate injection, USP), an investigational drug candidate, for the treatment of primary vitreoretinal lymphoma.
- https://seekingalpha.com/news/3943183-fda-accepts-for-priority-review-aldeyras-adx-2191-application-in-retinal-cancer
- Aldeyra Therapeutics, Inc. (ALDX)
- https://www.aldeyra.com/pipeline-disease-areas/
Milvexian
NUBEQA® (darolutamide)
Batiraxcept
The Bristol Myers Squibb-Janssen Collaboration Launches Pivotal Phase 3 Librexia Clinical Trial Program Evaluating Milvexian, an Investigational Oral Factor XIa Inhibitor
03/02/2023CATEGORY:
The Librexia program is the most comprehensive Factor XIa Phase 3 clinical development program, and will provide indispensable data from nearly 50,000 patients across three simultaneous trials including Librexia STROKE, Librexia ACS and Librexia AF
First patient has been enrolled in Librexia STROKE trial
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE: BMY) in collaboration with Janssen Pharmaceuticals, Inc., one of the Janssen Pharmaceutical Companies of Johnson and Johnson (Janssen) today announced the launch of the Phase 3 Librexia program studying milvexian, an investigational oral factor XIa (FXIa) inhibitor (antithrombotic).
The Librexia program is unrivaled as the most comprehensive FXIa development program to date and will provide important data from nearly 50,000 patients across three indication-seeking studies: Librexia STROKE, Librexia ACS and Librexia AF. Enrollment has begun for the Librexia STROKE trial, which is evaluating milvexian in addition to standard of care antiplatelet therapy for stroke prevention in patients after an acute ischemic stroke or high-risk transient ischemic attack. The Librexia ACS trial, which will evaluate event reduction in acute coronary syndromes in addition to standard of care antiplatelet therapy, and the Librexia AF trial, which will investigate milvexian compared to apixaban in the prevention of stroke in patients with atrial fibrillation, will also initiate during the first half of 2023.
“The depth and breadth of the Librexia clinical development program will capture data in three related but distinct areas of clinical need related to residual risk of thrombotic events and patient bleeding, and evaluate milvexian’s potential to advance beyond the current standard of care and improve patient outcomes in acute coronary syndromes, atrial fibrillation and ischemic stroke,” said Robert Harrington, M.D., Arthur L. Bloomfield professor of medicine and chair of the Department of Medicine, Stanford University, Librexia program chair. “A novel treatment that enhances the benefit-risk profile will be a clinically meaningful and welcomed advance in the treatment of these conditions.”
Important Phase 2 proof-of-concept data for milvexian demonstrated a differentiated antithrombotic profile as both a monotherapy and in combination with antiplatelet therapy. This included data in patients with ischemic stroke or high-risk transient ischemic attack that may suggest a compelling benefit-risk profile, ultimately enabling the initiation of the Librexia program this year.
“The Librexia program is a first-of-its-kind clinical program, with three Phase 3 trials running concurrently that aim to investigate whether milvexian can improve the benefit-risk profile in thrombotic care by delivering reduced thrombotic events with less bleeding for more patients in need,” said Roland Chen, M.D., senior vice president and head, Cardiovascular Development, Global Drug Development, Bristol Myers Squibb. “BMS and Janssen bring deep heritage and expertise in cardiovascular care to this program, in partnership with renowned experts, and we look forward to continuing to evaluate the potential of milvexian to address key unmet medical needs for patients living with thrombotic diseases.”
The Librexia STROKE trial is an event-driven registrational trial powered to show superiority in reducing the risk of stroke/ischemic events on top of standard of care antiplatelet therapy. Librexia ACS and Librexia AF trials are expected to begin enrolling within the first half of 2023. More information on the Librexia STROKE trial can be found on http://www.clinicaltrials.gov (NCT05702034).
About Milvexian*
Milvexian is an investigational, oral factor XIa (FXIa) inhibitor (antithrombotic) being studied for the prevention and treatment of major thrombotic conditions as part of the Librexia program, the most comprehensive FXIa clinical development program today.
*Milvexian is an investigational agent and has not been approved for use in any country, for any indication.
About the Librexia Program
The Librexia program is the most comprehensive and unrivaled FXIa clinical development program today, studying nearly 50,000 patients across three concurrent clinical trials (Librexia STROKE, Librexia ACS and Librexia AF). Grounded in strong Phase 2 efficacy and safety data, the Librexia program aims to investigate whether milvexian can enhance the benefit-risk profile associated with treating patients with these three conditions by delivering reduced thrombotic events with no increased risk of bleeding. The program is designed and powered for success to potentially advance beyond the standard of care and help improve outcomes in a wide range of patients with thrombotic diseases.
About Librexia STROKE
Librexia STROKE is a Phase 3, randomized, double-blind, parallel-group, placebo-controlled study to demonstrate the efficacy and safety of milvexian in addition to single or dual antiplatelet therapy for stroke prevention after an acute ischemic stroke or high-risk transient ischemic attack (TIA). More information can be found on http://www.clinicaltrials.gov (NCT05702034).
About Librexia ACS
Librexia ACS is a randomized, double-blind, placebo-controlled, event-driven study to demonstrate the efficacy and safety of milvexian after a recent acute coronary syndrome.
AboutLibrexia AF
Librexia AF is a randomized, double-blind, double-dummy, parallel group, active-controlled study to evaluate the efficacy and safety of milvexian versus apixaban in participants with atrial fibrillation.
About AXIOMATIC-SSP and AXIOMATIC-TKR
The milvexian Phase 2 clinical trial program consisted of two Phase 2 studies: AXIOMATIC-TKR, a randomized, open-label, parallel-group, dose-ranging multicenter study that evaluated the efficacy and safety of milvexian versus subcutaneous enoxaparin in patients undergoing elective total knee replacement (TKR) surgery, and AXIOMATIC-SSP, a Phase 2, global, randomized, double-blind, placebo-controlled, dose-ranging study that evaluated the efficacy and safety of milvexian for the prevention of new symptomatic ischemic stroke or new covert brain infarction in patients receiving aspirin and clopidogrel following acute ischemic stroke or transient ischemic attack (TIA).
A total of 3,608 patients were enrolled across both studies. More information can be found on http://www.clinicaltrials.gov (NCT03766581, NCT03891524).
About the Bristol Myers Squibb-Janssen Collaboration
Bristol Myers Squibb and the Janssen Pharmaceutical Companies of Johnson & Johnson (Janssen),two unsurpassed leaders in cardiovascular care, are determined to close the gap in unmet needs in thrombosis management by overcoming the limits of today’s treatments. The collaboration to develop and commercialize milvexian aims to leverage the combined scientific heritage and world-class commercial capabilities of each company, all in service of improved patient outcomes. The collaboration is uniquely equipped to deliver on the promise of FXIa inhibitors and is working diligently to ensure cutting-edge safe and effective treatment options are available for patients.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
Bristol Myers, Janssen launch late-stage Librexia program evaluating milvexian
Mar. 02, 2023 8:01 AM ET
Bristol-Myers Squibb Company (BMY)JNJ
By: Mamta Mayani, SA News Editor
- Bristol Myers Squibb (NYSE:BMY) in collaboration with Janssen Pharmaceuticals, a Johnson and Johnson (JNJ) company announces the launch of Phase 3 Librexia program studying milvexian, an investigational oral factor XIa (FXIa) inhibitor (antithrombotic).
- https://seekingalpha.com/news/3943202-bristol-myers-janssen-launch-late-stage-librexia-program-evaluating-milvexian
- Bristol-Myers Squibb Company (BMY)JNJ
- https://www.janssen.com/
- https://www.bms.com/
Batiraxcept
NUBEQA® (darolutamide)
Batiraxcept
Feb 28, 2023
Aravive Announces FDA Orphan Drug Designation Granted to Batiraxcept for the Treatment of Pancreatic Cancer
- Dose escalation portion of ongoing Phase 1b/2 pancreatic adenocarcinoma trial initiated, with preliminary results expected in 2H 2023
HOUSTON, Feb. 28, 2023 (GLOBE NEWSWIRE) -- Aravive, Inc. (Nasdaq: ARAV, “the Company”), a late clinical-stage oncology company developing targeted therapeutics to treat metastatic disease, today announced that the U.S. Food and Drug Administration (FDA) has granted Orphan Drug Designation (ODD) to batiraxcept for the treatment of pancreatic ductal adenocarcinoma cancer (PDAC).
The FDA’s Office of Orphan Products Development grants ODD status to a drug or biological product to prevent, diagnose or treat a rare disease or condition affecting fewer than 200,000 people in the USA. Companies that are granted ODD are eligible for incentives, including tax credits for qualified clinical trials, exemption from user fees and up to seven years of market exclusivity after approval.
“Receiving Orphan Drug Designation is another important milestone for batiraxcept, and it underscores the significant unmet medical need in patients with pancreatic cancer, typically diagnosed at an incurable advanced stage with a 5-year survival rate of 11%1,” said Gail McIntyre, Ph.D., DABT, Chief Executive Officer of Aravive. “Three patients from our P1b trial are still responding to treatment with 15mg/kg batiraxcept, gemcitabine and nab-paclitaxel after 1 year and one patient has a confirmed complete response. Consistent with our other clinical trials, we noted a relationship between clinical activity and batiraxcept drug levels, however highly fibrotic tumors like PDAC may require more batiraxcept than platinum-resistant ovarian cancer and clear cell renal cell cancer patients to reach the appropriate batiraxcept drug levels. Due to this characteristic of pancreatic cancer, we are testing higher doses of batiraxcept to see if we can increase the proportion of patients who benefit from the triplet regimen.”
Batiraxcept (15mg/kg on Days 1 & 15) is currently being evaluated in a Phase 1b/2 trial (NCT04983407) as first-line treatment in combination with gemcitabine (1000 mg/m2 on Days 1, 8, & 15) and nab-paclitaxel (125 mg/m2 on Days 1, 8, & 15) in patients with locally advanced (nonresectable Stage II or Stage III) or metastatic (Stage IV) pancreatic adenocarcinoma. The Phase 1b portion of the trial is ongoing and the dose escalation phase was initiated this month. Preliminary results from the 20mg/kg batiraxcept plus gemcitabine and nab-paclitaxel cohort are anticipated in the second half of 2023. In addition to ODD granted by the FDA in pancreatic cancer, batiraxcept was previously granted ODD by the European Commission in platinum resistant recurrent ovarian cancer (PROC) and was granted Fast Track Designation by the FDA in PROC and clear cell renal cell carcinoma (ccRCC).
About Aravive
Aravive, Inc. is a late clinical-stage oncology company developing targeted therapeutics to treat metastatic disease. Batiraxcept (formerly AVB-500), is an ultra-high affinity decoy protein that binds to GAS6, the sole ligand that activates AXL, thereby inhibiting metastasis and tumor growth, and restoring sensitivity to anti-cancer agents. Batiraxcept has been granted Fast Track Designation by the U.S. FDA for both clear cell renal cell carcinoma and platinum-resistant ovarian cancer and Orphan Drug Designation by the European Commission in platinum resistant recurrent ovarian cancer. Batiraxcept is in an active registrational Phase 3 trial in platinum resistant ovarian cancer (NCT04729608), a Phase 1b/2 trial in clear cell renal cell carcinoma (NCT04300140), and a Phase 1b/2 trial in pancreatic adenocarcinoma (NCT04983407). The Company is based in Houston, Texas and received a Product Development Award from the Cancer Prevention & Research Institute of Texas (CPRIT) in 2016. Additional information at www.aravive.com.
Aravive stock pops on FDA orphan drug status for batiraxcept to treat pancreatic cancer
Mar. 01, 2023 5:01 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted orphan drug designation (ODD) to Aravive's (NASDAQ:ARAV) batiraxcept to treat pancreatic ductal adenocarcinoma cancer (PDAC).
- https://seekingalpha.com/news/3942389-aravive-stock-pops-on-fda-orphan-drug-status-for-batiraxcept-to-treat-pancreatic-cancer
- Aravive, Inc. (ARAV)
- https://aravive.com/
- https://aravive.com/pipeline/
NUBEQA® (darolutamide)
NUBEQA® (darolutamide)
LEQEMBI™ (lecanemab-irmb) injection
3/1/2023
Darolutamide receives EU approval for additional indication in prostate cancer
Darolutamide receives EU approval for additional indication in prostate cancer
ORION CORPORATION
PRESS RELEASE
1 March 2023 at 13:00 EET
Darolutamide receives EU approval for additional indication in prostate cancer
- European Commission granted approval of darolutamide for the treatment of patients with metastatic hormone-sensitive prostate cancer (mHSPC)
- Approval is based on Phase III ARASENS trial data
The European Commission has granted marketing authorisation in the European Union (EU) for darolutamide, an oral androgen receptor inhibitor (ARi), plus androgen deprivation therapy (ADT) in combination with docetaxel, for the treatment of patients with metastatic hormone-sensitive prostate cancer (mHSPC). Darolutamide is already approved under the brand name Nubeqa® for the treatment of patients with non-metastatic castration-resistant prostate cancer (nmCRPC), who are at high risk of developing metastatic disease.
The EU approval is based on the positive results from the Phase III ARASENS trial, which demonstrated that darolutamide plus ADT in combination with docetaxel significantly reduced the risk of death by 32.5% compared to ADT with docetaxel, in patients with mHSPC. Additionally, the darolutamide combination showed consistent benefits across clinically relevant secondary endpoints, with the overall incidence of treatment-emergent adverse events being similar between treatment arms.
Prostate cancer is the most commonly diagnosed cancer in men in almost all northern and western European countries.1 Only 30% of men with mHSPC will survive five years or more after diagnosis.2 Most men with mHSPC eventually progress to metastatic castration-resistant prostate cancer (mCRPC), a condition with limited long-term survival.3,4
Darolutamide is being investigated in a broad development program with an additional three ongoing or planned large clinical studies, to investigate its potential across prostate cancer patients from the early- to the late-stage of this disease. This includes the ARANOTE Phase III trial evaluating darolutamide and ADT versus ADT alone for mHSPC.
Darolutamide is developed jointly by Orion and Bayer. Bayer is responsible for global commercialization, with co-promotion from Bayer and Orion in certain European markets, e.g. France, Germany, Italy, Spain, the UK, Scandinavia and Finland.
About the ARASENS Trial
The ARASENS trial is a randomized, Phase III, multi-center, double-blind, placebo-controlled trial which was prospectively designed to investigate the efficacy and safety of oral darolutamide, an androgen receptor inhibitor (ARi), plus androgen deprivation therapy (ADT) and the chemotherapy docetaxel in patients with metastatic hormone-sensitive prostate cancer (mHSPC). A total of 1,306 newly diagnosed patients were randomized in a 1:1 ratio to receive 600 mg of darolutamide twice a day or matching placebo, plus ADT and docetaxel.
The primary endpoint of this trial was overall survival (OS). Secondary endpoints included time to castration-resistant prostate cancer (CRPC), time to pain progression, time to first symptomatic skeletal event (SSE), time to initiation of subsequent anticancer therapy, all measured at 12‐week intervals, as well as adverse events (AEs) as a measure of safety and tolerability. Results from this trial were published in the New England Journal of Medicine.5 The ARASENS trial demonstrated that darolutamide plus androgen deprivation therapy (ADT) and docetaxel significantly reduced the risk of death by 32.5% compared to ADT plus docetaxel.5 Improvements in the secondary endpoints supported the benefit observed in the primary endpoint, overall survival.5
About Metastatic Hormone-Sensitive Prostate Cancer
Prostate cancer is the second most commonly diagnosed malignancy in men worldwide. In 2020, an estimated 1.4 million men were diagnosed with prostate cancer, and about 375,000 died from the disease worldwide.6
At the time of diagnosis, most men have localized prostate cancer, meaning their cancer is confined to the prostate gland and can be treated with curative surgery or radiotherapy. Upon relapse, when the disease will metastasise or spread, or if the disease is newly diagnosed, but has already spread, the disease is hormone-sensitive and androgen deprivation therapy (ADT) is the cornerstone of treatment for this hormone-sensitive disease. Current treatment options for men with metastatic hormone-sensitive prostate cancer (mHSPC) include hormone therapy, such as ADT, androgen receptor pathway inhibitors plus ADT or a combination of docetaxel chemotherapy and ADT. Despite these treatments, a large proportion of men with mHSPC will eventually experience progression to metastatic castration-resistant prostate cancer (mCRPC), a condition with limited survival.
About darolutamide
Darolutamide is an oral androgen receptor inhibitor (ARi) with a distinct chemical structure that binds to the receptor with high affinity and exhibits strong antagonistic activity, thereby inhibiting the receptor function and the growth of prostate cancer cells. The low potential for blood-brain barrier penetration for darolutamide is supported by preclinical models and neuroimaging data in healthy humans. This is supported by the overall low incidence of central nervous system (CNS)-related adverse events (AEs) compared to placebo as seen in the ARAMIS Phase III trial7 and the maintained verbal learning and memory observed in the darolutamide arm of the Phase II ODENZA trial.8
The product is approved under the brand name Nubeqa® in more than 80 countries around the world, including the U.S., EU, Japan and China, for the treatment of patients with non-metastatic castration-resistant prostate cancer (nmCRPC), who are at high risk of developing metastatic disease. It is also approved for the treatment of patients with metastatic hormone-sensitive prostate cancer (mHSPC) in a number of markets including the U.S. and Japan. Filings in other regions are underway or planned by Bayer. The compound is also being investigated in further studies across various stages of prostate cancer, including in the ARANOTE Phase III trial evaluating darolutamide plus androgen deprivation therapy (ADT) versus ADT alone for metastatic hormone-sensitive prostate cancer (mHSPC), as well as the Australian and New Zealand Urogenital and Prostate Cancer Trials Group (ANZUP) led international Phase III co-operative group DASL-HiCaP (ANZUP1801) trial evaluating darolutamide as an adjuvant treatment for localised prostate cancer with very high risk of recurrence. Information about these trials can be found at www.clinicaltrials.gov. In addition, a study to explore the potential of darolutamide in the early setting for patients who have experienced a rise in their prostate specific antigen (PSA) levels following surgery or radiation, is also planned.
Orion wins EU approval for darolutamide for additional indication in prostate cancer
Mar. 01, 2023 7:15 AM ET
By: Mamta Mayani, SA News Editor
The European Commission has granted marketing authorization in the European Union (EU) for Orion's (OTCPK:ORINY) darolutamide, an oral androgen receptor inhibitor (ARi), plus androgen deprivation therapy (ADT) in combination with docetaxel, for the treatment of patients with metastatic hormone-sensitive prostate cancer (mHSPC).
LEQEMBI™ (lecanemab-irmb) injection
Nirogacestat (Gamma Secretase Inhibitor)
LEQEMBI™ (lecanemab-irmb) injection
Biologics License Application for Lecanemab Designated for Priority Review by China National Medical Products Administration
FEBRUARY 27, 2023 • NEWS RELEASE
TOKYO and CAMBRIDGE, Mass., Feb. 27, 2023 (GLOBE NEWSWIRE) -- Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, "Eisai") and Biogen Inc. (Nasdaq: BIIB, Corporate headquarters: Cambridge, Massachusetts, CEO: Christopher A. Viehbacher, "Biogen") announced today that the Biologics License Application (BLA) for lecanemab (brand name in the U.S.: LEQEMBI™), an investigational anti-amyloid beta (Aβ) protofibril antibody, has been designated for Priority Review by the National Medical Products Administration (NMPA) in China. The Priority Review and Approval Procedure was implemented by the NMPA with the aim of accelerating research, development and launch of new medicines that have significant clinical value. Under this Procedure, the assessment period is expected to be shortened.
In China, Eisai initiated submission of data for the BLA to the NMPA in December 2022. Eisai initially submitted a package that includes data from the Phase II clinical trial (Study 201) and the top-line data of the large global Phase III Clarity AD study in mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) and mild AD (collectively known as early AD) with confirmed Aβ accumulation in the brain. Eisai will submit additional data including full data of the Clarity AD study, as directed by the NMPA.
Lecanemab selectively binds and eliminates soluble, toxic Aβ aggregates (protofibrils) that are thought to contribute to the neurotoxicity in AD. As such, lecanemab may have the potential to have an effect on disease pathology and to slow down the progression of the disease. The Clarity AD study of lecanemab met its primary endpoint and all key secondary endpoints with highly statistically significant results. In November 2022, the results of the Clarity AD study were presented at the 2022 Clinical Trials on Alzheimer’s Disease (CTAD) conference, and simultaneously published in the New England Journal of Medicine, a peer-reviewed medical journal.
In the U.S., lecanemab was granted accelerated approval by the U.S. Food and Drug Administration (FDA) on January 6, 2023. On the same day, Eisai submitted a supplemental Biologics License Application (sBLA) to the FDA for approval under the traditional pathway. In Europe, Eisai submitted a marketing authorization application (MAA) to the European Medicines Agency (EMA) on January 9, 2023, which was accepted on January 26, 2023. In Japan, Eisai submitted a marketing authorization application to the Pharmaceuticals and Medical Devices Agency (PMDA) on January 16, 2023, and Priority Review was designated by the Ministry of Health, Labour and Welfare (MHLW) on January 26, 2023.
Eisai serves as the lead of lecanemab development and regulatory submissions globally with both Eisai and Biogen co-commercializing and co-promoting the product and Eisai having final decision-making authority.
1. About Priority Review and Approval Procedure in China
The Priority Review and Approval Procedure was implemented by the National Medical Products Administration (NMPA) with the aim of accelerating research, development and launch of new medicines that have significant clinical value. Under this Procedure, the assessment period is expected to be shortened. There are six categories of priority review designations as follows and lecanemab was designated as Category 1: 1) Innovative new drugs and new dosage forms for the prevention and treatment of serious infectious diseases and rare diseases for which there is an urgent clinical need. 2) Drugs with additional indications and new dosage forms that are compatible with the physiological characteristics of children. 3) Vaccines and innovative vaccines that are urgently needed to prevent or control disease. 4) Drugs designated as breakthrough therapies. 5) Medicinal products that are reviewed under the conditional approval procedure. 6) Other drugs designated by NMPA for priority review.
2. About Lecanemab
Lecanemab (Brand Name in the U.S.: LEQEMBI™) is the result of a strategic research alliance between Eisai and BioArctic. Lecanemab is a humanized immunoglobulin gamma 1 (IgG1) monoclonal antibody directed against aggregated soluble (protofibril) and insoluble forms of amyloid-beta (Aβ). In the U.S., LEQEMBI was granted accelerated approval by the U.S. Food and Drug Administration (FDA) on January 6, 2023. LEQEMBI is indicated for the treatment of Alzheimer’s disease (AD) in the U.S. Treatment with LEQEMBI should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was initiated in clinical trials. There are no safety or effectiveness data on initiating treatment at earlier or later stages of the disease than were studied. This indication is approved under accelerated approval based on reduction in Aβ plaques observed in patients treated with LEQEMBI. Continued approval for this indication may be contingent upon verification of clinical benefit in a confirmatory trial.
Please see full Prescribing Information.
Eisai has completed lecanemab subcutaneous bioavailability study, and subcutaneous dosing is currently being evaluated in the Clarity AD (Study 301) OLE.
Since July 2020 the Phase 3 clinical study (AHEAD 3-45) for individuals with preclinical AD, meaning they are clinically normal and have intermediate or elevated levels of amyloid in their brains, is ongoing. AHEAD 3-45 is conducted as a public-private partnership between the Alzheimer’s Clinical Trial Consortium that provides the infrastructure for academic clinical trials in AD and related dementias in the U.S, funded by the National Institute on Aging, part of the National Institutes of Health, Eisai and Biogen.
Since January 2022, the Tau NexGen clinical study for Dominantly Inherited AD (DIAD), that is conducted by Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU), led by Washington University School of Medicine in St. Louis, is ongoing.
3. About the Collaboration between Eisai and Biogen for AD
Eisai and Biogen have been collaborating on the joint development and commercialization of AD treatments since 2014. Eisai serves as the lead of lecanemab development and regulatory submissions globally with both companies co-commercializing and co-promoting the product and Eisai having final decision-making authority.
4. About the Collaboration between Eisai and BioArctic for AD
Since 2005, Eisai and BioArctic have had a long-term collaboration regarding the development and commercialization of AD treatments. Eisai obtained the global rights to study, develop, manufacture and market lecanemab for the treatment of AD pursuant to an agreement with BioArctic in December 2007. The development and commercialization agreement on the antibody lecanemab back-up was signed in May 2015.
5. About Eisai Co., Ltd.
Eisai’s Corporate Concept is “to give first thought to patients and people in the daily living domain, and to increase the benefits that health care provides.” Under this Concept (also known as human health care (hhc) Concept), we aim to effectively achieve social good in the form of relieving anxiety over health and reducing health disparities. With a global network of R&D facilities, manufacturing sites and marketing subsidiaries, we strive to create and deliver innovative products to target diseases with high unmet medical needs, with a particular focus in our strategic areas of Neurology and Oncology.
In addition, we demonstrate our commitment to the elimination of neglected tropical diseases (NTDs), which is a target (3.3) of the United Nations Sustainable Development Goals (SDGs), with working on various activities together with global partners.
For more information about Eisai, please visit www.eisai.com (for global headquarters: Eisai Co., Ltd.), and connect with us on Twitter @Eisai_SDGs.
6. About Biogen
Founded in 1978, Biogen is a leading global biotechnology company that has pioneered multiple breakthrough innovations including a broad portfolio of medicines to treat multiple sclerosis, the first approved treatment for spinal muscular atrophy, and two co-developed treatments to address a defining pathology of Alzheimer’s disease. Biogen is advancing a pipeline of potential novel therapies across neurology, neuropsychiatry, specialized immunology and rare diseases and remains acutely focused on its purpose of serving humanity through science while advancing a healthier, more sustainable and equitable world.
The company routinely posts information that may be important to investors on its website at www.biogen.com. Follow Biogen on social media – Twitter, LinkedIn, Facebook, YouTube.
Biogen, Eisai's Alzheimer's therapy lecanemab gets priority review in Chinna
Feb. 28, 2023 4:32 AM ET
Biogen Inc. (BIIB), ESALFBRCTF
By: Ravikash, SA News Editor
China's National Medical Products Administration (NMPA) granted priority review to Biogen (NASDAQ:BIIB) and Eisai's (OTCPK:ESALF) application seeking approval of Alzheimer's disease (AD) therapy lecanemab.
https://us.eisai.com/eisai_leqembi_now_approved
https://www.leqembi.com/-/media/Files/Leqembi/Prescribing-Information.pdf
Nirogacestat (Gamma Secretase Inhibitor)
Nirogacestat (Gamma Secretase Inhibitor)
Nirogacestat (Gamma Secretase Inhibitor)
SpringWorks Therapeutics Announces FDA Acceptance and Priority Review of New Drug Application for Nirogacestat for the Treatment of Adults with Desmoid Tumors
February 27, 2023PDF Version
– PDUFA Action Date Set for August 27, 2023 –
STAMFORD, Conn., Feb. 27, 2023 (GLOBE NEWSWIRE) -- SpringWorks Therapeutics, Inc. (Nasdaq: SWTX), a clinical-stage biopharmaceutical company focused on developing life-changing medicines for patients with severe rare diseases and cancer, announced today that the U.S. Food and Drug Administration (FDA) has accepted the Company’s New Drug Application (NDA) for nirogacestat, an investigational gamma secretase inhibitor, for the treatment of adults with desmoid tumors. The NDA was granted Priority Review and has been given a Prescription Drug User Fee Act (PDUFA) action date of August 27, 2023. The FDA’s Priority Review designation is given to investigational medicines that treat a serious condition and offer significant improvements in safety or effectiveness. In addition, the FDA has stated that it is not currently planning to hold an advisory committee meeting to discuss the application.
"People with desmoid tumors can experience severe pain and other debilitating morbidities, and we are excited by the opportunity to potentially transform the standard of care for these patients,” said Saqib Islam, Chief Executive Officer of SpringWorks. "The acceptance of our NDA for nirogacestat with Priority Review represents a significant milestone in our ambition to provide the first approved therapy for patients with desmoid tumors. We look forward to working closely with the FDA during the review process and remain focused on ensuring that we are well-positioned to expeditiously serve the desmoid tumor patient and the physician communities following approval."
The NDA is being reviewed under the FDA’s Real-Time Oncology Review (RTOR) program and is based on the previously announced positive results from the Phase 3 DeFi trial, a global, randomized, double-blind, placebo-controlled trial evaluating nirogacestat in adult patients with desmoid tumors. The FDA granted Fast Track and Breakthrough Therapy designations to nirogacestat for the treatment of adult patients with progressive, unresectable, recurrent or refractory desmoid tumors or deep fibromatosis. Nirogacestat has also received Orphan Drug designation from the FDA for the treatment of desmoid tumors.
About the DeFi Trial
DeFi (NCT03785964) is a global, randomized (1:1), double-blind, placebo-controlled Phase 3 trial evaluating the efficacy, safety and tolerability of nirogacestat in adult patients with progressing desmoid tumors. The double-blind phase of the study randomized 142 patients (nirogacestat, n=70; placebo n=72) to receive 150 mg of nirogacestat or placebo twice daily. Key eligibility criteria included tumor progression by ≥20% as measured by Response Evaluation Criteria in Solid Tumors (RECIST 1.1) within 12 months prior to screening. The primary endpoint was progression-free survival, as assessed by blinded independent central review, or death by any cause. Secondary and exploratory endpoints included safety and tolerability measures, objective response rate (ORR), duration of response, changes in tumor volume assessed by magnetic resonance imaging (MRI), and changes in patient-reported outcomes (PROs). DeFi includes an open-label extension phase, which is ongoing.
About Desmoid Tumors
Desmoid tumors are rare, aggressive, locally invasive, and potentially morbid tumors of the soft tissues.1,2 While they do not metastasize, desmoid tumors are associated with a high rate of recurrence.2,3,4 Sometimes referred to as aggressive fibromatosis, or desmoid fibromatosis, these soft tissue tumors can be serious, debilitating, and, in rare cases when vital structures are impacted, they can be life-threatening.2,5
Desmoid tumors are most commonly diagnosed in patients between the ages of 20 and 44 years, with a two-to-three times higher prevalence in females.4,6,7,8 It is estimated that there are 1,000-1,650 new cases diagnosed per year in the United States.7,8,9
Historically, desmoid tumors were treated with surgical resection, but this approach has become less favored due to a high recurrence rate after surgery.1,4,10 There are currently no FDA-approved therapies for the treatment of desmoid tumors.
About Nirogacestat
Nirogacestat is an oral, selective, small molecule gamma secretase inhibitor in Phase 3 clinical development for desmoid tumors and in Phase 2 clinical development for ovarian granulosa cell tumors. Nirogacestat is an investigational drug for which safety and efficacy have not been established.
Gamma secretase cleaves multiple transmembrane protein complexes, including Notch, which is believed to play a role in activating pathways that contribute to growth of desmoid and ovarian granulosa cell tumors. Gamma secretase has also been shown to directly cleave membrane-bound B cell maturation antigen (BCMA), resulting in the release of the BCMA extracellular domain (ECD) from the cell surface. By inhibiting gamma secretase, membrane-bound BCMA can be preserved, increasing target density while reducing levels of soluble BCMA ECD, which may serve as decoy receptors for BCMA-directed therapies. Nirogacestat’s ability to enhance the activity of BCMA-directed therapies has been observed in preclinical models of multiple myeloma. SpringWorks is evaluating nirogacestat as a BCMA potentiator and has several collaborations with industry-leading BCMA developers to evaluate nirogacestat in combinations across modalities. SpringWorks has also formed research collaborations with Fred Hutchinson Cancer Research Center and Dana-Farber Cancer Institute to further characterize the ability of nirogacestat to modulate BCMA and potentiate BCMA-directed therapies using a variety of preclinical multiple myeloma models.
Nirogacestat has received Orphan Drug designation from the U.S. Food and Drug Administration (FDA) for the treatment of desmoid tumors and from the European Commission for the treatment of soft tissue sarcoma. The FDA also granted Fast Track and Breakthrough Therapy designations for the treatment of adult patients with progressive, unresectable, recurrent or refractory desmoid tumors or deep fibromatosis.
About SpringWorks Therapeutics
SpringWorks is a clinical-stage biopharmaceutical company applying a precision medicine approach to acquiring, developing and commercializing life-changing medicines for patients with severe rare diseases and cancer. SpringWorks has a differentiated targeted oncology pipeline spanning solid tumors and hematological cancers, including two late-stage clinical trials in rare tumor types as well as several programs addressing highly prevalent, genetically defined cancers. SpringWorks’ strategic approach and operational excellence in clinical development have enabled it to rapidly advance its two lead product candidates into late-stage clinical trials while simultaneously entering into multiple shared-value partnerships with innovators in industry and academia to unlock the full potential for its portfolio and create more solutions for patients with cancer. For more information, visit www.springworkstx.com and follow @SpringWorksTx on Twitter and LinkedIn.
SpringWorks wins FDA priority review for lead candidate
Feb. 27, 2023 7:33 AM ET
SpringWorks Therapeutics, Inc. (SWTX)
By: Dulan Lokuwithana, SA News Editor
- Clinical-stage biotech SpringWorks Therapeutics (NASDAQ:SWTX) announced Monday that the FDA accepted its New Drug Application (NDA) for lead candidate nirogacestat for priority review as a treatment for adults with soft tissue carcinoma desmoid tumors.
- https://seekingalpha.com/news/3941055-swtx-stock-watch-fda-grants-priority-review-lead-asset
- SpringWorks Therapeutics, Inc. (SWTX)
- https://springworkstx.com/pipeline/nirogacestat/
- https://clinicaltrials.gov/ct2/show/NCT03785964?term=nirogacestat&cond=desmoid+tumor&draw=2&rank=1
- https://springworkstx.com/
Nubeqa® (darolutamide)
Nirogacestat (Gamma Secretase Inhibitor)
Nirogacestat (Gamma Secretase Inhibitor)
2/27/2023
Darolutamide receives approval for additional prostate cancer indication in Japan
Darolutamide receives approval for additional prostate cancer indication in Japan
ORION CORPORATION
PRESS RELEASE
27 February 2023 at 9:00 EET
Darolutamide receives approval for additional prostate cancer indication in Japan
- Darolutamide approved for metastatic prostate cancer as well as non-metastatic castration-resistant prostate cancer
- New approval is based on data from the pivotal Phase III ARASENS trial
The Ministry of Health, Labor and Welfare (MHLW) in Japan has approved the oral androgen receptor inhibitor (ARi) darolutamide plus ADT in combination with docetaxel in the indication of metastatic prostate cancer. The MHLW approval is based on the positive results from the Phase III ARASENS trial, which demonstrated that darolutamide plus androgen deprivation therapy (ADT) in combination with docetaxel significantly reduced the risk of death by 32.5% compared to ADT with docetaxel, in patients with metastatic hormone-sensitive prostate cancer (mHSPC). Additionally, the darolutamide combination showed consistent benefits across clinically relevant secondary endpoints, with the overall incidence of treatment-emergent adverse events being similar between treatment arms. These results were published in The New England Journal of Medicine.1
Darolutamide is already approved in Japan for the treatment of patients with non-metastatic castration-resistant prostate cancer (nmCRPC) under the brand name Nubeqa®.
Darolutamide plus ADT in combination with docetaxel was recently recommended for EU marketing authorisation for the treatment of mHSPC by the European Medicine Agency’s Committee for Medicinal Products for Human Use (CHMP), with a final decision expected in the coming months. The compound is already approved in its second indication, mHSPC, in a number of markets including the U.S. Filings in other regions are underway or planned by Orion’s collaboration partner Bayer.
Darolutamide is being investigated in a broad development program with three additional ongoing or planned large clinical studies, to evauate its potential across prostate cancer patients from the early- to the late-stage of this disease. This includes the ARANOTE Phase III trial evaluating darolutamide plus androgen deprivation therapy (ADT) versus ADT alone for mHSPC.
Darolutamide is developed jointly by Orion and Bayer.
About the ARASENS Trial
The ARASENS trial is a randomized, Phase III, multi-center, double-blind, placebo-controlled trial which was prospectively designed to investigate the efficacy and safety of oral darolutamide, an androgen receptor inhibitor (ARi), plus androgen deprivation therapy (ADT) and the chemotherapy docetaxel in patients with metastatic hormone-sensitive prostate cancer (mHSPC). A total of 1,306 newly diagnosed patients were randomized in a 1:1 ratio to receive 600 mg of darolutamide twice a day or matching placebo, plus ADT and docetaxel.
The primary endpoint of this trial was overall survival (OS). Secondary endpoints included time to castration-resistant prostate cancer (CRPC), time to pain progression, time to first symptomatic skeletal event (SSE), time to initiation of subsequent anticancer therapy, all measured at 12‐week intervals, as well as adverse events (AEs) as a measure of safety and tolerability. Results from this trial were published in the New England Journal of Medicine.1 A plain language summary publication of these data was published in Future Oncology.2 The ARASENS trial demonstrated that darolutamide plus androgen deprivation therapy (ADT) and docetaxel significantly reduced the risk of death by 32.5% compared to ADT plus docetaxel.1 Improvements in the secondary endpoints supported the benefit observed in the primary endpoint, overall survival.1
About Metastatic Hormone-Sensitive Prostate Cancer
Prostate cancer is the second most commonly diagnosed malignancy in men worldwide. In 2020, an estimated 1.4 million men were diagnosed with prostate cancer, and about 375,000 died from the disease worldwide.3
At the time of diagnosis, most men have localized prostate cancer, meaning their cancer is confined to the prostate gland and can be treated with curative surgery or radiotherapy. Upon relapse, when the disease will metastasise or spread, or if the disease is newly diagnosed, but has already spread, the disease is hormone-sensitive and androgen deprivation therapy (ADT) is the cornerstone of treatment for this hormone-sensitive disease. Current treatment options for men with metastatic hormone-sensitive prostate cancer (mHSPC) include hormone therapy, such as ADT, androgen receptor pathway inhibitors plus ADT or a combination of docetaxel chemotherapy and ADT. Despite these treatments, a large proportion of men with mHSPC will eventually experience progression to metastatic castration-resistant prostate cancer (mCRPC), a condition with limited survival.
About darolutamide
Darolutamide is an oral androgen receptor inhibitor (ARi) with a distinct chemical structure that binds to the receptor with high affinity and exhibits strong antagonistic activity, thereby inhibiting the receptor function and the growth of prostate cancer cells. The low potential for blood-brain barrier penetration for darolutamide is supported by preclinical models and neuroimaging data in healthy humans. This is supported by the overall low incidence of central nervous system (CNS)-related adverse events (AEs) compared to placebo as seen in the ARAMIS Phase III trial4 and the maintained verbal learning and memory observed in the darolutamide arm of the Phase II ODENZA trial.5
The product is approved under the brand name Nubeqa® in more than 80 countries around the world, including the U.S., EU, Japan and China, for the treatment of patients with non-metastatic castration-resistant prostate cancer (nmCRPC), who are at high risk of developing metastatic disease. It is also approved for the treatment of patients with metastatic hormone-sensitive prostate cancer (mHSPC) in a number of markets including the U.S. Filings in other regions are underway or planned by Bayer. The compound is also being investigated in further studies across various stages of prostate cancer, including in the ARANOTE Phase III trial evaluating darolutamide plus androgen deprivation therapy (ADT) versus ADT alone for metastatic hormone-sensitive prostate cancer (mHSPC), as well as the Australian and New Zealand Urogenital and Prostate Cancer Trials Group (ANZUP) led international Phase III co-operative group DASL-HiCaP (ANZUP1801) trial evaluating darolutamide as an adjuvant treatment for localised prostate cancer with very high risk of recurrence. Information about these trials can be found at www.clinicaltrials.gov. In addition, a study to explore the potential of darolutamide in the early setting for patients who have experienced a rise in their prostate specific antigen (PSA) levels following surgery or radiation, is also planned.
Orion wins approval for darolutamide in Japan for metastatic prostate cancer
Feb. 27, 2023 6:12 AM ET
Orion Oyj (ORINY), BAYZF, BAYRY
By: Dulan Lokuwithana, SA News Editor
- Finnish pharmaceutical company Orion (OTCPK:ORINY) announced Monday that the government of Japan approved its oral androgen receptor inhibitor darolutamide for metastatic prostate cancer in combination with androgen deprivation therapy (ADT) and docetaxel.
- Darolutamide, which is developed by Orion (OTCPK:ORINY) in partnership with Bayer (OTCPK:BAYZF) (OTCPK:BAYRY), is already approved in Japan as Nubeqa for non-metastatic castration-resistant prostate cancer (nmCRPC).
- Orion Oyj (ORINY), BAYZF, BAYRY
- https://seekingalpha.com/news/3941019-orion-wins-japanese-nod-darolutamide-metastatic-prostate-cancer
- https://www.nubeqa-us.com/
- https://www.orion.fi/en/
biotecHOPE™ 2023
AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone
AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone
AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone
Janssen Receives Positive CHMP Opinion for AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone for the Treatment of Adult Patients with BRCA1/2 Gene-Mutated Metastatic Castration Resistant Prostate Cancer
Feb 24, 2023Belgium
If approved, niraparib in combination with abiraterone acetate (AA), will be the first dual action tablet (DAT) available in the European Union for first-line treatment of adult patients with metastatic castration-resistant prostate cancer (mCRPC) with BRCA1/2 mutations, when given with prednisone (P) or prednisolone.[1]
The positive CHMP opinion is based on results from the Phase 3 MAGNITUDE study where the addition of niraparib to AA plus P significantly improved radiographic progression-free survival (rPFS) compared to standard of care in untreated mCRPC patients with BRCA1/2 mutations.[2]
BEERSE, Belgium, 24 February 2023 – The Janssen Pharmaceutical Companies of Johnson & Johnson announced today that the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) has recommended marketing authorisation for AKEEGA® (niraparib and AA), in the form of a DAT, given with P or prednisolone, for the treatment of adult patients with metastatic castration-resistant prostate cancer (mCRPC) and BRCA1/2 mutations (germline and/or somatic) in whom chemotherapy is not clinically indicated.1
Niraparib is a highly selective poly adenosine diphosphate-ribose polymerase (PARP) inhibitor.2 Together with AA, a cytochrome P450 17α-hydroxylase (CYP17) inhibitor,[3] the combination DAT regimen targets two oncogenic drivers (mutations responsible for both the development and maintenance of prostate cancer) in patients with mCRPC, namely androgen receptor axis (AR-axis) and BRCA1/2 gene mutations.[4],[5]
Prostate cancer is the most common cancer in men in Europe.[6] Despite treatment advances, for those whose cancer has progressed to mCRPC, the impact can be devastating with an average overall survival ranging from 13-36 months.[7],[8],[9] Patients with mCRPC and BRCA gene mutations are more likely to have aggressive disease, poor outcomes and a shorter survival time.[10],[11],[12],[13] BRCA1/2 gene mutations have been identified in approximately 10-15 percent of patients with mCRPC.[14],[15]
“Metastatic castration-resistant prostate cancer remains a lethal disease, with high unmet needs in terms of treatment options, particularly for patients with BRCA1/2 gene mutations,” said Elena Castro*, Consultant Oncologist, Hospital Universitario 12 de Octubre, Instituto de Investigación Sanitaria Hospital 12 de Octubre, Madrid, Spain. “We’ve seen that in these patients, niraparib combined with abiraterone acetate and prednisone significantly reduces the risk of disease progression or death compared to AAP. This niraparib-based regimen is a welcomed targeted treatment option and, if approved, has the potential to impact the standard of care for men with mCRPC BRCA who are treated with first-line therapy.”
“In recent years, we’ve focused on precision medicine in prostate cancer because we know patients with gene mutations, such as BRCA1/2, face a worse prognosis than those without,” said Martin Vogel, EMEA Therapeutic Area Lead Oncology, Janssen-Cilag GmbH. “The positive CHMP opinion reinforces the benefit of this niraparib combination and marks an important milestone in addressing BRCA1/2 mutations as we continue to drive progress towards changing the outlook for patients with mCRPC.”
The positive CHMP opinion is based on results of the randomised, double-blind, placebo controlled, Phase 3 MAGNITUDE study (NCT03748641) which assessed whether the addition of niraparib to AAP improved outcomes in those with first-line mCRPC, with or without alterations in homologous recombination repair (HRR) associated genes.1,16 Patients with HRR gene alterations were randomised to receive niraparib 200 mg once daily plus AAP [n=212], or placebo and AAP [n=211]. In MAGNITUDE, a total of 423 patients with HRR gene alterations were enrolled, 225 (53.2 percent) of whom had BRCA mutations.14 This is the largest cohort of BRCA1/2-positive patients with mCRPC.16 First results, presented at the American Society of Clinical Oncology – Genitourinary Cancers Symposium (ASCO GU) 2022 Annual Meeting,2 showed niraparib plus AAP significantly improved rPFS (as analysed by blinded independent central review) in all HRR-positive patients. This improvement was most pronounced in patients with BRCA1/2 gene mutations, where a statistically significant 47 percent risk reduction was observed for rPFS (HR 0.53; p=0.001).2 Updated results from the second interim analysis (IA2) of MAGNITUDE were presented at the recent ASCO GU 2023 Annual Meeting.[16] In the IA2, at 24.8 months of median follow-up in the BRCA subgroup, rPFS by central review demonstrated a consistent and clinically meaningful treatment effect favouring niraparib plus AAP, with a median rPFS of 19.5 months compared with 10.9 months for placebo plus AAP. Additionally, in the BRCA subgroup, there was a trend towards improved overall survival (OS) with niraparib plus AAP, strong improvement in time to symptomatic progression (TSP) and continued consistent improvement of time-to-initiation of cytotoxic chemotherapy (TCC).16
The observed safety profile of the combination of niraparib and AAP was consistent with the known safety profile of each agent.2 Of the patients with HRR gene alterations, 67 percent experienced Grade 3/4 adverse events (AEs) in the combination arm versus 46.4 percent in the control arm. Discontinuation rates due to AEs for the combination arm and control arm were 10.8 percent and 4.7 percent, respectively. The combination of niraparib and AAP also maintained overall quality of life in comparison with placebo and AAP as measured on the Functional Assessment of Cancer Therapy–Prostate (FACT-P) scale.2
“Prostate cancer is a heterogeneous disease made up of many biologically distinct subpopulations. The data from MAGNITUDE supports the significant value of biomarker testing to identify the subgroup of patients most likely to derive a clinical benefit from a targeted treatment, and overcome the poor prognosis of mCRPC with BRCA mutations,” said Kiran Patel, M.D., Vice President, Clinical Development, Solid Tumors, Janssen Research & Development, LLC. “At Janssen, we are dedicated to continued innovation in prostate cancer and now look forward to working with health authorities to bring this niraparib-based treatment option to patients as soon as possible.”
#ENDS#
About Niraparib
Niraparib is an orally administered, highly selective poly (ADP ribose) polymerase (PARP) inhibitor, that is currently being studied by Janssen for the treatment of patients with prostate cancer.4 Additional ongoing studies include the Phase 3 AMPLITUDE study (NCT04497844) evaluating the combination of niraparib and AAP in a HRR biomarker-selected patient population with metastatic hormone-sensitive prostate cancer (mHSPC).[17]
In April 2016, Janssen Biotech, Inc. entered into a worldwide (except Japan) collaboration and license agreement with TESARO, Inc. (acquired by GSK in 2019), for exclusive rights to niraparib in prostate cancer.[18]
In the EU, niraparib is indicated as monotherapy for the maintenance treatment of adult patients with advanced epithelial high-grade ovarian, fallopian tube, or primary peritoneal cancer who are in a complete or partial response following completion of first-line platinum-based chemotherapy; and as monotherapy for the maintenance treatment of adult patients with platinum-sensitive relapsed high grade serious epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy.5 Niraparib is currently marketed by GSK as ZEJULA®.5
About abiraterone acetate
Abiraterone acetate is an orally administered androgen biosynthesis inhibitor. In the European Union, abiraterone acetate is indicated with prednisone or prednisolone for the treatment of newly diagnosed high risk mHSPC in adult men in combination with androgen deprivation therapy (ADT); the treatment of mCRPC in adult men who are asymptomatic or mildly symptomatic after failure of ADT in whom chemotherapy is not yet clinically indicated; and the treatment of mCRPC in adult men whose disease has progressed on or after a docetaxel-based chemotherapy regimen.3
Abiraterone acetate is currently marketed by Janssen-Cilag International NV as ZYTIGA®.3
About Metastatic Castration-Resistant Prostate Cancer
Metastatic castration-resistant prostate cancer (mCRPC) characterises cancer that no longer responds to ADT and has spread to other parts of the body.[19] The most common metastatic sites are bones, followed by the lymph nodes, liver and lungs.[20] Prostate cancer is the most common cancer in men in Europe.6 In 2020, more than one million men around the world were diagnosed with prostate cancer.[21] Patients with mCRPC and HRR gene alterations, of which BRCA mutations are the most common, are more likely to have aggressive disease, poor outcomes and a shorter survival time.10,11,12,13
About MAGNITUDE
MAGNITUDE (NCT03748641) is a Phase 3 randomised, double-blind, placebo-controlled, multicentre clinical study evaluating the safety and efficacy of the combination of niraparib and AAP for patients with mCRPC, with or without certain HRR gene alterations and who have not received prior therapy for mCRPC except for standard of care, next-generation androgen receptor inhibitors and up to 4 months of AAP.4 The study includes patients with (HRR biomarker [BM] positive; ATM, BRCA1, BRCA2, BRIP1, CDK12, CHEK2, FANCA, HDAC2, PALB2) and without specified gene alterations (HRR BM negative), who were randomised 1:1 to receive niraparib 200 mg once daily plus AAP or placebo plus AAP.4 Additionally in an open-label cohort of HRR-positive patients, all patients received the DAT formulation of niraparib and abiraterone acetate plus prednisone. The primary endpoint of the MAGNITUDE trial is rPFS assessed by blinded independent central review. Secondary endpoints include time-to-initiation of cytotoxic chemotherapy, time to symptomatic progression and overall survival.4
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we're creating a future where disease is a thing of the past. We're the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com/emea/. Follow us at www.twitter.com/JanssenEMEA for our latest news. Janssen Pharmaceutica NV, Janssen-Cilag GmBH and Janssen Research & Development, LLC are part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
*Dr. Castro has served as a consultant to Janssen; she has not been paid for any media work.
Johnson & Johnson wins EU nod for prostate cancer therapy
Feb. 24, 2023 2:12 PM ET
By: Dulan Lokuwithana, SA News Editor2 Comments
Johnson & Johnson's (NYSE:JNJ) Janssen unit announced Friday that a group of experts from the European Medicines Agency (EMA) recommended marketing authorization for its oral PARP inhibitor niraparib as a combination regimen for certain adults with prostate cancer.
With its latest decision, EMA's Committee for Medicinal Products for Human Use (CHMP) recommends niraparib with abiraterone acetate as Akeega for adults with metastatic castration-resistant prostate cancer (mCRPC) and BRCA1/2 mutations.
https://seekingalpha.com/news/3940807-johnson-johnson-wins-eu-nod-for-prostate-cancer-therapy
ALTUVIIIO™ (Efanesoctocog alfa (formerly BIVV001))
AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone
AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone
PRESS RELEASES •
February 23, 2023
Press Release: FDA approves once-weekly ALTUVIIIO™, a new class of factor VIII therapy for hemophilia A that offers significant bleed protection
- Home
- Media
- Press releases
- 2023
- Press Release: FDA approves once-weekly ALTUVIIIO™, a new class of factor VIII therapy for hemophilia A that offers significant bleed protection
FDA approves once-weekly ALTUVIIIO™, a new class of factor VIII therapy for hemophilia A that offers significant bleed protection
Paris and Stockholm – February 23, 2023 – The U.S. Food and Drug Administration (FDA) has approved ALTUVIIIO™ [Antihemophilic Factor (Recombinant), Fc-VWF-XTEN Fusion Protein-ehtl], previously referred to as efanesoctocog alfa, a first-in-class, high-sustained factor VIII replacement therapy. ALTUVIIIO is indicated for routine prophylaxis and on-demand treatment to control bleeding episodes, as well as perioperative management (surgery) for adults and children with hemophilia A. ALTUVIIIO is the first and only hemophilia A treatment that delivers normal to near-normal factor activity levels (over 40%) for most of the week with once-weekly dosing, and significantly reduces bleeds compared to prior factor VIII prophylaxis.
Paul Hudson
CEO, Sanofi
"Today’s approval of ALTUVIIIO allows patients and physicians to reimagine living with hemophilia. The high sustained factor activity levels that can be achieved with ALTUVIIIO have the potential to change the hemophilia landscape. For the first time, with a once-weekly dose, powerful bleed protection is a reality for patients. Significant shifts in treatment paradigms that improve people’s lives, like ALTUVIIIO, are what we have committed to delivering at Sanofi.”
Hemophilia A is a rare, lifelong condition in which the ability of a person’s blood to clot properly is impaired, leading to excessive bleeds and spontaneous bleeds into joints that can result in joint damage and chronic pain, and potentially impact quality of life. The severity of hemophilia is determined by the level of clotting factor activity in a person’s blood, and there is a negative correlation between risk of bleeding and factor activity levels.
Lynn Malec, MD
Medical Director of Comprehensive Center for Bleeding Disorders and Associate Investigator at The Versiti Blood Research Institute, and Associate Professor of Medicine and Pediatrics at The Medical College of Wisconsin
“This approval marks an important clinical advancement for the hemophilia community because we have an option that can achieve higher levels of factor activity with a single simplified weekly dose. By maintaining high levels of factor activity throughout the week, patients can be confident in the bleed protection ALTUVIIIO offers.”
This is the first approval of ALTUVIIIO. The FDA evaluated the application under Priority Review, which is granted to therapies that have the potential to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The FDA previously granted ALTUVIIIO Breakthrough Therapy designation in May 2022 – the first factor VIII therapy to receive this recognition – Fast Track designation in February 2021, and Orphan Drug designation in August 2017.
Regulatory submission in the EU is anticipated in the second half of 2023. The European Commission granted Orphan Drug designation in June 2019.
ALTUVIIIO helps elevate expectations for hemophilia A by providing protection for longer
The FDA approval is based on data from the pivotal XTEND-1 Phase 3 study recently published in The New England Journal of Medicine. Once-weekly ALTUVIIIO prophylaxis met the primary endpoint, providing significant bleed protection for people with severe hemophilia A with a mean annualized bleeding rate (ABR) of 0.70 (95% CI: 0.5-1.0) and a median ABR of 0.0 (Q1, Q3: 0.0, 1.0). ALTUVIIIO met the key secondary endpoint with a significant reduction of 77% in ABR versus prior factor prophylaxis based on an intra-patient comparison (95% CI:58%-87%).
Additional data showed prevention of joint bleeds with a median annualized joint bleeding rate of 0 (Q1, Q3: 0.0, 1.0). Treatment with ALTUVIIIO provided 100% resolution of target joints, which are joints that have recurrent bleeds (e.g., knee, ankle, or elbow). ALTUVIIIO provided mean factor VIII activity greater than 40% for most of the week and greater than 10% at Day 7; these levels were associated with a low bleed risk. In the study, ALTUVIIIO was well-tolerated and inhibitor development to factor VIII was not detected, although is possible following administration of ALTUVIIIO.
Additionally, interim data from XTEND-Kids showed that children younger than 12 years of age receiving once-weekly ALTUVIIIO for 26 weeks (n=23) experienced a mean ABR of 0.5 (95% CI: 0.2-1.3) and a median ABR of 0 (Q1, Q3: 0.0, 1.3). Safety results were consistent with data from the XTEND-1 trial. The full results from XTEND-Kids will be presented at a future medical meeting.
Across the studies, ALTUVIIIO has an established safety profile and there were no reports of factor VIII inhibitor development, although inhibitor formation is possible following administration of ALTUVIIIO. The most common side effects (>10%) of ALTUVIIIO are headache and arthralgia.
ALTUVIIIO is indicated for routine prophylaxis, on-demand treatment and control of bleeding episodes, and perioperative management of bleeding. The simple recommended dose of 50 IU/kg is intended for all patients and for different clinical scenarios.
To ensure that patients have access to the improved bleed protection provided by ALTUVIIIO, Sanofi will price ALTUVIIIO at parity to the annual cost of treating a prophylaxis patient on Eloctate®[Antihemophilic Factor (Recombinant), Fc Fusion Protein]. Sanofi will also provide comprehensive patient support services and resources online and at 1.855.MyALTUVIIIO (855.692.5888). In the U.S., ALTUVIIIO is expected to be commercially available in April.
About ALTUVIIIO™
ALTUVIIIO [Antihemophilic Factor (Recombinant), Fc-VWF-XTEN Fusion Protein-ehtl] is a novel von Willebrand Factor (VWF) independent recombinant factor VIII therapy that is designed to extend protection from bleeds with once-weekly prophylactic dosing for adults and children with hemophilia A. ALTUVIIIO has a 3 to 4 fold longer half-life relative to standard and extended half-life factor VIII products. It is the first factor VIII therapy that has been shown to break through the von Willebrand factor ceiling, which imposes a half-life limitation on earlier generation factor VIII therapies. ALTUVIIIO builds on the innovative Fc fusion technology by adding a region of von Willebrand factor and XTEN® polypeptides to extend its time in circulation.
About the XTEND Clinical Programs
The XTEND clinical program is comprised of two Phase 3 trials in hemophilia A: XTEND-1 in people 12 years or older and XTEND-Kids in children younger than 12 years old. There is also an ongoing extension study (XTEND-ed).
The Phase 3 XTEND-1 study (NCT04161495) was an open-label, non-randomized interventional study assessing the safety, efficacy, and pharmacokinetics of once-weekly ALTUVIIIO in people 12 years of age or older (n=159) with severe hemophilia A who were previously treated with factor VIII replacement therapy. The study consisted of two parallel treatment arms — the prophylaxis Arm A (n=133), in which patients who had received prior factor VIII prophylaxis were treated with once-weekly intravenous ALTUVIIIO prophylaxis (50 IU/kg) for 52 weeks, and the on-demand Arm B (n=26), in which patients who had received prior on-demand factor VIII therapy began with 26 weeks of on-demand ALTUVIIIO (50 IU/kg), then switched to once-weekly prophylaxis with ALTUVIIIO (50 IU/kg) for an additional 26 weeks.
The primary efficacy endpoint was the mean annualized bleeding rate (ABR) in Arm A, and the key secondary endpoint was an intra-patient comparison of ABR during the ALTUVIIIO weekly prophylaxis treatment period versus the prior factor VIII prophylaxis ABR for a subset of participants in Arm A who had participated in a previous observational study (Study 242HA201/OBS16221).
The XTEND-Kids study (NCT04759131) was an open-label, non-randomized interventional study of the safety, efficacy, and pharmacokinetics of once-weekly ALTUVIIIO in previously treated patients younger than 12 years of age (n=67) with severe hemophilia A. Patients received once-weekly ALTUVIIIO prophylaxis (50 IU/kg) for 52 weeks.
About the Sanofi and Sobi collaboration
Sobi and Sanofi collaborate on the development and commercialization of Alprolix® and Elocta®/Eloctate®. The companies also collaborate on the development and commercialization of efanesoctocog alfa or ALTUVIIIO™ in the US. Sobi has final development and commercialization rights in the Sobi territory (essentially Europe, North Africa, Russia and most Middle Eastern markets). Sanofi has final development and commercialization rights in North America and all other regions in the world excluding the Sobi territory.
About Sobi®
Sobi is a specialized international biopharmaceutical company transforming the lives of people with rare diseases. Providing sustainable access to innovative medicines in the areas of haematology, immunology and specialty care, Sobi has approximately 1,600 employees across Europe, North America, the Middle East and Asia. In 2022, revenue amounted to SEK 18.8 billion. Sobi’s share (STO:SOBI) is listed on Nasdaq Stockholm. More about Sobi at sobi.com, LinkedIn and YouTube.
About Sanofi
We are an innovative global healthcare company, driven by one purpose: we chase the miracles of science to improve people’s lives. Our team, across some 100 countries, is dedicated to transforming the practice of medicine by working to turn the impossible into the possible. We provide potentially life-changing treatment options and life-saving vaccine protection to millions of people globally, while putting sustainability and social responsibility at the center of our ambitions.
Sanofi is listed on EURONEXT: SAN and NASDAQ: SNY
Sanofi wins FDA nod for once-weekly bleeding disorder therapy
Feb. 24, 2023 5:46 AM ET
Sanofi (SNY), SNYNF, BIOVFRHHBY, NVO, BAYRY, BAYZF, NONOF, RHHBF, TAK
By: Dulan Lokuwithana, SA News Editor
- The FDA has greenlighted factor replacement therapy Altuviiio from Sanofi (NASDAQ:SNY) (OTCPK:SNYNF) as a once-weekly treatment for adults and children with an inherited bleeding disorder called hemophilia A, the French drugmaker announced.
- Specifically, the agency has approved Altuviiio for routine prophylaxis and on-demand treatment to control bleeding episodes and for the surgical management of hemophilia A patients.
- With the approval, Sanofi (SNY) and Swedish drug maker Sobi (OTCPK:BIOVF), its partner for U.S. commercialization of Altuviiio, will compete against Roche (OTCQX:RHHBY) (OTCQX:RHHBF), which markets its blockbuster hemophilia A therapy Hemlibra.
- https://seekingalpha.com/news/3940532-sanofi-wins-fda-nod-once-weekly-bleeding-disorder-therapy
- Sanofi (SNY), SNYNF, BIOVF
- https://www.sanofi.com/en/
- https://www.sobi.com/en
MRNA-4157/V940 -MRNA CANCER VACCINE, IN COMBINATION WITH KEYTRUDA(R) (PEMBROLIZUMAB)
AKEEGA® (Niraparib and Abiraterone Acetate Dual Action Tablet) Plus Prednisone or Prednisolone
MRNA-4157/V940 -MRNA CANCER VACCINE, IN COMBINATION WITH KEYTRUDA(R) (PEMBROLIZUMAB)
MODERNA AND MERCK ANNOUNCE MRNA-4157/V940, AN INVESTIGATIONAL PERSONALIZED MRNA CANCER VACCINE, IN COMBINATION WITH KEYTRUDA(R) (PEMBROLIZUMAB), WAS GRANTED BREAKTHROUGH THERAPY DESIGNATION BY THE FDA FOR ADJUVANT TREATMENT OF PATIENTS WITH HIGH-RISK MELANOMA FOLLOWING COMPLETE RESECTION
FEBRUARY, 22, 2023 DOWNLOAD(OPENS IN NEW WINDOW)
Designation based on positive data from Phase 2b KEYNOTE-942/mRNA-4157-P201 trial
CAMBRIDGE, MA and RAHWAY, NJ / ACCESSWIRE / February 22, 2023 / Moderna, Inc. (NASDAQ:MRNA), a biotechnology company pioneering messenger RNA (mRNA) therapeutics and vaccines, and Merck (NYSE:MRK), known as MSD outside of the United States and Canada, today announced that mRNA-4157/V940, an investigational personalized mRNA cancer vaccine, in combination with KEYTRUDA, Merck's anti-PD-1 therapy, has been granted Breakthrough Therapy Designation by the U.S. Food and Drug Administration (FDA) for the adjuvant treatment of patients with high-risk melanoma following complete resection. The FDA granted Breakthrough Therapy Designation based on positive data from the Phase 2b KEYNOTE-942/mRNA-4157-P201 trial.
"The FDA's Breakthrough Designation for mRNA-4157/V940 in combination with KEYTRUDA reflects the excitement that we have for the potential promise of individualized cancer treatments," said Stephen Hoge, M.D., Moderna's President. "mRNA-4157/V940 in combination with KEYTRUDA provided the first demonstration of efficacy for an investigational mRNA cancer treatment in a randomized clinical trial and potentially represents a new frontier in treating melanoma and other cancers. We look forward to publishing the full data set and sharing the results at an upcoming oncology medical conference, as well as continuing discussions with health authorities. We are grateful to the FDA for this designation."
"This is an important milestone in the development of mRNA-4157/V940 in combination with KEYTRUDA," said Dr. Eric H. Rubin, senior vice president, global clinical development, Merck Research Laboratories. "We look forward to working with the FDA, in collaboration with Moderna, to conduct a rigorous and rapid clinical development program with a focus on addressing the needs of this important patient population."
The FDA's Breakthrough Therapy Designation is granted to expedite the development and review of drugs that are intended to treat a serious condition, and when preliminary clinical evidence indicates that the product may demonstrate substantial improvement over available therapies on at least one clinically significant endpoint.[i]
The companies will continue to discuss the results with regulatory authorities, initiate a Phase 3 study in adjuvant melanoma in 2023, and rapidly expand to additional tumor types, including non-small cell lung cancer.
About mRNA-4157/V940
mRNA-4157/V940 is a novel investigational messenger ribonucleic acid (mRNA)-based personalized cancer vaccine consisting of a single synthetic mRNA coding for up to 34 neoantigens that is designed and produced based on the unique mutational signature of the patient's tumor. Upon administration into the body, the algorithmically derived and mRNA-encoded neoantigen sequences are endogenously translated and undergo natural cellular antigen processing and presentation, a key step in adaptive immunity.
Personalized cancer vaccines are designed to prime the immune system so that a patient can generate a tailored antitumor response specific to their tumor mutation signature. mRNA-4157/V940 is designed to stimulate an immune response by generating specific T cell responses based on the unique mutational signature of a patient's tumor. KEYTRUDA is an immunotherapy that works by increasing the ability of the body's immune system to help detect and fight tumor cells. Based on early clinical studies, combining mRNA-4157/V940 with KEYTRUDA may potentially provide an additive benefit and enhance T cell-mediated destruction of tumor cells.
About KEYNOTE-942/mRNA-4157-P201 ( NCT03897881 )
KEYNOTE-942 is an ongoing randomized, open-label Phase 2b trial that enrolled 157 patients with stage III/IV melanoma. Following complete surgical resection, patients were randomized to receive mRNA-4157/V940 (nine total doses of mRNA-4157) and KEYTRUDA (200 mg every three weeks up to 18 cycles [for approximately one year]) versus KEYTRUDA alone for approximately one year until disease recurrence or unacceptable toxicity. The primary endpoint is recurrence-free survival, and secondary endpoints include distant metastasis-free survival and safety.
Key eligibility criteria for the trial included: patients with resectable cutaneous melanoma at high risk of recurrence, patients with complete resection within 13 weeks prior to the first dose of KEYTRUDA, patients were disease free at study entry (after surgery) with no loco-regional relapse or distant metastasis and no clinical evidence of brain metastases.
About Melanoma
Melanoma, the most serious form of skin cancer, is characterized by the uncontrolled growth of pigment-producing cells. The rates of melanoma have been rising over the past few decades, with nearly 325,000 new cases diagnosed worldwide in 2020. In the U.S., skin cancer is one of the most common types of cancer diagnosed, and melanoma accounts for a large majority of skin cancer deaths. Each year, it is estimated there will be nearly 100,000 new cases of melanoma diagnosed and almost 8,000 deaths resulting from the disease in the U.S. The five-year survival rates are estimated to be 60.3% for stage III and 16.2% for stage IV.
About KEYTRUDA® (pembrolizumab) injection, 100 mg
KEYTRUDA is an anti-programmed death receptor-1 (PD-1) therapy that works by increasing the ability of the body's immune system to help detect and fight tumor cells. KEYTRUDA is a humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD-L1 and PD-L2, thereby activating T lymphocytes which may affect both tumor cells and healthy cells.
Merck has the industry's largest immuno-oncology clinical research program. There are currently more than 1,600 trials studying KEYTRUDA across a wide variety of cancers and treatment settings. The KEYTRUDA clinical program seeks to understand the role of KEYTRUDA across cancers and the factors that may predict a patient's likelihood of benefitting from treatment with KEYTRUDA, including exploring several different biomarkers.
Selected KEYTRUDA® (pembrolizumab) Indications in the U.S
Melanoma
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic melanoma.
KEYTRUDA is indicated for the adjuvant treatment of adult and pediatric (12 years and older) patients with stage IIB, IIC, or III melanoma following complete resection.
Non-Small Cell Lung Cancer
KEYTRUDA, in combination with pemetrexed and platinum chemotherapy, is indicated for the first-line treatment of patients with metastatic nonsquamous non-small cell lung cancer (NSCLC), with no EGFR or ALK genomic tumor aberrations.
KEYTRUDA, in combination with carboplatin and either paclitaxel or paclitaxel protein-bound, is indicated for the first-line treatment of patients with metastatic squamous NSCLC.
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with NSCLC expressing PD-L1 [tumor proportion score (TPS) ≥1%] as determined by an FDA-approved test, with no EGFR or ALK genomic tumor aberrations, and is:
- stage III where patients are not candidates for surgical resection or definitive chemoradiation, or
- metastatic.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with metastatic NSCLC whose tumors express PD-L1 (TPS ≥1%) as determined by an FDA-approved test, with disease progression on or after platinum-containing chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving KEYTRUDA.
KEYTRUDA, as a single agent, is indicated as adjuvant treatment following resection and platinum-based chemotherapy for adult patients with Stage IB (T2a ≥4 cm), II, or IIIA NSCLC.
Head and Neck Squamous Cell Cancer
KEYTRUDA, in combination with platinum and fluorouracil (FU), is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent head and neck squamous cell carcinoma (HNSCC).
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent HNSCC whose tumors express PD-L1 [Combined Positive Score (CPS) ≥1] as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic HNSCC with disease progression on or after platinum-containing chemotherapy.
Classical Hodgkin Lymphoma
KEYTRUDA is indicated for the treatment of adult patients with relapsed or refractory classical Hodgkin lymphoma (cHL).
KEYTRUDA is indicated for the treatment of pediatric patients with refractory cHL, or cHL that has relapsed after 2 or more lines of therapy.
Primary Mediastinal Large B-Cell Lymphoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after 2 or more prior lines of therapy.
KEYTRUDA is not recommended for treatment of patients with PMBCL who require urgent cytoreductive therapy.
Urothelial Carcinoma
KEYTRUDA is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma (mUC):
- who are not eligible for any platinum-containing chemotherapy, or
- who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
Non-muscle Invasive Bladder Cancer
KEYTRUDA is indicated for the treatment of patients with Bacillus Calmette-Guerin-unresponsive, high-risk, non-muscle invasive bladder cancer (NMIBC) with carcinoma in situ with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy.
Microsatellite Instability-High or Mismatch Repair Deficient Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. The safety and effectiveness of KEYTRUDA in pediatric patients with MSI-H central nervous system cancers have not been established.
Microsatellite Instability-High or Mismatch Repair Deficient Colorectal Cancer
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic MSI-H or dMMR colorectal cancer (CRC) as determined by an FDA-approved test.
Gastric Cancer
KEYTRUDA, in combination with trastuzumab, fluoropyrimidine- and platinum-containing chemotherapy, is indicated for the first-line treatment of patients with locally advanced unresectable or metastatic HER2-positive gastric or gastroesophageal junction (GEJ) adenocarcinoma.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Esophageal Cancer
KEYTRUDA is indicated for the treatment of patients with locally advanced or metastatic esophageal or gastroesophageal junction (GEJ) (tumors with epicenter 1 to 5 centimeters above the GEJ) carcinoma that is not amenable to surgical resection or definitive chemoradiation either:
- in combination with platinum- and fluoropyrimidine-based chemotherapy, or
- as a single agent after one or more prior lines of systemic therapy for patients with tumors of squamous cell histology that express PD-L1 (CPS ≥10) as determined by an FDA-approved test.
Cervical Cancer
KEYTRUDA, in combination with chemotherapy, with or without bevacizumab, is indicated for the treatment of patients with persistent, recurrent, or metastatic cervical cancer whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic cervical cancer with disease progression on or after chemotherapy whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
Hepatocellular Carcinoma
KEYTRUDA is indicated for the treatment of patients with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Merkel Cell Carcinoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with recurrent locally advanced or metastatic Merkel cell carcinoma (MCC). This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Renal Cell Carcinoma
KEYTRUDA, in combination with axitinib, is indicated for the first-line treatment of adult patients with advanced renal cell carcinoma (RCC).
KEYTRUDA is indicated for the adjuvant treatment of patients with RCC at intermediate-high or high risk of recurrence following nephrectomy, or following nephrectomy and resection of metastatic lesions.
Endometrial Carcinoma
KEYTRUDA, as a single agent, is indicated for the treatment of patients with advanced endometrial carcinoma that is MSI-H or dMMR, as determined by an FDA-approved test, who have disease progression following prior systemic therapy in any setting and are not candidates for curative surgery or radiation.
Tumor Mutational Burden-High Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥10 mutations/megabase] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. The safety and effectiveness of KEYTRUDA in pediatric patients with TMB-H central nervous system cancers have not been established.
Cutaneous Squamous Cell Carcinoma
KEYTRUDA is indicated for the treatment of patients with recurrent or metastatic cutaneous squamous cell carcinoma (cSCC) or locally advanced cSCC that is not curable by surgery or radiation.
Triple-Negative Breast Cancer
KEYTRUDA is indicated for the treatment of patients with high-risk early-stage triple-negative breast cancer (TNBC) in combination with chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
KEYTRUDA, in combination with chemotherapy, is indicated for the treatment of patients with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1 (CPS ≥10) as determined by an FDA-approved test.
Pediatric Use
In KEYNOTE-051, 161 pediatric patients (62 pediatric patients aged 6 months to younger than 12 years and 99 pediatric patients aged 12 years to 17 years) were administered KEYTRUDA 2 mg/kg every 3 weeks. The median duration of exposure was 2.1 months (range: 1 day to 24 months).
Adverse reactions that occurred at a ≥10% higher rate in pediatric patients when compared to adults were pyrexia (33%), vomiting (30%), leukopenia (30%), upper respiratory tract infection (29%), neutropenia (26%), headache (25%), and Grade 3 anemia (17%).
Please see Prescribing Information for KEYTRUDA (pembrolizumab) at http://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf and Medication Guide for KEYTRUDA at http://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_mg.pdf .
Merck's Focus on Cancer
Our goal is to translate breakthrough science into innovative oncology medicines to help people with cancer worldwide. At Merck, the potential to bring new hope to people with cancer drives our purpose and supporting accessibility to our cancer medicines is our commitment. As part of our focus on cancer, Merck is committed to exploring the potential of immuno-oncology with one of the largest development programs in the industry across more than 30 tumor types. We also continue to strengthen our portfolio through strategic acquisitions and are prioritizing the development of several promising oncology candidates with the potential to improve the treatment of advanced cancers. For more information about our oncology clinical trials, visit www.merck.com/clinicaltrials.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world - and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on Twitter, Facebook, Instagram, YouTube and LinkedIn.
About Moderna
In over 10 years since its inception, Moderna has transformed from a research-stage company advancing programs in the field of messenger RNA (mRNA), to an enterprise with a diverse clinical portfolio of vaccines and therapeutics across seven modalities, a broad intellectual property portfolio in areas including mRNA and lipid nanoparticle formulation, and an integrated manufacturing plant that allows for rapid clinical and commercial production at scale. Moderna maintains alliances with a broad range of domestic and overseas government and commercial collaborators, which has allowed for the pursuit of both groundbreaking science and rapid scaling of manufacturing. Most recently, Moderna's capabilities have come together to allow the authorized use and approval of one of the earliest and most effective vaccines against the COVID-19 pandemic.
Moderna's mRNA platform builds on continuous advances in basic and applied mRNA science, delivery technology and manufacturing, and has allowed the development of therapeutics and vaccines for infectious diseases, immuno-oncology, rare diseases, cardiovascular diseases and auto-immune diseases. Moderna has been named a top biopharmaceutical employer by Science for the past eight years. To learn more, visit www.modernatx.com.
[i] U.S. Food and Drug Administration (FDA). Breakthrough Therapy. https://www.fda.gov/forpatients/approvals/fast/ucm405397.htm. Updated January 4, 2018. Accessed January 26, 2023.
SOURCE: Moderna, Inc.
View source version on accesswire.com:
https://www.accesswire.com/740413/Moderna-and-Merck-Announce-mRNA-4157V940-an-Investigational-Personalized-mRNA-Cancer-Vaccine-in-Combination-With-KEYTRUDAR-pembrolizumab-was-Granted-Breakthrough-Therapy-Designation-by-the-FDA-for-Adjuvant-Treatment-of-Patients-With-High-Risk
Moderna, Merck's mRNA cancer vaccine/Keytruda combo gets FDA breakthrough therapy tag
Feb. 23, 2023 5:51 AM ET
By: Ravikash, SA News Editor1 Comment
- The U.S. Food and Drug Administration (FDA) granted breakthrough therapy designation to Moderna (NASDAQ:MRNA) and Merck's (NYSE:MRK) personalized mRNA cancer vaccine mRNA-4157/V940, in combination with Keytruda, for the adjuvant treatment of patients with high-risk melanoma after complete resection.
- https://seekingalpha.com/news/3939727-moderna-mercks-mrna-cancer-vaccinekeytruda-combo-gets-fda-breakthrough-therapy-tag
- Merck & Co., Inc. (MRK), MRNA
RGX-121
Sunlenca® (lenacapavir)
MRNA-4157/V940 -MRNA CANCER VACCINE, IN COMBINATION WITH KEYTRUDA(R) (PEMBROLIZUMAB)
ADDITIONAL POSITIVE INTERIM DATA FROM PHASE I/II/III CAMPSIITE™ TRIAL OF REGENXBIO'S RGX-121 FOR THE TREATMENT OF MPS II (HUNTER SYNDROME) PRESENTED AT 19TH ANNUAL WORLDSYMPOSIUMTM
February 22, 2023 at 3:00 PM EST
- RGX-121, a potential one-time gene therapy for the treatment of MPS II, continues to be well-tolerated with no drug-related SAEs across three dose levels
- Additional data from patients in Cohort 3 using pivotal program dose level continue to demonstrate largest reductions in CSF GAGs, continuing to approach normal levels at 48 weeks
- New, longer-term clinical measures demonstrated continued improvement in neurodevelopmental and daily activity skill acquisition up to three years after RGX-121 administration
- Positive interim data continues to support plan to file Biologics License Application in 2024 using the accelerated approval pathway
ROCKVILLE, Md., Feb. 22, 2023 /PRNewswire/ -- REGENXBIO Inc. (Nasdaq: RGNX) today announced additional positive interim data from the Phase I/II/III CAMPSIITE™ trial of RGX-121 for the treatment of patients up to 5 years old diagnosed with Mucopolysaccharidosis Type II (MPS II), also known as Hunter Syndrome. The results were presented at the 19th Annual WORLDSymposium™.
"These new results demonstrate sustained reductions in CSF GAGs and an encouraging, long-term clinical profile of RGX-121 up to three years," said Steve Pakola, M.D., Chief Medical Officer of REGENXBIO. "GAGs measured in CSF, specifically heparan sulfate, reflect disease manifestations in the CNS and are a direct cause of disease pathophysiology. Our data provide additional evidence to support the finding that meaningful changes in CSF heparan sulfate is an appropriate and reliable surrogate endpoint reasonably likely to predict the clinical benefit of CNS-targeted therapies for MPS II. We are excited to have taken RGX-121 into a pivotal program and plan to file a Biologics License Application in 2024 using the accelerated approval pathway."
"Treatment options to address the neurological manifestations of MPS II remain a significant unmet medical need for patients," said Can Ficicioglu, M.D., Ph.D., Professor of Pediatrics at the Perelman School of Medicine, University of Pennsylvania. "The data presented today are encouraging and continue to show the potential of a one- time gene therapy to provide meaningful, durable clinical benefits to the MPS II community. I look forward to continuing to follow RGX-121 as it progresses through the pivotal program."
RGX-121 is an investigational, one-time gene therapy designed to deliver the gene that encodes the iduronate-2-sulfatase (I2S) enzyme using the AAV9 vector. Data presented were from the Phase I/II portion of the CAMPSIITE trial in which the primary endpoint is to evaluate the safety of RGX-121. Secondary and exploratory endpoints include cerebral spinal fluid (CSF) glycosaminoglycans (GAGs), neurodevelopmental assessments, caregiver reported outcomes and systemic biomarkers. RGX-121 is administered directly to the central nervous system (CNS). As of January 3, 2023, 15 patients had been treated across three dose levels, 1.3x1010 genome copies per gram (GC/g) of brain mass (n=3), 6.5x1010 GC/g of brain mass (n=7), and 2.9x1011 GC/g of brain mass (n=5).
Data Summary and Safety Update
As of January 3, 2023, RGX-121 was reported to be well tolerated across all cohorts with no drug-related serious adverse events (SAEs) in 15 patients dosed. Time of post-administration follow-up ranges from eight weeks to more than three years. Thirteen patients have completed the 48-week immunosuppression regimen per study protocol. Twelve patients were receiving weekly, intravenous enzyme replacement therapy (ERT) at the time of enrollment, per standard of care; five of these patients remain discontinued from ERT at last time point available, per investigator discretion, as allowed in the protocol.
CSF GAGs Data
Biomarker data from patients in all three cohorts indicate encouraging, dose-dependent reductions of CSF GAGs following one-time administration of RGX-121. Heparan sulfate (HS) and D2S6, a component of HS closely correlated with severe MPS II, are GAGs that are key biomarkers of I2S enzyme activity and are being measured in the CSF at baseline and after administration of RGX-121. CSF GAGs have the potential to be considered a surrogate endpoint that is reasonably likely to predict clinical benefit in MPS II disease under the accelerated approval pathway, as buildup of GAGs in the CSF of MPS II patients correlates with clinical manifestations including neurodevelopmental deficits.
The majority of patients in all cohorts demonstrated reductions of CSF HS from baseline at the last time point available with dose-dependent reductions seen at Weeks 8, 24, and 48 post RGX-121 administration. At Week 48, median reduction of CSF HS from baseline was 33.5% in Cohort 1, 48.9% in Cohort 2 and 64.7% in Cohort 3.
Similarly, dose-dependent reductions of CSF HS D2S6 from baseline were observed at last time point available in the majority of patients, with Cohort 3 patients approaching normal levels at 48 weeks. All three cohorts demonstrated a reduction in HS D2S6 with dose-dependent reductions seen at Weeks 8, 24, and 48. Median reductions from baseline of 31.9% in Cohort 1, 71.9% in Cohort 2 and 83.3% in Cohort 3 were seen at Week 48.
In addition, I2S protein concentration in the CSF, which was undetectable in all patients prior to dosing, was measurable in 10 of 11 Cohort 2 and 3 patients after RGX-121 administration.
Neurodevelopmental and Systemic Data
Improvements in neurodevelopmental function and caregiver reported outcomes demonstrated CNS activity on two developmental scales up to three years after RGX-121 administration. As measured by the Bayley Scales of Infant and Toddler Development, 3rd Edition (BSID-III), the majority of participants with baseline function ≥-2 standard deviations (SD) from the normative mean had developmental function that remained within that range on at least two domains. The majority of participants with baseline function below -2SD from the normative mean stabilized or had an increase of ≥ 3 months in age equivalent scores on cognitive, expressive language or fine motor subtests. As measured by the Vineland Adaptive Behavior Scales Second Edition (VABS-II), the majority of participants demonstrated stabilization or ongoing skill acquisition on age-appropriate subtests of communication, daily living and socialization.
Additionally, evidence of systemic enzyme expression and biomarker activity was observed in all cohorts following RGX-121 administration. The majority of patients demonstrated increases in I2S protein concentration levels in plasma following administration of RGX-121. Total urine GAG measures demonstrated evidence of a systemic effect of RGX-121, independent of ERT treatment.
The study findings presented at the 2023 WORLDSymposium will be available under the Presentations & Publications page in the Media section of REGENXBIO's website located at www.regenxbio.com. Dr. Ficicioglu will share this data in a platform presentation at the WORLDSymposium Sunday, February 26, 2023, at 9 a.m. ET.
About the CAMPSIITE™ Trial
CAMPSIITE is a Phase I/II/III multicenter, open-label trial enrolling boys with MPS II, aged four months up to five years of age. As part of a pivotal program expansion, CAMPSIITE is expected to enroll up to 10 MPS II patients to support the BLA filing using the accelerated approval pathway, with the potential to enroll additional patients. These patients will receive a dose of 2.9x1011 GC/g of brain mass of RGX-121, which is the same dose being evaluated in Cohort 3 of the Phase I/II trial. The pivotal program is using commercial-scale cGMP material from REGENXBIO's proprietary, high-yielding suspension-based manufacturing process, named NAVXpress™. In addition to measuring GAGs in the CSF, the trial will continue to collect neurodevelopmental data and caregiver-reported outcomes.
CAMPSIITE is a global trial, which is expected to include sites in the United States, Brazil and Canada. REGENXBIO has begun dosing patients in the pivotal program.
About RGX-121
RGX-121 is designed to use the AAV9 vector to deliver the human iduronate-2-sulfatase gene (IDS) which encodes the iduronate-2-sulfatase (I2S) enzyme to the central nervous system (CNS). Delivery of the IDS gene within cells in the CNS could provide a permanent source of secreted I2S beyond the blood-brain barrier, allowing for long-term cross correction of cells throughout the CNS. RGX-121 has received orphan drug product, rare pediatric disease and Fast Track designations from the U.S. Food and Drug Administration.
About Mucopolysaccharidosis Type II (MPS II)
MPS II, or Hunter Syndrome, is a rare, X-linked recessive disease caused by a deficiency in the lysosomal enzyme iduronate-2-sulfatase (I2S) leading to an accumulation of glycosaminoglycans (GAGs), including heparan sulfate (HS) in tissues which ultimately results in cell, tissue, and organ dysfunction, including in the central nervous system (CNS). MPS II is estimated to occur in 1 in 100,000 to 170,000 births. In severe forms of the disease, early developmental milestones may be met, but developmental delay is readily apparent by 18 to 24 months. Specific treatment to address the neurological manifestations of MPS II remains a significant unmet medical need. Key biomarkers of I2S enzymatic activity in MPS II patients include its substrate heparan sulfate (HS) D2S6, which has been shown to correlate with neurocognitive manifestations of the disorder.
About REGENXBIO Inc.
REGENXBIO is a leading clinical-stage biotechnology company seeking to improve lives through the curative potential of gene therapy. REGENXBIO's NAV Technology Platform, a proprietary adeno-associated virus (AAV) gene delivery platform, consists of exclusive rights to more than 100 novel AAV vectors, including AAV7, AAV8, AAV9 and AAVrh10. REGENXBIO and its third-party NAV Technology Platform Licensees are applying the NAV Technology Platform in the development of a broad pipeline of candidates, including late-stage and commercial programs, in multiple therapeutic areas. REGENXBIO is committed to a "5x'25" strategy to progress five AAV Therapeutics from our internal pipeline and licensed programs into pivotal-stage or commercial products by 2025.

View original content to download multimedia:https://www.prnewswire.com/news-releases/additional-positive-interim-data-from-phase-iiiiii-campsiite-trial-of-regenxbios-rgx-121-for-the-treatment-of-mps-ii-hunter-syndrome-presented-at-19th-annual-worldsymposiumtm-301753564.html
SOURCE REGENXBIO Inc.
Regenxbio touts interim results from trial of pediatric rare disease gene therapy
Feb. 22, 2023 3:35 PM ET
By: Jonathan Block, SA News Editor
- Regenxbio said that interim results of RGX-121, a gene therapy for the rare pediatric inherited condition Mucopolysaccharidosis Type II (MPS II), also known as Hunter Syndrome, were positive.
- https://seekingalpha.com/news/3939376-regenxbio-touts-interim-results-from-trial-of-pediatric-rare-disease-gene-therapy
- REGENXBIO Inc. (RGNX)
- https://regenxbio.com/
- https://regenxbio.com/rgx-121/
Sunlenca® (lenacapavir)
Sunlenca® (lenacapavir)
Sunlenca® (lenacapavir)
February 22, 2023
Gilead Presents Positive Proof-of-Concept Data for Investigational Combination Regimen of Lenacapavir with Broadly Neutralizing Antibodies as a Potential Twice-Yearly Approach for the Treatment of HIV
– Study Demonstrates the Potential of Lenacapavir in Combination with Broadly Neutralizing HIV Antibodies Teropavimab and Zinlirvimab –
– Findings Support Further Evaluation of the Investigational Combination as a Long-Acting HIV Treatment Option in a Phase 2 Study –
FOSTER CITY, Calif.--(BUSINESS WIRE)-- Gilead Sciences, Inc. (Nasdaq: GILD) today announced data evaluating lenacapavir in combination with broadly neutralizing antibodies (bNAbs) teropavimab and zinlirvimab as a potential long-acting treatment regimen with twice-yearly dosing.Results fromthe Phase 1b clinical trial demonstrated the investigational combination was generally well tolerated with high efficacy in select virologically suppressed participants living with HIV. These data were presented at the 30th Conference on Retroviruses and Opportunistic Infections (CROI).
“Novel long-acting HIV treatment options will drive the next chapter in care and may help meet the therapy needs and preferences of people living with HIV. In this study we found that lenacapavir and bNAbs in a combination approach may have a significant role to play in the future treatment of HIV,” said Dr. Joseph Eron, MD, lead study investigator and the Chief of the Division of Infectious Diseases at the University of North Carolina School of Medicine. “As a clinician who strives to support the people living with the virus under my care, it will be exciting to continue evaluating the combination regimen as a potential twice-yearly long-acting HIV treatment option.”
The study evaluated the safety and efficacy profile of lenacapavir + teropavimab + zinlirvimab in selected adults living with HIV who were virologically suppressed (HIV-1 RNA <50 copies/mL) for ≥2 years while taking antiretroviral therapy (ART). Study participants (n=20) were sensitive to both bNAbs by HIV proviral DNA phenotype and had a CD4 cell count of ≥500 at study entry. The median age was 44 years (14% female, 14% Black, 14% Asian, and 33% Hispanic/Latinx).
Doses of teropavimab and zinlirvimab were weight-based, with participants randomly allocated in a 1:1 ratio into two active treatment groups replacing their baseline ART with lenacapavir (927mg subcutaneous after oral loading) + teropavimab (30mg/kg body weight intravenous) + zinlirvimab (Group 1: 10mg/kg body weight; Group 2: 30mg/kg body weight, both intravenous).
At Week 26, 90% of participants receiving the complete study regimen (n=18/20) maintained virologic suppression (HIV-1 RNA ≤50 copies/mL). At Week 12, one participant withdrew from the study with documented viral suppression (HIV-1 RNA <50 copies/mL). At Week 16, one participant had a confirmed virologic rebound and later resuppressed on baseline oral ART. There were no serious adverse events (AEs), including no grade 4 or 5 AEs, and no AEs that led to study drug discontinuation. Two participants experienced grade 3 AEs with one experiencing injection site cellulitis and the other experiencing injection site erythema.
“We’re excited to share these promising results that reinforce lenacapavir’s potential to be a foundational agent for long-acting combination HIV treatment options, and we are especially pleased to see the potential of the combination of lenacapavir plus bNAbs dosed once every six months,” said Jared Baeten, MD, PhD, Vice President, HIV Clinical Development, Gilead Sciences. “We are committed to exploring novel therapy approaches that may help deliver care for all people living with HIV, with a focus on developing person-centric options that fit into the diverse lives of people living with the virus, as we continue in our pursuit of ending the HIV epidemic for everyone, everywhere.”
The combination of lenacapavir with teropavimab and zinlirvimab will advance to a Phase 2 study (NCT05729568) later this year in virologically suppressed people living with HIV. The study will assess two different dose levels of the bNAbs and assess safety and efficacy of the regimen in participants followed longitudinally for multiple doses of the study regimen. For more information, please visit: https://clinicaltrials.gov/ct2/show/NCT05729568
Lenacapavir is being developed as a foundation for future HIV therapies with the goal of offering both long-acting oral and injectable options with several dosing frequencies, in combination with other antiretroviral agents for treatment or as monotherapy for prevention, that help address individual patient needs and preferences. Lenacapavir is being evaluated as a long-acting option in multiple ongoing and planned early and late-stage clinical studies in Gilead's prevention and treatment research program.
Sunlenca® (lenacapavir), alone or in combination, is not approved by any regulatory authority outside of the United States, United Kingdom, Canada or the European Union for any use.
Please see below for the U.S. Indication and Important Safety Information for Sunlenca.
Teropavimab (GS-5423) and zinlirvimab (GS-2872) are investigational compounds and are not approved by the U.S. Food and Drug Administration or any other regulatory authority for any use. The use of these compounds in combination with lenacapavir are investigational. Their safety and efficacy are unknown.
There is currently no cure for HIV or AIDS.
About Sunlenca
Sunlenca (300 mg tablet and 463.5 mg/1.5 mL injection) [(lenacapavir)] is a first-in-class, long-acting HIV capsid inhibitor approved in the United States, the United Kingdom, Canada and the European Union, for the treatment of HIV infection, in combination with other antiretroviral(s), in people with multi-drug resistant HIV who are heavily treatment-experienced. Sunlenca tablets are approved for oral loading during initiation of Sunlenca treatment, prior to or at the time of the first long-acting lenacapavir injection depending on initiation option. Sunlenca is the only HIV treatment option administered twice-yearly.
The multi-stage mechanism of action of Sunlenca’s active pharmaceutical agent, lenacapavir, is distinguishable from other currently approved classes of antiviral agents. While most antivirals act on just one stage of viral replication, Sunlenca is designed to inhibit HIV at multiple stages of its lifecycle and has no known cross resistance exhibited in vitro to other existing drug classes.
U.S. Indication for Sunlenca
Sunlenca, a human immunodeficiency virus type 1 (HIV-1) capsid inhibitor, in combination with other antiretroviral(s), is indicated for the treatment of HIV-1 infection in heavily treatment-experienced adults with multidrug resistant HIV-1 infection failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations.
About Gilead Sciences
Gilead Sciences, Inc. is a biopharmaceutical company that has pursued and achieved breakthroughs in medicine for more than three decades, with the goal of creating a healthier world for all people. The company is committed to advancing innovative medicines to prevent and treat life-threatening diseases and address unmet needs in virology, oncology and inflammation.
For 35 years, Gilead has been a leading innovator in the field of HIV, driving advances in treatment, prevention and cure research. Gilead researchers have developed 12 HIV medications, including the first single-tablet regimen to treat HIV, the first antiretroviral for pre-exposure prophylaxis (PrEP) to reduce the risk of acquiring HIV infection, and the first long-acting injectable HIV treatment medication administered twice-yearly. Our advances in medical research have helped to transform HIV into a treatable, preventable, chronic condition for millions of people.
Gilead is committed to continued scientific innovation to provide solutions for the evolving needs of people affected by HIV around the world. Through partnerships and collaborations, the company also aims to improve education, expand access and address barriers to care, with the goal of ending the HIV epidemic for everyone, everywhere. Gilead was recognized as the number one philanthropic funder of HIV-related programs in a report released by Funders Concerned About AIDS.
Gilead operates in more than 35 countries worldwide, with headquarters in Foster City, California.
U.S. full Prescribing Information for Sunlenca is available at www.gilead.com .
Sunlenca, Gilead and the Gilead logo are registered trademarks of Gilead Sciences, Inc., or its related companies. All other trademarks are the property of their respective owner(s).
For more information about Gilead, please visit the company’s website at www.gilead.com , follow Gilead on Twitter ( @Gilead Sciences ) and LinkedIn , or call Gilead Public Affairs at 1-800-GILEAD-5 or 1-650-574-3000.
Source: Gilead Sciences, Inc.
Gilead posts Phase 1 data to support twice yearly potential of HIV therapy
Feb. 22, 2023 12:05 PM ET
By: Dulan Lokuwithana, SA News Editor
Gilead Sciences (NASDAQ:GILD) announced Phase 1 data for its HIV antiviral lenacapavir on Wednesday to support its twice-yearly use along with investigational HIV antibodies Teropavimab and Zinlirvimab.
https://seekingalpha.com/news/3939164-gilead-posts-data-support-twice-yearly-potential-hiv-therapy
Elranatamab
Sunlenca® (lenacapavir)
Sunlenca® (lenacapavir)
Pfizer’s Elranatamab Receives FDA and EMA Filing Acceptance
Wednesday, February 22, 2023 - 06:45am
- Submissions based on favorable MagnetisMM-3 trial results in patients with relapsed or refractory multiple myeloma
NEW YORK--(BUSINESS WIRE)-- Pfizer Inc. (NYSE:PFE) announced today that the U.S. Food and Drug Administration (FDA) has granted Priority Review for the company’s Biologics License Application (BLA) for elranatamab, an investigational B-cell maturation antigen (BCMA) CD3-targeted bispecific antibody (BsAb), for the treatment of patients with relapsed or refractory multiple myeloma (RRMM). Priority Review is intended to direct attention and resources from regulatory authorities toward drugs that, if approved, could offer significant improvements over existing options for serious conditions in order to make these drugs available to patients faster. The FDA’s decision on the application is expected in 2023. The European Medicines Agency (EMA) has also accepted elranatamab’s marketing authorization application (MAA). The company is working closely with the EMA to facilitate their review and will provide updates on timing as appropriate.
"Today, multiple myeloma is a fatal hematologic malignancy, with a median survival of just over five years. As an off-the-shelf treatment, BCMA bispecific antibodies are heralding a new treatment paradigm that can greatly impact the lives of people with this disease.” said Chris Boshoff, M.D., Ph.D., Chief Development Officer, Oncology and Rare Disease, Pfizer Global Product Development. “We believe that elranatamab, if approved, has the potential to become the next standard of care for multiple myeloma given its favorable clinical results and convenient subcutaneous route of administration. We look forward to working with the FDA and EMA to bring this new innovative medicine to patients globally.”
Elranatamab is designed to bind to BCMA, which is highly expressed on the surface of multiple myeloma (MM) cells, and CD3 receptors found on the surface of T-cells, bridging them together and activating the T-cells to kill the myeloma cells. The BLA and MAA for elranatamab are primarily based on data from cohort A (BCMA-naïve - n=123) of MagnetisMM-3 (NCT04649359), an ongoing, open-label, multicenter, single-arm, Phase 2 study designed to evaluate the safety and efficacy of elranatamab monotherapy in patients with RRMM. Enrolled patients represent a heavily pretreated population, who previously received at least three classes of therapies, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
With a median follow up of 10.4 months, patients who received elranatamab as their first BCMA-targeted therapy achieved a high objective response rate of 61% (55% had a very good partial response rate or better), with an 84% probability of maintaining the response at nine months. The MagnetisMM-3 results also suggest elranatamab has a manageable safety profile. The two-step-up priming dose regimen (12/32 mg) helped mitigate the rate and severity of cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) among the 119 patients in cohort A who were treated with this priming regimen. All cases of CRS were Grade 1 or 2 and the majority occurred after the first (43% of patients) or second (24% of patients) dose, with only 6% of patients experiencing CRS after dose 3 and fewer than 1% experiencing CRS after dose 4. Observed cases of ICANS (3%) were neither common nor severe (Grade 1/2 only were reported). No fatal neurotoxicity events were observed. These data were presented at the 64th American Society of Hematology Annual Meeting and Exposition in December 2022.
This study is part of the MagnetisMM clinical research program that expands to additional patient populations over time, with ongoing registrational-intent trials that explore elranatamab both as monotherapy and in combination with standard or novel therapies, spanning multiple patient populations, from newly diagnosed MM to RRMM. This includes MagnetisMM-5 (NCT05020236) in the double class exposed setting, MagnetisMM-6 (NCT05623020) in transplant ineligible newly diagnosed patients, and MagnetisMM-7 (NCT05317416) as maintenance treatment in newly diagnosed patients after transplant, all of which are currently enrolling.
In November 2022, Pfizer announced that elranatamab was granted Breakthrough Therapy Designation by the FDA. In addition, elranatamab has been granted Orphan Drug Designation by the FDA and the EMA for the treatment of MM. The FDA and EMA have also granted elranatamab Fast Track Designation and the PRIME scheme, respectively, for the treatment of patients with RRMM. The UK Medicines and Healthcare Products Regulatory Agency (MHRA) has granted elranatamab Innovative Medicine Designation and the Innovation Passport for the treatment of MM. The FDA has accepted elranatamab for Project ORBIS, which is a framework for the concurrent submission and review of oncology products to potentially expedite approvals in certain countries outside of the US; currently 5 countries (Switzerland, Brazil, Canada, Australia, and Singapore) have accepted to participate.
About Elranatamab
Elranatamab is an investigational, off-the-shelf, humanized BCMA CD3-targeted BsAb. BsAbs are a novel form of cancer immunotherapy that bind to and engage two different targets at once. One arm binds directly to specific antigens on cancer cells and the other arm binds to T-cells, bringing both cell types together. The binding affinity of elranatamab for BCMA and CD3 has been engineered to elicit potent T-cell-mediated anti-myeloma activity. Elranatamab is administered subcutaneously, which offers more convenience over intravenous administration.
About MagnetisMM-3
MagnetisMM-3 (NCT04649359) is an ongoing, open-label, multicenter, single-arm, Phase 2 study designed to evaluate the safety and efficacy of elranatamab monotherapy in patients with RRMM. Patients received subcutaneous (SC) elranatamab 76 mg weekly (QW) on a 28-day cycle with a step-up priming dose regimen, wherein 12 mg and 32 mg are administered on Day 1 and Day 4, respectively, during Cycle 1. For patients receiving 6 or more cycles and achieving a partial response or better for at least 2 months, the dosing interval was once every two weeks (Q2W).
About Multiple Myeloma
MM is a blood cancer that affects plasma cells made in the bone marrow. Healthy plasma cells make antibodies that help the body fight infection. There are over 34,000 new cases of MM diagnosed annually in the U.S. and 176,000 globally.1,2 Despite treatment advances, there is currently no cure. The median survival is just over five years, and most patients receive four or more lines of therapy.3
About Pfizer in Hematology
At Pfizer, we have an industry-leading portfolio of 24 approved innovative cancer medicines and biosimilars, including seven therapies to treat hematologic malignancies. We have taken bold new approaches over the past decade to translate scientific research into transformative medicines for people living with blood cancer. For the millions living with blood cancer today and for those diagnosed tomorrow, we work tirelessly to deliver on our mission: Breakthroughs that change patients’ lives.
About Pfizer: Breakthroughs That Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world’s premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.Pfizer.com. In addition, to learn more, please visit us on www.Pfizer.com and follow us on Twitter at @Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230222005105/en/
Source: Pfizer Inc.
Pfizer's blood cancer drug elranatamab gets review in US, EU
Feb. 22, 2023 7:20 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted priority review to Pfizer's (NYSE:PFE) application seeking approval of elranatamab to treat patients with relapsed or refractory multiple myeloma (RRMM).
- https://seekingalpha.com/news/3938950-pfizers-blood-cancer-drug-elranatamab-gets-review-in-us-eu
- Pfizer Inc. (PFE)
- https://www.pfizer.com/science/drug-product-pipeline
Taldefgrobep alfa (also known as BHV2000)
(RSV) vaccine candidate PF-06928316 or RSVpreF
(RSV) vaccine candidate PF-06928316 or RSVpreF
FEBRUARY 21, 2023 AT 7:30 AM EST
Biohaven's Taldefgrobep Alfa Receives FDA Fast Track Designation for Spinal Muscular Atrophy
- Taldefgrobep alfa, a myostatin-targeting biologic investigational agent, in Phase 3 development to increase muscle mass for Spinal Muscular Atrophy patients now granted Fast Track in addition to previously receiving Orphan Drug Designation in the US
NEW HAVEN, Conn., Feb. 21, 2023 /PRNewswire/ -- Biohaven Ltd. (NYSE: BHVN; "Biohaven") announced today that it received Fast Track designation from the U.S. Food and Drug Administration (FDA) for taldefgrobep alfa, a novel anti-myostatin adnectin, for the treatment of spinal muscular atrophy (SMA). Fast Track designation enables important new drugs to reach patients earlier by facilitating more frequent communications with the FDA and expeditious review of a drug which treats a serious condition and fills an unmet medical need. Biohaven previously received orphan drug designation from the FDA for taldefgrobep in the treatment of SMA.
SMA is a rare, progressively debilitating motor neuron disease in which development and growth of muscle mass are compromised, resulting in progressive weakness and muscle atrophy, reduced motor function, impaired quality of life and often death. Inhibition of myostatin, a naturally occurring protein that limits skeletal muscle growth, an important process in healthy muscular development, is a potential therapeutic target for SMA.
Taldefgrobep has the potential to be a novel therapy to be used in combination with disease modifying therapies to enhance muscle function by blocking myostatin activity. Taldefgrobep's novelty in a field of myostatin inhibitors is based on its mechanism of action. It binds to myostatin to both lower overall myostatin levels and also function as a receptor antagonist, thereby blocking myostatin signaling in skeletal muscles.
Lindsey Lee Lair, M.D., M.B.A., F.A.A.N, Vice President, Clinical Development, Biohaven commented, "We are very pleased the FDA granted Fast Track designation for taldefgrobep alfa for the treatment of SMA. Children and adults living with SMA experience significant muscle weakness and functional impairments affecting their quality of life daily, and a substantial unmet medical need persists. We are excited about the potential for taldefgrobep alfa to improve the lives of patients and families affected by SMA."
Karen Chen, Ph.D., CEO, SMA Foundation, added, "Fast Track designation from the FDA underscores the high unmet medical need in SMA and supports the need for additional novel combination therapies in children and adults living with this progressive neurologic disease. The SMA Foundation is heavily investing in supporting the development of additional muscle and neuromuscular regenerative medicine therapies that provide functional benefits to patients. We are happy to see the commitment of health authorities to rapidly advance the development of new therapies"
As a leader in innovative trials addressing neurodegenerative diseases, Biohaven is currently enrolling a Phase 3 clinical trial of taldefgrobep in SMA: A Study to Evaluate the Efficacy and Safety of Taldefgrobep Alfa in Participants with Spinal Muscular Atrophy (RESILIENT) (NCT05337553).
About Taldefgrobep alfa
Taldefgrobep alfa (also known as BHV2000) is a modified adnectin designed to specifically bind to myostatin (GDF-8). Taldefgrobep is a fully human anti-myostatin recombinant protein that lowers free myostatin and acts as an Activin 2b receptor antagonist with the myostatin-taldefgrobep complex. Adnectins are an established proprietary protein therapeutic class based on human fibronectin, an extracellular protein that is naturally abundant in human serum.
About Biohaven
Biohaven is a global clinical-stage biopharmaceutical company focused on the discovery, development and commercialization of life-changing therapies for people with debilitating neurological and neuropsychiatric diseases, including rare disorders. The company is advancing a pipeline of therapies for diseases with little or no treatment options, leveraging its proven drug development capabilities and proprietary platforms, including Kv7 ion channel modulation for epilepsy and neuronal hyperexcitability; glutamate modulation for obsessive-compulsive disorder and spinocerebellar ataxia and myostatin inhibition for neuromuscular diseases. Biohaven's portfolio of early- and late-stage product candidates also includes discovery research programs focused on TRPM3 channel activation for neuropathic pain, CD-38 antibody recruiting, bispecific molecules for multiple myeloma, antibody drug conjugates (ADCs), and extracellular target degrader platform technology (MoDE™) with potential application in neurological disorders, cancer, and autoimmune diseases.
View original content to download multimedia:https://www.prnewswire.com/news-releases/biohavens-taldefgrobep-alfa-receives-fda-fast-track-designation-for-spinal-muscular-atrophy-301751239.html
SOURCE BIOHAVEN LTD
Biohaven's spinal muscular atrophy therapy gets FDA fast track status
Feb. 21, 2023 9:10 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted fast track designation to Biohaven (NYSE:BHVN) medicine taldefgrobep alfa to treat spinal muscular atrophy (SMA).
- https://seekingalpha.com/news/3938384-biohavens-spinal-muscular-atrophy-therapy-gets-fda-fast-track-status
- Biohaven Ltd. (BHVN)
- https://www.biohaven.com/
(RSV) vaccine candidate PF-06928316 or RSVpreF
(RSV) vaccine candidate PF-06928316 or RSVpreF
(RSV) vaccine candidate PF-06928316 or RSVpreF
U.S. FDA Accepts Biologics License Application for Pfizer’s Respiratory Syncytial Virus Maternal Vaccine Candidate for Priority Review
Tuesday, February 21, 2023 - 06:45am
- U.S. FDA has set an action date for August 2023. If approved, RSVpreFwould be the first vaccine for administration to pregnant individuals to help protect against the complications of RSV disease in infants from birth through six months
- This action follows the recent acceptance of the Marketing Authorization Application (MAA) for Pfizer’s RSV vaccine candidate by the European Medicines Agency (EMA) under accelerated assessment for both older adults and maternal immunization
- The maternal immunization regulatory filings are supported by results of the pivotal Phase 3 trial MATISSE, which will be presented to the CDC’s Advisory Committee on Immunization Practices (ACIP), as well as during the ReSViNET Foundation’s 2023 Global Conference, on February 23
NEW YORK--(BUSINESS WIRE)-- Pfizer Inc. (NYSE:PFE) today announced that the U.S. Food and Drug Administration (FDA) has accepted for review a Biologics License Application (BLA) for its respiratory syncytial virus (RSV) vaccine candidate PF-06928316 or RSVpreF for the prevention of medically attended lower respiratory tract illness (MA-LRTI) and severe MA-LRTI caused by RSV in infants from birth up to six months of age by active immunization of pregnant individuals. This decision follows the FDA’s Breakthrough Therapy Designation for RSVpreF in March 2022. The FDA has accepted the BLA for priority review and has set a Prescription Drug User Fee Act (PDUFA) action date of August 2023.
“If approved, RSVpreF would help protect infants at their first breath from the devastating effects of this infectious disease, which though well-known, has been particularly evident throughout this RSV season,” said Annaliesa Anderson, Ph.D., Senior Vice President and Chief Scientific Officer, Vaccine Research & Development, Pfizer. “We look forward to progressing the review of Pfizer’s RSV maternal vaccine candidate with the FDA and other regulatory authorities, given its significant potential to positively contribute to global health in the prevention of RSV in infants.”
In addition, the European Medicines Agency (EMA) has accepted Pfizer’s marketing authorization application (MAA) under accelerated assessment for its RSV vaccine candidate for both older adults and maternal immunization to help protect infants. A decision is expected in the second half of 2023.
The maternal immunization regulatory submission is supported by the positive top-line results from MATISSE (MATernal Immunization Study for Safety and Efficacy), a Phase 3 clinical trial evaluating the efficacy, safety, and immunogenicity of RSVpreF against MA-LRTI and severe MA-LRTI in infants born to healthy women vaccinated during pregnancy. These data will be presented on February 23 to the U.S. Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP) and, separately, during the ReSViNET Foundation’s 2023 Global Conference on Novel RSV Preventive and Therapeutic Interventions.
Additional ACIP Presentations
During the ACIP meeting on February 22-23, the company also will present positive Phase 3 results supporting the regulatory filings of Pfizer’s pentavalent meningococcal vaccine (MenABCWY) candidate, as well as Pfizer’s 20-valent pneumococcal conjugate vaccine (20vPnC) candidate for pediatric use.
In December 2022, Pfizer announced that the FDA had accepted for review a BLA for its MenABCWY candidate for the prevention of meningococcal disease caused by the most common serogroups in individuals 10 through 25 years of age. The PDUFA goal date for a decision by the FDA on the MenABCWY application is in October 2023. If approved and recommended, MenABCWY could help simplify the meningococcal vaccination schedule and provide the broadest serogroup coverage of any meningococcal vaccine. Top-line results from a randomized, active-controlled, and observer-blinded Phase 3 trial of Pfizer’s pentavalent meningococcal vaccine candidate (NCT04440163) were previously announced in September 2022.
Similarly, in January 2023, Pfizer announced that the FDA had granted priority review to a supplemental BLA for its 20vPnC candidate for the prevention of invasive pneumococcal disease (IPD) caused by the 20 Streptococcus pneumoniae (pneumococcus) serotypes contained in the vaccine in infants and children 6 weeks through 17 years of age, and for the prevention of otitis media caused by seven of the 20 Streptococcus pneumoniae serotypes contained in the vaccine. The PDUFA goal date for the FDA’s decision on the 20vPnC application is in April 2023. If approved, 20vPnC would have the potential to cover more of the clinically significant remaining burden of infant pneumococcal disease than any other available pneumococcal conjugate vaccine. In August 2022 Pfizer announced top-line results from its pivotal U.S. Phase 3 study (NCT04382326), which support the FDA application.
Burden of RSV
RSV is a contagious virus and a common cause of respiratory illness.1 The virus can affect the lungs and breathing passages of an infected individual and can potentially cause severe illness in young infants, older adults, and individuals with certain chronic medical conditions.2,3,4
Among children younger than five years old in the U.S., RSV infections account for approximately 2.1 million outpatient visits and 58,000 hospitalizations each year.5,6 Virtually all children get an RSV infection by the time they are 2 years old7, and RSV is a leading cause of hospitalization in children <1 year of age.8 Worldwide, RSV results in the death of approximately 102,000 children annually, with about half of those in infants less than six months old and the vast majority in developing countries.9,10
RSV bronchiolitis is the leading cause of infant hospitalization due to viral respiratory illness, characterized by respiratory distress that can result in death. There is no specific treatment for RSV, only supportive care measures like oxygen and fluids. Currently, there is no vaccine to help prevent RSV in the U.S., leaving most infants without protection. The only available preventive agent is recommended for use among the highest-risk infants in limited settings as a monthly injection with five doses administered during the RSV season.
Among adults 65 years and older, RSV infections account for approximately 60,000–160,000 hospitalizations and 6,000–10,000 deaths each year in the U.S. alone.11,12,13,14,15,16,17,18 There are currently no targeted prophylactic, therapeutic, or vaccine options for RSV in older adults, and treatment is limited to offering supportive care for adults with the illness.
About RSVpreF
Pfizer’s investigational RSV vaccine candidate builds on foundational basic science discoveries including those made at the National Institutes of Health (NIH), which detailed the crystal structure of prefusion F, a key form of the viral fusion protein (F) that RSV uses to enter human cells. The NIH research showed that antibodies specific to the prefusion form were highly effective at blocking virus infection, suggesting a prefusion F-based vaccine may confer optimal protection against RSV. After this important discovery, Pfizer tested numerous versions of a stabilized prefusion F protein and identified a candidate that elicited a strong anti-viral immune response in pre-clinical evaluations. The bivalent vaccine candidate is composed of equal amounts of recombinant RSV prefusion F from subgroups A and B.
Pfizer is currently the only company with a maternal RSV vaccine candidate in late-stage development to help protect against RSV. In December 2022, Pfizer announced that the FDA had granted priority review to a biologics license application for RSVpreF for the prevention of RSV disease in older adults.
About the Pentavalent Meningococcal Vaccine Candidate (MenABCWY)
Pfizer’s pentavalent meningococcal vaccine candidate combines the components from its two licensed meningococcal vaccines, Trumenba® (meningococcal group B vaccine) and Nimenrix® (meningococcal groups A, C, W-135, and Y conjugate vaccine); approvals of Nimenrix® and Trumenba® vary by country. Together, the 5 serogroups included in MenABCWY are responsible for the majority of currently circulating meningococcal disease globally.19
INDICATIONS FOR TRUMENBA® IN THE U.S.
- Trumenba® is a vaccine indicated for individuals 10 through 25 years of age for active immunization to prevent invasive disease caused by Neisseria meningitidis group B
INDICATION FOR NIMENRIX® IN THE E.U.
- Nimenrix® is a vaccine indicated for individuals six weeks of age and older for active immunization to prevent invasive disease caused by Neisseria meningitidis groups A, C, W-135 and Y
View source version on businesswire.com: https://www.businesswire.com/news/home/20230221005199/en/
Source: Pfizer Inc.
Pfizer wins priority review for maternal RSV vaccine candidate
Feb. 21, 2023 8:52 AM ET
By: Dulan Lokuwithana, SA News Editor2 Comments
Pfizer (NYSE:PFE) announced Tuesday that the FDA accepted its Biologics License Application (BLA) for its respiratory syncytial virus (RSV) vaccine candidate PF-06928316 for priority review targeting pregnant women for the prevention of RSV in infants.
Beyfortus (nirsevimab)
(RSV) vaccine candidate PF-06928316 or RSVpreF
VLA1553 (Chikungunya Vaccine )
ReSViNet 2023 data reinforce AstraZeneca’s commitment to help prevent Respiratory Syncytial Virus in infants
PUBLISHED21 February 2023
21 February 2023 07:00 GMT
Beyfortus continues to demonstrate consistent protection against
RSV disease through the RSV season
New Canadian analysis demonstrates Synagis to be highly cost-effective in
29-35 weeks gestational age infants
AstraZeneca will showcase new data across its Vaccines and Immune Therapies Respiratory Syncytial Virus (RSV) portfolio at the 7th Respiratory Syncytial Virus Foundation (ReSViNET) Conference in Lisbon, Portugal from 22-24 February 2023, reinforcing its commitment to help protect infants from RSV. The Company is set to present five abstracts and posters at the event, including new data featuring Beyfortus (nirsevimab) and Synagis (palivizumab).
Iskra Reic, Executive Vice President, Vaccines and Immune Therapies, AstraZeneca, said: “I am proud of AstraZeneca’s commitment to respiratory syncytial virus (RSV) and our continued focus on innovating antibodies to provide protection to the most vulnerable. We believe that Beyfortus has the potential to transform the medical community’s approach to preventing RSV infections in infants, and this is of particular importance given the recent surges of the virus amongst infants this past winter season.”
Underscoring the continued need for RSV protection
AstraZeneca is working with the global clinical community to advance the understanding of RSV and is partnering with the ReSViNET Foundation to create the first global RSV surveillance dashboard set to launch in March 2023. RSV is a highly contagious virus that causes respiratory illness in infants, including lung infections such as bronchiolitis and pneumonia.1 This seasonal respiratory virus is the most common cause of lower respiratory tract infections and a leading cause of hospitalisation in infants.1-5
Dr. Louis Bont, Pediatrician Infectologist at the Wilhelmina Children’s Hospital in the University Medical Center Utrecht, The Netherlands, and the founder and chairman of ReSViNET, said: “The ReSViNET Foundation’s new dashboard will make it easier and more accessible to track worldwide changes in RSV seasonality, helping clinicians to protect babies and prevent the rise in hospitalisations that RSV can cause.”
Pursuing a breakthrough for broad RSV prevention
AstraZeneca is presenting the safety and efficacy findings from the full cohort of the Phase III MELODY clinical trial investigating Beyfortus in healthy late preterm and term infants (35 weeks gestational age or greater) entering their first RSV season. These data reinforce Beyfortus’ consistent efficacy across endpoints and studies with approximately 70-80% efficacy against medically attended RSV lower respiratory tract infections vs placebo, including hospitalisations.6-10
New cost effectiveness data for high-risk infant protection
Synagis continues to build on 25 years of real-world usage with a new cost effectiveness analysis being presented at ReSViNet. This analysis is the first to incorporate the International Risk Scoring Tool, which helps clinicians identify pre-term infants with the highest risk of hospitalisation.
RSV
RSV is the most common cause of lower respiratory infections, including bronchiolitis and pneumonia in infants.1 It is also a leading cause of hospitalisation in all infants.1-5 Globally, in 2019, there were approximately 33 million cases of acute lower respiratory infections leading to more than three million hospitalisations, and it was estimated that there were 26,300 in-hospital deaths of children younger than five years.11 RSV-related direct medical costs, globally – including hospital, outpatient and follow-up care – were estimated at €4.82 billion in 2017.12
Beyfortus (nirsevimab)
Beyfortus is a single dose long-acting antibody, developed and commercialised in partnership by AstraZeneca and Sanofi using AstraZeneca’s YTE technology. It is designed to protect infants entering or during their first RSV season and for children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season.
Beyfortus has been developed to offer newborns and infants direct RSV protection via an antibody to help prevent LRTI caused by RSV. Monoclonal antibodies do not require the activation of the immune system to help offer timely, rapid and direct protection against disease.14
Beyfortus has been granted regulatory and other designations to facilitate expedited development by several major regulatory agencies around the world. These include Breakthrough Therapy Designation by the China Center for Drug Evaluation under the National Medical Products Administration; Breakthrough Therapy Designation from the US Food and Drug Administration; access granted to the European Medicines Agency (EMA) PRIority Medicines (PRIME) scheme; and named “a medicine for prioritized development” under the Project for Drug Selection to Promote New Drug Development in Pediatrics by the Japan Agency for Medical Research and Development (AMED). In November 2022, Beyfortus was approved by the European Commission and by the UK Medicines and Healthcare products Regulatory Agency (MHRA).15-16
Sanofi Alliance
In March 2017, AstraZeneca and Sanofi announced an agreement to develop and commercialise nirsevimab. Under the terms of the agreement, AstraZeneca leads all development and manufacturing activities, and Sanofi leads commercialisation activities and records revenue. Under the terms of the global agreement, Sanofi made an upfront payment of €120m, has paid a development milestone of €30m and will pay up to a further €465m upon achievement of certain development and sales-related milestones. The two companies share costs and profits. Revenue from the agreement is reported as Collaboration Revenue in the Company’s financial statements.
Sobi agreement
Related, in November 2018, AstraZeneca agreed to sell US commercial rights for Synagis (palivizumab) to Swedish Orphan Biovitrum AB (publ) (Sobi) in addition to the right to participate in payments that may be received by AstraZeneca from the US profits or losses for nirsevimab. Under the agreement, AstraZeneca received upfront consideration, non-contingent payments for nirsevimab during 2019-2021, and following the FDA’s acceptance of the Biologics License Application (BLA) filing for nirsevimab, will receive a $175m cash payment. AstraZeneca is also entitled to receive certain other milestone payments for nirsevimab, including a $90m cash payment following the date on which BLA approval in the US occurs. AstraZeneca will continue to manufacture and supply nirsevimab globally and is entitled to an additional royalty from Sobi if profits from nirsevimab in the US exceed a pre-specified level.
Synagis (palivizumab)
Synagis (palivizumab) is an RSV F protein inhibitor monoclonal antibody indicated for the prevention of serious lower respiratory tract disease caused by RSV in paediatric patients with a history of premature birth (less than or equal to 35 weeks gestational age) and who are 6 months of age or younger at the beginning of the RSV season, with bronchopulmonary dysplasia (BPD) that required medical treatment within the previous 6 months and who are 24 months of age or younger at the beginning of the RSV season, or with hemodynamically significant congenital heart disease (CHD) and who are 24 months of age or younger at the beginning of the RSV season.13
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca, Sanofi's RSV therapy Beyfortus for infants shows 'consistent protection' in trial
Feb. 21, 2023 5:01 AM ET
Swedish Orphan Biovitrum AB (publ) (BIOVF), SNY, AZN
By: Ravikash, SA News Editor
AstraZeneca (NASDAQ:AZN) and Sanofi's (NASDAQ:SNY) antibody therapy Beyfortus continues to show consistent protection against Respiratory Syncytial Virus (RSV) disease through the RSV season in infants, the British drugmaker said on Tuesday.
Swedish Orphan Biovitrum AB (publ) (BIOVF), SNY, AZN
VLA1553 (Chikungunya Vaccine )
VLA1553 (Chikungunya Vaccine )
VLA1553 (Chikungunya Vaccine )
FDA Accepts Valneva’s Chikungunya Vaccine License Application for Priority Review
February 20, 2023
Saint-Herblain (France),
February 20, 2023 –
Valneva SE (Nasdaq: VALN; Euronext Paris: VLA), a specialty vaccine company, today announced that the U.S. Food and Drug Administration (FDA) has completed a filing review of its Biologics License Application for Valneva’s single-shot chikungunya vaccine candidate VLA1553 and has determined that the application is sufficiently complete to permit a substantive review. The review classification is Priority.
VLA1553 has been assigned a Prescription Drug User Fee Act (PDUFA) review goal date at the end of August 2023, which is the date by which the FDA intends to take action on the application. The FDA’s acknowledgement of filing does not mean that a license will be granted, nor does it represent any evaluation of the adequacy of the data submitted.
About Chikungunya
Chikungunya is a mosquito-borne viral disease caused by the chikungunya virus (CHIKV), a Togaviridae virus, transmitted by Aedes mosquitoes. Chikungunya virus often causes sudden large outbreaks with high attack rates, affecting one-third to three-quarters of the population in areas where the virus is circulating. There are no preventive vaccines or effective treatments available and, as such, chikungunya is considered to be a major public health threat. As of July 2022, there were more than 3 million reported cases in the Americas[1] and the economic impact is considered to be significant. The medical and economic burden is expected to grow as the CHIKV primary mosquito vectors continue to spread geographically. Infection leads to symptomatic disease in up to 97% of humans after three to seven days following the mosquito bite. While mortality with CHIKV is low, morbidity is high. Clinical symptoms include acute onset of fever, debilitating joint and muscle pain, headache, nausea, rash and chronic arthralgia. It is estimated that over three quarters of the world’s population live in areas at-risk of CHIKV transmission[2]. High risk areas of infection are places where chikungunya virus-carrying mosquitos are currently endemic, including the Americas, parts of Africa, and Southeast Asia.
About VLA1553
VLA1553 is a live-attenuated, single dose investigational vaccine candidate targeting the chikungunya virus, which has spread to over 100 countries. It has been designed by deleting a part of the chikungunya virus genome.
To make VLA1553 more accessible to Low- and Middle-Income Countries (LMIC), Valneva and Instituto Butantan in Brazil signed an agreement in January 2021 for the development, manufacturing and marketing of VLA1553[3]. The collaboration falls within the framework of the agreement signed between CEPI and Valneva in July 2019[4], which provides funding of up to $24.6 million with support from the European Union’s Horizon 2020 program.
Valneva reported final data from the pivotal Phase 3 trial of VLA1553 in March 2022[5], final lot-to-lot consistency results in May 2022[6] and positive twelve-month persistence data in December 2022[7].
If approved, VLA1553 would expand Valneva’s existing commercial vaccines portfolio and as such, Valneva intends to commercialize this vaccine, leveraging its existing manufacturing and commercial operations.
About Valneva SE
Valneva is a specialty vaccine company focused on the development, manufacturing and commercialization of prophylactic vaccines for infectious diseases with significant unmet medical need. The Company takes a highly specialized and targeted approach to vaccine development and then applies its deep understanding of vaccine science to develop prophylactic vaccines addressing these diseases. Valneva has leveraged its expertise and capabilities both to commercialize three vaccines and to rapidly advance a broad range of vaccine candidates into and through the clinic, including candidates against the chikungunya virus and Lyme disease.
Valneva's single-shot chikungunya vaccine VLA1553 gets FDA priority review
Feb. 20, 2023 5:35 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted priority review to Valneva (NASDAQ:VALN) application seeking approval of single-shot chikungunya vaccine candidate VLA1553.
- https://seekingalpha.com/news/3937917-valnevas-single-shot-chikungunya-vaccine-vla1553-gets-fda-priority-review
- Valneva SE (VALN)
- https://valneva.com/research-development/chikungunya/
Zavegepant
VLA1553 (Chikungunya Vaccine )
Zavegepant
Pfizer Announces The Lancet Neurology Has Published Phase 3 Data for Zavegepant for the Acute Treatment of Migraine in Adults
Thursday, February 16, 2023 - 06:45am
- Zavegepant is the first and only calcitonin gene-related peptide (CGRP) receptor antagonist in development as an intranasal formulation studied in a Phase 3 trial
NEW YORK--(BUSINESS WIRE)-- Pfizer Inc. (NYSE: PFE) today announced publication of results in The Lancet Neurologyfrom the Phase 3 pivotal clinical trial of zavegepant, an investigational calcitonin gene-related peptide (CGRP) receptor antagonist nasal spray for the acute treatment of migraine. The study met its co-primary endpoints, showing that a single 10 mg dose of zavegepant was more effective than placebo for both pain freedom and freedom from the most bothersome symptom (MBS) at two hours post-dose. Additionally, zavegepant demonstrated relief from migraine pain in 15 minutes, with relief lasting up to 48 hours for many patients. Zavegepant was well tolerated, and there were no serious adverse events reported in treated participants.
“The results from this study demonstrate zavegepant’s potential as an effective acute nasal spray treatment for migraine, a neurological disorder that affects more than one billion people worldwide,” said Richard B. Lipton, M.D., Lead Author, Department of Neurology at the Albert Einstein College of Medicine. “This was the first Phase 3 clinical trial of a non-oral CGRP receptor antagonist developed for the acute treatment of migraine in adults. With this evidence of sustained treatment benefits, good tolerability and an alternative administration method, I believe zavegepant has the potential to fill an important gap in the available options for the acute treatment of migraine.”
In the trial, 1,405 people were randomized to receive a single 10 mg dose of either zavegepant or placebo. Participants historically experienced two to eight moderate or severe migraine attacks per month, and their untreated attacks lasted a mean of 30.8 hours. During the study, participants recorded their migraine headache pain intensity based on a four-point scale, identified their current MBS associated with migraine (selected from phonophobia, photophobia or nausea) and recorded their level of functional disability immediately before dosing the treated attack and at various intervals post-dose.
Zavegepant was demonstrated to be effective in the acute treatment of migraine, as measured by superiority to placebo on the co-primary efficacy endpoints of pain freedom (24% vs 15%, P<0·0001) and freedom from the MBS (40% vs 31%, P=0·0012) at two hours post-dose. Additionally, zavegepant was more effective than placebo on 13 of the 17 secondary endpoints, including treatment benefits for pain relief beginning as early as 15 minutes and sustained pain relief from two through 48 hours post-dose. On the 14th endpoint, return to normal function at 15 minutes post-dose, the difference between zavegepant and placebo was not significant. Consequently, in keeping with the analysis plan, the remaining secondary endpoints were not formally tested. Treatment with zavegepant was also associated with higher rates of return to normal functional ability at 30 minutes post treatment and two hours.
Zavegepant was well tolerated in this study. The most common adverse events (AE) in either treatment group (≥2%) were dysgeusia (an altered sense of taste), occurring in 20.5% of zavegepant patients as compared to 4.7% of patients on placebo, nasal discomfort, occurring in 3.7% of zavegepant patients as compared to 0.8% of patients on placebo, and nausea, occurring in 3.2% of zavegepant patients and 1.1% of patients on placebo. The AE safety profile was consistent with earlier studies of zavegepant. There were no serious AEs reported in treated participants, and no signal of hepatotoxicity due to zavegepant was identified in the trial.
“The intranasal formulation for zavegepant embodies breakthrough innovation in patient-centric drug development,” said James Rusnak, M.D., Ph.D., Senior Vice President, Chief Development Officer, Internal Medicine and Hospital, Global Product Development, Pfizer. “If approved by the FDA, zavegepant has the potential to be a significant new treatment option for people with migraine, particularly those who desire fast-acting relief or would benefit from an alternative delivery method. We are excited by the momentum the publication of these study results offers, as we anticipate potentially bringing a new medical breakthrough to millions of people suffering from migraine in the U.S.”
About Zavegepant
Zavegepant is a third generation, high affinity, selective and structurally unique, small molecule CGRP receptor antagonist and the only CGRP receptor antagonist in clinical development with both intranasal and oral formulations. The New Drug Application (NDA) was filed for intranasal zavegepant with the U.S. Food and Drug Administration for the acute treatment of migraine in adults. The Prescription Drug User Fee Act (PDUFA) goal date for completion of the FDA review of the NDA is set for 1Q2023.
About Migraine
Nearly 40 million people in the U.S. suffer from migraine1 and the World Health Organization classifies migraine as one of the 10 most disabling medical illnesses.2 Migraine is characterized by debilitating attacks lasting four to 72 hours with multiple symptoms, including pulsating headaches of moderate to severe pain intensity that can be associated with nausea or vomiting, and/or sensitivity to sound (phonophobia) and sensitivity to light (photophobia).3
About CGRP Receptor Antagonism
Small molecule CGRP receptor antagonists represent a novel class of drugs for the treatment of migraine. For acute treatment, this unique mode of action potentially offers an alternative to other agents, particularly for patients who have contraindications to the use of triptans or who have a poor response to triptans or are intolerant to them. CGRP signal-blocking therapies have not been associated with medication overuse headache (MOH) or rebound headaches which can limit the clinical utility of other acute treatments.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230216005209/en/
Source: Pfizer Inc.
Pfizer migraine nasal spray drug zavegepant meets phase 3 goals
Feb. 16, 2023 7:15 AM ET
By: Ravikash, SA News Editor2 Comments
Pfizer (NYSE:PFE) said results from a phase 3 trial of nasal spray zavegepant for the acute treatment of migraine were published in The Lancet Neurology.
Pfizer inherited zavegepant from its ~$11.6B acquisition of migraine drugmaker Biohaven. The drug is currently under review in the U.S. with an FDA decision expected in Q1 2023.
KIN-3248
VLA1553 (Chikungunya Vaccine )
Zavegepant
Kinnate Biopharma Inc. Receives Fast Track Designation from the U.S. Food and Drug Administration for KIN-3248, an Investigational Pan-FGFR Inhibitor
February 14, 2023 at 4:05 PM EST
SAN FRANCISCO and SAN DIEGO, Feb. 14, 2023 (GLOBE NEWSWIRE) --
Kinnate Biopharma Inc. (Nasdaq: KNTE) (“Kinnate”), a clinical-stage precision oncology company, today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation for Kinnate’s investigational pan-FGFR inhibitor, KIN-3248, for the treatment of patients with unresectable, locally advanced or metastatic cholangiocarcinoma (CCA) harboring fibroblast growth factor receptor 2 (FGFR2) gene fusions or other alterations, who have received at least one prior systemic therapy.
Cholangiocarcinoma, also known as bile duct cancer, is a rare condition, often diagnosed when it is advanced. Research has shown that FGFR is an actionable alteration in patients with CCA. FGFRs are tyrosine kinases that play a crucial role in cell proliferation, differentiation, migration and survival. FGFR2 gene fusions or other alterations are identified in approximately 16% of intrahepatic cholangiocarcinoma (ICC) tumors.
Fast Track is a process designed by the FDA to facilitate the development and expedite the review of drugs to treat serious conditions and fulfill an unmet medical need. A therapeutic candidate that receives Fast Track designation is eligible for more frequent interactions with the FDA to discuss the candidate’s development plan, and if relevant criteria are met, for Accelerated Approval and Priority Review.
About KIN-3248
KIN-3248 is an irreversible, small molecule pan-FGFR inhibitor designed to address primary FGFR2 and FGFR3 oncogenic alterations, including those predicted to drive acquired resistance to current FGFR-targeted therapies, such as gatekeeper, molecular brake, and activation loop mutations observed in cancers such as ICC and urothelial carcinoma (UC). In preclinical studies, KIN-3248 demonstrated inhibitory activity across a wide range of clinically relevant mutations that drive primary disease and acquired resistance to other FGFR inhibitors.
The KN-4802 clinical trial (NCT05242822) is an ongoing multi-center, open-label, two-part study of approximately 120 patients to evaluate the safety, tolerability, pharmacokinetics, and preliminary efficacy of KIN-3248 in adults with advanced tumors harboring FGFR2 and/or FGFR3 gene alterations. In dose escalation (Part A), the trial will determine the recommended dose and schedule of KIN-3248 for further evaluation in patients with FGFR2 and/or FGFR3 gene alteration-driven cancers. Dose expansion (Part B) will assess the safety and efficacy of KIN-3248 at the recommended dose and schedule in FGFR inhibitor naïve and FGFR inhibitor pretreated patients with cancers driven by FGFR2 and/or FGFR3 gene alterations, including ICC, UC, and other advanced or metastatic solid tumors in adults.
This trial is currently enrolling across multiple sites in the U.S. and Taiwan, with additional sites expected globally. Initial dose escalation data is anticipated in the second half of 2023.
The company previously announced that a poster presentation of the design and rationale of the KN-4802 clinical trial will be presented at the upcoming American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium. Details are included below.
ASCO Genitourinary Cancers Symposium, February 16-18, 2023
Title: First-in-Human Phase 1/1b Study Evaluating KIN-3248, a Next‑Generation, Irreversible Pan-FGFR Inhibitor, in Patients With Advanced Urothelial Carcinoma and Other Solid Tumors Harboring FGFR2 and/or FGFR3 Gene Alterations
Author: Benjamin Garmezy, MD
Abstract Number: TPS593
Poster Board: P16
Session Type and Track: Trials in Progress Poster Session, Urothelial Carcinoma
Session Date: February 17, 2023, 12:30 p.m. PT / 3:30 p.m. ET
For additional information, visit the ASCO Meeting webpage: https://conferences.asco.org.
About Kinnate Biopharma Inc.
Kinnate Biopharma Inc. is a clinical-stage precision oncology company focused on expanding on the promise of targeted therapies for those battling cancer. The company is developing medicines for known oncogenic drivers where there are no approved targeted drugs and to overcome the limitations of marketed cancer therapies, such as non-responsiveness or acquired and intrinsic resistance. Kinnate has two lead clinical programs being studied in solid tumors with RAF, NRAS and FGFR-driven alterations, and is rapidly progressing a pipeline of additional small molecule drug candidates as part of the Kinnate Discovery Engine. The company is driven by the urgency and knowledge that patients are waiting for new, effective cancer medicines. For more information, visit Kinnate.com and follow us on LinkedIn.
Kinnate Biopharma gets FDA fast track designation for its bile duct cancer treatment
Feb. 14, 2023 5:26 PM ET
By: Anuron Mitra, SA News Editor
- Kinnate Biopharma (NASDAQ:KNTE) on Tuesday said the U.S. Food and Drug Administration (FDA) had granted a fast track designation to its inhibitor KIN-3248 for the treatment of bile duct cancer.
- https://seekingalpha.com/news/3936095-kinnate-biopharma-gets-fda-fast-track-designation-for-its-bile-duct-cancer-treatment
- Kinnate Biopharma Inc. (KNTE)
- https://www.kinnate.com/science-and-pipeline/
- https://www.kinnate.com/
biotecHOPE™ 2023
Povorcitinib (INCB54707)
Povorcitinib (INCB54707)
Povorcitinib (INCB54707)
Incyte Announces 52-Week Results From Phase 2 Study Evaluating Povorcitinib (INCB54707) In Patients With Hidradenitis Suppurativa
February 10, 2023 at 8:20 AM EST
- Results from open-label extension period of the Phase 2 trial demonstrate that longer-term treatment with povorcitinib 75 mg resulted in sustained and durable efficacy across all treatment arms
- Data featured as an oral presentation at the European Hidradenitis Suppurativa Foundation conference
- Hidradenitis suppurativa (HS) is a chronic and debilitating inflammatory skin condition characterized by painful nodules and abscesses that can lead to irreversible tissue destruction and scarring1
WILMINGTON, Del.--(BUSINESS WIRE)--Feb. 10, 2023-- Incyte (Nasdaq:INCY) today announced new 52-week results from a Phase 2 study evaluating the efficacy and safety of povorcitinib (formerly INCB54707), an oral JAK1 inhibitor, in adult patients with hidradenitis suppurativa (HS). These data were presented as an oral presentation (Abstract #258) at the 12th Conference of the European Hidradenitis Suppurativa Foundation, held from February 8-10, 2023, in Florence, Italy.
The study previously met its primary endpoint, demonstrating that at Week 16 – the double-blind, placebo-controlled portion of the study – patients receiving povorcitinib once daily (QD) had significantly greater decreases from baseline in Abscess and Inflammatory Nodule (AN) count versus placebo (least squares mean change, −2.5 [0.9], placebo vs. −5.2 [0.9], P=0.0277, povorcitinib 15 mg; −6.9 [0.9], P=0.0006, povorcitinib 45 mg; −6.3 [0.9], P=0.0021), povorcitinib 75 mg)2.
New results at Week 52, which include the 36-week open-label extension period during which all patients received povorcitinib 75 mg once daily (QD), show that average efficacy was sustained for all treatment arms following the switch to povorcitinib 75 mg QD (mean change in AN count from Day 1 baseline at Week 52 was −5.7 [7.3], placebo→75 mg; −8.4 [5.6], 15→75 mg; −10.4 [14.6], 45→75 mg; and −5.4 [5.6], 75 mg). Importantly, povorcitinib also demonstrated durable efficacy at Week 52 in high-threshold outcomes, as evidenced by 22-29% of patients achieving HS Clinical Response 100 (HiSCR100), which is defined as a 100% reduction from baseline in total AN count with no increase from baseline in abscess or draining tunnel count.
Povorcitinib was generally well tolerated and the safety profile was consistent with previously-reported data. The most common treatment-emergent adverse events (TEAEs) at Week 52 (n=174) were COVID-19 (21.3%), acne (11.5%), upper respiratory tract infection (10.9%), headache (5.7%), nasopharyngitis (5.7%), urinary tract infection (5.7%) and increased blood creatine kinase (CK) (5.2%). In total, six patients (3.4%) experienced a TEAE that led to treatment discontinuation. No fatal TEAEs were observed.
“HS is a chronic, progressive and debilitating condition for which there is no cure. We are encouraged by these Phase 2 data and believe they reinforce the potential of povorcitinib to be a safe and efficacious treatment for HS that is tolerable with longer-term administration, even at the higher doses,” said Kurt Brown, M.D., Global Program Head, Povorcitinib, and Associate Vice President, Drug Development, Inflammation & AutoImmunity, Incyte. “Despite the available treatments for HS, no uniformly-effective therapy has been found, underscoring the need for additional options. We look forward to continuing to progress the development of povorcitinib through our ongoing Phase 3 trial in patients with moderate-to-severe HS.”
“Given the nature of HS, which presents with persistent, painful nodules and abscesses, this immune-mediated skin condition often has a severe impact on a patient’s quality of life,” said Joslyn Kirby, M.D., M.S., M.Ed., Associate Professor and Vice Chair for Education, Department of Dermatology at Penn State Health. “I am encouraged by these promising results suggesting that povorcitinib may be a favorable oral treatment option that could provide substantial relief from common HS symptoms for patients.”
This presentation will be made available for registered participants on the EHSF website at https://www.eventclass.org/contxt_ehsf2023/scientific/online-program/session?s=S-09#e268 and can be accessed until August 31, 2023.
About Hidradenitis Suppurativa
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by painful nodules and abscesses that can lead to irreversible tissue destruction and scarring.1 Over-activity of the JAK/STAT signaling pathway is believed to drive inflammation involved in the pathogenesis and progression of HS3. More than 150,000 patients in the U.S. are estimated to have moderate to severe HS4. Given the debilitating nature of condition, it can have a profoundly negative effect on patients’ quality of life5.
About the Phase 2 Study (NCT04476043)
This Phase 2, randomized, double-blind, placebo-controlled, dose-ranging study is evaluating the efficacy and safety of povorcitinib (formerly INCB54707) in adult patients with hidradenitis suppurativa (HS).
The first part of the study spanned 16 weeks and enrolled 209 adults (aged 18-75 years) who were randomized 1:1:1:1 to povorcitinib 15 mg once daily (QD; n=52), 45 mg QD (n=52), 75 mg QD (n=53) or placebo (n=52). Eligible patients had an HS (Hurley stage I, II or III) disease duration of ≥3 months prior to screening, and active HS in at least two distinct anatomical areas. The primary efficacy endpoint is mean change from baseline in Abscess and Inflammatory Nodule (AN) count at Week 16. The key secondary endpoint is percentage of patients achieving HS Clinical Response (HiSCR; ≥50% reduction from baseline in AN count with no increase in number of abscesses or draining tunnels) at Week 16.
The second part of the study, the open-label extension (OLE) period, spanned an additional 36 weeks (52 weeks total) and included patients enrolled in the first part of the study. All OLE patient participants (n=174) received treatment with povorcitinib 75 mg QD. After Week 52, patients who completed baseline, Week 16 and Week 52 assessments could continue to receive open-label treatment with povorcitinib 75 mg QD for an additional 48 weeks.
Endpoints at Week 52 include mean change from baseline in AN count, HiSCR and HiSCR75/90/100 (≥75%/90%/100% reduction from baseline in AN count with no increase in the number of abscesses or draining tunnels), HS flare occurrence, mean change from baseline in International Hidradenitis Suppurativa Severity Score System (IHS4) and IHS455/75/90/100 (≥55%/75%/90%/100% reduction from baseline in IHS4 score). Safety of povorcitinib was assessed by the frequency and severity of treatment-emergent adverse events (TEAEs).
For more information about this Phase 2 study, please visit https://clinicaltrials.gov/ct2/show/NCT04476043.
About Povorcitinib (INCB54707)
Povorcitinib (INCB54707) is an oral small-molecule JAK1 inhibitor currently in Phase 2 clinical trials for hidradenitis suppurativa (HS), vitiligo and prurigo nodularis. A Phase 3 study in HS is also ongoing.
About Incyte
Incyte is a Wilmington, Delaware-based, global biopharmaceutical company focused on finding solutions for serious unmet medical needs through the discovery, development and commercialization of proprietary therapeutics. For additional information on Incyte, please visit Incyte.com and follow @Incyte.
Incyte skin disorder drug shows durable efficacy in 1 year data from mis-stage trial
Feb. 10, 2023 9:17 AM ET
By: Ravikash, SA News Editor
Incyte (NASDAQ:INCY) said an extension period of a phase 2 trial showed that longer-term treatment with povorcitinib 75 mg resulted in sustained and durable efficacy in patients with a type of skin condition called Hidradenitis suppurativa (HS).
Rigosertib
Povorcitinib (INCB54707)
Povorcitinib (INCB54707)
Feb 07, 2023
Onconova Therapeutics Announces Additional Clinical Data Demonstrating Rigosertib’s Monotherapy Activity In RDEB-Associated Squamous Cell Carcinoma
Two of two evaluable participants in an ongoing investigator-sponsored program of rigosertib in RDEB-associated squamous cell carcinoma (SCC) have achieved a complete response of all cancerous skin lesions
First evaluable participant has been in complete remission with no signs of metastatic disease for >18 months; the second patient has achieved a complete response in all squamous cell skin lesions following four cycles of treatment and remains on therapy with additional scans to follow to evaluate metastatic disease
Onconova plans to review initial data with regulators to gain insights on the optimal regulatory pathway for rigosertib in RDEB-associated SCC, an ultra-rare and invariably fatal condition
NEWTOWN, Pa., Feb. 07, 2023 (GLOBE NEWSWIRE) -- Onconova Therapeutics, Inc. (NASDAQ: ONTX), (“Onconova”), a clinical-stage biopharmaceutical company focused on discovering and developing novel products for patients with cancer, today announced that the second of two evaluable participants in an investigator-initiated Phase 2 program evaluating rigosertib monotherapy in advanced squamous cell carcinoma complicating recessive dystrophic epidermolysis bullosa (RDEB-associated SCC) achieved a complete response of all cancerous skin lesions following 4 treatment cycles and remains on oral rigosertib.
The Company previously announced that the RDEB-associated SCC program’s first evaluable participant achieved a RECIST-defined complete response. Both of the program’s evaluable participants remain on therapy, with the first participant in complete remission with no signs of metastatic disease for more than 18 months. Rigosertib continues to demonstrate a favorable safety profile in this indication that is similar to that displayed in prior studies in other indications.
“Though from only two participants, the emerging data from this Phase 2 program show rigosertib displaying a level of anti-cancer activity in RDEB-associated SCC that far exceeds what we have seen with currently available treatments,” said Professor Andrew P South from Sidney Kimmel Cancer Center, Thomas Jefferson University. “Given its ultra-orphan nature and the extremely high unmet need in RDEB-associated SCC, I believe regulatory discussions to enable rigosertib’s expeditious advancement to potential approval in this indication are warranted. In parallel, we plan to continue advancing this Phase 2 program and to report more detailed data at a future medical meeting.”
RDEB is caused by insufficient expression of type VII collagen protein, which is responsible for anchoring the skin’s inner layer to its outer layer. This leads to extreme skin fragility as well as chronic blistering and wound formation with recurrent infections in RDEB patients, many of whom go on to develop metastatic squamous cell carcinoma driven by over expression of polo like kinase 1 (PLK1). RDEB-associated SCC tumors show a highly aggressive and early metastasizing course that makes them the primary cause of death for these patients, with a cumulative risk of death of 70% and 78.7% by ages 45 and 55, respectively1,2. RDEB-associated SCC can appear in pediatric patients or in young adults. Currently available treatments such as targeted therapies and conventional chemo- and/or radiotherapy have demonstrated limited response rates and poor durability in RDEB-associated SCC1,3.
Steven M. Fruchtman, M.D., President and Chief Executive Officer of Onconova, commented, “We are pleased to be building on this Phase 2 program’s initial single-patient data with a second participant showing complete resolution of all cancerous skin lesions, with the most recent patient notably seeing this result after only four cycles of therapy. We look forward to reviewing our findings with the FDA to determine the most expeditious regulatory path for rigosertib in RDEB-associated SCC. In addition, these findings may have important implications beyond this orphan indication, as they and prior preclinical data demonstrate rigosertib’s activity against the PLK1 protein. Although the company is focusing its resources mainly on the lead narazaciclib program, preclinical studies exploring rigosertib’s activity in other PLK1-dependent tumors are underway and will hopefully open a broader regulatory path for rigosertib.”
Onconova and a program investigator plan to present more detailed data on the first two evaluable participants from the Phase 2 RDEB-associated SCC program at a future medical meeting. In addition, preclinical data on rigosertib’s mechanism of action have been accepted for presentation at the American Association for Cancer Research (AACR) Targeting RAS Conference, which is taking place in Philadelphia, Pennsylvania from March 5 – 8, 2023.
About Rigosertib
Rigosertib is an investigational product candidate with a multi-faceted mechanism of action targeting proteins containing the RAS binding domain, allowing it to modulate the PI3K and PLK-1 pathways, as well as the tumor immune microenvironment. It is currently being evaluated in multiple investigator-sponsored studies, including a dose-escalation and expansion Phase 1/2a study of oral rigosertib in combination with nivolumab for patients with KRAS+ non-small cell lung cancer refractory to pembrolizumab, the current standard of care for these patients, and a Phase 2 program evaluating rigosertib monotherapy in advanced squamous cell carcinoma complicating recessive dystrophic epidermolysis bullosa.
About Onconova Therapeutics, Inc.
Onconova Therapeutics is a clinical-stage biopharmaceutical company focused on discovering and developing novel products for patients with cancer. The Company has proprietary targeted anti-cancer agents designed to disrupt specific cellular pathways that are important for cancer cell proliferation.
Onconova’s novel, proprietary multi-kinase inhibitor narazaciclib (formerly ON 123300) is being evaluated in two separate and complementary Phase 1 dose escalation and expansion studies. These trials are currently underway in the United States and China. Based on preclinical and clinical studies of CDK 4/6 inhibitors, Onconova is also planning a combination trial of narazaciclib with estrogen blockade in advanced endometrial cancer, as well as its clinical study in additional indications.
Onconova’s product candidate rigosertib is being studied in multiple investigator-sponsored studies, including a dose-escalation and expansion Phase 1/2a study of oral rigosertib in combination with nivolumab in patients with KRAS+ non-small cell lung cancer, and a Phase 2 program evaluating rigosertib monotherapy in advanced squamous cell carcinoma complicating recessive dystrophic epidermolysis bullosa.
For more information, please visit www.onconova.com.
Onconova Therapeutics posts positive data from squamous cell carcinoma treatment trial
Feb. 07, 2023 9:38 AM ET
Onconova Therapeutics, Inc. (ONTX)
By: Dania Nadeem, SA News Editor
- Onconova Therapeutics (NASDAQ:ONTX) said on Tuesday a Phase 2 trial testing rigosertib monotherapy in advanced squamous cell carcinoma complicating recessive dystrophic epidermolysis bullosa achieved a complete response of all cancerous skin lesions following four treatment cycles.
- https://seekingalpha.com/news/3932872-onconova-therapeutics-posts-positive-data-from-squamous-cell-carcinoma-treatment-trial
- Onconova Therapeutics, Inc. (ONTX)
- https://www.onconova.com/pipeline/
Nipocalimab
Povorcitinib (INCB54707)
Zuranolone (SAGE-217/BIIB125)
Janssen Reports Positive Topline Phase 2 Results for Nipocalimab in Pregnant Individuals at High Risk for Severe Hemolytic Disease of the Fetus and Newborn (HDFN)
Feb 06, 2023
United States
There are currently no approved therapeutics for the treatment of HDFN which, in severe cases, can cause life-threatening anemia in the fetus
SPRING HOUSE, PENNSYLVANIA, February 6, 2023 – The Janssen Pharmaceutical Companies of Johnson & Johnson today announced positive topline results from the proof-of-concept Phase 2 open-label UNITY clinical trial for the treatment of pregnant adults at high risk for severe hemolytic disease of the fetus and newborn (HDFN). HDFN is a serious and rare condition which can cause life-threatening anemia in the fetus. It occurs when the blood types of a pregnant individual and their fetus are incompatible.1The trial met the primary endpoint, with the majority of pregnant patients who received nipocalimab achieving a live birth at or after the gestational age (GA) of 32 weeks, without the need for an intrauterine transfusion (IUT) throughout their entire pregnancy. During the treatment period of approximately 20 weeks, nipocalimab demonstrated a safety profile that supports further development of the treatment in HDFN.
Nipocalimab was granted Fast Track designation in July 2019 and orphan drug status in June 2020 by the U.S. Food and Drug Administration (FDA), and orphan medicinal product designation by the European Medicines Agency in October 2019 for HDFN.
“These early results represent an important step towards delivering a potential medication for expectant mothers at high risk of severe HDFN, and we are encouraged by what this treatment could mean for families affected by this potentially devastating disease. I would like to thank our patients and investigators for their participation and commitment in completing UNITY,” said Katie Abouzahr, M.D., Vice President, Autoantibody Portfolio Development Leader, Janssen Research & Development, LLC. “We look forward to sharing the full Phase 2 results of the UNITY trial at an upcoming scientific medical meeting while we continue to plan for a pivotal Phase 3 trial.”
About UNITY
UNITY is a global, multicenter, open-label, non-blinded Phase 2 clinical trial to evaluate the safety and efficacy of nipocalimab for the treatment of pregnant adults at high risk for severe HDFN.2 In the trial, 14 participants received once weekly intravenous infusions. The primary endpoint was live birth at or after GA of 32 weeks, without a need for an intrauterine transfusion (IUT) throughout the entire pregnancy. Adverse events were monitored up to approximately 24 weeks post-delivery for parents and up to approximately 96 weeks post-birth for children.2
About HDFN
HDFN is a rare autoantibody-driven disease where antibodies produced in a pregnant person’s immune system cross the placenta and attack fetal red blood cells — causing fetal hemolysis leading to anemia.1 The severe form of HDFN, which is categorized as an ultra-rare disease, can lead to life-threatening anemia.3Today, there are no approved therapeutics for the treatment of HDFN, and pregnancies affected by severe HDFN may necessitate repeated IUTs. IUTs are invasive, technically complex surgical procedures performed by specialists that may be associated with an increased rate of fetal mortality and premature birth.4 According to the American Journal of Obstetrics and Gynecology, in the U.S., it is estimated that up to 80 out of every 100,000 pregnancies are affected by HDFN each year.5
About Nipocalimab
Nipocalimab is an investigational, high affinity, fully human, aglycosylated, effectorless, monoclonal antibody that is believed to selectively block the Fc receptor (FcRn) to reduce levels of circulating immunoglobulin G (IgG) antibodies, including autoantibodies and alloantibodies that underlie multiple conditions. Nipocalimab is being studied in all three segments of autoantibody-driven disease: maternal fetal diseases mediated by maternal autoantibodies – also known as alloantibodies (e.g., HDFN); rare autoantibody diseases (e.g., generalized myasthenia gravis in adults and children, chronic inflammatory demyelinating polyneuropathy, warm autoimmune hemolytic anemia, and idiopathic inflammatory myopathies); and prevalent rheumatologic diseases (e.g., rheumatoid arthritis, Sjögren's syndrome, and systemic lupus erythematosus).2,6-14 Blockade of FcRn by nipocalimab has the potential to reduce overall autoantibody levels while maintaining immune function. FcRn blockade is also believed to prevent placental transfer of maternal alloantibodies to the fetus.2,15 Currently, nipocalimab is the only therapy in clinical development for the treatment of alloimmunized pregnant adults at risk of severe HDFN.
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we’re creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com. Follow us at www.twitter.com/JanssenGlobal.
Janssen Research & Development, LLC is a part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
Johnson & Johnson succeeds in mid-stage trial for fetal disorder candidate
Feb. 06, 2023 9:15 AM ET
By: Dulan Lokuwithana, SA News Editor1 Comment
The Janssen unit of Johnson & Johnson (NYSE:JNJ) announced Monday that its candidate for rare fetal disorder severe hemolytic disease of the fetus and newborn (HDFN) reached the main goal in a Phase 2 study.
Zuranolone (SAGE-217/BIIB125)
ACI-24.060 Anti-Amyloid Beta Vaccine
Zuranolone (SAGE-217/BIIB125)
February 6, 2023
Sage Therapeutics and Biogen Announce FDA Accepts Filing of New Drug Application and Grants Priority Review of Zuranolone in the Treatment of Major Depressive Disorder and Postpartum Depression
Zuranolone is being evaluated as a potential 14-day, rapid-acting, once-daily, oral medication to treat major depressive disorder (MDD) and postpartum depression (PPD)
Depression is a public health issue with significant unmet medical need
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Feb. 6, 2023-- Sage Therapeutics, Inc. (Nasdaq: SAGE) and Biogen Inc. (Nasdaq: BIIB) announced the U.S. Food and Drug Administration (FDA) has accepted the filing of a New Drug Application (NDA) for zuranolone in the treatment of major depressive disorder (MDD) and postpartum depression (PPD). Zuranolone is an investigational drug being evaluated as a 14-day, rapid-acting, once-daily, oral treatment in adults with MDD and PPD. The application has been granted priority review and the FDA has assigned a Prescription Drug User Fee Act (PDUFA) action date of August 5, 2023.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20230205005025/en/
“We see potential for zuranolone, if approved, to be a meaningful new option that can help address the serious unmet need faced by the diverse populations struggling with MDD and PPD,” said Priya Singhal, M.D., M.P.H., Executive Vice President, Head of Development and Interim Head of Research and Global Safety and Regulatory Sciences at Biogen. “The FDA filing acceptance and granting of priority review are important milestones in the mission Biogen and our collaboration partner Sage share to advance the understanding and treatment of depression.”
Depression is one of the leading contributors to disability worldwide.1 It is estimated that more than 21 million adults in the U.S. experienced at least one major depressive episode in 2020, with nearly 14 million people diagnosed with major depressive disorder,2 and an estimated 500,000 cases of PPD annually.3 Symptoms of MDD and PPD have been shown to have an impact on a person’s overall quality of life, functioning and well-being. In 2018, the incremental economic burden of MDD was an estimated $326 billion in the U.S. alone.4
The zuranolone NDA includes data from the LANDSCAPE and NEST clinical development programs as well as a Phase 2 study of zuranolone completed by Shionogi in Japan in adults with MDD. The LANDSCAPE program includes five studies of zuranolone in adults with MDD (MDD-201B, MOUNTAIN, SHORELINE, WATERFALL, and CORAL). The NEST program includes two studies of zuranolone in adult women with PPD (ROBIN and SKYLARK).
“We feel a tremendous responsibility to patients with MDD and PPD to deliver a potential new treatment option, which is so desperately needed. Most current approved therapies may take weeks or months to work. We are committed to advancing treatments that could help physicians and patients by addressing depression symptoms quickly,” said Laura Gault, M.D., Ph.D., Chief Medical Officer at Sage. “We believe zuranolone, if approved, could offer a new way for physicians to support patients.”
Zuranolone, a neuroactive steroid, has a novel mechanism of action as a positive allosteric modulator of GABA-A receptors. In people with depression, it is thought to work by rapidly rebalancing dysregulated neuronal networks to help reset brain function. Zuranolone targets brain networks responsible for functions such as mood, arousal, behavior, and cognition.
Priority Review is granted by the FDA to applications for medicines that, if approved, would provide significant improvements in the effectiveness or safety of the treatment, diagnosis, or prevention of serious conditions.
About Major Depressive Disorder (MDD)
Major depressive disorder (MDD) is a common but serious mood disorder in which people experience depressive symptoms that impair their social, occupational, educational, or other important functioning, such as a depressed mood or loss of interest or pleasure in daily activities, consistently for at least a two-week period. It is estimated that in 2020, more than 21 million adults in the U.S. experienced at least one major depressive episode in the past year with nearly 14 million people diagnosed with major depressive disorder.2 There were approximately 190 million cases of MDD worldwide in 2020.5
About Postpartum Depression (PPD)
Postpartum depression (PPD) is one of the most common medical complications during and after pregnancy.6 PPD can have a serious negative impact on a woman, including significant functional impairment, depressed mood and/or loss of interest in her newborn, and associated symptoms of depression such as loss of appetite, difficulty sleeping, motor challenges, lack of concentration, loss of energy and poor self-esteem. PPD is estimated to affect approximately one in eight women who have given birth in the U.S. or approximately 500,000 women annually.3
About ZURANOLONE
Zuranolone (SAGE-217/BIIB125) is a once-daily, 14-day, investigational drug in development for the treatment of major depressive disorder (MDD) and postpartum depression (PPD). Zuranolone is an oral neuroactive steroid (NAS) GABA-A receptor positive allosteric modulator (PAM). The GABA system is the major inhibitory signaling pathway of the brain and central nervous system and contributes to regulating brain function.
Zuranolone is being evaluated in the LANDSCAPE and NEST clinical development programs. The two development programs include multiple studies examining use of zuranolone in several thousand people with a variety of dosing, clinical endpoints, and treatment paradigms. The LANDSCAPE program includes five studies of zuranolone in people with MDD (MDD-201B, MOUNTAIN, SHORELINE, WATERFALL, and CORAL Studies). The NEST program includes two placebo-controlled studies of zuranolone in women with PPD (ROBIN and SKYLARK Studies). Additionally, Shionogi completed a Phase 2 study of zuranolone in Japan in people with MDD.
About Sage Therapeutics
Sage Therapeutics is a biopharmaceutical company fearlessly leading the way to create a world with better brain health. Our mission is to pioneer solutions to deliver life-changing brain health medicines, so every person can thrive. For more information, please visit www.sagerx.com.
About Biogen
As pioneers in neuroscience, Biogen discovers, develops, and delivers worldwide innovative therapies for people living with serious neurological diseases as well as related therapeutic adjacencies. One of the world’s first global biotechnology companies, Biogen was founded in 1978 by Charles Weissmann, Heinz Schaller, Sir Kenneth Murray, and Nobel Prize winners Walter Gilbert and Phillip Sharp. Today, Biogen has a leading portfolio of medicines to treat multiple sclerosis, has introduced the first approved treatment for spinal muscular atrophy, and developed the first approved treatment to address a defining pathology of Alzheimer’s disease. Biogen is also commercializing biosimilars and focusing on advancing one of the industry’s most diversified pipelines in neuroscience that will transform the standard of care for patients in several areas of high unmet need.
We routinely post information that may be important to investors on our website at www.biogen.com. Follow us on social media - Twitter, LinkedIn, Facebook, YouTube.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230205005025/en/
Source: Sage Therapeutics, Inc.
Biogen, Sage win FDA priority review for depression therapy
Feb. 06, 2023 7:25 AM ET
Biogen Inc. (BIIB), SAGESGIOF, SGIOY
By: Dulan Lokuwithana, SA News Editor
- Biogen (NASDAQ:BIIB) and Sage Therapeutics (NASDAQ:SAGE) announced Monday that the FDA accepted their New Drug Application (NDA) for oral depression therapy zuranolone under the agency’s priority review. Sage (SAGE) shares have added ~5%, while Biogen (BIIB) is trading flat in reaction.
- The FDA has granted August 05, 2023, as the action date for the NDA, which is intended for the U.S. approval of zuranolone for major depressive disorder (MDD) and postpartum depression (PPD).
- https://seekingalpha.com/news/3932229-biogen-sage-win-fda-priority-review-for-depression-therapy
- Biogen Inc. (BIIB), SAGE
- https://www.biogen.com/
- https://www.sagerx.com/home
aypirca™ (pirtobrutinib)
ACI-24.060 Anti-Amyloid Beta Vaccine
ACI-24.060 Anti-Amyloid Beta Vaccine
U.S. FDA Approves Jaypirca™ (pirtobrutinib), the First and Only Non-Covalent (Reversible) BTK Inhibitor, for Adult Patients with Relapsed or Refractory Mantle Cell Lymphoma After at Least Two Lines of Systemic Therapy, Including a BTK Inhibitor
January 27, 2023
Jaypirca is the first BTK inhibitor of any kind specifically approved for patients with mantle cell lymphoma previously treated with a covalent BTK inhibitor
In the BRUIN Phase 1/2 trial, covalent BTK inhibitor pre-treated patients with relapsed or refractory MCL achieved an overall response rate of 50%, with 13% of patients achieving a complete response
INDIANAPOLIS, Jan. 27, 2023 /PRNewswire/ -- Loxo@Lilly, the oncology unit of Eli Lilly and Company (NYSE: LLY), today announced that the U.S. Food and Drug Administration (FDA) approved Jaypirca™ (pirtobrutinib, 100 mg & 50 mg tablets) for the treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL) after at least two lines of systemic therapy, including a Bruton's tyrosine kinase (BTK) inhibitor. Jaypirca was approved under the FDA's Accelerated Approval pathway based on response rate from the open-label, single-arm, international, Phase 1/2 study, called the BRUIN trial.1 Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
Jaypirca, a highly selective kinase inhibitor, utilizes a novel binding mechanism and is the first and only FDA approved non-covalent (reversible) BTK inhibitor. Jaypirca can reestablish BTK inhibition in MCL patients previously treated with a covalent BTK inhibitor (ibrutinib, acalabrutinib, or zanubrutinib) and extend the benefit of targeting the BTK pathway.
"The approval of Jaypirca represents an important advance for patients with relapsed or refractory MCL, who currently have limited options and historically have had a poor prognosis following discontinuation of treatment with a covalent BTK inhibitor," said Michael Wang, M.D., Puddin Clarke Endowed Professor of Lymphoma and Myeloma at The University of Texas MD Anderson Cancer Center. "These data indicate that Jaypirca can provide efficacy in patients previously treated with a covalent BTK inhibitor, potentially extending the time patients may benefit from BTK inhibition therapy. Jaypirca offers a new approach to targeting the BTK pathway following treatment with a covalent BTK inhibitor and has the potential to meaningfully impact the treatment paradigm for relapsed and refractory MCL patients."
The labeling for Jaypirca contains warnings and precautions for infections, hemorrhage, cytopenias, atrial fibrillation and flutter, second primary malignancies, and embryo-fetal toxicity. See Important Safety Information below and full Prescribing Information for additional information, including dosing modifications.
"We are pleased to bring a meaningful new therapeutic option to patients with MCL that can reestablish the benefit of targeting the BTK pathway after receiving multiple prior therapies, including a covalent BTK inhibitor," said Jacob Van Naarden, chief executive officer, Loxo@Lilly. "We are grateful to the patients, investigators, and other members of the clinical care teams for their contributions. Our team has been committed to rapidly advancing the development of Jaypirca for patients with MCL, and we look forward to building on this milestone by continuing to bring forward important new treatments for people with hematologic malignancies."
The FDA approval is based on data from a subset of patients in the BRUIN Phase 1/2 trial. The assessment of efficacy was based on 120 patients with MCL treated with Jaypirca 200 mg once daily until disease progression or unacceptable toxicity. Patients with active central nervous system lymphoma or allogeneic hematopoietic stem cell transplantation or CAR T-cell therapy within 60 days were excluded. Patients had received a median of three prior lines of therapy (range: 1 to 9), with 93% having two or more prior lines; all patients received one or more prior lines of therapy containing a covalent BTK inhibitor. Eighty-three percent (83%) of patients discontinued their last BTK inhibitor due to refractory or progressive disease. Efficacy was based on overall response rate (ORR) and duration of response (DOR) as assessed by an independent review committee (IRC) using 2014 Lugano criteria.
Jaypirca is expected to be available in the United States in the coming weeks.
The confirmatory Phase 3 trial (NCT04662255; BRUIN MCL-321) is currently enrolling patients.
See Important Safety Information below and full Prescribing Information for additional information.
Click here to view the mantle cell lymphoma infographic.
Click to view the Jaypirca product photos: 100 mg and 50 mg.
Click here to view the Jaypirca logo.
About the BRUIN Phase 1/2 Trial
The BRUIN Phase 1/2 clinical trial is the ongoing first-in-human, global, multi-center evaluation of Jaypirca in patients with hematologic malignancies, including mantle cell lymphoma (MCL).
The trial includes a Phase 1 dose-escalation phase, a Phase 1b combination arm, and a Phase 2 dose-expansion phase. The primary endpoint of the Phase 1 study is maximum tolerated dose (MTD)/recommended Phase 2 dose (RP2D). Secondary endpoints include safety, pharmacokinetics (PK), and preliminary efficacy measured by overall response rate (ORR) for monotherapy. The primary endpoint of the Phase 1b study is safety of the drug combinations. The secondary endpoints are PK and preliminary efficacy measured by ORR for the drug combinations. The primary endpoint for the Phase 2 study is ORR as determined by an independent review committee (IRC). Secondary endpoints include ORR as determined by investigator, best overall response (BOR), duration of response (DOR), progression-free survival (PFS), overall survival (OS), safety, and PK.
About Jaypirca™ (pirtobrutinib)
Jaypirca (pirtobrutinib, formerly known as LOXO-305) (pronounced jay-pihr-kaa) is a highly selective (300 times more selective for BTK versus 98% of other kinases tested in preclinical studies), non-covalent (reversible) inhibitor of the enzyme BTK.2 BTK is a validated molecular target found across numerous B-cell leukemias and lymphomas including mantle cell lymphoma.3,4 Jaypirca is a U.S. FDA-approved oral prescription medicine, 100 mg or 50 mg tablets taken as a once-daily 200 mg dose with or without food until disease progression or unacceptable toxicity.
About Mantle Cell Lymphoma
MCL is a rare blood cancer and a form of non-Hodgkin lymphoma (NHL). Annually, about one in 200,000 people worldwide develop MCL.5
MCL arises in B lymphocytes, a type of white blood cell and part of the immune system. MCL frequently begins in B cells located in the mantle zone of the outer edge of lymph nodes. As the cancer progresses, it can spread to bone marrow, the spleen, the liver, or the digestive tract.5
INDICATIONS FOR JAYPIRCA
Jaypirca is a kinase inhibitor indicated for the treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL) after at least two lines of systemic therapy, including a BTK inhibitor. This indication is approved under accelerated approval based on response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
Please see Prescribing Information and Patient Information for Jaypirca.
About Lilly
Lilly unites caring with discovery to create medicines that make life better for people around the world. We've been pioneering life-changing discoveries for nearly 150 years, and today our medicines help more than 47 million people across the globe. Harnessing the power of biotechnology, chemistry and genetic medicine, our scientists are urgently advancing new discoveries to solve some of the world's most significant health challenges, redefining diabetes care, treating obesity and curtailing its most devastating long-term effects, advancing the fight against Alzheimer's disease, providing solutions to some of the most debilitating immune system disorders, and transforming the most difficult-to-treat cancers into manageable diseases. With each step toward a healthier world, we're motivated by one thing: making life better for millions more people. That includes delivering innovative clinical trials that reflect the diversity of our world and working to ensure our medicines are accessible and affordable. To learn more, visit Lilly.com and Lilly.com/newsroom or follow us on Facebook, Instagram and LinkedIn. P-LLY
Jaypirca™ is a trademark owned by or licensed to Eli Lilly and Company, its subsidiaries, or affiliates.

View original content to download multimedia:https://www.prnewswire.com/news-releases/us-fda-approves-jaypirca-pirtobrutinib-the-first-and-only-non-covalent-reversible-btk-inhibitor-for-adult-patients-with-relapsed-or-refractory-mantle-cell-lymphoma-after-at-least-two-lines-of-systemic-therapy-including-a-301732669.html
SOURCE Eli Lilly and Company
Eli Lilly wins FDA accelerated approval for lymphoma therapy
Jan. 27, 2023 2:42 PM ET
By: Dulan Lokuwithana, SA News Editor1 Comment
The oncology division of Eli Lilly (NYSE:LLY) announced Friday that the FDA greenlighted its Bruton's tyrosine kinase (BTK) inhibitor Jaypirca as a late-line option for certain patients with mantle cell lymphoma (MCL), a rare blood cancer.
https://seekingalpha.com/news/3929112-lly-stock-wins-fda-accelerated-approval-lymphoma-therapy
ACI-24.060 Anti-Amyloid Beta Vaccine
ACI-24.060 Anti-Amyloid Beta Vaccine
ACI-24.060 Anti-Amyloid Beta Vaccine
AC Immune’s ACI-24.060 Anti-Amyloid Beta Vaccine For Alzheimer’s Shows Positive Initial Interim Safety And Immunogenicity In Phase 1b/2 ABATE Trial
Jan 26, 2023
AC Immune’s ACI-24.060 Anti-Amyloid Beta Vaccine for Alzheimer’s Shows Positive Initial Interim Safety and Immunogenicity in Phase 1b/2 ABATE Trial
- ACI-24.060 elicited an anti-Abeta antibody response in ABATE’s first, low dose cohort
- ACI-24.060 was generally well tolerated with no safety concerns observed
- With these findings, dosing in the second, higher dose Alzheimer’s cohort has begun
- Screening of cohort of study participants with Down syndrome also cleared to begin
- Further safety and immunogenicity findings from ABATE cohorts expected in H2 2023
- Initial data on amyloid plaque reduction measured via PET imaging anticipated in 2024
Lausanne, Switzerland, January 26, 2023 – AC Immune SA (NASDAQ: ACIU), a clinical-stage biopharmaceutical company pioneering precision medicine for neurodegenerative diseases, today announced the first interim safety, tolerability and immunogenicity findings from the Phase 1b/2 ABATE trial of its anti-amyloid-beta (Abeta) vaccine ACI-24.060 in patients with prodromal Alzheimer’s disease (AD). ABATE will now be expanded, as planned, to include individuals with Down syndrome (DS) and to evaluate higher doses in Alzheimer’s patients.
Targeting Abeta using antibodies has recently been validated with FDA approvals of new monoclonal antibody treatments for patients with AD. By eliciting polyclonal anti-Abeta antibodies, the ACI-24.060 anti-Abeta vaccine development program aims to ultimately deliver significant benefits to patients, their caregivers, and healthcare systems in terms of potential safety and tolerability, low frequency dosing, low overall costs and durable responses.
Early results from the first cohort of AD patients in ABATE showed that low dose ACI-24.060 could elicit an anti-Abeta antibody response as soon as week 6 (2 weeks after the second injection). The data show that ACI-24.060 vaccination has been safe and well tolerated to date. As a result, dosing in ABATE’s second, higher dose AD cohort has now begun and the trial is cleared to begin screening individuals with DS for part 2 of the study.
Dr. Andrea Pfeifer, CEO of AC Immune SA, commented: “We are delighted with the encouraging initial safety and immunogenicity findings for ACI-24.060 in ABATE reported today. We believe ACI-24.060’s successful development could provide patients with a novel therapeutic option offering numerous potential advantages in treatment, maintenance, and prevention settings. These early findings from ABATE represent an important step towards this goal, and we look forward to reporting more detailed data at a future conference.”
Dr. Johannes Streffer, CMO of AC Immune SA, commented: “ABATE’s innovative design includes interim Abeta PET imaging analyses that can be benchmarked against the levels of plaque clearance achieved with clinically-validated monoclonal antibodies. This will provide an opportunity for early de-risking of ACI-24.060 and potentially a rapid transition to a pivotal program. Moreover, the inclusion of cohorts of participants with DS in the trial positions us to potentially address the needs of a vastly underserved vulnerable population, virtually all of whom will develop amyloid plaques and AD. While looking forward to the trial’s continued advancement and upcoming data readouts, I want to thank the participants and investigators for their participation and support.”
About the Phase 1b/2 ABATE Study (ClinicalTrials.gov Identifier: NCT05462106)
The ABATE study is a Phase 1b/2, multicenter, adaptive, double-blind, randomized, placebo-controlled study to assess the safety, tolerability, immunogenicity, and pharmacodynamic effects of ACI-24.060 in subjects with prodromal Alzheimer’s disease and in adults with Down syndrome. All participants in the trial must have brain Abeta pathology confirmed by a positron emission tomography (PET) scan. The trial begins with a dose escalation phase in AD patients, during which various doses/dosing regimens may be evaluated, and also includes individuals with DS.
About ACI-24.060
ACI-24.060, derived from AC Immune’s SupraAntigen® platform, has been shown in preclinical studies to induce a strong polyclonal antibody response that matures and is maintained against both oligomeric and pyroglutamate-Abeta species, key pathological forms of Abeta believed to drive Abeta plaque formation and disease progression. ACI-24.060 is designed to enhance the formation of broad-spectrum protective antibodies with the same safety and tolerability previously demonstrated in the ACI-24 program in Phase 1 and 2 trials. This investigational candidate has the potential to efficiently inhibit plaque formation and increase plaque clearance, and thereby may reduce or prevent disease progression.
About AC Immune SA
AC Immune SA is a clinical-stage biopharmaceutical company that aims to become a global leader in precision medicine for neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and NeuroOrphan indications driven by misfolded proteins. The Company’s two clinically validated technology platforms, SupraAntigen® and Morphomer®, fuel its broad and diversified pipeline of first- and best-in-class assets, which currently features ten therapeutic and three diagnostic candidates, five of which are currently in Phase 2 clinical trials and one of which is in Phase 3. AC Immune has a strong track record of securing strategic partnerships with leading global pharmaceutical companies including Genentech, a member of the Roche Group, Eli Lilly and Company, and others, resulting in substantial non-dilutive funding to advance its proprietary programs and >$3 billion in potential milestone payments.
SupraAntigen® is a registered trademark of AC Immune SA in the following territories: AU, EU, CH, GB, JP, RU, SG and USA. Morphomer® is a registered trademark of AC Immune SA in CN, CH, GB, JP, KR, NO and RU.
The information on our website and any other websites referenced herein is expressly not incorporated by reference into, and does not constitute a part of, this press release.
![]()
Source: AC Immune SA
AC Immune rises ~10% as Alzheimer’s vaccine shows promise in early-stage trial
Jan. 26, 2023 7:51 AM ET
By: Ravikash, SA News Editor
- AC Immune (NASDAQ:ACIU) said its ACI-24.060 anti-amyloid beta (Abeta) vaccine for Alzheimer's disease (AD) showed positive initial interim safety and immunogenicity in a phase 1b/2 trial called ABATE.
- https://seekingalpha.com/news/3928320-ac-immune-rises-10-as-alzheimers-vaccine-shows-promise-in-early-stage-trial
- AC Immune SA (ACIU)
- https://www.acimmune.com/pipeline/
Breyanzi® (lisocabtagene maraleucel)
BXCL701 in combination with KEYTRUDA® (pembrolizumab)
Breyanzi® (lisocabtagene maraleucel)
Bristol Myers Squibb Announces TRANSCEND CLL 004 Trial of Breyanzi® (lisocabtagene maraleucel) Met Primary Endpoint of Complete Response Rate in Patients with Relapsed or Refractory Chronic Lymphocytic Leukemia
01/26/2023
CATEGORY:
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE: BMY) today announced topline results from TRANSCEND CLL 004, a Phase 1/2, open-label, single-arm, multicenter study evaluating Breyanzi (lisocabtagene maraleucel) in adults with relapsed or refractory (R/R) chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). Results from TRANSCEND CLL 004 showed the study met the primary endpoint of complete response rate compared to historical controlin the prespecified subset of patients with R/R CLL that was refractory to a BTK inhibitor and pretreated with a BCL-2 inhibitor. No new safety signals were reported for Breyanzi in this study.
“CLL is an incurable disease with complex biology and immune dysregulation that has made the development of T cell-based therapies that provide deep remission very challenging,” said Anne Kerber, senior vice president, head of Cell Therapy Development, Bristol Myers Squibb. “In a population that has limited options, the TRANSCEND CLL 004 study represents the first multicenter trial evaluating a CAR T cell therapy in heavily pre-treated patients with relapsed or refractory CLL or SLL, with results showing the potential of Breyanzi as a personalized one-time treatment approach for patients with this difficult-to-treat disease.”
Bristol Myers Squibb will complete a full evaluation of the TRANSCEND CLL 004 data and work with investigators to present detailed results at an upcoming medical meeting, as well as discuss these results with health authorities. Bristol Myers Squibb thanks the patients and investigators who are participating in the TRANSCEND CLL 004 clinical trial.
About TRANSCEND CLL 004
TRANSCEND CLL 004 (NCT03331198) is a Phase 1/2 open-label, single-arm, multicenter study evaluating Breyanzi in patients with relapsed or refractory chronic lymphocytic leukemia or small lymphocytic lymphoma. The Phase 1 dose escalation portion of the study assessed the safety and recommended dose for the subsequent Phase 2 expansion cohort. The Phase 2 portion of the study is evaluating Breyanzi at the recommended dose from the Phase 1 monotherapy arm. The primary endpoint of the Phase 2 portion of the study was complete response rate, including complete remission with incomplete bone marrow recovery, based on independent review committee according to the International Workshop on Chronic Lymphocytic Leukemia (iwCLL) 2018 guidelines.
About CLL and SLL
Chronic lymphocytic leukemia (CLL) is one of the most common types of leukemia in adults. In CLL, too many blood stem cells in the bone marrow become abnormal lymphocytes, and these abnormal cells have difficulty fighting infections. As the number of abnormal cells grows, there is less room for healthy white blood cells, red blood cells and platelets. Small lymphocytic lymphoma (SLL) also affects the lymphocytes, with cancer cells found mostly in the lymph nodes. While there are several treatments available for CLL and SLL, there is a need for additional effective therapies as there is no standard of care for relapsed or refractory CLL or SLL after prior therapy with targeted agents. Patients with relapsed or refractory disease have limited treatment options and generally experience shorter periods of response with each subsequent treatment.
About Breyanzi
Breyanzi is a CD19-directed CAR T cell therapy with a 4-1BB costimulatory domain, which enhances the expansion and persistence of the CAR T cells. Breyanzi is approved by the U.S. Food and Drug Administration (FDA) for the treatment of adult patients with large B-cell lymphoma (LBCL), including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B-cell lymphoma, primary mediastinal LBCL, and follicular lymphoma grade 3B who have refractory disease to first-line chemoimmunotherapy or relapse within 12 months of first-line chemoimmunotherapy, or refractory disease to first-line chemoimmunotherapy or relapse after first-line chemoimmunotherapy and are not eligible for hematopoietic stem cell transplant due to comorbidities or age, or relapsed or refractory disease after two or more lines of systemic therapy. Breyanzi is not indicated for the treatment of patients with primary central nervous system lymphoma. Please see the Important Safety Information section below, including Boxed WARNINGS for Breyanzi regarding cytokine release syndrome and neurotoxicity.
Breyanzi is also approved in Europe, Switzerland, Canada and Japan for relapsed and refractory LBCL after two or more lines of systemic therapy. Bristol Myers Squibb’s clinical development program for Breyanzi includes clinical studies in earlier lines of treatment for patients with relapsed or refractory LBCL and other types of lymphoma and leukemias. For more information, visit clinicaltrials.gov.
BREYANZI REMS
Because of the risk of CRS and neurologic toxicities, BREYANZI is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the BREYANZI REMS. The required components of the BREYANZI REMS are:
- Healthcare facilities that dispense and administer BREYANZI must be enrolled and comply with the REMS requirements.
- Certified healthcare facilities must have on-site, immediate access to tocilizumab.
- Ensure that a minimum of 2 doses of tocilizumab are available for each patient for infusion within 2 hours after BREYANZI infusion, if needed for treatment of CRS.
- Certified healthcare facilities must ensure that healthcare providers who prescribe, dispense, or administer BREYANZI are trained on the management of CRS and neurologic toxicities.
Further information is available at www.BreyanziREMS.com, or contact Bristol Myers Squibb at 1-888-423-5436.
Please see full Prescribing Information, including Boxed WARNINGS and Medication Guide.
Bristol Myers Squibb: Creating a Better Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision—transforming patients’ lives through science. The goal of the company’s cancer research is to deliver medicines that offer each patient a better, healthier life and to make cure a possibility. Building on a legacy across a broad range of cancers that have changed survival expectations for many, Bristol Myers Squibb researchers are exploring new frontiers in personalized medicine, and through innovative digital platforms, are turning data into insights that sharpen their focus. Deep scientific expertise, cutting-edge capabilities and discovery platforms enable the company to look at cancer from every angle. Cancer can have a relentless grasp on many parts of a patient’s life, and Bristol Myers Squibb is committed to taking actions to address all aspects of care, from diagnosis to survivorship. Because as a leader in cancer care, Bristol Myers Squibb is working to empower all people with cancer to have a better future.
Learn more about the science behind cell therapy and ongoing research at Bristol Myers Squibb here.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
Bristol Myers says trial for CAR T therapy met main goal in leukemia
Jan. 26, 2023 7:22 AM ET
Bristol-Myers Squibb Company (BMY)
By: Dulan Lokuwithana, SA News Editor
- Bristol Myers Squibb (NYSE:BMY) announced Thursday that a Phase 1/2 trial for its CAR T cell therapy Breyanzi reached the primary endpoint in adults with relapsed or refractory chronic lymphocytic leukemia (CLL).
- https://seekingalpha.com/news/3928300-bristol-myers-says-trial-car-t-therapy-met-main-goal-leukemia
- Bristol-Myers Squibb Company (BMY)
- https://www.breyanzi.com/
MRTX1133
BXCL701 in combination with KEYTRUDA® (pembrolizumab)
Breyanzi® (lisocabtagene maraleucel)
Mirati Announces IND Clearance by U.S. FDA Enabling Phase 1 Initiation for First-in-Class Oral KRASG12D Selective Inhibitor, MRTX1133
01/19/2023
IND demonstrates Mirati's leadership in KRAS, representing the Company's third KRAS or KRAS-signaling program to enter clinical development
SAN DIEGO, Jan. 19, 2023 /PRNewswire/ -- Mirati Therapeutics, Inc. (NASDAQ: MRTX), announced today the U.S. Food and Drug Administration (FDA) has cleared the Investigational New Drug (IND) application of MRTX1133, a potential first-in-class oral KRASG12D selective inhibitor for clinical evaluation. KRASG12D mutations impact approximately 180,000 patients in the US and Europe, representing approximately a 2.5-fold increase in prevalence compared to KRASG12C mutations. No targeted oncology treatment options currently exist for these patients.
MRTX1133 is a highly potent investigational inhibitor of the KRASG12D driver mutation and demonstrated selective and reversible inhibition of KRASG12D in both its active and inactive states. In addition, MRTX1133 administration resulted in marked tumor response in preclinical KRASG12D mutated pancreatic cancer models as well as lung and colorectal cancer models. MRTX1133 has demonstrated favorable properties including a low risk for off-target activity and drug interactions and a predicted human half-life of greater than 50 hours.
"The clearance by the FDA to initiate clinical evaluation of MRTX1133, the third program in our KRAS franchise to enter clinical development, is illustrative of the innovative approach to drug discovery and demonstrates the best-in-class capabilities of the Mirati team. This particular mutation has been difficult to target, and we are confident in our novel oral formulation strategy, which we believe will enable near-complete target inhibition over the full dosing interval," said James Christensen, Ph.D. chief scientific officer, Mirati Therapeutics, Inc. "We are thrilled to advance MRTX1133 into clinical development and the potential to positively impact people living with KRASG12D-mutated cancers."
The Phase 1/2 clinical trial will launch in early 2023 with plans for multiple expansion cohorts in pancreatic, colorectal, lung and other KRASG12D tumor types.
About Mirati Therapeutics, Inc.
Mirati Therapeutics, Inc. is a biotechnology company whose mission is to discover, design and deliver breakthrough therapies to transform the lives of patients with cancer and their loved ones. The company is relentlessly focused on bringing forward therapies that address areas of high unmet need, including lung cancer, and advancing a pipeline of novel therapeutics targeting the genetic and immunological drivers of cancer. Unified for patients, Mirati's vision is to unlock the science behind the promise of a life beyond cancer.
For more information about Mirati, visit us at Mirati.com or follow us on Twitter, LinkedIn and Facebook.
About MRTX1133
MRTX1133 is an investigational, highly potent, selective and reversible small molecule inhibitor of KRASG12D that is optimized to sustain near complete target inhibition with the potential to be both a first and best-in-class treatment option. MRTX1133 is entering Phase 1 clinical evaluation in 2023 investigating the drug's impact on KRASG12D-driven cancers. For more information visit Mirati.com/science.
View original content to download multimedia:https://www.prnewswire.com/news-releases/mirati-announces-ind-clearance-by-us-fda-enabling-phase-1-initiation-for-first-in-class-oral-krasg12d-selective-inhibitor-mrtx1133-301726331.html
SOURCE Mirati Therapeutics, Inc.
FDA clears Mirati's investigational new drug application for its inhibitor MRTX1133
Jan. 19, 2023 5:15 PM ET
Mirati Therapeutics, Inc. (MRTX)
By: Anuron Mitra, SA News Editor
- Mirati Therapeutics (NASDAQ:MRTX) on Thursday said the U.S. Food and Drug Administration had cleared its investigational new drug (IND) application for its inhibitor MRTX1133.
- https://seekingalpha.com/news/3926159-fda-clears-miratis-investigational-new-drug-application-for-its-inhibitor-mrtx1133
- Mirati Therapeutics, Inc. (MRTX)
- https://www.mirati.com/science/programs/kras-inhibitors/kras-g12d-inhibitor/
- https://www.mirati.com/
BXCL701 in combination with KEYTRUDA® (pembrolizumab)
BXCL701 in combination with KEYTRUDA® (pembrolizumab)
BXCL701 in combination with KEYTRUDA® (pembrolizumab)
BioXcel Therapeutics Announces Promising Top-Line Results from Phase 2 Trial of BXCL701 in Aggressive Form of Rare Prostate Cancer
Jan 11, 2023
Results demonstrate encouraging response rate of BXCL701 plus KEYTRUDA® (pembrolizumab) in patients with SCNC
Full data will be presented at the 2023 ASCO Genitourinary Cancers Symposium in February
NEW HAVEN, Conn., Jan. 11, 2023 (GLOBE NEWSWIRE) --
BioXcel Therapeutics, Inc. (Nasdaq: BTAI), a biopharmaceutical company utilizing artificial intelligence approaches to develop transformative medicines in neuroscience and immuno-oncology, today announced promising top-line data from its Phase 2 trial of BXCL701, the Company's investigational, oral innate immune activator, in combination with KEYTRUDA® (pembrolizumab) in small cell neuroendocrine metastatic castration-resistant prostate cancer (SCNC) patients. Full data have been submitted to the 2023 American Society of Clinical Oncology Genitourinary Cancers Symposium (ASCO GU).
“We are pleased that BXCL701 in combination with pembrolizumab has demonstrated an encouraging response rate in this difficult-to-treat cancer with no currently approved FDA therapies,” said Vincent J. O’Neill, M.D., Chief R&D Officer, OnkosXcel Therapeutics, a wholly owned subsidiary of BioXcel Therapeutics. “BXCL701’s promising profile as an oral innate immune activator with a large safety dataset and novel mechanism of action further supports OnkosXcel’s pipeline and use of BioXcel’s AI platform, and reinforces our confidence in BXCL701’s potential to enable checkpoint inhibitor therapy in traditionally cold cancers.”
SCNC represents a rare, underserved, growing patient population, with SCNC cases increasing due to earlier and more widespread use of androgen receptor inhibitors. In 2022, there were an estimated 268,5001 new prostate cancer patients, with approximately 10,740 patients progressing to SCNC.
The Phase 2a trial is an open-label, multicenter study to evaluate the safety and efficacy of BXCL701 in combination with pembrolizumab in men with SCNC. Eligibility criteria include histologically confirmed de novo or treatment-emergent SCNC, progression as defined by PCWG3 criteria, and at least 1 prior line of chemotherapy for locally advanced or metastatic prostate cancer. 28 evaluable SCNC patients received 0.3 mg of BXCL701 twice daily (BID) on days 1 through 14 of a 21-day cycle (0.2 mg BID the first week of Cycle 1) plus 200 mg of pembrolizumab administered intravenously on day 1 and every subsequent 21 days. The primary endpoint of the trial is a composite response rate defined as RECIST 1.1 and/or PSA50 and/or CTC count conversion. Secondary endpoints include duration of response, progression-free survival, overall survival, and biomarker evaluation as measured by changes in circulating cytokines and correlation of outcome with baseline tumor characteristics.
About BXCL701
BXCL701 is an investigational, oral innate immune activator designed to initiate inflammation in the tumor microenvironment. Approved and experimental immunotherapies often struggle to address cancers that appear “cold” or uninflamed. Therefore, BXCL701 may render “cold” tumors “hot,” making them more detectable by the adaptive immune system and thereby facilitating the development of a strong anti-cancer immune response. BioXcel Therapeutics’ preclinical data supports BXCL701’s synergy with both current checkpoint inhibitor-based therapies and emerging immunotherapies directed to activate T-cells. BXCL701 is currently being developed as a potential therapy for the treatment of aggressive forms of prostate cancer and advanced solid tumors that are refractory or treatment naïve to checkpoint inhibitors. BXCL701 has received Orphan Drug Designation from the U.S. Food & Drug Administration in four indications: acute myelogenous leukemia, pancreatic cancer, stage IIb to IV melanoma, and soft tissue sarcoma.
About OnkosXcel Therapeutics, LLC
OnkosXcel Therapeutics, LLC is a wholly owned subsidiary of BioXcel Therapeutics, Inc., focused on developing transformative medicines in oncology utilizing artificial intelligence approaches. The subsidiary was formed in 2022 to develop BXCL701, a Phase 2, investigational, oral innate immune activator for the treatment of aggressive forms of prostate cancer and advanced solid tumors that are refractory or treatment naïve to checkpoint inhibitors, as well as other immuno-oncology focused assets.
About BioXcel Therapeutics, Inc.
BioXcel Therapeutics, Inc., is a biopharmaceutical company utilizing artificial intelligence approaches to develop transformative medicines in neuroscience and immuno-oncology. The Company’s drug re-innovation approach leverages existing approved drugs and/or clinically validated product candidates together with big data and proprietary machine learning algorithms to identify new therapeutic indications. The Company’s commercial product, IGALMI™ (developed as BXCL501), is a proprietary, sublingual film formulation of dexmedetomidine approved for the acute treatment of agitation associated with schizophrenia or bipolar I or II disorder in adults. The safety and effectiveness of IGALMI have not been established beyond 24 hours from the first dose. For more information, please visit IGALMIhcp.com and also see the IGALMI full Prescribing Information. BXCL501 is under evaluation for at-home use for the acute treatment of agitation in bipolar and schizophrenia patients, for acute treatment of Alzheimer’s-related agitation, and as an adjunctive treatment for major depressive disorder. The safety and efficacy of BXCL501 for these uses have not been established. The Company is also developing BXCL502 as a potential therapy for chronic agitation in dementia. Under its subsidiary, OnkosXcel Therapeutics LLC, the Company is developing BXCL701, an investigational, oral innate immune activator for the treatment of aggressive forms of prostate cancer and advanced solid tumors that are refractory or treatment naïve to checkpoint inhibitors. The safety and efficacy of BXCL502 and BXCL701 have not been established. For more information, please visit bioxceltherapeutics.com.
Source: BioXcel Therapeutics, Inc.
BioXcel's BXCL701, Keytruda combo shows promise in mid-stage trial for prostate cancer
Jan. 11, 2023 7:33 AM ET
BioXcel Therapeutics, Inc. (BTAI), MRK
By: Ravikash, SA News Editor
- BioXcel Therapeutics (NASDAQ:BTAI) said its oral medicine BXCL701 in combination with Merck's (NYSE:MRK) Keytruda showed encouraging response rate in patients with a type of prostate cancer in a phase 2a trial.
- The study evaluated BXCL701 in combination with Keytruda (pembrolizumab) in men with small cell neuroendocrine metastatic castration-resistant prostate cancer (SCNC).
- In the trial, 28 evaluable patients received the drug combination. The main goal of the study is a composite response rate, while secondary goals include duration of response, progression-free survival, overall survival, and biomarker evaluation.
- https://seekingalpha.com/news/3923614-bioxcels-bxcl701-keytruda-combo-shows-promise-in-mid-stage-trial-for-prostate-cancer
- BioXcel Therapeutics, Inc. (BTAI), MRK
- https://www.bioxceltherapeutics.com/our-pipeline/
LP-284
IBI351 (KRASG12C Inhibitor)
BXCL701 in combination with KEYTRUDA® (pembrolizumab)
FDA Grants Lantern Pharma Orphan Drug Designation for Drug Candidate LP-284 in Mantle Cell Lymphoma
January 05, 2023 8:59am EST
- The Orphan Drug Designation strengthens LP-284’s clinical development path and provides the opportunity for additional market exclusivity and commercial protection.
- Lantern is anticipating filing the IND with the FDA and initiating a first-in-human Phase 1 trial for LP-284 in B-cell non-Hodgkin’s lymphomas (NHL), including mantle cell lymphoma (MCL), by mid 2023.
- In the US, MCL is diagnosed in approximately 4,500 patients each year and has an estimated annual market potential of $600 million.
DALLAS--(BUSINESS WIRE)-- Lantern Pharma Inc. (NASDAQ: LTRN), a clinical stage biopharmaceutical company using its proprietary RADR® artificial intelligence ("A.I.") and machine learning (“M.L.”) platform to transform the cost, pace, and timeline of oncology drug discovery and development, today announced that the U.S. Food and Drug Administration (FDA) has granted LP-284 Orphan Drug Designation (ODD) for the treatment of mantle cell lymphoma (MCL). MCL is a rare and aggressive form of B-cell non-Hodgkin's lymphoma (NHL) that is typically diagnosed at advanced stages in elderly patients. As nearly all MCL patients acquire resistance and relapse from treatment with standard-of-care (SOC) agents, there is an urgent and unmet clinical need for new and effective therapies to treat MCL.
LP-284 is a novel small molecule agent that preferentially damages DNA in cancer cells harboring mutations in DNA damage repair pathways. Lantern is developing LP-284 for several aggressive B-cell NHL’s, including MCL and double hit lymphoma (DHL), where LP-284 has shown potent anti-tumor activity in preclinical models. Lantern has been able to advance LP-284 from initial RADR® A.I. insights regarding anti-cancer activity and potential mechanisms of action in hematological cancers, to selection of specific subtypes of lymphomas with superior response, to late stage IND enabling studies and initial design of first in human clinical trials in less than 2 years.
"Receiving Orphan Drug Designation is an important milestone for our latest drug candidate, LP-284, and further validates our data-driven approach to oncology drug discovery and development” stated Panna Sharma, President & CEO of Lantern Pharma. "At ASH, we recently reported positive preclinical data demonstrating LP-284’s potent anti-tumor activity in new MCL tumors and also against tumors that had grown resistant to the MCL standard-of-care agents Ibrutinib and Bortezomib. These findings are critically pertinent due to the high relapse rate, and poor prognosis of the majority of MCL patients,” continued Sharma.
“This orphan designation is the fourth overall designation granted to Lantern, with the other three granted for our drug candidate LP-184. Acquiring these orphan designations is a key element of our business model as they provide a number of benefits including seven years of market exclusivity and eligibility for expedited drug development programs. Looking forward, these designations further position Lantern to advance our discussions with biopharma companies for partnering and collaborative development opportunities.”
The FDA's Office of Orphan Products Development grants orphan status to drugs intended for the safe and effective treatment, diagnosis or prevention of rare diseases or conditions affecting fewer than 200,000 people in the United States. ODD is designed to provide drug developers with various benefits to support the development of novel drugs, including market exclusivity for seven years upon FDA approval, eligibility for tax credits for qualified clinical trials, waiver of marketing registration application fees, reduced annual product fees, clinical protocol assistance and qualification for expedited development programs.
In addition to the ODD granted for LP-284 in MCL, Lantern was previously granted ODD’s by the FDA for its drug candidate LP-184 for the treatment of malignant gliomas, atypical teratoid rhabdoid tumors (ATRT), and pancreatic cancer. Lantern has also been granted a Rare Pediatric Disease Designation for LP-184 in ATRT.
About Lantern Pharma:
Lantern Pharma (NASDAQ: LTRN) is a clinical-stage oncology-focused biopharmaceutical company leveraging its proprietary RADR® A.I. and machine learning platform to discover biomarker signatures that identify patients most likely to respond to its pipeline of genomically-targeted therapeutics. Lantern is currently developing four drug candidates and an ADC program across 12 disclosed tumor targets, including two phase 2 programs. By targeting drugs to patients whose genomic profile identifies them as having the highest probability of benefiting from the drug, Lantern's approach represents the potential to deliver best-in-class outcomes.
FDA grants orphan drug designation to Lantern Pharma's lymphoma treatment candidate
Jan. 05, 2023 9:51 AM ET
By: Anuron Mitra, SA News Editor
- Lantern Pharma (NASDAQ:LTRN) on Thursday said the U.S. Food and Drug Administration (FDA) had granted an orphan drug designation to its LP-284 candidate for the treatment of mantle cell lymphoma (MCL).
- https://seekingalpha.com/news/3922371-fda-grants-orphan-drug-designation-to-lantern-pharmas-lymphoma-treatment-candidate
- Lantern Pharma Inc. (LTRN)
- https://www.lanternpharma.com/pipeline#lp284
VAX-24
IBI351 (KRASG12C Inhibitor)
IBI351 (KRASG12C Inhibitor)
Vaxcyte’s VAX-24 Granted FDA Breakthrough Therapy Designation for the Prevention of Invasive Pneumococcal Disease in Adults
January 5, 2023PDF Version
-- Breakthrough Therapy Designation for 24-Valent Investigational Pneumococcal Conjugate Vaccine Candidate Based on Positive Topline Proof-of-Concept Data Results in Adults Aged 18-64 That Suggest Potential Best-in-Class Profile --
-- Topline Safety, Tolerability and Immunogenicity Data from VAX-24 Phase 2 Study in Adults 65 and Older Expected in Q2 2023 --
-- Company Continues to Advance PCV Franchise, Including VAX-24 and VAX-31, While Progressing Early-Stage Vaccine Programs --
SAN CARLOS, Calif., Jan. 05, 2023 (GLOBE NEWSWIRE) -- Vaxcyte, Inc. (Nasdaq: PCVX), a clinical-stage vaccine innovation company engineering high-fidelity vaccines to protect humankind from the consequences of bacterial diseases, announced today that the U.S. Food and Drug Administration (FDA) granted Breakthrough Therapy designation for VAX-24, the Company’s investigational 24-valent pneumococcal conjugate vaccine (PCV) candidate for the prevention of invasive pneumococcal disease (IPD), in adults. The FDA’s decision was based on positive topline results from the Phase 1/2 proof-of-concept study, which evaluated the safety, tolerability and immunogenicity of VAX-24 in adults 18-64 years of age.
In the Phase 1/2 clinical study, VAX-24 met the primary safety and tolerability objectives, demonstrating a safety profile similar to Prevnar 20™ (PCV20) for all doses studied. The study also demonstrated that VAX-24 met or exceeded the established regulatory immunogenicity standards for all 24 serotypes at the conventional 2.2mcg dose, which the Company intends to move forward into a pivotal Phase 3 program. At this dose, VAX-24 met the standard opsonophagocytic activity response non-inferiority criteria for all 20 serotypes common with PCV20, of which 16 achieved higher immune responses.
“The FDA’s Breakthrough Therapy designation supports further acceleration of the VAX-24 development program in adults, while also providing validation of the potential of VAX-24 to deliver broader coverage and better immune responses relative to the standard of care,” said Grant Pickering, Chief Executive Officer and Co-Founder of Vaxcyte. “Our focus remains on advancing our VAX-24 clinical programs in both adults and infants and we anticipate announcing the topline data from the Phase 2 study in adults 65 and older in the second quarter of 2023.”
The FDA’s Breakthrough Therapy process is designed to expedite the development and review of drugs that are intended to treat a serious or life-threatening condition. The designation is based upon preliminary clinical evidence indicating that the drug or vaccine may demonstrate substantial improvement over available therapies on one or more clinically significant endpoints. With Breakthrough Therapy designation, Vaxcyte will have access to all of the elements of the FDA’s Fast Track program, as well as the ability to receive guidance and support from the FDA on an efficient drug development program and an organizational commitment from senior managers within the FDA.
“We are pleased to have received this important designation for VAX-24, which we believe underscores the public health need for broader protection from IPD, as well as the importance of innovative technology platforms in vaccine development, such as our cell-free, carrier-sparing approach,” said Jim Wassil, Executive Vice President and Chief Operating Officer of Vaxcyte. “In addition to our PCV franchise, comprising VAX-24 and VAX-31, our PCV candidate with 31 strains (formerly VAX-XP), we are also leveraging the XpressCF™ cell-free platform to develop earlier-stage vaccines, including VAX-A1 and VAX-PG, that are designed to prevent or treat bacterial infectious diseases and further demonstrate the full potential of our platform.”
Anticipated Key Milestones
Vaxcyte is advancing the clinical development of its PCV and early-stage programs with several anticipated key milestones, including:
VAX-24 Adult Program
- Topline safety, tolerability and immunogenicity data from the Phase 2 study in adults 65 and older are anticipated in the second quarter of 2023.
- Final results with the 6-month safety data from the two Phase 2 adult studies are anticipated in the first half of 2023.
- Following the receipt of the final safety reports from the two adult Phase 2 studies, regulatory interactions to inform the Phase 3 program are anticipated in the second half of 2023.
- Topline safety, tolerability and immunogenicity data from the pivotal Phase 3 non-inferiority study in adults are expected in 2025.
VAX-24 Pediatric Program
- The infant Investigational New Drug (IND) application submission and the Phase 2 study initiation are both anticipated in first half of 2023.
- Topline safety, tolerability and immunogenicity data from the infant Phase 2 study following the primary 3-dose immunization series are expected by 2025. The study design will include a primary immunization series consisting of three doses followed by a subsequent booster dose.
VAX-31 (Formerly VAX-XP) Adult Program
- The IND application submission for VAX-31 is anticipated in the second half of 2023.
- Topline safety, tolerability and immunogenicity data from a Phase 1/2 study in adults 18 years of age and older are expected in 2024.
VAX-A1
- Vaxcyte continues to advance the development of VAX-A1, a novel conjugate vaccine designed to prevent infections caused by Group A Strep bacteria, and further information about the anticipated timing of an IND application will be provided as the program progresses.
VAX-PG
- Vaxcyte nominated a final vaccine candidate for VAX-PG, its novel therapeutic vaccine designed to treat periodontal disease, in the fourth quarter of 2022 and continues to progress the program.
About VAX-24
VAX-24 is an investigational 24-valent PCV candidate designed to prevent IPD, which can be most serious for infants, young children, older adults and those with immune deficiencies or certain chronic health conditions. The public health community continues to affirm the need for vaccines that offer broader protection to prevent IPD. VAX-24 is intended to improve upon the standard-of-care PCVs for both children and adults by covering the serotypes that are responsible for most of the pneumococcal disease currently in circulation. Vaxcyte aims to efficiently create and deliver high-fidelity, broad-spectrum vaccines, such as VAX-24, by using modern synthetic techniques, including advanced chemistry and the XpressCF™ cell-free protein synthesis platform. Vaxcyte is deploying this approach with VAX-24 in order to add more pneumococcal strains without compromising the overall immune response.
About Vaxcyte
Vaxcyte is a vaccine innovation company engineering high-fidelity vaccines to protect humankind from the consequences of bacterial diseases. The Company is developing broad-spectrum conjugate and novel protein vaccines to prevent or treat bacterial infectious diseases. Vaxcyte’s lead candidate, VAX-24, is a 24-valent, broad-spectrum, carrier-sparing PCV being developed for the prevention of IPD. Vaxcyte is re-engineering the way highly complex vaccines are made through modern synthetic techniques, including advanced chemistry and the XpressCF™ cell-free protein synthesis platform, exclusively licensed from Sutro Biopharma, Inc. Unlike conventional cell-based approaches, the Company’s system for producing difficult-to-make proteins and antigens is intended to accelerate its ability to efficiently create and deliver high-fidelity vaccines with enhanced immunological benefits. Vaxcyte’s pipeline also includes VAX-31, a PCV with coverage of 31 strains; VAX-A1, a prophylactic vaccine candidate designed to prevent Group A Strep infections; and VAX-PG, a therapeutic vaccine candidate designed to slow or stop the progression of periodontal disease. Vaxcyte is driven to eradicate or treat invasive bacterial infections, which have serious and costly health consequences when left unchecked.
FDA grants breakthrough therapy designation to Vaxcyte's pneumococcal conjugate vaccine
Jan. 05, 2023 9:35 AM ETVaxcyte, Inc. (PCVX)By: Anuron Mitra, SA News Editor
- Vaxcyte (NASDAQ:PCVX) on Thursday said the U.S. Food and Drug Administration (FDA) had granted a breakthrough therapy designation to its pneumococcal conjugate vaccine (PCV) candidate VAX-24.
- https://seekingalpha.com/news/3922358-fda-grants-breakthrough-therapy-designation-to-vaxcytes-pneumococcal-conjugate-vaccine
- V Vaxcyte, Inc. (PCVX) Vaxcyte, Inc. (PCVX)
- https://vaxcyte.com/
- https://vaxcyte.com/pipeline/
IBI351 (KRASG12C Inhibitor)
IBI351 (KRASG12C Inhibitor)
IBI351 (KRASG12C Inhibitor)
- Innovent Announces NMPA’s Breakthrough Therapy Designation for IBI351 (KRASG12C Inhibitor) as Monotherapy for Previous Treated Advanced Non-small Cell Lung CancerPublished on: Jan 5th, 2023Back
- ROCKVILLE, U.S. and SUZHOU, China, January 5, 2023 - Innovent Biologics, Inc. (“Innovent”) (HKEX: 01801), a world-class biopharmaceutical company that develops, manufactures and commercializes high-quality medicines for the treatment of oncology, autoimmune, metabolic, ophthalmology and other major diseases, announced that the Center for Drug Evaluation (CDE) of China’s National Medical Products Administration (NMPA) has granted Breakthrough Therapy Designation (BTD) for IBI351 (GFH925) for the treatment of advanced non-small cell lung cancer patients with KRASG12C mutation that have received at least one prior line of systemic therapy.
- The NMPA BTD for IBI351 was based on the results from a phase I/II trial (CDE Registration No. CTR20211933). This study aims to evaluate the safety, tolerability and efficacy of IBI351 monotherapy in patients with advanced solid tumors who failed or intolerant to standard of care treatment.
- The latest results of IBI351 from the phase I study were presented at the 2022 Chinese Society of Clinical Oncology (CSCO) Annual Meeting. As data cutoff (29 July 2022), of 55 evaluable NSCLC patients, the investigator assessed objective response rate (ORR) was 50.9% and disease control rate (DCR) was 92.7%. Of 21 patients with NSCLC treated at 600mg BID (the recommended phase 2 dose), better efficacy signal was observed, with investigator assessed ORR 61.9% and DCR 100%. Median duration of response (DOR) and median progression free survival (PFS) were not reached yet.
As data cutoff date, IBI351 was well tolerated. No DLT was reported and MTD was not reached. Treatment-related adverse events (TRAEs) occurred in 92.5% (62/67) patients and the most common TRAEs were anemia, transferase increased, bilirubin increased, pruritus and fatigue. The majority of the TRAEs were grade 1-2 with 19.4% (13/67) of patients reporting grade 3 or higher TRAEs. There were no grade 5 TRAEs or TRAEs led to treatment discontinuation.
Favorable safety and tolerability and promising antitumor activity of IBI351 monotherapy were observed. The single-arm registrational trial of IBI351 monotherapy in previously-treated advanced non-small cell lung cancer patients with KRASG12C mutation is ongoing. Relevant updated study results will be published at an upcoming medical conference in 2023.
“We are glad to see the NMPA grants Breakthrough Therapy Designation based on the results of Phase I data of IBI351,” said Dr. Hui Zhou, Senior Vice President of Innovent. “KRASG12C mutated NSCLC patients have limited treatment options. IBI351 demonstrated encouraging efficacy and safety data in Phase I study. A single arm registrational trial of IBI351 monotherapy in previously-treated advanced NSCLC is ongoing. We are working to advance into late stage clinical development to explore the potential of IBI351 as monotherapy and in combo-therapy.”
NMPA Breakthrough Therapy Designation is intended to facilitate and expedite the development and review of an investigational drug to treat a serious disease or condition when preliminary clinical evidence indicates that the drug has demonstrated substantial improvement over current therapies. The BTD will not only qualify a drug candidate to receive status for rapid review by the CDE, but it will also allow the sponsor to obtain timely advice and communication from the CDE to accelerate the approval and launch to address the unmet clinical need of patients at an accelerated pace. Click here for the published list of drugs which have been granted BTD by NMPA.
About Non-small Cell Lung Cancer
Lung cancer is one of the malignancies with the highest incidence and mortality worldwide, among which non-small cell lung cancer (NSCLC) is the most common pathological type, accounting for about 85% of all lung cancers. KRAS mutations are common driver gene mutations in NSCLC, most of which occur in lung adenocarcinoma. KRAS mutations rarely co-exist with driver mutations such as EGFR and ALK, and patients with advanced NSCLC with KRASG12C mutations are often unable to benefit from the multiple drugs already on the market that target these mutations or rearrangements. After the progress of first-line standard treatment in this population, there are limited second-line treatment options with low effective rate and poor prognosis.
About IBI351/GFH925(KRASG12C Inhibitor)
Discovered by GenFleet Therapeutics, GFH925 (Innovent R&D code: IBI351) is a novel, orally active, potent KRASG12C inhibitor designed to effectively target the GTP/GDP exchange, an essential step in pathway activation, by modifying the cysteine residue of KRASG12C protein covalently and irreversibly. Preclinical cysteine selectivity studies demonstrated high selectivity of IBI351 towards KRASG12C. Subsequently, IBI351 effectively inhibits the downstream signal pathway to induce tumor cells’ apoptosis and cell cycle arrest.
In September 2021, Innovent and GenFleet Therapeutics entered into an exclusive license agreement for the development and commercialization of IBI351 in China (including mainland China, Hong Kong, Macau and Taiwan) with additional option-in rights for global development and commercialization.
About Innovent
Inspired by the spirit of "Start with Integrity, Succeed through Action," Innovent's mission is to develop, manufacture and commercialize high-quality biopharmaceutical products that are affordable to ordinary people. Established in 2011, Innovent is committed to developing, manufacturing and commercializing high-quality innovative medicines for the treatment of cancer, autoimmune disease, metabolic disorder and other major diseases. On October 31, 2018, Innovent was listed on the Main Board of the Stock Exchange of Hong Kong Limited with the stock code: 01801.HK.
Since its inception, Innovent has developed a fully integrated multi-functional platform which includes R&D, CMC (Chemistry, Manufacturing, and Controls), clinical development and commercialization capabilities. Leveraging the platform, the company has built a robust pipeline of 36 valuable assets in the fields of cancer, metabolic disorder, autoimmune disease and other major therapeutic areas, with 8 approved products on the market. These include: TYVYT® (sintilimab injection), BYVASDA® (bevacizumab biosimilar injection), SULINNO® (adalimumab biosimilar injection), HALPRYZA® (rituximab biosimilar injection) , Pemazyre® (pemigatinib oral inhibitor), olverembatinib (BCR-ABL TKI) , Cyramza® (ramucirumab) and Retsevmo® (selpercatinib). An additional 2 assets are under NMPA NDA review, 6 assets are in Phase 3 or pivotal clinical trials, and 20 more molecules are in clinical studies.
Innovent has built an international team with advanced talent in high-end biological drug development and commercialization, including many global experts. The company has also entered into strategic collaborations with Eli Lilly and Company, Sanofi, Adimab, Incyte, MD Anderson Cancer Center and other international partners. Innovent strives to work with many collaborators to help advance China's biopharmaceutical industry, improve drug availability and enhance the quality of the patients' lives. For more information, please visit: www.innoventbio.com. and www.linkedin.com/company/innovent-biologics/.
Innovent wins China’s breakthrough therapy status for KRASG12C Inhibitor
Jan. 05, 2023 6:48 AM ET
Innovent Biologics, Inc. (IVBIY), IVBXF
By: Dulan Lokuwithana, SA News Editor
- Innovent Biologics (OTCPK:IVBIY) (OTCPK:IVBXF) announced that China's Center for Drug Evaluation (CDE) issued Breakthrough Therapy Designation (BTD) for its KRASG12C inhibitor IBI351 (GFH925) as a treatment for advanced non-small-cell-lung cancer (NSCLC).
- https://seekingalpha.com/news/3922252-innovent-wins-chinas-breakthrough-therapy-status-for-krasg12c-inhibitor
- Innovent Biologics, Inc. (IVBIY), IVBXF
- https://www.innoventbio.com/
- https://www.innoventbio.com/ScienceAndProducts/Pipeline
biotecHOPE™ 2022
BT8009
fidanacogene elaparvovec
fidanacogene elaparvovec
CAMBRIDGE, England & BOSTON--(BUSINESS WIRE)--Jan. 4, 2023--
Bicycle Therapeutics plc (NASDAQ:BCYC), a biotechnology company pioneering a new and differentiated class of therapeutics based on its proprietary bicyclic peptide (Bicycle®) technology, today announced that the United States Food and Drug Administration (FDA) has granted Fast Track Designation (FTD) to Bicycle’s BT8009 monotherapy for the treatment of adult patients with previously treated locally advanced or metastatic urothelial cancer. BT8009 is a potential first in class Bicycle Toxin Conjugate (BTC®) targeting Nectin-4, a protein that is highly expressed in urothelial cancer (UC) and other solid tumors.
“FTD represents another positive step in the development of BT8009 and reflects the pressing need for a clinically meaningful, differentiated therapy compared to what is available for patients,” said Kevin Lee, Ph.D., Chief Executive Officer. “We believe this designation is a valuable component of our future clinical and regulatory strategy as we work to align with the FDA to address the pressing unmet needs of people living with urothelial cancer.”
FTD is intended to facilitate and expedite development and review of new drugs to address unmet medical need in the treatment of a serious or life-threatening condition. This unmet medical need is defined as providing a therapy where either none exists or providing a therapy which may prove superior to existing therapy. A clinical program that receives FTD may benefit from more frequent meetings and communications with the FDA to discuss development plans and ensure the collection of appropriate data needed to support approval. Clinical programs conducted under FTD may be eligible for Accelerated Approval and Priority Review if relevant criteria are met. More information on the Fast Track process is available here.
About Bicycle Therapeutics
Bicycle Therapeutics (NASDAQ: BCYC) is a clinical-stage biopharmaceutical company developing a novel class of medicines, referred to as Bicycles, for diseases that are underserved by existing therapeutics. Bicycles are fully synthetic short peptides constrained with small molecule scaffolds to form two loops that stabilize their structural geometry. This constraint facilitates target binding with high affinity and selectivity, making Bicycles attractive candidates for drug development. Bicycle is evaluating BT5528, a second-generation Bicycle Toxin Conjugate (BTC®) targeting EphA2; BT8009, a second-generation BTC targeting Nectin-4, a well-validated tumor antigen; and BT7480, a Bicycle TICA® targeting Nectin-4 and agonizing CD137, in company-sponsored Phase I/II trials. In addition, BT1718, a BTC that targets MT1-MMP, is being investigated in an ongoing Phase I/IIa clinical trial sponsored by the Cancer Research UK Centre for Drug Development. Bicycle is headquartered in Cambridge, UK, with many key functions and members of its leadership team located in Lexington, MA. For more information, visit bicycletherapeutics.com.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230104005096/en/
Source: Bicycle Therapeutics plc
Bicycle Therapeutics adds 10% on FDA’s fast track tag for bladder cancer therapy
Jan. 04, 2023 7:52 AM ET
Bicycle Therapeutics plc (BCYC)
By: Dulan Lokuwithana, SA News Editor
- Clinical-stage biotech Bicycle Therapeutics (NASDAQ:BCYC) jumped ~10% pre-market Wednesday after announcing that the FDA granted Fast Track Designation for its experimental bladder cancer therapy BT8009.
- hhttps://www.bicycletherapeutics.com/ttps://seekingalpha.com/news/3921890-bcyc-stock-gains-fdas-fast-track-tag-for-bladder-cancer-therapy
- Bicycle Therapeutics plc (BCYC)
- https://www.bicycletherapeutics.com/programs/bicycle-conjugates/
fidanacogene elaparvovec
fidanacogene elaparvovec
fidanacogene elaparvovec
Pfizer Announces Positive Top-Line Results from Phase 3 Study of Hemophilia B Gene Therapy Candidate
Thursday, December 29, 2022 - 06:45amOpen in tab
NEW YORK--(BUSINESS WIRE)-- Pfizer Inc. (NYSE: PFE) today announced positive top-line results from the Phase 3 BENEGENE-2 study (NCT03861273) evaluating fidanacogene elaparvovec, an investigational gene therapy, for the treatment of adult males with moderately severe to severe hemophilia B.
The BENEGENE-2 study met its primary endpoint of non-inferiority and superiority in the annualized bleeding rate (ABR) of total bleeds post-fidanacogene elaparvovec infusion versus prophylaxis regimen with Factor IX (FIX), administered as part of usual care. The results demonstrated superiority with a mean ABR for all bleeds of 1.3 for the 12 months from week 12 to month 15 compared to an ABR of 4.43 during the lead-in pre-treatment period of at least six months, resulting in a 71% reduction in ABR (p<0.0001) after a single dose of 5e11 vg/kg of fidanacogene elaparvovec. Key secondary endpoints demonstrated a 78% reduction in treated ABR (p=0.0001) and a 92% reduction in annualized infusion rate (p<0.0001). Mean FIX activity was 27% at 15 months by one-stage SynthASil assay and 25% at 24 months. The mean steady-state FIX:C was significantly higher than the pre-specified threshold of 5% (p<0.0001).
Fidanacogene elaparvovec was generally well-tolerated, with a safety profile consistent with Phase 1/2 results. Fourteen serious adverse events (SAEs) were reported in seven (16%) patients, with two assessed as related to treatment, a duodenal ulcer hemorrhage occurring in the setting of corticosteroid use, and an immune-mediated elevation of liver aminotransferase levels. No deaths, SAEs associated with infusion reactions, thrombotic events, or FIX inhibitors were reported.
Fidanacogene elaparvovec is a novel, investigational vector that contains a bio-engineered adeno-associated virus (AAV) capsid (protein shell) and a high-activity human coagulation FIX gene. The goal of this gene therapy for people living with hemophilia B, once treated, is that they will be able to produce FIX via this one-time treatment rather than having to regularly receive exogenous FIX. In this Phase 3 trial, eligible study participants (n=45) completed a minimum six months of routine exogeneous FIX prophylaxis therapy during the lead-in study (NCT03587116) and then received one intravenous dose of fidanacogene elaparvovec at a dose of 5e11 vg/kg. Participants in the BENEGENE-2 study were screened with a validated assay designed to identify individuals who test negative for neutralizing antibodies to the gene therapy vector. Clinical trial participants will be evaluated as part of a long-term study over the course of 15 years.
“Pfizer has more than 30 years of experience in developing and commercializing therapies for hematological disorders, and a deep understanding of the significant challenges that people living with hemophilia continually face. We are proud to advance the latest innovation for people living with hemophilia B and are encouraged by the potential of this investigational gene therapy,” said Chris Boshoff, M.D., Ph.D., Chief Development Officer, Oncology and Rare Disease, Pfizer Global Product Development. “We are extremely appreciative of those who are participating in the trial and to the investigators contributing to this innovative research as we work to unlock the full potential of gene therapies for people living with hemophilia.”
Pfizer currently has three Phase 3 programs investigating gene therapy in populations where there is a high unmet need: hemophilia B, hemophilia A, and Duchenne muscular dystrophy. A Phase 3 trial is also ongoing investigating marstacimab, a potential novel subcutaneous therapy option being studied for the treatment of people with hemophilia A and B with and without inhibitors.
“The burden people living with hemophilia B face is significant, with many receiving routine infusions or injections which can interfere with their ability to take part in day-to-day activities that many take for granted,” said Adam Cuker, M.D., M.S., Director, Penn Comprehensive and Hemophilia Thrombosis Program. “The BENEGENE-2 data demonstrate the promise of this gene therapy candidate as a potential one-time option for people living with hemophilia B as a means of reducing the clinical and treatment burden over the long term.”
Fidanacogene elaparvovec has been granted breakthrough, regenerative medicines advance therapy (RMAT), and orphan drug designations from the US Food and Drug Administration, as well as PRIority MEdicines (PRIME) and orphan drug designation from the European Medicines Agency. Pfizer will discuss these data with regulatory authorities in early 2023.
Additional key data will be presented at a scientific conference in early 2023 as well.
About fidanacogene elaparvovec
Fidanacogene elaparvovec is a novel, investigational gene therapy that contains a bio-engineered AAV capsid and a high-activity human coagulation FIX gene. The goal of this investigational treatment for people living with hemophilia B, once treated, is that they will be able to produce FIX themselves via this one-time treatment rather than having to receive exogenous FIX.
Pfizer licensed SPK-9001 (fidanacogene elaparvovec), from Spark Therapeutics pursuant to a December 2014 agreement under which Spark Therapeutics was responsible for conducting all Phase 1/2 studies for the investigational gene therapy while Pfizer assumed responsibility for pivotal studies, any regulatory activities, and potential global commercialization.
View source version on businesswire.com: https://www.businesswire.com/news/home/20221229005024/en/
Pfizer:
Source: Pfizer Inc.
Pfizer says hemophilia B gene therapy met key goal in Phase 3 trial
Dec. 29, 2022 7:08 AM ET
Pfizer Inc. (PFE), RHHBY, RHHBF
By: Dulan Lokuwithana, SA News Editor1 Comment
Pfizer (NYSE:PFE) announced Thursday that the company’s investigational gene therapy for hemophilia B, fidanacogene elaparvovec, met the primary endpoint in a Phase 3 trial called BENEGENE-2 involving adults males with a moderately severe to severe form of the disease.
Pfizer Inc. (PFE), RHHBY, RHHBF
https://www.pfizer.com/science/drug-product-pipeline
GTX-102
fidanacogene elaparvovec
Renazorb (lanthanum dioxycarbonate)
Acasti Announces Preliminary Topline Results Met All Outcome Measures in the Pharmacokinetic Bridging Study for GTX-102, the Company’s Drug Candidate for the Treatment of Ataxia Telangiectasia
December 28, 2022
LAVAL, Québec, Dec. 28, 2022 (GLOBE NEWSWIRE) -- Acasti Pharma Inc. (“Acasti” or the “Company”) (Nasdaq: ACST and TSX-V: ACST), a late-stage, specialty pharma company advancing three clinical stage drug candidates addressing rare and orphan diseases, announces that the preliminary topline results of the pharmacokinetic (PK) bridging study for GTX-102 met all outcome measures. The objectives of the study were to evaluate the bioavailability, pharmacokinetics, and safety of GTX-102, a novel, concentrated oral-mucosal metered spray of betamethasone in healthy volunteers. This new formulation is intended to improve the neurological symptoms of Ataxia Telangiectasia (A-T) in a pediatric population for which there are currently no FDA-approved therapies. GTX-102 can be sprayed conveniently over the tongue of A-T patients, who often have difficulties swallowing. This PK study was the next step in the proposed 505(b)(2) regulatory pathway for GTX-102.
Jan D’Alvise, Chief Executive Officer of Acasti, stated, “The completion of this PK bridging study is an important milestone in the advancement of our GTX-102 program designed to provide a new and convenient therapy for treating the chronic symptoms of A-T in children with this rare genetic disorder. We are very pleased to report the results of this study, which we expect will now support the advancement of the program directly into Phase 3. Currently there are no drugs approved for A-T, and we are pleased to report the topline findings of this pivotal study as we remain committed to bring this exciting and proprietary treatment to children who suffer from A-T.”
This PK bridging study is a Phase 1, randomized, open-label, crossover study in healthy adult subjects to evaluate the comparative bioavailability, PK, and safety of GTX-102 administered as an oral spray compared to intramuscular (IM) betamethasone (which is expected to be the reference product for bridging purposes), and to an oral solution (OS) of betamethasone, which is available in Europe but not approved in the US. The betamethasone OS was shown to reduce neurological symptoms in children with A-T in a published multicenter, double-blind, randomized, placebo-controlled crossover trial conducted in Italy (Zannolli et al, 2012).
The primary objective of this PK bridging study was to evaluate and characterize the PK profile of GTX-102 as an oral spray. Details of the study design can be found on ClinicalTrials.gov (Identifier: NCT05531890).
A total of 48 healthy adult subjects (27 males and 21 females) were enrolled in this single center, 5-treatment, 8-sequence, 2-period cross-over study. The 5 treatments assessed in the study were:
- GTX-102: low dose at 0.0125 mg/kg, medium dose at 0.05 mg/kg, and high dose at 0.1 mg/kg
- OS betamethasone at 0.1 mg/kg
- IM betamethasone at 0.1 mg/kg
Each subject received a single dose of 2 treatments in a cross-over fashion, in a randomized sequence over 2 treatment periods separated by 15 days. The dosing started on September 13, 2022 and ended on November 24, 2022. Betamethasone blood levels were compared between all treatment groups.
GTX-102 PK study outcome measures definitions and preliminary topline findings are as follows:
- Primary outcome measures and their definitions include:
- AUC0-72 is the area under the concentration time curve up to 72 hours post-dose
- AUC∞ is the area under the concentration time curve extrapolated to infinity
- Cmax is the maximum concentration occurring between 0 hour to 72 hours after study drug administration.
- GTX-102 given at doses of 0.0125 (low), 0.5 (medium) or 0.1 (high) mg/kg, showed betamethasone blood concentrations that were highly predictable and consistent based on AUC and Cmax, indicating good linearity and dose-proportionality.
- Following the high dose of GTX-102 (0.1 mg/kg), betamethasone blood concentrations were within the same range of exposure as IM betamethasone (0.1 mg/kg), based on AUC. The IM formulation of betamethasone will serve as a bridge for GTX-102 in the context of the proposed 505(b)(2) regulatory pathway.
- In addition, Betamethasone blood concentrations following the high dose of GTX-102 (0.1 mg/kg) were within the same range of exposure as OS betamethasone (0.1 mg/kg), based on AUC. This OS formulation was the same one that was used by Zannolli et al and may serve as a clinical comparator for further clinical development of GTX-102.
- There was statistically no significant difference (p>0.05) between GTX-102 (0.05 mg/kg) when comparing a fast rate of administration (each spray immediately following the preceding one) to a slow rate (1 spray/minute), as indicated by Cmax and AUC. This is important because being able to use the fast or the slow rate of administration may provide greater flexibility for patients and caregivers.
- The Cmax of GTX-102 was within the same range of exposure as the OS, but the Cmax for the IM formulation was lower than both GTX-102 and the OS, as well as what has been reported previously for the IM in the literature. It is important to note that achieving bioequivalence with the IM was not an objective of this study, nor was it expected.
- No serious adverse events (AE) were reported during the study. AEs leading to study discontinuation consisted of cough/fever/body pain/stuffy nose (1 case), Covid-19 (1 case) and elevated creatinine kinase (1 case), and all events occurred prior to receiving the second treatment. None were judged as being related to the study drugs by the investigator. The most frequent drug-related AE was mild headache (4 cases).
- Based on this data, Acasti will work with our clinical experts and FDA to determine the best final dosing regimen for GTX-102 to incorporate into our Phase 3 study design.
D’Alvise concluded, “With the completion of this important comparative PK bridging study, we are confident that the expected final development step for GTX-102 will be to conduct a Phase 3 safety and efficacy trial in A-T patients using a treatment regimen similar to the one already proved effective by Zannolli, et al. We plan to request a Type B meeting with the FDA following the receipt of the full PK study dataset sometime in calendar H1 2023 to confirm the proposed Phase 3 study design. If all proceeds as planned, the Phase 3 study is expected to be initiated in the second half of calendar 2023. If the Phase 3 program meets the primary endpoints, an NDA filing for GTX-102 under Section 505(b)(2) is expected to follow.”
About A-T
A-T is a progressive, genetic, neurodegenerative disorder that primarily effects young children, causing severe disability, impairment of the immune system and an increasing susceptibility to infections and cancer. The hallmark symptoms of A-T are cerebellar ataxia and other motor dysfunction, and dilated blood vessels (telangiectasia) that occur in the sclera of the eyes and on the skin. Children begin to experience balance and coordination problems when they begin to walk (toddler age), and ultimately become wheelchair bound in their second decade of life. In pre-adolescence (age 5-8 years), patients experience oculomotor apraxia, dysarthria, and dysphagia. They often develop compromised immune systems and are at increased risk of developing respiratory tract infections and cancer (typically lymphomas and leukemia). Patients typically die by age 25 years from complications of lung disease or cancer.
A-T is diagnosed through a combination of clinical assessments, laboratory analysis, and genetic testing. There is no known treatment to slow disease progression, and treatments that are used are strictly aimed at symptoms (e.g., physical, occupational or speech therapy for neurologic issues), or conditions secondary to the disease (e.g., antibiotics for lung infections, chemotherapy for cancer, etc.).
A market research study commissioned by Acasti found that A-T affects approximately 4,300 patients per year in the United States and has a potential total addressable market of $150 million, based on the number of treatable patients (as disclosed in Acasti’s most recently filed quarterly report on Form 10-Q).
About Acasti
Acasti is a late-stage specialty pharma company with drug delivery technologies and drug candidates addressing rare and orphan diseases. Acasti’s novel drug delivery technologies have the potential to improve the performance of currently marketed drugs by achieving faster onset of action, enhanced efficacy, reduced side effects, and more convenient drug delivery—all which could help to increase treatment compliance and improve patient outcomes. Acasti’s three lead clinical assets have each been granted Orphan Drug Designation by the FDA, which provide the assets with seven years of marketing exclusivity post-launch in the United States, and additional intellectual property protection with over 40 granted and pending patents. Acasti’s lead clinical assets target underserved orphan diseases: (i) GTX-104, an intravenous infusion targeting Subarachnoid Hemorrhage (SAH), a rare and life threatening medical emergency in which bleeding occurs over the surface of the brain in the subarachnoid space between the brain and skull; (ii) GTX-102, an oral mucosal spray targeting Ataxia-telangiectasia (A-T), a progressive, neurodegenerative genetic disease that primarily affects children, causing severe disability, and for which no treatment currently exists; and (iii) GTX-101, a topical spray targeting Postherpetic Neuralgia (PHN), a persistent and often debilitating neuropathic pain caused by nerve damage from the varicella zoster virus (shingles), which may persist for months and even years.
For more information, please visit: https://www.acasti.com/en.
Source: Acasti Pharma, Inc.
Released December 28, 2022
Acasti soars ~15% as phase 1 bridging study of neurodegenerative disorder drug shows promise
Dec. 28, 2022 9:07 AM ET
Acasti Pharma Inc. (ACST), ACST:CA
By: Ravikash, SA News Editor
Acasti Pharma (NASDAQ:ACST) said results from a pharmacokinetic (PK) phase 1 bridging study of GTX-102 met all outcome measures.
Renazorb (lanthanum dioxycarbonate)
Renazorb (lanthanum dioxycarbonate)
Renazorb (lanthanum dioxycarbonate)
Unicycive Achieves Primary Endpoint in Pivotal Bioequivalence Study of Renazorb
December 28, 2022 8:30am EST Download as PDF
Renazorb demonstrates pharmacodynamic bioequivalence to Fosrenol
Renazorb’s enhanced product profile features reduced pill burden and small, swallowable tablets, which may improve patient compliance
On track to file New Drug Application mid-2023
LOS ALTOS, Calif., Dec. 28, 2022 (GLOBE NEWSWIRE) -- Unicycive Therapeutics, Inc. (Nasdaq: UNCY), a clinical-stage biotechnology company developing therapies for patients with kidney disease, today announced that the primary endpoint was met in the Company’s pivotal bioequivalence (BE) study comparing Renazorb to Fosrenol®. Based on the topline results, pharmacodynamic (PD) BE of Renazorb to Fosrenol was established and met the regulatory criteria for PD BE in the healthy volunteer BE study.
Renazorb is an investigational phosphate binding agent utilizing proprietary nanoparticle technology that is being developed to treat hyperphosphatemia in chronic kidney disease (CKD) patients on dialysis. If approved, Renazorb may dramatically reduce the pill burden that patients endure with currently available medications. The global market opportunity for treating hyperphosphatemia is projected to be in excess of $2.5 billion in 2022, with the United States accounting for more than $1 billion of that total. Despite the availability of several U.S. Food and Drug Administration (FDA)-cleared medications, 75 percent of U.S. dialysis patients fail to achieve the target phosphorus levels recommended by published medical guidelines. Market research indicates that the top reason for this significant unmet medical need is related to the high pill burden, which leads to poor patient compliance.
Unicycive previously received confirmatory guidance from the FDA that this single BE study in healthy volunteers would satisfy all clinical regulatory requirements and that no other clinical studies would be required for a New Drug Application (NDA) filing through the 505(b)(2) pathway.
Today's positive results are from a randomized, open-label, two-way crossover BE study to establish PD BE between Renazorb and Fosrenol. The study enrolled 40 subjects per treatment arm. The study design, including the dose, primary endpoint, and sample size, was reviewed, and aligned by the FDA before the initiation of the study.
"We are delighted with the successful outcome of our registrational BE study of Renazorb. This is a major milestone for Unicycive that brings us one step closer to obtaining market approval for Renazorb to treat hyperphosphatemia,” said Shalabh Gupta, M.D., Chief Executive Officer of Unicycive. “Our R&D team has extensive experience filing NDA submissions and a demonstrated track record of multiple product approvals from the FDA. We look forward to filing the NDA for Renazorb in mid-2023 and for its potential approval in order to benefit the multitude of hyperphosphatemia patients who are not well served by current treatment options.”
The primary outcome measure of the BE study was Least Square (LS) mean change in urinary phosphate excretion (in mg/day) from baseline to the evaluation period (PD variable). Based on the mixed-effect linear model, the 90% Confidence Interval (CI) was constructed for the difference in PD variable for Renazorb and Fosrenol. In addition, the acceptable range was defined as ± 20% of the LS mean of the PD variability for Fosrenol. PD BE was achieved because the 90% CI was completely contained within the acceptable range.
About Renazorb (lanthanum dioxycarbonate)
Renazorb is an investigational next-generation lanthanum-based phosphate binding agent utilizing proprietary nanoparticle technology being developed for the treatment of hyperphosphatemia in patients with chronic kidney disease (CKD). Its potential best-in-class profile has meaningful patient adherence benefits over currently available treatment options as it requires smaller and fewer number of pills per dose and is swallowed instead of chewed.
https://unicycive.com/focus/renazorb/
About Unicycive Therapeutics
Unicycive Therapeutics is a biotechnology company developing novel treatments for kidney diseases. Unicycive’s lead drug, Renazorb, is a novel phosphate binding agent being developed for the treatment of hyperphosphatemia. UNI-494 is a patent-protected new chemical entity in late preclinical development for the treatment of acute kidney injury. For more information, please visit www.unicycive.com.
Source: Unicycive Therapeutics, Inc.
Released December 28, 2022
Unicycive jumps 25% as kidney disease drug meets main goal in key trial
Dec. 28, 2022 8:57 AM ET
Unicycive Therapeutics, Inc. (UNCY)TAK
By: Dulan Lokuwithana, SA News Editor
- Nano-cap biotech Unicycive Therapeutics (NASDAQ:UNCY) added ~25% pre-market Wednesday after announcing that its pivotal bioequivalence (BE) study for kidney disease therapy Renazorb met the primary goal.
- https://seekingalpha.com/news/3920905-uncy-stock-jumps-as-kidney-disease-drug-meets-main-goal-in-key-trial
- Unicycive Therapeutics, Inc. (UNCY)
- https://unicycive.com/focus/renazorb/
GS-1811 (formerly JTX-1811)
Renazorb (lanthanum dioxycarbonate)
Olpruva (sodium phenylbutyrate)
Gilead To Acquire All Remaining Rights To Potential First-In-Class Immunotherapy GS-1811 From Jounce Therapeutics
-- Agreement Covers Buyout of Remaining Financial Obligations for Anti-CCR8 Antibody in Development as a Potential Treatment for Solid Tumors --
FOSTER CITY, Calif. and CAMBRIDGE, Mass., Dec. 27, 2022 (GLOBE NEWSWIRE) -- Gilead Sciences, Inc. (Nasdaq: GILD) and Jounce Therapeutics, Inc. (Nasdaq: JNCE) amended their existing license agreement for GS-1811 (formerly JTX-1811), enabling Gilead to buyout remaining contingent payments potentially due under the license agreement executed in August 2020. As part of the transaction, certain operational obligations of the parties related to GS-1811, an anti-CCR8 antibody, set forth in the license agreement have also been terminated. Gilead will acquire certain related intellectual property, including all outstanding rights of Jounce to GS-1811, pursuant to the transaction agreement. GS-1811, a potentially first-in-class immunotherapy, is designed to selectively deplete immunosuppressive tumor-infiltrating T regulatory cells in the tumor microenvironment and is currently in Phase 1 clinical development as a possible treatment for patients with solid tumors.
“We are pleased to announce the signing of this transaction with Gilead who have a strong track record of developing and successfully commercializing leading brands in biotechnology,” said Richard Murray, Ph.D., chief executive officer and president of Jounce. “This transaction allows us to extend our runway and remain focused on delivering meaningful and long-lasting benefits to cancer patients. It was important for Jounce at this time to bolster our cash resources given challenges in capital markets for biotech companies.”
Jounce will receive proceeds of $67 million for this transaction and Gilead will be solely responsible for all further research, development, and commercialization of GS-1811 globally.
“Today’s news about GS-1811 further demonstrates our commitment to our rapidly evolving oncology franchise and mission of pioneering next-generation medicines for people with cancer,” said Bill Grossman, M.D., Ph.D., Senior Vice President, Therapeutic Area Head, Gilead Oncology. “GS-1811, with its potential new pathway of activating the immune system, gives us the opportunity to potentially change the standard of care with a treatment that works from inside cancerous cells to shrink solid tumors.”
Beginning in the first quarter of 2022, consistent with recent industry communications from the U.S. Securities and Exchange Commission (SEC), Gilead no longer excludes acquired IPR&D expenses from its non-GAAP financial measures. We expect the transaction with Jounce to reduce Gilead’s GAAP and non-GAAP 2022 EPS by approximately $0.04.
Jounce will no longer be entitled to receive the remaining contingent payments of up to $645 million in milestones and high single digit to mid-teens royalties based upon worldwide sales under the original license agreement. Additional details of the transaction, including related agreements and matters, will be contained in a Current Report on Form 8-K to be filed by Jounce.
About Jounce Therapeutics
Jounce Therapeutics, Inc. is a clinical-stage immunotherapy company dedicated to transforming the treatment of cancer by developing therapies that enable the immune system to attack tumors and provide long-lasting benefits to patients through a biomarker-driven approach. Jounce currently has multiple development stage programs ongoing while simultaneously advancing additional early-stage assets from its robust discovery engine based on its Translational Science Platform. Jounce’s highest priority program, JTX-8064, is a LILRB2 (ILT4) receptor antagonist shown to reprogram immune-suppressive tumor associated macrophages to an anti-tumor state in preclinical studies. JTX-8064 is being investigated alone and in combination with pimivalimab (formerly JTX-4014), Jounce’s internal PD-1 inhibitor, in one monotherapy and seven indication-specific combination therapy cohorts in the Phase 1/2 INNATE trial and is currently enrolling patients with advanced solid tumors in the Phase 2 portion of the study. Jounce’s most advanced product candidate, vopratelimab, is a monoclonal antibody that binds to and activates ICOS, and is currently being studied in the SELECT Phase 2 trial. Pimivalimab is a PD-1 inhibitor intended for combination use with Jounce’s broader pipeline. For more information, please visit www.jouncetx.com.
About Gilead Sciences
Gilead Sciences, Inc. is a biopharmaceutical company that has pursued and achieved breakthroughs in medicine for more than three decades, with the goal of creating a healthier world for all people. The company is committed to advancing innovative medicines to prevent and treat life-threatening diseases, including HIV, viral hepatitis, and cancer. Gilead operates in more than 35 countries worldwide, with headquarters in Foster City, California.
Jounce soars 59% after Gilead will acquire remaining rights to cancer immunotherapy
Dec. 27, 2022 5:12 PM ET
Jounce Therapeutics, Inc. (JNCE), GILD
By: Jonathan Block, SA News Editor1 Comment
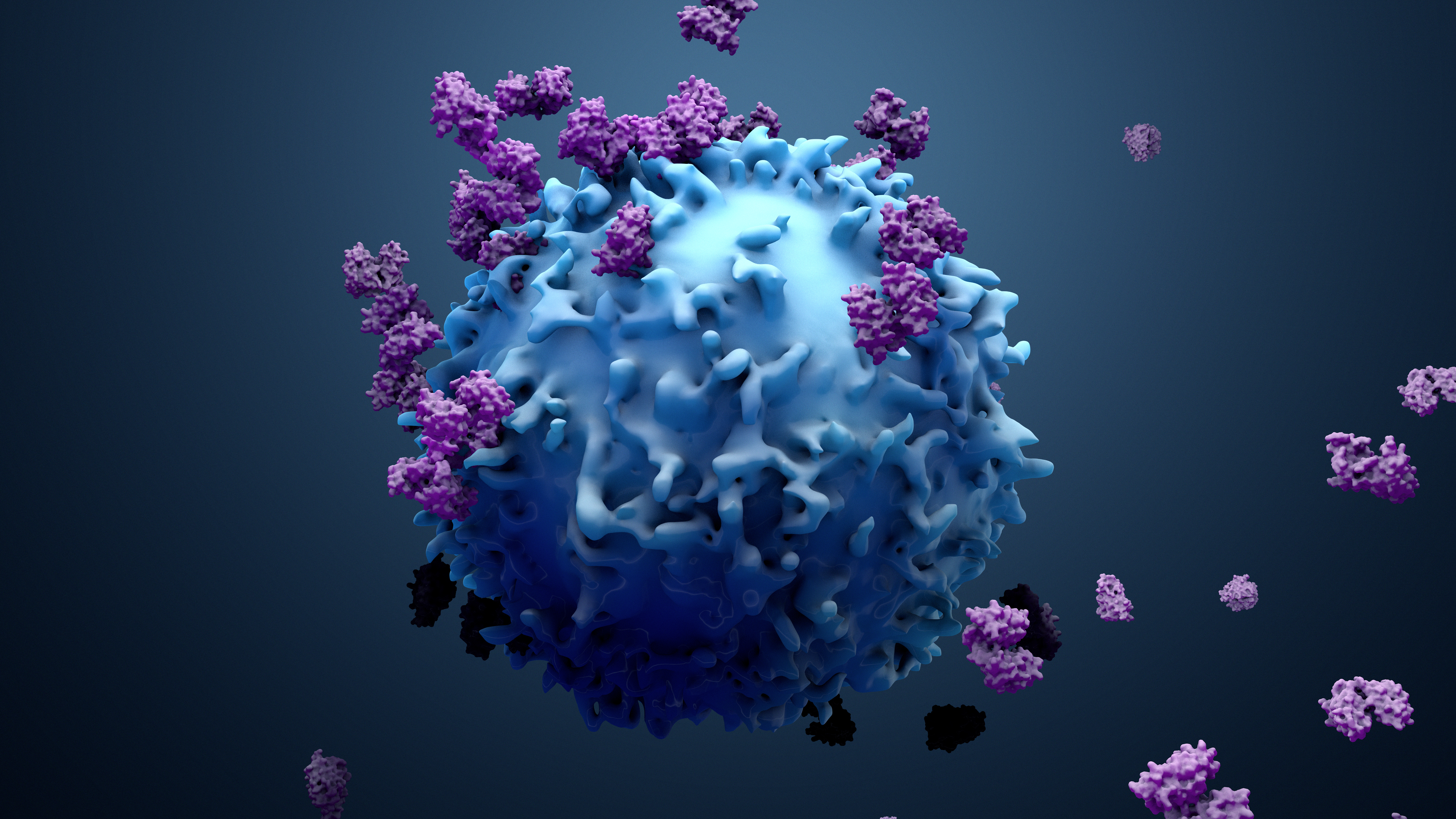
- Jounce Therapeutics (NASDAQ:JNCE) is receiving $67M from Gilead Sciences (NASDAQ:GILD) in exchange for giving up rights to its phase 1 cancer immunotherapy GS-1811 (formerly JTX-1811).
- https://seekingalpha.com/news/3920812-jounce-therapeutics-soars-59-after-gilead-will-acquire-remaining-rights-to-cancer-immunotherapy
- Jounce Therapeutics, Inc. (JNCE), GILD
- https://jouncetx.com/our-pipeline/
- https://jouncetx.com/
Olpruva (sodium phenylbutyrate)
Renazorb (lanthanum dioxycarbonate)
Olpruva (sodium phenylbutyrate)
NDA 214860 NDA APPROVAL Acer Therapeutics Inc. Attention: Renée M. Carroll, MS, RAC Vice President, Head of Regulatory Affairs One Gateway Center, Suite 356 300 Washington Street Newton, MA 02458 Dear Ms. Carroll:
Please refer to your new drug application (NDA) dated and received August 5, 2021, and your amendments, submitted pursuant to section 505(b)(2) of the Federal Food, Drug, and Cosmetic Act (FDCA) for Olpruva (sodium phenylbutyrate) for oral suspension. We acknowledge receipt of your amendment dated July 15, 2022, which constituted a complete response to our June 15, 2022, action letter. This NDA provides for the use of Olpruva (sodium phenylbutyrate) for oral suspension as adjunctive therapy to standard of care, which includes dietary management, for the chronic management of adult and pediatric patients weighing 20 kg or greater and with a body surface area (BSA) of 1.2 m2 or greater, with urea cycle disorders (UCDs) involving deficiencies of carbamylphosphate synthetase (CPS), ornithine transcarbamylase (OTC), or argininosuccinic acid synthetase (AS). APPROVAL & LABELING We have completed our review of this application, as amended. It is approved, effective on the date of this letter, for use as recommended in the enclosed agreed-upon labeling. CONTENT OF LABELING As soon as possible, but no later than 14 days from the date of this letter, submit the content of labeling [21 CFR 314.50(l)] in structured product labeling (SPL) format using the FDA automated drug registration and listing system (eLIST), as described at FDA.gov.1 Content of labeling must be identical to the enclosed labeling (text for the Prescribing Information, Patient Package Insert, and Instructions for Use) as well as annual reportable changes not included in the enclosed labeling. Information on 1 http://www.fda.gov/ForIndustry/DataStandards/StructuredProductLabeling/default.htm Reference ID: 5100040 NDA 214860 Page 2 U.S. Food and Drug Administration Silver Spring, MD 20993 www.fda.gov submitting SPL files using eLIST may be found in the guidance for industry SPL Standard for Content of Labeling Technical Qs and As. 2 The SPL will be accessible via publicly available labeling repositories. CARTON AND CONTAINER LABELING Submit final printed carton and container labeling that are identical to the enclosed carton and container labeling as soon as they are available, but no more than 30 days after they are printed. Please submit these labeling electronically according to the guidance for industry SPL Standard for Content of Labeling Technical Qs & As. For administrative purposes, designate this submission “Final Printed Carton and Container Labeling for approved NDA 214860.” Approval of this submission by FDA is not required before the labeling is used. DATING PERIOD Based on the stability data submitted to date, the expiry dating period for Olpruva (sodium phenylbutyrate) for oral suspension shall be 36 months from the date of manufacture when stored at 20º to 25ºC (68º to 77ºF) and excursions permitted to 15º to 30ºC (59º to 86ºF) [see USP Controlled Room Temperature] in the proposed container closure system. REQUIRED PEDIATRIC ASSESSMENTS Under the Pediatric Research Equity Act (PREA) (21 U.S.C. 355c), all applications for new active ingredients (which includes new salts and new fixed combinations), new indications, new dosage forms, new dosing regimens, or new routes of administration are required to contain an assessment of the safety and effectiveness of the product for the claimed indication in pediatric patients unless this requirement is waived, deferred, or inapplicable. We are deferring submission of your pediatric study for patients who weigh <20 kg and patients who weigh ≥20 kg with a BSA <1.2 m2 for this application because this product is ready for approval for use in adult and pediatric patients weighing 20 kg or greater and with a BSA of 1.2 m2 or greater. Pediatric studies in patients who weigh <20 kg and patients who weigh ≥20 kg with a BSA <1.2 m2 have not been completed. Studies to develop appropriate dosage strength(s) for dosing patients who weigh <20 kg and patients who weigh ≥20 kg with a BSA <1.2 m2 are necessary to ensure appropriate dosing of Olpruva in these patients, and the development of such dosage strength(s) will depend upon the feasibility of manufacturing and demonstration of stability of lower strength(s). 2 We update guidances periodically. For the most recent version of a guidance, check the FDA Guidance Documents Database https://www.fda.gov/RegulatoryInformation/Guidances/default.htm. Reference ID: 5100040 NDA 214860 Page 3 U.S. Food and Drug Administration Silver Spring, MD 20993 www.fda.gov Your deferred pediatric study required by section 505B(a) of the FDCA is a required postmarketing study. The status of this postmarketing study must be reported annually according to 21 CFR 314.81 and section 505B(a)(4)(C) of the FDCA. This required study is listed below. 4380-1 Develop dosage strength(s) to accommodate the recommended dosing for pediatric patients who weigh <20 kg and patients who weigh ≥20 kg with a body surface area <1.2 m2. The timetable you submitted on December 12, 2022, states that you will conduct this trial according to the following schedule: Draft Protocol Submission: 03/2023 Final Protocol Submission: 05/2023 Study Completion: 09/2023 Final Report Submission: 10/2023 FDA considers the term final to mean that the applicant has submitted a protocol, the FDA review team has sent comments to the applicant, and the protocol has been revised as needed to meet the goal of the study or clinical trial.3 Submit the protocol(s) to your IND 143822, with a cross-reference letter to this NDA. Reports of this required pediatric postmarketing study must be submitted as an NDA or as a supplement to your approved NDA with the proposed labeling changes you believe are warranted based on the data derived from this study. When submitting the reports, please clearly mark your submission "SUBMISSION OF REQUIRED PEDIATRIC ASSESSMENTS" in large font, bolded type at the beginning of the cover letter of the submission. This product is appropriately labeled for use in pediatric patients weighing 20 kg or greater and with a BSA of 1.2 m2 or greater for this indication. Therefore, no additional studies are needed in this pediatric group.
Acer wins FDA OK for Olpruva to treat urea cycle disorders
Dec. 23, 2022 2:30 PM ET
Acer Therapeutics Inc. (ACER), RLFTF, RLFTY
By: Dulan Lokuwithana, SA News Editor
The U.S. Food and Drug Administration (FDA) has greenlighted Olpruva, being developed by Acer Therapeutics (NASDAQ:ACER) and Swiss biotech Relief Therapeutics (OTCQB:RLFTF) (OTCQB:RLFTY) as a treatment for patients with urea cycle disorders (UCD).
Acer Therapeutics Inc. (ACER), RLFTF, RLFTY
https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2022/214860Orig1s000ltr.pdf
Eftilagimod Alpha (Efti)
VLA1553 a live-attenuated, single dose investigational vaccine candidate targeting chikungunya virus
VLA1553 a live-attenuated, single dose investigational vaccine candidate targeting chikungunya virus
ASX/Media Release Immutep Announces Successful Meeting with the FDA on Eftilagimod Alpha plus Chemotherapy for the Treatment of Metastatic Breast Cancer • Agreement with FDA on Phase II/III trial design positions the Company to exploit eftilagimod alpha’s potential to address high unmet need for metastatic breast cancer patients • Patient population expanded to include patients with triple-negative breast cancer • Late-stage clinical development efforts remain focused on frontline non-small cell lung cancer (NSCLC) in combination with anti-PD-1 therapy • Immutep’s cash runway extended to the end of the 1st half of calendar year 2024 SYDNEY, AUSTRALIA – 23 December 2022 – Immutep Limited (ASX: IMM; NASDAQ: IMMP) ("Immutep” or “the Company”), a clinical-stage biotechnology company developing novel LAG-3 immunotherapiesfor cancer and autoimmune disease, today announces the results of a positive follow-up Type C meeting with the US Food and Drug Administration (FDA) regarding late-stage clinical development plans for its first-in-class soluble LAG-3 protein, eftilagimod alpha (“efti”), in conjunction with standard-of-care chemotherapy for the treatment of metastatic breast cancer (MBC). The Company and the FDA have agreed to an integrated Phase II/III trial design that will help inform a Biologics License Application (BLA). Based on the encouraging efficacy, favourable safety, and learnings from the randomised AIPAC Phase IIb trial, which administered efti and chemotherapy on different days and ceased chemotherapy at six months, patients will receive efti and paclitaxel on the same day and treatment will continue until disease progression. The patient population has also been expanded to include triple-negative breast cancer (TNBC), an aggressive form of breast cancer with limited treatment options. Immutep CEO, Marc Voigt, commented: “As recently announced, our late-stage clinical development efforts for efti are now focused on frontline NSCLC in combination with anti-PD-1 therapy, given the large market opportunity and need for more durable and tolerable options. With this said, progress reported to date with the FDA and EMA provides Immutep and its potential partners flexibility for late-stage clinical development of efti plus standard-of-care chemotherapy to address the high unmet need for metastatic breast cancer patients, while maintaining their quality of life as was shown in the AIPAC trial.” Immutep CSO & CMO, Dr. Frédéric Triebel, stated: “We are excited about efti’s promise to stimulate the immune system and improve standard-of-care chemotherapy by activating dendritic cells to present antigens from chemo-induced cancer cell death to cytotoxic T cells. Our engagement with regulatory agencies to establish the optimal design of a registrational trial has steadily progressed during the year and we are pleased with the FDA’s positive feedback during this follow up meeting. The chosen trial design provides us with a very risk-balanced approach before potentially embarking on the Phase 3 part of this study.” Subject to regulatory and ethic committee feedback, the Phase II portion of the MBC trial is expected to begin during the first quarter of 2023. In addition to the biologically active 30mg dosing for efti, the Company and FDA have agreed to test 90mg efti dosing in combination with paclitaxel driven predominantly by the excellent safety profile of the AIPAC Phase IIb trial, along with the FDA’s Project Optimus initiative in oncology. The trial design has a safety lead in of 6 to 12 patients, given the higher 90mg dosing of efti, followed by 58 patients for the randomised Phase II portion of the trial. Depending on Phase II results and resources, the Phase III portion will follow and be directed to MBC patients most likely to benefit from treatment, taking into consideration the strong overall survival results in pre-specified and post-hoc subgroups from the AIPAC trial. The Phase II portion of the MBC trial and the initiation of the registrational trial in 1st line NSCLC are included in the budget of the Company and have no impact on its expected cash runway to the end of the 1st half of calendar year 2024. About Eftilagimod Alpha (Efti) Efti is Immutep’s proprietary soluble LAG-3 clinical stage candidate that is a first-in-class antigen presenting cell (APC) activator for the treatment of cancer, capitalising on LAG-3’s unique characteristics to stimulate both innate and adaptive immunity. Efti binds to and activates antigen presenting cells via MHC II molecules leading to expansion and proliferation of CD8+ (cytotoxic) T cells, CD4+ (helper) T cells, dendritic cells, NK cells, and monocytes. It also upregulates the expression of key biological molecules like CXCL10 that further boost the immune system’s ability to fight cancer. Efti is under evaluation for a variety of solid tumours including non-small cell lung cancer (NSCLC), head and neck squamous cell carcinoma (HNSCC), and HER2–/HR+ metastatic breast cancer. Its favourable safety profile enables various combinations, including with anti-PD-[L]1 immunotherapy and/or chemotherapy. Efti has received Fast Track Designation in 1st line HNSCC and in 1st line NSCLC from the United States Food and Drug Administration (FDA). About Immutep Immutep is a clinical stage biotechnology company leading the development of LAG-3 related immunotherapy products for the treatment of cancer and autoimmune disease. The Company is dedicated to leveraging its technology and expertise to bring innovative treatment options to market for patients and to maximise value to shareholders. Immutep’s lead product candidate is eftilagimod alpha (“efti” or “IMP321”), a soluble LAG-3 fusion protein (LAG-3Ig), which is a first-in-class antigen presenting cell (APC) activator being explored in cancer in multiple clinical trials. The Company is also developing an agonist of LAG-3 (IMP761) for autoimmune disease. Additional LAG-3 product candidates, including antibodies for immune response modulation, are being developed under license by Immutep’s large pharmaceutical partners. Further information can be found on the Company’s website www.immutep.com or by contacting:
Immutep surges 25% after 'positive' FDA meeting for eftilagimod's trial in breast cancer
Dec. 23, 2022 9:01 AM ET
By: Ravikash, SA News Editor1 Comment
Immutep (NASDAQ:IMMP) (OTCPK:PRRUF) said it had a positive follow-up Type C meeting with the U.S. Food and Drug Administration (FDA) regarding late-stage clinical development plans for eftilagimod alpha (efti), with standard-of-care chemotherapy, to treat metastatic breast cancer (MBC).
VLA1553 a live-attenuated, single dose investigational vaccine candidate targeting chikungunya virus
VLA1553 a live-attenuated, single dose investigational vaccine candidate targeting chikungunya virus
VLA1553 a live-attenuated, single dose investigational vaccine candidate targeting chikungunya virus
Valneva Completes BLA Submission to U.S. FDA for its Single-Shot Chikungunya Vaccine Candidate
December 23, 2022
Saint-Herblain (France), December 23, 2022 – Valneva SE (Nasdaq: VALN; Euronext Paris: VLA), a specialty vaccine company, today announces that it has completed rolling submission of the Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA) for its single-shot chikungunya vaccine candidate, VLA1553. Valneva is seeking approval of its investigational chikungunya vaccine in persons aged 18 years and above.
This BLA application follows final pivotal Phase 3 data reported in March 2022[1] and final lot-to-lot consistency results reported in May 2022[2]. A clinical study of VLA1553 in adolescents is ongoing in Brazil[3], which may support future regulatory submissions in this group if VLA1553 is initially approved in adults. The Company also recently reported positive antibody persistence data with a 99% seroresponse rate 12 months after a single-dose vaccination[4].
Juan Carlos Jaramillo, MD, Chief Medical Officer of Valneva, commented, “The completion of our BLA submission is extremely important as it takes us a step closer to potentially bringing a preventative solution to fight this debilitating disease. Chikungunya is a major public health threat transmitted to humans by infected mosquitoes, and no vaccine or specific treatments for the disease are currently available. If the FDA approves the submission, our goal is to provide a tool to help curtail this growing, unmet medical need.”
The FDA will now review the filing for acceptance, determine priority review eligibility and the action date which it targets to complete its evaluation. The program received FDA Fast Track and Breakthrough Therapy designations in 2018 and 2021, respectively. VLA1553 was also granted PRIority MEdicine (PRIME) designation by the European Medicines Agency (EMA) in 2020, and Valneva plans to make regulatory submissions for VLA1553 in Europe in the second half of 2023.
About Chikungunya
Chikungunya is a mosquito-borne viral disease caused by the chikungunya virus (CHIKV), a Togaviridae virus, transmitted by Aedes mosquitoes. Infection leads to symptomatic disease in 72-92% of humans after four to seven days following the mosquito bite. While mortality with CHIKV is low, morbidity is high, and the global market for vaccines against chikungunya is estimated to exceed $500 million annually by 2032[5]. Clinical symptoms include acute onset of fever, debilitating joint and muscle pain, headache, nausea, rash and chronic arthralgia. Chikungunya virus often causes sudden large outbreaks with high attack rates, affecting one-third to three-quarters of the population in areas where the virus is circulating. The high-risk areas of infection for travelers are places where chikungunya virus-carrying mosquitos are endemic, including the Americas, parts of Africa, and Southeast Asia, and the virus has spread to more than 100 countries. As of July 2022, more than three million cases have been reported in the Americas[6] and the economic impact is considered to be significant. The medical and economic burden is expected to grow as the CHIKV primary mosquito vectors continue to spread geographically. There are no preventive vaccines or effective treatments available and, as such, chikungunya is considered to be a major public health threat.
About VLA1553
VLA1553 is a live-attenuated, single dose investigational vaccine candidate targeting the chikungunya virus, which has spread to over 100 countries. It has been designed by deleting a part of the chikungunya virus genome.
Valneva reported final data from the pivotal Phase 3 trial of VLA1553 in March 2022[7] and final lot-to-lot consistency results in May 2022[8].
If approved, VLA1553 would expand Valneva’s existing commercial vaccines portfolio and as such, Valneva intends to commercialize this vaccine, leveraging its existing manufacturing and commercial operations.
To make VLA1553 more accessible to Low- and Middle-Income Countries (LMIC), Valneva and Instituto Butantan in Brazil signed an agreement in January 2021 for the development, manufacturing and marketing of VLA1553[9]. The collaboration falls within the framework of the agreement signed between CEPI and Valneva in July 2019[10], which provides funding of up to $23.4 million with support from the European Union’s Horizon 2020 program.
About Valneva SE
Valneva is a specialty vaccine company focused on the development and commercialization of prophylactic vaccines for infectious diseases with significant unmet medical need. The Company takes a highly specialized and targeted approach to vaccine development and then applies its deep understanding of vaccine science to develop prophylactic vaccines addressing these diseases. Valneva has leveraged its expertise and capabilities both to successfully commercialize two vaccines and to rapidly advance a broad range of vaccine candidates into and through the clinic, including candidates against Lyme disease, the chikungunya virus and COVID-19.
Valneva stock rises as it seeks FDA approval of single-shot chikungunya vaccine
Dec. 23, 2022 5:03 AM ET
By: Ravikash, SA News Editor
- Valneva (NASDAQ:VALN) (OTCPK:INRLF) said it completed a rolling submission of an application to the U.S. Food and Drug Administration (FDA) seeking approval of its single-shot chikungunya vaccine VLA1553 in people aged 18 years and above.
- https://seekingalpha.com/news/3920173-valneva-stock-rises-as-it-seeks-fda-approval-of-single-shot-chikungunya-vaccine
- Valneva SE (VALN), INRLF
- https://valneva.com/research-development/chikungunya/
BNT163
VLA1553 a live-attenuated, single dose investigational vaccine candidate targeting chikungunya virus
ABI-H3733 and ABI-4334
BioNTech Starts Phase 1 Clinical Trial for Prophylactic Herpes Simplex Virus-2 Vaccine Candidate BNT163
- First-in-human study aims to evaluate the safety and immunogenicity of prophylactic herpes virus vaccine candidate BNT163
- BNT163 is the first candidate from BioNTech’s infectious disease mRNA vaccine collaboration with the University of Pennsylvania to enter the clinic
- The program is part of BioNTech’s strategy to address diseases with high unmet medical need, as no vaccine has been approved for prevention of genital lesions caused by HSV
MAINZ, Germany, December 21, 2022 – BioNTech SE
(Nasdaq: BNTX, “BioNTech” or the "Company”) today announced that the first subject was dosed in a first-in-human Phase 1 clinical research study with BNT163, a herpes simplex virus (HSV) vaccine candidate for the prevention of genital lesions caused by HSV-2 and potentially HSV-1. The trial (NCT05432583) will evaluate the safety, tolerability, and immunogenicity of BNT163. The mRNA vaccine encodes three HSV-2 glycoproteins with the aim of helping to prevent HSV cellular entry and spread, as well as counteract the immunosuppressive properties of HSVs.
According to the World Health Organization (“WHO”), approximately 500 million people globally are estimated to be affected by genital infections caused by HSV-2,1 with painful genital lesions, an increased risk for meningitis and high levels of emotional distress. Once acquired, HSV persists lifelong in the body with reoccurring symptomatic outbreaks. Moreover, HSV-2 infection increases the risk of acquiring HIV infections by approximately three-fold, and co-infections with both HIV and HSV-2 increase the likelihood of transmitting HIV to others according to the WHO.2 No vaccine has been approved for prevention of genital lesions caused by HSV to date. Currently available HSV therapies only reduce the severity and frequency of symptoms.
BioNTech’s placebo-controlled, observer blinded, dose-escalation Phase 1 trial is expected to enroll around 100 healthy volunteers aged 18 to 55 years without current or history of symptomatic genital herpes infections in the U.S. The study consists of a first dose escalation part that will focus on safety evaluations and assess the optimal dose-response in various dose levels. The second part of the trial is designed to expand the safety characterization for the selected dosing of BNT163 for a more comprehensive assessment of the impact of pre-existing immunity to HSV-1 and -2 on the safety and BNT163-induced immune responses.
“This program is part of our strategy to help address diseases with a high unmet medical need and of global health relevance by combining our new technologies such as mRNA and our expertise in immune engineering,” said Prof. Özlem Türeci, M.D., Chief Medical Officer and Co-Founder of BioNTech. “BNT163 is based on three non-infectious mRNA-encoded HSV-2 glycoproteins. We aim to induce a broad immune response which is directed against multiple antigens of the virus and mobilizes various immune effectors to support virus neutralization and clearance.”
“HSV-2 is a very challenging and life-altering disease which can only be partially prevented. My colleagues and I are proud to have contributed to the early development and preclinical testing of this exciting new mRNA vaccine candidate that may have the potential to prevent people from contracting the virus,” said Prof. Harvey M. Friedman, M.D., Professor of Infectious Diseases at the University of Pennsylvania’s Perelman School of Medicine, who conducted preclinical and discovery science work on HSV and is the University of Pennsylvania’s principal investigator for the preclinical discovery and IND-enabling studies.
In 2018, Penn and BioNTech entered a research collaboration and license agreement to develop novel mRNA vaccine candidates for the prevention and treatment of various infectious diseases. Under the terms of the agreement, BioNTech can obtain an exclusive worldwide license to further develop and commercialize product candidates arising from the research collaboration. After completion of all IND-enabling studies, BNT163 is the first candidate from this collaboration to enter the clinic.
Editor’s Note: The University of Pennsylvania has licensed some intellectual property related to the BNT163 vaccine candidate to BioNTech. The University of Pennsylvania receives sponsored research funding from BioNTech related to preclinical development of the BNT163 vaccine candidate. As inventors of certain intellectual property related to the BNT163 vaccine candidate, some of the scientists involved in the preclinical development of the candidate along with Penn, may receive additional financial benefits under the BioNTech license in the future.
About BioNTech
Biopharmaceutical New Technologies is a next generation immunotherapy company pioneering novel therapies for cancer and other serious diseases. The Company exploits a wide array of computational discovery and therapeutic drug platforms for the rapid development of novel biopharmaceuticals. Its broad portfolio of oncology product candidates includes individualized and off-the-shelf mRNA-based therapies, innovative chimeric antigen receptor T cells, bispecific immune checkpoint modulators, targeted cancer antibodies and small molecules. Based on its deep expertise in mRNA vaccine development and in-house manufacturing capabilities, BioNTech and its collaborators are developing multiple mRNA vaccine candidates for a range of infectious diseases alongside its diverse oncology pipeline. BioNTech has established a broad set of relationships with multiple global pharmaceutical collaborators, including Genmab, Sanofi, Genentech, a member of the Roche Group, Regeneron, Genevant, Fosun Pharma, and Pfizer. For more information, please visit www.BioNTech.com.
BioNTech starts phase 1 trial of mRNA herpes vaccine
Dec. 21, 2022 7:46 AM ET
By: Ravikash, SA News Editor
- BioNTech (NASDAQ:BNTX) said the first person was dosed in a phase 1 trial of its mRNA herpes simplex virus (HSV) vaccine candidate BNT163 to prevent genital lesions caused by HSV-2 and potentially HSV-1.
- https://seekingalpha.com/news/3919346-biontech-starts-phase-1-trial-of-mrna-herpes-vaccine
- BioNTech SE (BNTX)
- https://www.biontech.com/int/en/home/pipeline-and-products/pipeline.html
- https://www.biontech.com/int/en/home.html
ABI-H3733 and ABI-4334
ABI-H3733 and ABI-4334
ABI-H3733 and ABI-4334
Assembly Biosciences Announces Promising Interim Results from Two Clinical Trials Evaluating Highly Potent Next-Generation Core Inhibitor Candidates ABI-H3733 and ABI-4334
December 19, 2022 at 8:01 AM EST
- In initial ABI-H3733 cohort of 50 mg in 28-day Phase 1b study, six of eight HBV patients on treatment reached lower limit of quantification for HBV DNA by day 21 and patients showed a mean reduction of 3.1 logs in plasma HBV DNA
- Initial ABI-4334 Phase 1a single-dose 30 mg cohort demonstrated pharmacokinetic profile supportive of once-daily oral dosing and provides early indication that ABI-4334's very high potency seen preclinically can be accessed clinically
- No serious adverse events or significant laboratory abnormalities including alanine aminotransferase (ALT) elevation were observed in either study
- Given potent antiviral activity in the initial 50 mg cohort, second 25 mg cohort ongoing in Phase 1b trial of ABI-H3733 to explore dose-response curve; 100 mg cohorts ongoing for both studies with further data expected in Q1 2023
SOUTH SAN FRANCISCO, Calif., Dec. 19, 2022 (GLOBE NEWSWIRE) -- Assembly Biosciences, Inc. (Nasdaq: ASMB), a clinical-stage biotechnology company developing innovative, investigational therapeutics targeting hepatitis B virus (HBV) and other viral diseases, today announced promising interim efficacy, safety and pharmacokinetic (PK) results from two ongoing clinical studies of its investigational next-generation HBV core inhibitors, a Phase 1b clinical study of ABI-H3733 (3733) and a Phase 1a clinical study of ABI-4334 (4334).
“We are excited to see that these interim results from ongoing Phase 1 studies of our next-generation core inhibitors 3733 and 4334 are exceeding our expectations for key elements of the clinical profile we’re looking for to impact chronic HBV infection,” said John McHutchison, AO, MD, chief executive officer of Assembly Bio.
Assembly Bio specifically designed 3733 and 4334 to optimize potency against both new virus production (first mechanism) and formation of covalently closed circular DNA (cccDNA), the viral reservoir (second mechanism). Both compounds have demonstrated significantly increased potency preclinically against both mechanisms compared to first-generation core inhibitors. This increased potency, particularly against cccDNA formation, is critical to Assembly Bio’s HBV strategy to bring finite therapies and cures for those living with chronic HBV (cHBV) infection.
“In this first look at antiviral activity for 3733 in the Phase 1b study, we are seeing steep declines in HBV DNA at the low starting dose of 50 mg,” continued Dr. McHutchison. “The antiviral activity from this cohort against the first mechanism surpasses both what we demonstrated preclinically for 3733 as well as what we saw clinically in similar time frames with our first-generation core inhibitors at much higher doses. We are also highly encouraged by the initial pharmacokinetic data from our first-in-human clinical study of our most potent core inhibitor, 4334, which show the potential to reach high levels of activity against both mechanisms clinically at a low dose.”
Jason Okazaki, president and chief operating officer and CEO-elect of Assembly Bio, concluded, “With 100 mg cohorts of both 3733 (28-day dosing) and 4334 (single dose) underway, we are eager to see and share data in early 2023 that we anticipate will drive the optimal dose selection to maximize activity against both mechanisms of action. While early, we believe the interim results in both studies are an encouraging indication that the preclinical potency documented for our next-generation core inhibitors against the second mechanism of cccDNA formation will translate into the clinic with longer-term dosing.”
Complete results of these clinical trials, when available, together with ongoing nonclinical and chronic toxicity studies, will inform future clinical development planning for Assembly Bio’s next-generation core inhibitor programs.
Phase 1b Study for 3733 – Study ABI-H3733-102
The ongoing Phase 1b clinical trial is a randomized, multi-center, double-blind and placebo-controlled study evaluating the safety, PK and antiviral activity of 3733, including changes in HBV DNA and other viral parameters associated with 3733 treatment in adults with cHBV infection who are treatment naïve or off treatment. Patients were randomized 8:2 between the new tablet formulation of 3733 and placebo for a period of 28 days. The patient population for the data included here consists primarily of e-antigen negative patients. The study remains externally blinded, so individual patient data are not provided.
The dose selected for the first cohort was 50 mg. Given the potent antiviral activity observed at 50 mg, a 25 mg dose was selected for the second cohort to further explore the dose response curve of 3733. A dose of 100 mg has been selected for the third cohort, for which dosing is ongoing with initial data anticipated in the first quarter of 2023.
50 mg Cohort Efficacy (Viral Nucleic Acids):
As of the data cutoff date of December 18, 2022, dosing in the 3733 Phase 1b trial has been completed for all 10 patients in the first cohort of 50 mg. Nine of 10 patients enrolled were HBeAg negative, so efficacy data are provided for these patients. Interim efficacy results from this cohort at the data cutoff date include HBV DNA, HBV RNA and antigen measurements for all patients for the full 28-day dosing period.
In the 50 mg cohort, six of eight patients receiving 3733 achieved HBV DNA less than the lower limit of quantification (<LLOQ) within 21 days, with a mean decline in HBV DNA over the treatment period of approximately 3.1 logs. Data on HBV RNA declines were limited due to low baseline levels in predominantly e-antigen negative patients.
25 mg Cohort Efficacy (Viral Nucleic Acids):
The second cohort, evaluating a dose of 25 mg, is fully enrolled. Nine of 10 patients enrolled were HBeAg negative, so efficacy data are provided for these patients. In the five patients that have so far completed 28 days of treatment, the mean reduction in HBV DNA was approximately 1.9 logs. Data on HBV RNA levels were not available as of the data cutoff date.
50 and 25 mg Cohorts (Safety, PK and Viral Antigens):
Safety data reported here reflect data received for both cohorts through the data cutoff date. In these initial cohorts, all treatment-emergent adverse events (AEs) and laboratory abnormalities reported were Grade 1 or Grade 2. Further, no AEs led to treatment discontinuation, and no clinically significant ECG abnormalities or patterns of AEs or lab abnormalities were noted.
The observed PK for the new tablet formulation of 3733 was consistent with predictions from preclinical studies, providing exposure equivalent to the liquid formulation evaluated in the Phase 1a study for 3733. Clinical PK exposures exhibited dose-proportional increases from 25 mg to 50 mg, as measured by maximum concentration (Cmax) and area-under-curve (AUC).
As expected given the 28-day dosing period, limited changes in viral antigens were observed in both the 50 mg and 25 mg cohorts.
Phase 1a Study for 4334 – Study ABI-4334-101
The Phase 1a clinical trial is a randomized, blinded and placebo-controlled study evaluating the safety, tolerability and PK of 4334 following single ascending dose and multiple ascending dose administration in healthy subjects. The objectives of the study include assessment of the proportion of subjects with AEs, premature treatment discontinuation due to AEs and abnormal laboratory results.
Dosing has completed for all eight subjects in the initial 30 mg single dose cohort. In this cohort, 4334 had a mean half-life of 24 hours, supporting once-a-day (QD) dosing. Based on the PK data from this initial cohort and preclinical studies, daily minimum plasma trough concentrations (Cmin) are projected to achieve double-digit multiples of the protein-adjusted EC50 for both antiviral activity and against cccDNA formation at a low dose of 4334.
In this initial cohort, treatment-emergent AEs and laboratory abnormalities were mild to moderate and all were considered not related to study treatment. There were no clinically significant ECG abnormalities or patterns of AEs or laboratory abnormalities noted.
A dose of 100 mg has been selected for the second single-dose cohort. Dosing for the second cohort is complete and initial data from this cohort are anticipated in the first quarter of 2023.
About Assembly Biosciences
Assembly Bio is a clinical-stage biotechnology company pioneering the development of novel therapeutics for serious viral diseases. Assembly Bio is advancing a leading portfolio of more potent, next-generation core inhibitor drug candidates that aim to break the complex viral replication cycle of hepatitis B virus (HBV) to achieve finite and potentially curative therapies for the 296 million people living with HBV worldwide. The company’s research pipeline includes differentiated antiviral approaches against HBV/hepatitis delta virus and herpesviruses. For more information, visit assemblybio.com.
Assembly Biosciences surges 19% on positive data from two trials to treat hepatitis B virus
Dec. 19, 2022 9:07 AM ET
Assembly Biosciences, Inc. (ASMB)
By: Dania Nadeem, SA News Editor
- Assembly Biosciences (NASDAQ:ASMB) is trading ~19% higher premarket after it announced positive data from two ongoing studies of its investigational hepatitis B virus (HBV) inhibitors, a Phase 1b clinical study of ABI-H3733 and a Phase 1a clinical study of ABI-4334.
- https://seekingalpha.com/news/3918396-assembly-biosciences-surges-19-on-positive-data-from-two-trials-to-treat-hepatitis-b-virus
- Assembly Biosciences, Inc. (ASMB)
- https://www.assemblybio.com/
- https://www.assemblybio.com/pipeline/
resmetirom
ABI-H3733 and ABI-4334
Zolbetuximab
Madrigal Announces Positive Topline Results from the Pivotal Phase 3 MAESTRO-NASH Clinical Trial of Resmetirom for the Treatment of NASH and Liver Fibrosis
- In MAESTRO-NASH, a 52-week serial liver biopsy Phase 3 study in more than 950 patients, resmetirom achieved both primary endpoints and potentially clinically meaningful effects with both daily oral doses, 80 mg and 100 mg, relative to placebo
- NASH resolution (ballooning of 0, inflammation of 0-1) and ≥2-point NAS reduction with no worsening of fibrosis (p<0.0001 at both doses)
- Fibrosis improvement by at least one stage with no worsening of NAS (p=0.0002 and <0.0001 at 80 and 100 mg, respectively)
- Potentially clinically meaningful LDL-lowering, a key secondary endpoint (p<0.0001)
- Multiple positive effects on NASH biomarkers and imaging
- Resmetirom was safe and well-tolerated in the MAESTRO-NASH study, consistent with the overall safety in Phase 3 MAESTRO trials, expanding the large safety database
- Madrigal intends to file a new drug application seeking accelerated approval of resmetirom for the treatment of non-cirrhotic NASH with liver fibrosis
Madrigal to host conference call at 8:00 am ET to review the results
CONSHOHOCKEN, Pa., Dec. 19, 2022 (GLOBE NEWSWIRE) -- Madrigal Pharmaceuticals, Inc. (NASDAQ:MDGL), a clinical-stage biopharmaceutical company pursuing novel therapeutics for nonalcoholic steatohepatitis (NASH), today announced positive topline results from the pivotal Phase 3 MAESTRO-NASH biopsy clinical trial of resmetirom, a liver-directed selective thyroid hormone receptor agonist. MAESTRO-NASH, a registrational Phase 3 trial, has achieved both liver histological improvement endpoints that FDA proposed as reasonably likely to predict clinical benefit to support accelerated approval for the treatment NASH with liver fibrosis.
Becky Taub, M.D., Chief Medical Officer and President of Research & Development of Madrigal, stated, “These pivotal Phase 3 results demonstrate the potential for resmetirom to help patients achieve improvement in both the underlying steatohepatitis that drives this disease and the resulting fibrosis that is associated with progression to cirrhosis and its complications. The topline data also reinforce our confidence in the safety and tolerability profile of resmetirom. We believe the Phase 3 MAESTRO clinical development program, including the MAESTRO-NAFLD-1 and MAESTRO-NAFLD-OLE safety clinical trials and the recently initiated MAESTRO-NASH-OUTCOMES clinical trial, provides a strong foundation for our new drug application (NDA) and the potential accelerated approval of resmetirom for the treatment of non-cirrhotic NASH with liver fibrosis.”
Dr. Taub added, “I want to thank the MAESTRO-NASH investigators and study sites participating in the study, my colleagues on the R&D team at Madrigal, and, most of all, the patients who made achievement of this important milestone possible.”
Stephen Harrison, M.D., Chairman for both Pinnacle Clinical Research and Summit Clinical Research, San Antonio, Texas, Visiting Professor of Hepatology, Oxford University, and lead Principal Investigator of the MAESTRO studies, commented, “NASH with liver fibrosis puts patients at risk of progressing to liver failure, liver cancer, need for liver transplant, and premature mortality; with no approved treatment, this disease represents one of the most urgent unmet needs in healthcare today. These unprecedented results from the MAESTRO-NASH clinical trial signal a major turning point for the field.”
Paul Friedman, M.D., Chief Executive Officer of Madrigal, stated, “MAESTRO-NASH achieved both primary endpoints proposed by the FDA as reasonably likely to predict clinical benefit and we have established a large safety database, supported by a second Phase 3 clinical trial (MAESTRO-NAFLD-1) and MAESTRO-NAFLD-OLE, to inform benefit-risk assessment. With these unequivocally positive Phase 3 data in hand, our path forward is clear. In the first half of 2023, we intend to file a new drug application seeking accelerated approval of resmetirom. I want to thank my colleagues for their sustained efforts and strong execution; our team is committed to delivering resmetirom to patients in need.”
MAESTRO-NASH Week 52 Results
MAESTRO-NASH is an ongoing blinded Phase 3 clinical trial, and enrolled patients continue on therapy after the Week 52 liver biopsy for up to a total of 54 months to accrue hepatic clinical outcome events including histologic conversion to cirrhosis and hepatic decompensation events.
Efficacy Results
Patients meeting eligibility requirements for MAESTRO-NASH were randomized 1:1:1 to receive resmetirom 80 mg, resmetirom 100 mg, or placebo taken orally once daily. Baseline characteristics in the 966 randomized patients in the primary analysis NASH population (ITT, safety population) were balanced across treatment arms and include age 57 (10) (mean (SD)), female 56%, white 89%, Hispanic 21%, BMI 36 (7) kg/m2, type 2 diabetes 67%, hypertension 78%, dyslipidemia 71%, hypothyroidism 13%, FibroScan, kilopascals (kPa) 13 (7), CAP 348 (38), MRI-PDFF 18% (7), FIB-4 1.4 (0.7), ALT 55 (32) IU, AST 41 (23) IU, LDL 99 (40) mg/dL, triglycerides 188 (132) mg/dL, hemoglobin A1C 6.6 (1) %, ELF 9.8 (0.9). Medications included 49% on statins, 14% on GLP-1 agonists, 14% on SGLT2 inhibitors. Baseline liver biopsy fibrosis scores included F3 (~60%), F2 (~35%), F1B (~5%) (primary analysis population) with 84% with NAS ≥5 based on independent primary glass slide reads of the entire study by two central pathologists.
A second biopsy was conducted after 52 weeks of treatment for assessment of the dual primary endpoints. The primary efficacy analysis assessed histological response at 52 weeks in 955 patients with biopsy-confirmed NASH with fibrosis (modified intent-to-treat (mITT) population) that excluded 11 ITT patients who had their Week 52 biopsy after Week 60 due to COVID-related reasons per regulatory guidelines. Patients without a second biopsy due to early study discontinuation or missing liver biopsy (~17% across treatment arms) were included and considered as non-responders in the primary efficacy analyses (mITT). The compliance to treatment was high and minimally impacted by COVID pandemic restrictions.
All biopsies were read independently by two central pathologists. Each pathologist's scores showed a similar statistically significant magnitude of response at both doses for both liver biopsy endpoints. Biopsy endpoints were achieved independent of baseline fibrosis stage or diabetes status, including similar statistical significance and magnitude of effect at both doses in subgroups of F2, F3, and F2/F3 patients. Other secondary liver biopsy endpoints that were achieved at both doses include ≥2 point reduction in NAS with no worsening of fibrosis, ≥2 point reduction in NAS with ≥1-stage improvement in fibrosis, NASH resolution (with ≥2 point reduction in NAS) with ≥1-stage improvement in fibrosis, and a 2-stage reduction in fibrosis without worsening of NAS.
Multiple secondary endpoints were achieved, including statistically significant reduction from baseline in liver enzymes (ALT, AST and GGT). Reductions in atherogenic lipids and lipoproteins, fibrosis biomarkers and imaging tests (MRI-PDFF, CAP and liver stiffness measures) were observed in resmetirom treatment arms as compared with placebo.
MAESTRO-NASH included many biomarker and imaging assessments that may be used in real world clinical practice to identify appropriate patients for treatment and monitor response to resmetirom, if approved.
Madrigal intends to submit primary results for publication in a peer-reviewed journal and present study results at a future scientific congress.
Safety Results
Resmetirom was safe and well-tolerated at both the 80 mg and 100 mg doses. The frequency of serious adverse events (SAEs) was similar across treatment arms: 11.8%, 12.7% and 12.1% for the 80 mg, 100 mg, and placebo groups, respectively. The rate of study discontinuation for adverse events was low: 2.8%, 7.7% and 3.7% for the 80 mg, 100 mg and placebo groups, respectively. SAEs occurred at expected rates based on the patient population.
Consistent with previous Phase 2 and Phase 3 data, the most common adverse events reported with greater frequency in the resmetirom groups vs placebo were an excess of generally mild and transient diarrhea at the beginning of therapy, in 28%, 34%, 16% in the 80 mg, 100 mg and placebo groups, respectively, and generally mild nausea that occurred at rates of 22%, 19% and 13% in the 80 mg, 100 mg and placebo arms, respectively.
About the Resmetirom Phase 3 Registration Program for the Treatment of NASH
Madrigal is currently conducting four Phase 3 clinical trials to demonstrate the safety and efficacy of resmetirom for the treatment of NASH: MAESTRO-NASH, MAESTRO-NAFLD-1, MAESTRO-NAFLD-OLE, and MAESTRO-NASH-OUTCOMES.
MAESTRO-NASH is a multicenter, randomized, double-blind, placebo-controlled Phase 3 study of resmetirom in patients with liver biopsy-confirmed NASH and was initiated in March 2019. The subpart H portion of the study enrolled more than 1,000 patients with biopsy-proven NASH (at least half with F3 (advanced) fibrosis, the remainder F2 or F1B (moderate fibrosis) with a few earlier F1 patients), randomized 1:1:1 to receive once-daily resmetirom 80 mg, resmetirom 100 mg, or placebo. After 52 weeks of treatment, a second liver biopsy is performed. The dual primary surrogate endpoints on biopsy are NASH resolution with ≥2-point reduction in NAS (NAFLD Activity Score), and with no worsening of fibrosis OR a 1-point decrease in fibrosis with no worsening of NAS. Achievement of either primary endpoint is considered a successful trial outcome. A key secondary endpoint is lowering of LDL-C.
All patients enrolled in the MAESTRO-NASH study (up to 2,000 in total) continue on therapy after the initial 52-week treatment period for up to 54 months to accrue and measure hepatic clinical outcome events including progression to cirrhosis on biopsy (52 weeks and 54 months) and hepatic decompensation events, as well as all-cause mortality.
MAESTRO-NAFLD-1 was initiated in December 2019 and the 52-week multicenter, randomized, placebo-controlled Phase 3 study of resmetirom in over 1,200 patients with NAFLD, presumed NASH, has completed the double-blind arms and an open-label 100 mg arm. An additional open-label active treatment arm in patients with early (well-compensated) NASH cirrhosis is ongoing. The primary endpoint was to evaluate the safety and tolerability of resmetirom. A separate 52 week Phase 3 clinical trial, an open-label extension study of MAESTRO-NAFLD-1 (MAESTRO-NAFLD-OLE), is ongoing.
Patients in the 52-week Phase 3 MAESTRO-NAFLD-1 study were randomized 1:1:1:1 to receive once-daily resmetirom 80 mg, resmetirom 100 mg, placebo in double-blind arms or resmetirom 100 mg in an open-label arm. MAESTRO-NAFLD-1 (unlike MAESTRO-NASH), did not include a liver biopsy and represents a “real-life” NASH study. Patients with 3 metabolic risk factors were documented with NASH or NAFLD by historical liver biopsy or noninvasive techniques. Using noninvasive measures, MAESTRO-NAFLD-1 was designed to provide incremental safety information to support the NASH indication as well as provide additional data regarding clinically relevant key secondary efficacy endpoints to better characterize the potential clinical benefits of resmetirom on cardiovascular- and liver-related endpoints. The primary safety endpoint and several key secondary endpoints were met, including LDL-C, apolipoprotein B, and triglyceride lowering and reduction of liver fat as determined by MRI-PDFF. Additional secondary and exploratory endpoints were assessed including reduction in liver enzymes, FibroScan, and MRE scores, and other NASH biomarkers.
Data from the 52-week first 1,000 patient portion of MAESTRO-NASH, together with data from MAESTRO-NAFLD-1, MAESTRO-NAFLD-OLE, Phase 2 and Phase 1 data, including safety parameters, will form the basis for a potential subpart H submission to FDA for accelerated approval of resmetirom for treatment of NASH.
In August 2022, Madrigal initiated MAESTRO-NASH-OUTCOMES, a randomized double-blind placebo-controlled study in approximately 700 patients with early NASH cirrhosis to allow for noninvasive monitoring of progression to liver decompensation events. A positive outcome is expected to support the full approval of resmetirom for noncirrhotic NASH, potentially accelerating the timeline to full approval. In addition, this study has the potential to support an additional indication for resmetirom in patients with well-compensated NASH cirrhosis.
About NASH
Nonalcoholic steatohepatitis (NASH) is a more advanced form of nonalcoholic fatty liver disease (NAFLD). NAFLD is estimated to afflict more than 20% of adults globally, about 30% in the United States. Of that population, 20% may have NASH.
NASH is a leading cause of liver related mortality and an increasing burden on healthcare systems globally. Additionally, patients with NASH, especially those with more advanced metabolic risk factors (hypertension, concomitant type 2 diabetes), are at increased risk for adverse cardiovascular events and increased morbidity and mortality.
Once NASH progresses to significant liver fibrosis (stages F2 and F3) the risk of adverse liver outcomes increases dramatically. NASH is rapidly becoming the leading cause of liver transplantation in the U.S. There are currently no FDA-approved therapies available for the treatment of NASH.
About Madrigal Pharmaceuticals
Madrigal Pharmaceuticals, Inc. (Nasdaq: MDGL) is a clinical-stage biopharmaceutical company pursuing novel therapeutics for nonalcoholic steatohepatitis (NASH), a liver disease with high unmet medical need. Madrigal’s lead candidate, resmetirom, is a once daily, oral, thyroid hormone receptor (THR)-β selective agonist designed to target key underlying causes of NASH in the liver. For more information, visit www.madrigalpharma.com.
Source: Madrigal Pharmaceuticals, Inc.
Madrigal up 210% on positive late-stage results for NASH candidate resmetirom
Dec. 19, 2022 8:48 AM ET
Madrigal Pharmaceuticals, Inc. (MDGL)VKTX
By: Jonathan Block, SA News Editor5 Comments
- Madrigal Pharmaceuticals (NASDAQ:MDGL) is up 210% in premarket trading after releasing late-stage results on resmetirom for nonalcoholic steatohepatitis (NASH) and liver fibrosis.
- https://seekingalpha.com/news/3918385-madrigal-up-210-on-positive-late-stage-results-for-nash-liver-candidate-resmetirom
- Madrigal Pharmaceuticals, Inc. (MDGL)
- https://www.madrigalpharma.com/our-programs/resmetirom/
- https://www.madrigalpharma.com/
Zolbetuximab
ABI-H3733 and ABI-4334
Zolbetuximab
Astellas Announces Zolbetuximab Meets Primary Endpoint in Phase 3 GLOW Trial as First-Line Treatment in Claudin 18.2 Positive, HER2-negative Locally Advanced Unresectable or Metastatic Gastric and Gastroesophageal Junction (GEJ) Cancers
Astellas' GLOW trial, the second Phase 3 trial in CLDN18.2 positive, HER2-negative locally advanced unresectable or metastatic gastric and GEJ cancers, meets primary endpoint for progression-free survival (PFS) and key secondary endpoint for overall survival (OS)
GLOW results, along with SPOTLIGHT topline results, mark progress in Astellas' gastric cancer development program
TOKYO, Dec. 15, 2022 /PRNewswire/ -- Astellas Pharma Inc. (TSE: 4503, President and CEO: Kenji Yasukawa, Ph.D., "Astellas") today announced positive topline results from the Phase 3 GLOW clinical trial evaluating the efficacy and safety of zolbetuximab in combination with CAPOX (a combination chemotherapy regimen that includes capecitabine and oxaliplatin). Zolbetuximab is an investigational first-in-class Claudin-18.2 (CLDN18.2) targeted monoclonal antibody, for the first-line treatment of patients with CLDN18.2-positive, HER2-negative, locally advanced unresectable or metastatic gastric or gastroesophageal junction (GEJ) adenocarcinoma.
The GLOW study met its primary endpoint showing statistical significance in progression-free survival (PFS) for patients treated with zolbetuximab plus CAPOX compared to placebo plus CAPOX. In addition, the study met a key secondary endpoint, overall survival (OS), showing statistical significance for patients treated with zolbetuximab plus CAPOX compared to placebo plus CAPOX. The most frequent treatment-emergent adverse events (TEAEs) were nausea and vomiting. Detailed results will be presented at a future scientific congress and submitted for publication.
"Zolbetuximab has the potential to be an innovative therapeutic option for patients with locally advanced unresectable or metastatic gastric or GEJ cancer, a difficult disease for which treatment options are still limited," said Ruihua Xu, MD, PhD, Primary Investigator for the GLOW study and Professor in the Department of Medical Oncology, Sun Yat-Sen University Cancer Center, Guangzhou, China. "I am so pleased with the topline results from GLOW that establish progression-free survival and overall survival in patients treated with zolbetuximab plus CAPOX."
"We are extremely pleased to share positive topline results from GLOW following the positive SPOTLIGHT readout last month. This further confirms the potential role of zolbetuximab in gastric cancer treatment, an important milestone in our gastric cancer development program," said Ahsan Arozullah, MD, MPH, Senior Vice President and Head of Development Therapeutic Areas, Astellas. "We intend to discuss these results with regulatory authorities as we continue to develop zolbetuximab for the first-line treatment of patients with locally advanced unresectable or metastatic gastric and GEJ cancer."
Zolbetuximab acts by binding to CLDN18.2 on the cancer cell surface of gastric epithelial cells. In pre-clinical studies, this binding interaction then induces cancer cell death by activating two distinct immune system pathways – antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC).1 CLDN18.2 is a type of transmembrane protein found in normal gastric cells and is a major component of epithelial tight junctions controlling the flow of molecules between cells.2 Pre-clinical studies have shown that CLDN18.2, which is frequently present in gastric tumors, may become more exposed and accessible to targeted antibodies as gastric tumors develop.3,4,5 Based on the SPOTLIGHT and GLOW studies, approximately 38% of these patients have CLDN18.2-positive tumors, meeting the qualification of CLDN18.2 expression in ≥75% of tumor cells with strong to moderate staining intensity based on a validated immunohistochemistry assay.6
The Phase 3 GLOW trial (n=507) is a global, multi-center, double-blind, randomized study assessing the efficacy and safety of zolbetuximab plus CAPOX compared to placebo plus CAPOX. This study, and the Phase 3 SPOTLIGHT trial (n=565), which evaluated the efficacy and safety of zolbetuximab plus a combination regimen of oxaliplatin, leucovorin and fluorouracil (mFOLFOX6) compared to placebo plus mFOLFOX6, were conducted to provide foundational data for regulatory submissions in the U.S., Europe, Asia and other countries globally. These studies are part of Astellas' gastric cancer development program to investigate new treatment options such as zolbetuximab and address patient needs in locally advanced unresectable or metastatic gastric or GEJ adenocarcinoma.
Gastric cancer is often diagnosed in the advanced or metastatic stage, or once it has spread from the tumor's origin to other body tissues or organs.7 The five-year relative survival rate for patients at the metastatic stage is approximately six percent.8,9
About Zolbetuximab
Zolbetuximab is an investigational, first-in-class chimeric IgG1 monoclonal antibody (mAb) that targets and binds to CLDN18.2, a transmembrane protein. Zolbetuximab acts by binding to CLDN18.2 on the cancer cell surface of gastric epithelial cells. In pre-clinical studies, this binding interaction then induces cancer cell death by activating two distinct immune system pathways — antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC).1 The safety and efficacy of zolbetuximab are under investigation in gastric, gastroesophageal and pancreatic cancers and have not been established. There is no guarantee the agent will receive regulatory approval or become commercially available for the uses being investigated.
About GLOW Phase 3 Clinical Trial
GLOW is a Phase 3, global, multi-center, double-blind, randomized study, assessing the efficacy and safety of zolbetuximab (IMAB362) plus CAPOX (a combination chemotherapy regimen which includes capecitabine and oxaliplatin) compared to placebo plus CAPOX as a first-line treatment of patients with CLDN18.2 positive, HER2- negative, locally advanced unresectable or metastatic gastric or GEJ cancer. The study enrolled 507 patients at 165 study locations in the U.S., Canada, United Kingdom, Europe, South America and Asia. The primary endpoint is progression-free survival of participants treated with combination of zolbetuximab plus CAPOX compared to those treated with placebo plus CAPOX. Secondary endpoints include overall survival, objective response rate, duration of response, safety and tolerability and quality-of-life parameters.
For more information, please visit clinicaltrials.gov under Identifier NCT03653507.
About SPOTLIGHT Phase 3 Clinical Trial
SPOTLIGHT is a Phase 3, global, multi-center, double-blind, randomized study, assessing the efficacy and safety of zolbetuximab (IMAB362) plus mFOLFOX6 (combination regimen of oxaliplatin, leucovorin and fluorouracil) compared to placebo plus mFOLFOX6 as a first-line treatment of patients with CLDN18.2-positive, HER2- negative, locally advanced unresectable or metastatic gastric or gastroesophageal junction cancer. The study enrolled 565 patients at 220 study locations in the U.S., United Kingdom, Australia, Europe, South America and Asia. The primary endpoint is progression-free survival of participants treated with combination of zolbetuximab plus mFOLFOX6 compared to those treated with placebo plus mFOLFOX6. Secondary endpoints include overall survival, objective response rate, duration of response, safety and tolerability and quality-of-life parameters.
For more information, please visit clinicaltrials.gov under Identifier NCT03504397
About Astellas
Astellas Pharma Inc. is a pharmaceutical company conducting business in more than 70 countries around the world. We are promoting the Focus Area Approach that is designed to identify opportunities for the continuous creation of new drugs to address diseases with high unmet medical needs by focusing on Biology and Modality. Furthermore, we are also looking beyond our foundational Rx focus to create Rx+® healthcare solutions that combine our expertise and knowledge with cutting-edge technology in different fields of external partners. Through these efforts, Astellas stands on the forefront of healthcare change to turn innovative science into VALUE for patients. For more information, please visit our website at https://www.astellas.com/en.
Astellas zolbetuximab shows survival benefit, meets main goal in 2nd gastric cancer trial
Dec. 16, 2022 6:29 AM ET
Astellas Pharma Inc. (ALPMY), ALPMF
By: Ravikash, SA News Editor
Astellas Pharma (OTCPK:ALPMF) (OTCPK:ALPMY) said its drug zolbetuximab, in combination with CAPOX, met the main goal of progression-free survival (PFS) in patients with gastric cancer in a phase 3 trial.
Astellas Pharma Inc. (ALPMY), ALPMF
https://www.astellas.com/en/system/files/2q2022_pip_en_1.pdf
biotecHOPE™ 2022
MVP-S, in combination with pembrolizumab
MVP-S, in combination with pembrolizumab
MVP-S, in combination with pembrolizumab
IMV Inc. Announces Initial Data from the Ongoing Phase 2B VITALIZE Trial in Patients with r/r DLBCL
DECEMBER 15, 2022 7:05AM EST
Complete responses were observed in patients who received at least three previous lines of treatment (including CAR-T's)
Recent clinical data add to the growing enthusiasm for the therapeutic potential of cancer vaccines in combination with checkpoint inhibitors
Oral presentation of the clinical data at the Immuno-Oncology 360° conference in February 2023
DARTMOUTH, Nova Scotia, & CAMBRIDGE, Mass.--(BUSINESS WIRE)-- IMV Inc. (Nasdaq: IMV; TSX: IMV) (“IMV” or the “Company”), a clinical-stage biopharmaceutical company developing a portfolio of immune-educating therapies based on its novel DPX® platform to treat solid and hematologic cancers, today announced positive initial patient data from the VITALIZE Phase 2B trial evaluating its lead DPX product, MVP-S, in combination with pembrolizumab in patients with relapsed, refractory Diffuse Large B Cell Lymphoma (“r/r DLBCL”) who received at least three previous lines of treatment. Detailed results will be presented in a podium presentation at the Immuno-Oncology 360° conference to be held in New York City on February 7-10, 2023.
“The initial clinical data from the VITALIZE trial are encouraging and the accelerating recruitment in this study reflects a growing interest for this therapeutic combination in DLBCL,” said Dr. Matthew Matasar, Chief of Blood Disorders at Rutgers Cancer Institute of New Jersey and RWJBarnabas Health, and primary investigator of the VITALIZE trial. He added: “We find it remarkable that we have seen complete responses in this trial in patients that were refractory to prior cellular therapy and other advanced therapies.”
“Positive initial results for the VITALIZE trial are an important development milestone for MVP-S” said Andrew Hall, CEO of IMV “Alongside other compelling cancer vaccine data announced this week, these data on MVP-S highlight renewed interest in the potential for cancer vaccines as a therapeutic class.”
Andrew Hall added “A well-tolerated, easy-to-administer therapy, such as MVP-S, that provides durable clinical benefit is meaningful for patients who have already been subject to aggressive, toxic treatment regimens. Clinical activity in a highly refractory patient population may represent a path to registration in DLBCL.”
About the VITALIZE Study
The VITALIZE Phase 2B trial is a randomized, parallel group, Simon two-stage study designed to assess IMV’s lead candidate, MVP-S, in combination with pembrolizumab with or without cyclophosphamide. Across the arms of this study, the combination will be evaluated in up to 102 subjects with r/r DLBCL who have received at least two prior lines of systemic therapy and who are ineligible or have failed autologous stem cell transplant (ASCT) or CAR-T therapy.
The primary endpoint is Objective Response Rate (ORR), centrally evaluated per Lugano (2014) and measured by the number of subjects per arm achieving a best clinical response of Partial or Complete Response (PR+CR) during the 2-year treatment period. All subjects will be evaluated for their baseline PD-L1 expression. Exploratory endpoints include evaluation of cell-mediated immune response, tumor immune cell infiltration, and other biomarker analyses.
About IMV
IMV Inc. is a clinical-stage immuno-oncology company advancing a portfolio of therapies based on the Company’s immune-educating platform, DPX®. Through a differentiated mechanism of action, the DPX platform delivers instruction to the immune system to generate a specific, robust, and persistent immune response. IMV’s lead candidate, maveropepimut-S (MVP-S), delivers antigenic peptides from survivin, a well-recognized cancer antigen commonly overexpressed in advanced cancers. MVP-S also delivers an innate immune activator and a universal CD4 T cell helper peptide. These elements foster maturation of antigen presenting cells as well as robust activation of CD8 T cell effector and memory function. MVP-S treatment has been well tolerated and has demonstrated defined clinical benefit in multiple cancer indications as well as the activation of a targeted and sustained, survivin-specific anti-tumor immune response. MVP-S is currently being evaluated in clinical trials for hematologic and solid cancers, including Diffuse Large B Cell Lymphoma (DLBCL) as well as ovarian, bladder and breast cancers. IMV is also developing a second immunotherapy leveraging the DPX immune delivery platform, DPX-SurMAGE. This dual-targeted immunotherapy combines antigenic peptides for both the survivin and MAGE-A9 cancer proteins to elicit immune responses to these two distinct cancer antigens simultaneously. A Phase 1 clinical trial in bladder cancer, using MVP-S or DPX-SurMAGE, was initiated in early 2022. For more information, visit www.imv-inc.com and connect with us on Twitter and LinkedIn.
View source version on businesswire.com: https://www.businesswire.com/news/home/20221215005319/en/
Source: IMV Inc.
Released December 15, 2022
IMV surges 40% on positive initial data from trial to treat Diffuse Large B Cell Lymphoma
Dec. 15, 2022 8:57 AM ET
By: Dania Nadeem, SA News Editor
- IMV (NASDAQ:IMV) is trading ~40% higher premarket after a mid-stage trial testing its lead DPX product, MVP-S, in combination with Merck's drug Keytruda (pembrolizumab) to treat relapsed, refractory Diffuse Large B Cell Lymphoma showed complete response in patients who received at least three previous lines of treatment.
- https://seekingalpha.com/news/3917557-imv-surges-40-on-positive-initial-data-from-trial-to-treat-diffuse-large-b-cell-lymphoma
- IMV Inc. (IMV), IMV:CA
- https://www.imv-inc.com/product-pipeline/maveropepimut-S
KT-474 (IRAK4)
MVP-S, in combination with pembrolizumab
MVP-S, in combination with pembrolizumab
Kymera Announces Positive Results from Phase 1 Clinical Trial Evaluating KT-474 in Patients with HS and AD and Sanofi’s Decision to Advance KT-474 into Phase 2 Clinical Trials
Dec 14, 2022
KT-474 Phase 1 clinical data in HS and AD patients demonstrate robust IRAK4 knockdown in blood and active skin lesions and systemic suppression of proinflammatory cytokines and chemokines with a favorable safety profile
Clinical endpoints addressing disease burden and symptoms demonstrate a highly competitive profile after four weeks of dosing, with substantial responses in majority of both HS and AD patients
Modest, non-adverse QTc prolongation spontaneously resolves back to baseline during the 4-week dosing period
Sanofi has committed to advance KT-474 (SAR444656) into Phase 2 clinical trials
Oncology programs KT-413 and KT-333 demonstrate substantial target knockdown in ongoing Phase 1a dose escalation clinical trials, with no dose limiting toxicities observed
MDM2 (KT-253) IND cleared by FDA; Phase 1 to start in early 2023
Kymera to host webcast today at 8:00 a.m. EST; webcast link available here.
WATERTOWN, Mass., Dec. 14, 2022 (GLOBE NEWSWIRE) -- Kymera Therapeutics, Inc. (NASDAQ: KYMR), a clinical-stage biopharmaceutical company advancing targeted protein degradation (TPD) to deliver novel small molecule protein degrader medicines, today announced positive clinical results from the patient cohort portion of its KT-474 (IRAK4) Phase 1 clinical trial, as well as updates on its three oncology programs: KT-413 (IRAKIMiD), KT-333 (STAT3) and KT-253 (MDM2).
“This is a pivotal moment for Kymera and for the field of protein degradation,” said Nello Mainolfi, PhD, Founder, President and CEO. “Kymera was founded to harness the enormous potential of targeted protein degradation and bring more effective therapies to patients. We believe that, for the first time, we have demonstrated clinical impact of a degrader, KT-474, outside of oncology and in complex inflammatory diseases such as HS and AD. We have also demonstrated the superior clinical potential of an IRAK4 degrader over a small molecule inhibitor, validating our platform and target selection strategy. In addition, we are excited that programs from our oncology pipeline continue to show fidelity of translation of PK, PD and safety from preclinical to human patients, validating our proprietary molecular design and translational quantitative system pharmacology modelling. We are on track to achieve our ambitious objectives of building a disease- and technology-agnostic, fully integrated global biopharmaceutical company that will continue to advance degrader drugs with potentially best-in-class, differentiated profiles across multiple indications.”
IRAK4 Degrader (KT-474)
Part C of Kymera’s KT-474 Phase 1 clinical trial was designed to confirm that the PK/PD and safety data previously demonstrated in healthy volunteers would translate into patients with hidradenitis suppurativa (HS) and atopic dermatitis (AD). Data was also collected on the change in circulating inflammatory biomarkers and proinflammatory gene transcripts in the patients’ skin, as well as on multiple clinical endpoints.
“The patient cohort results exceeded our expectations for a trial with only 4 weeks of dosing, demonstrating not only robust IRAK4 degradation in blood and skin with a favorable safety profile comparable to what was observed in healthy volunteers, but also a systemic anti-inflammatory response associated with improvement in skin lesions and symptoms in both HS and AD patients,” said Jared Gollob, MD, Chief Medical Officer. “We believe these results provide the first clinical validation for targeting the IRAK4 pathway with a degrader in TLR/IL-1R-driven inflammatory diseases, with KT-474 exhibiting activity that is clearly differentiated from IRAK4 small molecule kinase inhibitors and that has the potential to improve the lives of patients with HS and AD.”
Sanofi, which is collaborating with Kymera on the development of KT-474 (SAR444656) outside of the oncology and immune-oncology fields, has notified Kymera of its commitment to advance KT-474 into Phase 2 clinical studies. Initial Phase 2 clinical trial of KT-474 will investigate its potential in HS and AD with the first study initiating in 2023.
“The HS and AD patient data are encouraging as they highlight the broad potential of KT-474 and continue to validate Sanofi’s commitment to the target and to TPD’s unique ability to unlock this critical pathway,” said Naimish Patel, MD, Head of Global Development, Immunology and Inflammation at Sanofi. “We look forward to advancing the program into Phase 2 studies, and the potential that KT-474 offers to patients with a variety of immunological conditions.”
Study Design: Part C patients were dosed for 28 days and subsequently followed for an additional 2 weeks out to Day 42. Patients received 75 mg of KT-474 once daily in the fed state. That dose was selected to achieve similar exposures to healthy volunteers in the multiple ascending dose (MAD) portion of the Phase 1 clinical trial who received 100 mg in the fasted state (MAD3).
Baseline Characteristics and Disposition: A total of 21 patients were enrolled in the trial, including 13 HS and 8 AD patients, with median age 31-40 years (13 female, 8 male). Disease severity for HS was moderate (10), severe (1) and very severe (2) and for AD was mild (1), moderate (5) and severe (2). One HS and 1 AD patient withdrew from treatment early due to personal reasons, resulting in 12 HS and 7 AD patients evaluable for PD and clinical efficacy.
Pharmacokinetics/IRAK4 Pharmacodynamics: In patients with HS and AD, KT-474 demonstrated plasma PK in Part C that was comparable to healthy volunteers in MAD3. Baseline IRAK4 level in skin lesions of HS and AD patients was approximately two-fold higher compared to healthy volunteers. KT-474 demonstrated IRAK4 knockdown in both blood and skin that was comparable to MAD3, with maximum degradation exceeding 90%. Target degradation was similar across HS and AD patients in both blood and skin.
Activity Against Biomarkers of Inflammation: In ex vivo cytokine stimulation assays, KT-474 demonstrated broad and deep inhibition of multiple disease-relevant cytokines, including inhibition of up to 84% in HS and up to 98% in AD. Cytokine reductions across both patient groups in Part C were comparable or superior to what was observed in MAD3. KT-474 also reduced several circulating cytokines and acute phase reactants in vivo such as IL-6, CRP, IL-1b and serum amyloid A (SAA). In serial biopsies of skin lesions, proinflammatory gene transcripts that were strongly downregulated in at least 50% of evaluable patients included but not limited to: IL-5, NLRP3, CXCL1 and IL-2RB in AD and IL-1b, IL-36A, IL-17A, IFN-g, IL-8, granzyme B, IL-2RA and CSF3 in HS.
Safety: KT-474 was generally safe and well-tolerated, with no serious adverse events, no drug-related infections, and no dose interruptions or discontinuations due to adverse events. Adverse events, which included headache, fatigue and diarrhea, were predominantly mild, and all fully resolved. Previously seen modest, non-adverse QTcF prolongation was observed at Days 7-14, the mean of which was slightly below the mean levels at similar timepoints in HV MAD3. The QTcF prolongation declined spontaneously with continued dosing, with resolution to baseline by Day 28, and remained in the same normal range after cessation of dosing.
“I am pleased to see the positive clinical activity signals in both HS and AD in this patient cohort, with the internal consistency between effects on inflammatory biomarkers and impact on clinical endpoints increasing confidence in results from a single-arm trial,” said Afsaneh Alavi, MD, Professor of Dermatology at Mayo Clinic. “I believe these promising early efficacy and safety data in patients support the further development and exciting potential of orally-administered KT-474 in HS and AD.”
Oncology Degraders: KT-333, KT-413, KT-253
Kymera’s oncology programs include two molecules in Phase 1 clinical trials, KT-333 and KT-413, and KT-253, a program that is scheduled to enter the clinic in early 2023.
“We believe the initial data from the dose escalation phase of our ongoing KT-333 and KT-413 trials are very encouraging, as they are demonstrating fidelity of PK/PD translation from preclinical models to patients, and showing that, even at low doses, we are seeing target degradation in blood and tumor without any dose limiting toxicities observed,” said Dr. Gollob. “We view this as important proof of mechanism and a critical first step in our plans to escalate dosing to levels which we expect will demonstrate clinical impact in our target patient populations and look forward to sharing additional data in 2023.”
STAT3 degrader program (KT-333)
KT-333 is a potent degrader of STAT3, a transcriptional regulator that has been linked to numerous cancers and other inflammatory and autoimmune diseases. KT-333 is being developed for the treatment of STAT3-dependent hematological malignancies and solid tumors. The Phase 1 clinical trial of KT-333 is designed to evaluate the safety, tolerability, PK/PD and clinical activity of KT-333 dosed weekly on Days 1, 8 and 15 of 28-day cycles in adult patients with relapsed and/or refractory lymphomas, leukemias and solid tumors.
The Phase 1a dose escalation portion of the trial is ongoing; dose level 1 (DL1, 0.05 mg/kg) has been completed with a total of four patients enrolled. All patients were heavily pretreated with multiple prior lines of therapy and included three patients with solid tumors and one patient with cutaneous T-cell lymphoma. Plasma PK and PD translated as expected in humans with mean maximum STAT3 degradation in PBMC following the first 2 doses averaging 66%, with maximum STAT3 knockdown of up to 86% as measured by mass spectrometry. There were no DLTs or treatment-related SAEs observed in DL1. DL2 [0.10 mg/kg] is currently enrolling.
Kymera plans to share additional STAT3 clinical data in 2023.
IRAKIMiD degrader program (KT-413)
KT-413 is a novel heterobifunctional degrader targeting both IRAK4 and the IMiD substrates Ikaros and Aiolos. Designed to address both the IL-1R/TLR and Type 1 IFN pathways synergistically with a single molecule, KT-413 is in development for the treatment of MYD88-mutant B cell malignancies. The Phase 1 clinical trial of KT-413 is designed to evaluate the safety, tolerability, PK/PD and clinical activity of KT-413 administered as an IV infusion once every 3 weeks to adult patients with relapsed and/or refractory B-cell non-Hodgkin's lymphomas.
The Phase 1a dose escalation portion of the trial is ongoing; dose level 1 (DL1, 0.16 mg/kg) and dose level 2 (DL2, 0.32 mg/kg) have been completed. Patients in both dose cohorts were heavily pretreated, having received multiple prior lines of therapy, and included follicular lymphoma and nodular lymphocyte-predominant Hodgkin lymphoma, which were both wild-type for MYD88. Plasma PK and PD also translated as expected in humans with DL1 and DL2 showing dose-dependent degradation of IRAK4, Ikaros and Aiolos in PBMC, with up to 95/100% knockdown of Ikaros/Aiolos and 40% knockdown of IRAK4 in DL2. Serial tumor biopsies at Cycle 3/Day 4 in the patient treated at DL1 showed comparable knockdown of Ikaros/Aiolos and IRAK4 as in plasma. There were no DLTs or treatment-related SAEs and no neutropenia observed in DL1 and DL2 patient cohorts. Phase 1a dose escalation is ongoing and DL3 (0.51 mg/kg) is currently enrolling.
Kymera plans to share additional IRAKIMiD clinical data in 2023.
MDM2 degrader program (KT-253)
The FDA has cleared the IND for KT-253, a degrader that targets MDM2, the crucial regulator of the most common tumor suppressor, p53, which remains intact (WT) in more than 50% of cancers. Unlike small molecule inhibitors, KT-253 has been shown preclinically to have the ability to suppress the MDM2 feedback loop and rapidly induce apoptosis, even with brief exposures. Kymera is currently preparing to initiate a Phase 1 clinical trial evaluating the safety, tolerability, PK/PD and clinical activity of KT-253 in adult patients with liquid and solid tumors in 2023. Kymera plans to share more details around the trial design and timelines in early 2023.
About Kymera Therapeutics
Kymera is a biopharmaceutical company pioneering the field of targeted protein degradation, a transformative approach to address disease targets and pathways inaccessible with conventional therapeutics. Kymera’s Pegasus platform is a powerful drug discovery engine, advancing novel small molecule programs designed to harness the body’s innate protein recycling machinery to degrade dysregulated, disease-causing proteins. With a focus on undrugged nodes in validated pathways, Kymera is advancing a pipeline of novel therapeutic candidates designed to address the most promising targets and provide patients with more effective treatments. Kymera’s initial programs target IRAK4, IRAKIMiD, and STAT3 within the IL-1R/TLR or JAK/STAT pathways, and the MDM2 oncoprotein, providing the opportunity to treat patients with a broad range of immune-inflammatory diseases, hematologic malignancies, and solid tumors. For more information, visit www.kymeratx.com.
Founded in 2016, Kymera is headquartered in Watertown, Mass. Kymera has been named a “Fierce 15” company by Fierce Biotech and has been recognized by both the Boston Globe and the Boston Business Journal as one of Boston’s top workplaces. For more information about our people, science, and pipeline, please visit www.kymeratx.com or follow us on Twitter or LinkedIn.
Kymera surges 30% as Sanofi plans to advance drug after promising data in skin disorders
Dec. 14, 2022 7:54 AM ET
Kymera Therapeutics, Inc. (KYMR), SNY
By: Ravikash, SA News Editor
Kymera Therapeutics (NASDAQ:KYMR) reported data from a patient group portion of its drug KT-474 (IRAK4) from a phase 1 trial, and updates on its three oncology programs: KT-413 (IRAKIMiD), KT-333 (STAT3) and KT-253 (MDM2).
KT-474:
The company said Part C of its KT-474 phase 1 trial was designed to confirm that the Pharmacokinetics/Pharmacodynamics ((PK/PD)) and safety data previously shown in healthy people would translate into patients with hidradenitis suppurativa (HS) and atopic dermatitis (AD), also known as eczema.
Kymera Therapeutics, Inc. (KYMR), SNY
https://www.kymeratx.com/pipeline/
upifitamab rilsodotin (UpRi)
MVP-S, in combination with pembrolizumab
upifitamab rilsodotin (UpRi)
European Commission Designates UpRi as an Orphan Medicinal Product for the Treatment of Ovarian Cancer
December 14, 2022
CAMBRIDGE, Mass., Dec. 14, 2022 (GLOBE NEWSWIRE) -- Mersana Therapeutics, Inc. (NASDAQ: MRSN), a clinical-stage biopharmaceutical company focused on discovering and developing a pipeline of antibody-drug conjugates (ADCs) targeting cancers in areas of high unmet medical need, today announced that the European Commission (EC) has designated upifitamab rilsodotin (UpRi) as an orphan medicinal product for the treatment of ovarian cancer. UpRi is Mersana’s first-in-class NaPi2b-targeting ADC with a novel scaffold-linker-payload that is designed to enable a high drug-to-antibody ratio and controlled bystander effect.
“Receiving this orphan designation in the European Union is an important regulatory milestone for Mersana as we seek to expedite UpRi’s global development,” said Anna Protopapas, President and Chief Executive Officer of Mersana Therapeutics. “This designation reinforces the unmet needs that patients with ovarian cancer continue to face today. We look forward to advancing our ongoing clinical trials, which aim to establish UpRi as a foundational medicine in ovarian cancer.”
The European Commission designates drugs as orphan medicinal products based on positive opinions adopted by the European Medicines Agency (EMA) Committee for Orphan Medicinal Products (COMP). Orphan designations are granted for potential treatments for rare diseases that are life-threatening or chronically debilitating that affect fewer than five in 10,000 people across the European Union. Medicines designated as orphan medicinal products by the EMA may qualify for financial and regulatory incentives, including protocol assistance at reduced fees during product development, access to centralized marketing authorization and 10 years of marketing exclusivity in the European Union after product approval.
About Mersana Therapeutics
Mersana Therapeutics is a clinical-stage biopharmaceutical company using its differentiated and proprietary ADC platforms to rapidly develop novel ADCs with optimal efficacy, safety and tolerability to meaningfully improve the lives of people fighting cancer. Mersana’s lead product candidate, upifitamab rilsodotin (UpRi), is a Dolaflexin ADC targeting NaPi2b that is being studied in UPLIFT, a single-arm registrational trial in patients with platinum-resistant ovarian cancer; UPGRADE-A, a Phase 1/2 clinical trial evaluating UpRi in combination with carboplatin; and UP-NEXT, a Phase 3 clinical trial of UpRi as monotherapy maintenance following treatment with platinum doublets in recurrent platinum-sensitive ovarian cancer. Mersana is also advancing XMT-1660, a Dolasynthen ADC targeting B7-H4, and XMT-2056, an Immunosynthen ADC targeting a novel epitope of human epidermal growth factor receptor 2 (HER2), in addition to other earlier-stage assets. In addition, multiple partners are using Mersana’s platforms to advance their ADC pipelines. Mersana routinely posts information that may be useful to investors on the “Investors & Media” section of its website at www.mersana.com.
Mersana Therapeutics gets European orphan drug designation for ovarian cancer treatment
Dec. 14, 2022 9:05 AM ET
Mersana Therapeutics, Inc. (MRSN)
By: Anuron Mitra, SA News Editor
- Mersana Therapeutics (NASDAQ:MRSN) on Wednesday said the European Commission had granted an orphan drug designation to its antibody drug conjugate for the treatment of ovarian cancer.
- https://seekingalpha.com/news/3916921-mersana-gets-european-orphan-drug-designation-for-ovarian-cancer-treatment
- Mersana Therapeutics, Inc. (MRSN)
- https://www.mersana.com/pipeline/xmt-1536/
KRAZATI™ (adagrasib)
AYVAKIT® (avapritinib)
upifitamab rilsodotin (UpRi)
Mirati Therapeutics Announces U.S. FDA Accelerated Approval of KRAZATI™ (adagrasib) as a Targeted Treatment Option for Patients with Locally Advanced or Metastatic Non-Small Cell Lung Cancer (NSCLC) with a KRASG12C Mutation
12/12/2022
SAN DIEGO, Dec. 12, 2022 /PRNewswire/ -- Mirati Therapeutics, Inc. (NASDAQ: MRTX), a targeted oncology company, today announced that the U.S. Food and Drug Administration (FDA) has granted accelerated approval for KRAZATI™ (adagrasib), a targeted treatment option for adult patients with KRASG12C-mutated locally advanced or metastatic non-small cell lung cancer (NSCLC), as determined by an FDA-approved test, who have received at least one prior systemic therapy.
Experience the full interactive Multichannel News Release here: https://www.multivu.com/players/English/8999051-mirati-therapeutics-fda-accelerated-approval-of-krazati-adagrasib/
This indication is approved under accelerated approval based on objective response rate (ORR) and duration of response (DOR). Continued approval for this indication may be contingent upon verification and description of a clinical benefit in a confirmatory trial(s).
To view the multimedia assets associated with this release, please visit: Mirati.com/approval
"The FDA approval of KRAZATI is a positive development for thousands of patients with KRASG12C mutations, including the approximately 14% of patients with NSCLC adenocarcinomas histology that harbor a KRASG12C mutation.1 Mirati is thrilled to make KRAZATI available in a tablet formulation to patients in the U.S. with advanced NSCLC who have progressed beyond a first-line treatment for the historically difficult-to-treat KRAS mutation," David Meek, chief executive officer, Mirati Therapeutics, Inc., continued, "We look forward to continuing to advance our KRAZATI development program including several monotherapy and combination studies in KRASG12C-mutated solid tumors."
KRAZATI has demonstrated a positive benefit-risk profile with accelerated approval based on the Phase 2 registration-enabling cohort of the KRYSTAL-1 study, evaluating KRAZATI 600 mg capsules administered orally twice daily in 116 patients with KRASG12C-mutated advanced NSCLC who previously received treatment with a platinum-based regimen and an immune checkpoint inhibitor. The primary efficacy endpoints were confirmed ORR and DOR as evaluated by blinded independent central review (BICR) according to response evaluation criteria in solid tumors (RECIST v1.1).
The trial demonstrated an ORR of 43% (95% CI: 34-53) with 80% (95% CI: 71-87) of patients achieving disease control. The median DOR was 8.5 months (95% CI: 6.2-13.8).
In a pooled efficacy analysis (n=132) including Phase 1/1b NSCLC and registrational Phase 2 NSCLC cohorts from the KRYSTAL-1 study evaluating adagrasib as a single agent at 600 mg capsules orally twice daily, adagrasib showed an ORR of 44% and a disease control rate of 81% based on BICR, a median DOR of 12.5 months (95% CI, 7.3-NE) and median overall survival of 14.1 months (94% CI, 9.2-19.2).
The safety profile of KRAZATI was evaluated in a pooled patient population with NSCLC and other solid tumors as a single agent at 600 mg orally twice daily in 366 patients enrolled in KRYSTAL-1 and KRYSTAL-12. The most common (≥ 25%) adverse reactions were nausea, diarrhea, vomiting, fatigue, musculoskeletal pain, hepatotoxicity, renal impairment, edema, dyspnea and decreased appetite. Permanent discontinuation of KRAZATI due to an adverse reaction occurred in 13% of patients.
Although KRASG12C is the most common KRAS mutation in NSCLC, patients have had limited options for the treatment of this debilitating and difficult-to-treat condition.2,3
"The approval of KRAZATI offers an effective therapy for patients with advanced NSCLC harboring the KRASG12C mutation. The positive ORR and DOR results, as observed in previously treated patients with NSCLC harboring the KRASG12C mutation, demonstrate the effectiveness of KRAZATI as an option for these difficult-to-treat patients," said Shirish M. Gadgeel, MD, chief of the Division of Hematology and Oncology, Department of Internal Medicine, Henry Ford Cancer Institute/Henry Ford Health System.
"KRASG12C in NSCLC is an area of high unmet need and new treatment options offer patients and our community new hope for survivorship," said Bonnie J. Addario, co-founder and board chair of the GO2 Foundation for Lung Cancer. "I'm pleased that patients have options, there's more awareness of this disease and we are all focused on improving the journeys of people living with KRASG12C-mutated NSCLC."
The Company partnered with Agilent and QIAGEN to develop blood- and tissue-based companion diagnostics (CDx), respectively, for KRAZATI that are now available. With tissue and blood modalities for companion diagnostics, patients have more flexibility, and clinicians have greater options for biomarker testing. These solutions help to personalize a patient's treatment path.
Mirati Therapeutics is launching Mirati & Me, a comprehensive program dedicated to supporting patients, caregivers and the oncology community including coverage and access, financial, educational and emotional support services. Learn more by visiting the Mirati & Me website or 1-844-647-2842.
For more information, visit KRAZATI.com.
About KRAZATI (adagrasib)
Mirati has risen to meet one of the most challenging mutations in cancer research by developing KRAZATI, a highly selective and potent oral small-molecule inhibitor of KRASG12C.
Intentionally designed to meet the challenge of KRASG12C, adagrasib is optimized to sustain target inhibition, an attribute that could be important to treat KRASG12C-mutated cancers, as the KRASG12C protein regenerates every 24−48 hours.4 Adagrasib has shown clinically to be a CNS penetrant, which may be important given that CNS metastases frequently occur in NSCLC and lead to poor prognosis.5,6,7
In the U.S., KRAZATI was reviewed by the FDA for Accelerated Approval (Subpart H), which allows for the approval of drugs that treat serious conditions, and that fill an unmet medical need based on surrogate endpoints. KRAZATI was reviewed under the FDA Real-Time Oncology Review (RTOR) pilot program, which aims to explore a more efficient review process that ensures safe and effective treatments are made available to patients as early as possible. Mirati submitted a Marketing Authorization Application (MAA) in the EU in May 2022. In 2021, adagrasib achieved Breakthrough Therapy Designation in the U.S. as a potential treatment for patients with NSCLC harboring the KRASG12C mutation who have received at least one prior systemic therapy.
Adagrasib continues to be evaluated as monotherapy and in combination with other anti-cancer therapies in patients with advanced KRASG12C-mutated solid tumors, including NSCLC, colorectal cancer, and pancreatic cancer. For more information, visit Mirati.com/science.
Mirati has an Expanded Access Program (EAP) for adagrasib for the treatment of eligible patients with KRASG12C-mutated cancers, regardless of tumor type, including patients with treated or untreated CNS metastases, in the U.S. Learn more about the EAP at Mirati.com/expanded-access-policy.
KRAZATI (adagrasib) U.S. Indication
KRAZATI is indicated for the treatment of adult patients with KRASG12C-mutated locally advanced or metastatic non-small cell lung cancer (NSCLC), as determined by an FDA-approved test, who have received at least one prior systemic therapy.
This indication is approved under accelerated approval based on objective response rate (ORR) and duration of response (DOR). Continued approval for this indication may be contingent upon verification and description of a clinical benefit in a confirmatory trial(s).
Please see Full Prescribing Information .
About Mirati Therapeutics, Inc.
Mirati Therapeutics, Inc. is a commercial-stage biotechnology company whose mission is to discover, design and deliver breakthrough therapies to transform the lives of patients with cancer and their loved ones. The company is relentlessly focused on bringing forward therapies that address areas of high unmet need, including lung cancer, and advancing a pipeline of novel therapeutics targeting the genetic and immunological drivers of cancer. Unified for patients, Mirati's vision is to unlock the science behind the promise of a life beyond cancer.
For more information about Mirati, visit us at Mirati.com or follow us on Twitter, LinkedIn and Facebook.
SOURCE Mirati Therapeutics, Inc.
Mirati non-small cell lung cancer treatment adagrasib gains FDA approval - Bloomberg
Dec. 12, 2022 5:28 PM ET
Mirati Therapeutics, Inc. (MRTX)AMGN
By: Jonathan Block, SA News Editor3 Comments
- The US FDA has approved Mirati Therapeutics' (NASDAQ:MRTX) Krazati (adagrasib) a second-line treatment for non-small cell lung cancer, Bloomberg reported.
- https://seekingalpha.com/news/3916337-mirati-non-small-cell-lung-cancer-treatment-adagrasib-gains-fda-approval-bloomberg
- Mirati Therapeutics, Inc. (MRTX)
- https://www.mirati.com/science/pipeline/
- https://www.statnews.com/2022/12/12/lung-cancer-mirati-krazati-fda-approval-kras/
VX-522
AYVAKIT® (avapritinib)
AYVAKIT® (avapritinib)
Dec 12, 2022
Vertex Announces Investigational New Drug (IND) Application for VX-522, mRNA Therapy for People With Cystic Fibrosis, Cleared by FDA
- Novel, inhaled mRNA therapy intended for the ~5,000 people with CF who cannot benefit from CFTR modulators -
- VX-522 clinical trial in people with CF to initiate in coming weeks -
BOSTON--(BUSINESS WIRE)--Dec. 12, 2022-- Vertex Pharmaceuticals Incorporated (Nasdaq: VRTX) today announced that the U.S. Food and Drug Administration has cleared its Investigational New Drug (IND) application for VX-522, a messenger ribonucleic acid (mRNA) therapy targeted at treating the underlying cause of cystic fibrosis (CF) lung disease for the approximately 5,000 people with CF who cannot benefit from a cystic fibrosis transmembrane conductance regulator (CFTR) modulator. Vertex plans to initiate a single ascending dose clinical trial for VX-522 in people with CF in the coming weeks.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20221208005977/en/
VX-522 is delivered to the lung through inhalation of a CFTR mRNA encapsulated by a lipid nanoparticle. Once delivered to the target lung cells, the mRNA is designed to produce functional copies of the CFTR protein. VX-522 is the result of an exclusive research collaboration established with Moderna in 2016.
“It has been our longstanding goal to bring highly effective therapies to all people with CF. Clearance of the IND represents a pivotal turning point in reaching the remaining ~5,000 people with CF who are still waiting for a medicine to treat the underlying cause of their disease,” said Reshma Kewalramani, M.D., FASN, Chief Executive Officer and President, Vertex. “The partnership with Moderna that began more than five years ago has been instrumental in achieving this milestone, and we look forward to continuing our work together.”
“This partnership brings together Vertex’s scientific expertise and decades of experience in developing cystic fibrosis medicines with Moderna’s proven leadership in mRNA technologies,” said Moderna Chief Executive Officer Stéphane Bancel. “Moderna’s development of a proprietary inhalable lipid nanoparticle to deliver a functional cystic fibrosis treatment to the lungs could lead to a transformational medical achievement. We are excited by the progress that has been made with the upcoming advancement of VX-522 to the clinic and look forward to our ongoing collaboration to develop treatments for the underlying cause of cystic fibrosis.”
About VX-522
This investigational messenger ribonucleic acid (mRNA) therapy aims to address the underlying cause of cystic fibrosis (CF). It is being evaluated by Vertex to treat lung disease for people living with CF who cannot benefit from cystic fibrosis transmembrane conductance regulator (CFTR) modulator treatments because they do not make any CFTR protein that responds to a CFTR modulator therapy. Globally, this represents a population of approximately 5,000 people living with this very rare form of the disease. The therapy is designed to deliver full length CFTR mRNA encapsulated in a lipid nanoparticle via inhalation directly to the lungs. Once delivered to target airway cells, the mRNA enables the production of functional CFTR protein. Improvements in CFTR quantity and function can lead to transformative benefits for people living with CF.
About the VX-522 Clinical Trial
Vertex plans to initiate a single dose escalation study in the coming weeks evaluating the safety and tolerability of VX-522 in people 18 years of age and older with cystic fibrosis and a CFTR genotype not responsive to CFTR modulator therapy.
About the Vertex and Moderna Collaboration
VX-522 is the result of an exclusive research collaboration Vertex established with Moderna in 2016 to discover and develop mRNA therapeutics for CF. Under the terms of the collaboration, Moderna leads asset identification efforts, combining its leading mRNA platform technology and mRNA delivery expertise together with Vertex's scientific experience in CF biology, functional understanding of CFTR, and Vertex’s proprietary assay platform that utilizes human bronchial epithelial (HBE) cells of multiple different CF gene mutations from people with CF. Vertex leads preclinical and clinical development, regulatory and commercialization activities associated with the advancement of mRNA therapeutics that result from this collaboration and will fund all expenses related to the collaboration. Moderna is responsible for mRNA and lipid nanoparticle (LNP) process development and manufacturing. Per Vertex's agreement with Moderna, Moderna will receive certain milestone payments, as well as royalty payments from this collaboration.
About Vertex
Vertex is a global biotechnology company that invests in scientific innovation to create transformative medicines for people with serious diseases. The company has multiple approved medicines that treat the underlying cause of cystic fibrosis (CF) — a rare, life-threatening genetic disease — and has several ongoing clinical and research programs in CF. Beyond CF, Vertex has a robust clinical pipeline of investigational small molecule, cell and genetic therapies in other serious diseases where it has deep insight into causal human biology, including sickle cell disease, beta thalassemia, APOL1-mediated kidney disease, pain, type 1 diabetes and alpha-1 antitrypsin deficiency.
Founded in 1989 in Cambridge, Mass., Vertex's global headquarters is now located in Boston's Innovation District and its international headquarters is in London. Additionally, the company has research and development sites and commercial offices in North America, Europe, Australia and Latin America. Vertex is consistently recognized as one of the industry's top places to work, including 13 consecutive years on Science magazine's Top Employers list and one of Fortune’s Best Workplaces in Biotechnology and Pharmaceuticals and Best Workplaces for Women. For company updates and to learn more about Vertex's history of innovation, visit www.vrtx.com or follow us on Facebook, Twitter, LinkedIn, YouTube and Instagram.
View source version on businesswire.com: https://www.businesswire.com/news/home/20221208005977/en/
Source: Vertex Pharmaceuticals Incorporated
Vertex receives IND clearance for mRNA cystic fibrosis therapy
Dec. 12, 2022 10:54 AM ET
Vertex Pharmaceuticals Incorporated (VRTX)
By: Jonathan Block, SA News Editor1 Comment
- The US FDA has cleared an IND application from Vertex Pharmaceuticals (NASDAQ:VRTX) for VX-522, an mRNA candidate for cystic fibrosis ("CF").
- https://seekingalpha.com/news/3916164-vertex-receives-ind-clearance-for-mrna-cystic-fibrosis-therapy
- Vertex Pharmaceuticals Incorporated (VRTX)
- https://www.vrtx.com/our-science/pipeline/
AYVAKIT® (avapritinib)
AYVAKIT® (avapritinib)
AYVAKIT® (avapritinib)
Blueprint Medicines Reports Clinical Data Highlighting Leadership in Developing Targeted Treatment Options for Patients with Systemic Mastocytosis
December 11, 2022 at 5:45 PM EST
-- 95 percent confirmed overall response rate and 37 percent confirmed complete remission rate in treatment-naïve patients with SM-AHN, the most common subtype of advanced SM, in PATHFINDER trial of AYVAKIT® (avapritinib) --
-- Ongoing survival benefits, with up to six years of follow-up, in patients with advanced SM from EXPLORER trial of AYVAKIT --
-- Top-line, 12-week Part 1 data from HARBOR trial show elenestinib (BLU-263) improved measures of mast cell burden and patient-reported symptoms in indolent SM --
CAMBRIDGE, Mass., Dec. 11, 2022 /PRNewswire/ -- Blueprint Medicines Corporation (NASDAQ: BPMC) today announced AYVAKIT® (avapritinib) data showing high, durable response rates and prolonged overall survival (OS) in patients with advanced systemic mastocytosis (Advanced SM), including SM with an associated hematological neoplasm (SM-AHN). The findings are being reported in two presentations, including an oral presentation featuring updated follow-up from treatment-naïve patients in the PATHFINDER trial, at the 64th American Society of Hematology (ASH) Annual Meeting and Exposition in New Orleans. AYVAKIT is approved by the U.S. Food and Drug Administration (FDA) for the treatment of adults with Advanced SM.
SM is a rare hematologic disorder driven by the KIT D816V mutation in approximately 95 percent of cases. In advanced SM, the median OS has ranged from less than six months to approximately 3.5 years, depending on the subtype.1 AYVAKIT was designed to potently and selectively inhibit D816V mutant KIT.
"AYVAKIT has demonstrated significant clinical benefits in patients with advanced systemic mastocytosis, including complete remissions and durable responses that have translated into a highly meaningful impact on overall survival," said Deepti Radia, M.D., a hematologist and an investigator on the PATHFINDER and EXPLORER trials. "As a physician specializing in SM and other myeloproliferative neoplasms, I am encouraged that treatment-naïve patients with SM-AHN had a 95 percent response rate and an estimated two-year survival rate of 86 percent in the PATHFINDER trial. Before the introduction of KIT D816V-targeted therapy, physicians often focused on treating the AHN component of SM-AHN. AYVAKIT represents a practice-changing advancement for this patient population, and updated PATHFINDER data highlight the importance of treating the SM for early therapeutic intervention in SM-AHN patients with measurable 'C' findings, excluding those with aggressive AHNs."
"AYVAKIT has become the standard of care treatment for advanced systemic mastocytosis in the U.S., with a growing number of patients receiving the therapy early in the course of their disease. This position is further reinforced by updated AYVAKIT results in the treatment-naïve setting, which include overall response, complete remission and survival rates that establish a new benchmark for patients with advanced SM," said Becker Hewes, M.D., Chief Medical Officer at Blueprint Medicines. "Through our long-term partnership with the SM community, we have amassed datasets reflecting hundreds of patient years of clinical experience across advanced and non-advanced forms of the disease. This breadth of data highlights strong clinical execution and reflects our leadership in developing a portfolio of targeted treatment options designed to address the medical needs of patients with SM."
AYVAKIT – Updated data from the PATHFINDER and EXPLORER trials in advanced SM
Long-term follow-up of 38 treatment-naïve patients from the PATHFINDER trial and 69 patients from the EXPLORER trial – regardless of line of therapy – further validate the clinical efficacy and safety profile of AYVAKIT in advanced SM. Based on modified IWG-MRT-ECNM criteria, the overall response rate (ORR) was defined as complete remission with full or partial recovery of peripheral blood counts (CR/CRh), partial remission or clinical improvement. All responses were confirmed.
In the PATHFINDER trial, AYVAKIT showed broad clinical activity in treatment-naïve patients evaluable for response (n=25), including those with SM-AHN (n=19), as of a data cutoff date of April 20, 2021.
For treatment-naïve patients across advanced SM subtypes:
- ORR was 84 percent and CR/CRh rate was 32 percent.
- Median time to response was two months and median time to CR/CRh was six months.
- Median duration of response (DOR) has not been reached.
- Estimated 24-month OS rate was 88 percent.
For treatment-naïve patients with SM-AHN:
- ORR was 95 percent and CR/CRh rate was 37 percent.
- Estimated 24-month OS rate was 86 percent.
In addition, improvements were observed across hematologic parameters, such as monocytes and eosinophils in the peripheral blood, suggesting multi-lineage involvement of the KIT D816V mutation.
In the EXPLORER trial, 57 patients across lines of therapy were evaluable for response as of a data cutoff date of April 5, 2022. The ORR was 77 percent, with median DOR and OS not reached in patients followed for up for six years.
Safety data from the PATHFINDER and EXPLORER trials were consistent with previously reported results and the FDA approved labeling for AYVAKIT, and reinforce the favorable benefit-risk profile of AYVAKIT at the 200 mg once-daily (QD) recommended dose. The most common treatment-related adverse events (AEs) included periorbital edema, thrombocytopenia, peripheral edema, anemia and nausea. Discontinuations due to treatment-related AEs occurred in four treatment-naïve patients (11 percent) since the initiation of the PATHFINDER trial in 2018, and seven patients across lines of therapy (10 percent) since the initiation of the EXPLORER trial in 2016.
Copies of Blueprint Medicines data presentations from the ASH annual meeting are available in the "Science—Publications and Presentations" section of the company's website at www.BlueprintMedicines.com.
Elenestinib (BLU-263) – Top-line results from Part 1 of HARBOR trial in indolent SM
In addition, Blueprint Medicines today announced top-line, 12-week results from the dose-finding Part 1 of the HARBOR trial of elenestinib, a next-generation KIT D816V inhibitor, reflecting the company's long-term commitment to SM. HARBOR Part 1 was designed to assess concurrent dose cohorts of elenestinib plus best available therapy (elenestinib group) versus placebo plus best available therapy (placebo group) in patients with indolent SM. The trial included 29 patients in the elenestinib group (n=10 at 25 mg QD; n=10 at 50 mg QD; n=9 at 100 mg QD), and 10 patients in the placebo group.
Elenestinib showed evidence of clinical activity and safety consistent with its preclinical profile and a completed Phase 1 healthy volunteer trial. Elenestinib treatment led to rapid improvements in objective measures of mast cell burden, including serum tryptase and KIT D816V allele fraction, and total symptom score (TSS) as measured by the Indolent SM Symptom Assessment Form (ISM-SAF). At 12 weeks, elenestinib demonstrated similar reductions in TSS across dose cohorts. In addition, consistent with previously reported data from the PIONEER trial of AYVAKIT in indolent SM, change in serum tryptase was not correlated with change in TSS. Safety results show that elenestinib was generally well-tolerated, and there were no discontinuations due to AEs. Blueprint Medicines plans to present data from Part 1 of the HARBOR trial at a medical congress in 2023.
About AYVAKIT (avapritinib)
AYVAKIT (avapritinib) is a kinase inhibitor approved by the FDA for the treatment of adults with Advanced SM, including aggressive SM (ASM), SM with an associated hematological neoplasm (SM-AHN) and mast cell leukemia (MCL), and adults with unresectable or metastatic gastrointestinal stromal tumor (GIST) harboring a PDGFRA exon 18 mutation, including PDGFRA D842V mutations. For more information, visit AYVAKIT.com. This medicine is approved in Europe (AYVAKYT®) for the treatment of adults with ASM, SM-AHN or MCL, after at least one systemic therapy, and adults with unresectable or metastatic GIST harboring the PDGFRA D842V mutation. Please click here to see the full U.S. Prescribing Information for AYVAKIT, and click here to see the European Summary of Product Characteristics for AYVAKYT. AYVAKIT/AYVAKYT is not approved for the treatment of any other indication in the U.S. or Europe.
To learn about ongoing or planned clinical trials, contact Blueprint Medicines at medinfo@blueprintmedicines.com or 1-888-BLU-PRNT (1-888-258-7768). Additional information is available at blueprintclinicaltrials.com or clinicaltrials.gov.
Please click here to see the full Prescribing Information for AYVAKIT.
About Blueprint Medicines
Blueprint Medicines is a global precision therapy company that invents life-changing therapies for people with cancer and blood disorders. Applying an approach that is both precise and agile, we create medicines that selectively target genetic drivers, with the goal of staying one step ahead across stages of disease. Since 2011, we have leveraged our research platform, including expertise in molecular targeting and world-class drug design capabilities, to rapidly and reproducibly translate our scientific innovation into a broad pipeline of important approved and investigational precision therapies aimed at addressing difficult-to-treat cancers and blood disorders. Today, we are delivering our approved medicines to patients in the United States, Europe, and in other geographies ourselves or through our partners. In addition, we are globally advancing multiple programs for systemic mastocytosis, lung cancer, breast cancer, and other genomically defined cancers, and cancer immunotherapy. For more information, visit www.BlueprintMedicines.com and follow us on Twitter (@BlueprintMeds) and LinkedIn.
Trademarks
Blueprint Medicines, AYVAKIT, AYVAKYT, GAVRETO and associated logos are trademarks of Blueprint Medicines Corporation.
SOURCE Blueprint Medicines Corporation
Blueprint reports long term data for Ayvakit; elenestinib shows promise in phase 1 trial
Dec. 12, 2022 5:34 AM ET
Blueprint Medicines Corporation (BPMC)
By: Ravikash, SA News Editor
Blueprint Medicines (NASDAQ:BPMC) reported long term updated of Ayvakit from the PATHFINDER and EXPLORER trials in patients with advanced systemic mastocytosis (SM) and part of 1 of the HARBOR study of elenestinib.
Blueprint Medicines Corporation (BPMC)
IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb)
IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb)
IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb)
Innovent Presents Phase Ib Clinical Data Update of IBI110 (Anti-LAG-3 Monoclonal Antibody) at the 2022 European Society For Medical Oncology Immuno-Oncology Congress
Published on: Dec 9th, 2022Back
ROCKVILLE, M.D. and SUZHOU, China, Dec 9, 2022 — Innovent Biologics, Inc. (“Innovent”) (HKEX: 01801), a world-class biopharmaceutical company that develops, manufactures and commercializes high-quality medicines for the treatment of oncology, autoimmune, metabolic, ophthalmology and other major diseases, today announced that updated clinical data of IBI110 (anti-LAG-3 monoclonal antibody) in advanced squamous non-small cell lung cancer (sqNSCLC) is presented at the 2022 European Society for Medical Oncology Immuno-Oncology Congress (ESMO-IO), held Dec 7-9, 2022.
Efficacy and safety of IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb) in Advanced Squamous Non-small Cell Lung Cancer (sqNSCLC): Updated Results from a Phase Ib Study
Poster #: 86P
IBI110 is an IgG4κ recombinant human anti-LAG-3 monoclonal antibody developed by Innovent Biologics. The Phase Ib study aims to evaluate the efficacy and safety of IBI110 in combination with sintilimab and chemotherapy (paclitaxel plus carboplatin) as first-line therapy for advanced sqNSCLC.
• 20 treatment naïve sqNSCLC patients received IBI110 (200 mg, Q3W) combined with sintilimab and chemotherapy and received at least 1 post-baseline tumor assessment. As of the data cutoff date of Oct 25, 2022, median follow-up time was 12.0 (95% CI, 11.9 -13.1) months, 16 patients achieved partial response (PR), the objective response rate (ORR) was 80%; the 12-month progression free survival (PFS) rate was 60.0% (95% CI, 35.7-77.6), the median PFS was not reached; the 12-month overall survival (OS) rate was 85.0% (95% CI, 60.4-94.9) .
• For safety results, the most common treatment related adverse events (TRAEs) ≥ grade 3 were decreased neutrophil count (30.0%) and decreased white blood cell count (20.0%). Immune-related AEs (irAEs) occurred in 14 patients, in which only 4 patients experienced irAE ≥ grade 3. No treatment-related deaths occurred.
• IBI110 combined with sintilimab and chemotherapy in advanced sqNSCLC continues to show robust anti-tumor activity and favorable safety. The study is ongoing with the clinical data in squamous NSCLC continuing to mature and will be disclosed in the future academic conference/journals.
Professor Caicun Zhou, Shanghai Pulmonary Hospital, stated: “Lung cancer is the most commonly diagnosed cancer and the leading cause of cancer death worldwide, of which non-small cell lung cancer accounts for about 80% . In recent years, PD-1/PD-L1 inhibitors have shown promising efficacy in non-small cell lung cancer . However, persistent response to immune checkpoint inhibitor monotherapy remains a challenge in clinical practice. IBI110 plus sintilimab indicate promising antitumor activity and a manageable safety profile in untreated squamous non-small cell lung cancer patients. In the current 20 patients, the ORR reached 80% and the 12-month PFS rate was 60%, which warrants further investigation into the safety and efficacy of IBI110 combination therapy in this indication.”
Dr. Hui Zhou, Senior Vice President of Innovent, stated: “We are pleased to present our clinical development updates at the 2022 ESMO-IO Meeting. IBI110 in combination with sintilimab demonstrated encouraging efficacy and safety data in sqNSCLC. We will continue to provide updates on the PoC data for IBI110 and plan to initiate pivotal clinical studies. As immunotherapy moves into the next era, we are actively advancing the development of next-generation immune checkpoint inhibitors, among which IBI110 represents a high-potential LAG-3 asset, which we hope will benefit patients in need soon.”
To learn more about Innovent’s R&D updates and activities, please visit https://investor.innoventbio.com/cn/investors/webcasts-and-presentations/.
About IBI110
IBI110 is an IgG4κ recombinant human anti-LAG-3 monoclonal antibody independently developed by Innovent Biologics. Based on the mechanism of action and preclinical data of IBI110, it is assumed that IBI110 can inhibit the immune checkpoint signaling to achieve anti-tumor effect, which may further improve the efficacy of immunotherapy, overcome the primary drug resistance, and overcome the drug resistance after anti-PD-1 /PD-L1 monoclonal antibody treatment . Based on the urgent clinical needs, Innovent has carried out clinical studies to explore PK/PD characteristics of IBI110 single agent and combined with sintilimab in humans as well as its efficacy and safety in various advanced tumors. This clinical trial (NCT04085185) is the first in human clinical study of IBI110.
About Innovent
Inspired by the spirit of "Start with Integrity, Succeed through Action," Innovent's mission is to develop, manufacture and commercialize high-quality biopharmaceutical products that are affordable to ordinary people. Established in 2011, Innovent is committed to developing, manufacturing and commercializing high-quality innovative medicines for the treatment of cancer, autoimmune disease, metabolic disorder and other major diseases. On October 31, 2018, Innovent was listed on the Main Board of the Stock Exchange of Hong Kong Limited with the stock code: 01801.HK.
Since its inception, Innovent has developed a fully integrated multi-functional platform which includes R&D, CMC (Chemistry, Manufacturing, and Controls), clinical development and commercialization capabilities. Leveraging the platform, the company has built a robust pipeline of 35 valuable assets in the fields of cancer, metabolic disorder, autoimmune disease and other major therapeutic areas, with 8 approved products on the market. These include: TYVYT® (sintilimab injection), BYVASDA®(bevacizumab biosimilar injection), SULINNO® (adalimumab biosimilar injection), HALPRYZA®(rituximab biosimilar injection), Pemazyre®(pemigatinib oral inhibitor), olverembatinib (BCR ABL TKI), Cyramza® (ramucirumab) and selpercatinib. An additional 2 assets are under NMPA NDA review, 5 assets are in Phase 3 or pivotal clinical trials, and 20 more molecules are in clinical studies.
Innovent has built an international team with advanced talent in high-end biological drug development and commercialization, including many global experts. The company has also entered into strategic collaborations with Eli Lilly and Company, Sanofi, Adimab, Incyte, MD Anderson Cancer Center and other international partners. Innovent strives to work with many collaborators to help advance China's biopharmaceutical industry, improve drug availability and enhance the quality of the patients' lives. For more information, please visit: www.innoventbio.com. and www.linkedin.com/company/innovent-biologics/.
Note:
TYVYT® (sintilimab injection) is not an approved product in the United States.
BYVASDA® (bevacizumab biosimilar injection), SULINNO®, and HALPRYZA® (rituximab biosimilar injection) are not approved products in the United States.
TYVYT® (sintilimab injection, Innovent)
BYVASDA® (bevacizumab biosimilar injection, Innovent)
HALPRYZA® (rituximab biosimilar injection, Innovent)
SULINNO® (adalimumab biosimilar injection, Innovent)
Pemazyre® (pemigatinib oral inhibitor, Incyte Corporation). Pemazyre® was discovered by Incyte Corporation and licensed to Innovent for development and commercialization in Mainland China, Hong Kong, Macau and Taiwan.
CYRAMZA® (ramucirumab, Eli Lilly). CYRAMZA® was discovered by Eli Lilly and licensed to Innovent for commercialization in Mainland China.
Selpercatinib (Eli Lilly). Selpercatinib was discovered by Eli Lilly and licensed to Innovent for commercialization in Mainland China.
Disclaimer:
1. The indications are still under clinical study, which haven’t been approved in China.
2. Innovent does not recommend any off-label usage.
Innovent's drug shows promise in advanced lung cancer patients in early-stage trial
Dec. 09, 2022 5:27 AM ET
Innovent Biologics, Inc. (IVBIY), LLY, IVBXF
By: Ravikash, SA News Editor
Innovent Biologics (OTCPK:IVBIY) (OTCPK:IVBXF) reported data from a phase 1b trial of IBI939 in combination with the company and Eli Lilly's (NYSE:LLY) Tyvyt (sintilimab) in patients with previously untreated, locally advanced unresectable or metastatic PD-L1 TPS≥50% non-small cell lung cancer (NSCLC) without sensitizing mutations.
Innovent Biologics, Inc. (IVBIY), LLY, IVBXF
https://www.innoventbio.com/Collaborations/Partners
Datopotamab deruxtecan (Dato-DXd)
IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb)
IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb)
Datopotamab deruxtecan showed encouraging and durable efficacy in patients with heavily pretreated HR-positive, HER2-low or negative metastatic breast cancer
PUBLISHED8 December 2022
8 December 2022 23:00 GMT
First results for AstraZeneca and Daiichi Sankyo’s TROP2-directed ADC in this setting reported from TROPION-PanTumor01 Phase I trial
Pivotal TROPION-Breast01 Phase III trial is ongoing, evaluating datopotamab deruxtecan in these patients in earlier lines of treatment
Initial results from the TROPION-PanTumor01 Phase I trial of datopotamab deruxtecan (Dato-DXd) showed encouraging and durable efficacy in patients with heavily pretreated hormone receptor (HR)-positive, HER2-low (immunohistochemistry [IHC] 1+ or IHC 2+/in-situ hybridisation [ISH] negative) or HER2-negative (IHC 0) unresectable or metastatic breast cancer. Safety results were consistent with previous trials of datopotamab deruxtecan. Results were presented today at the 2022 San Antonio Breast Cancer Symposium (abstract #PD13-08).
Datopotamab deruxtecan is a specifically engineered TROP2-directed DXd antibody drug conjugate (ADC) being jointly developed by Daiichi Sankyo and AstraZeneca.
In this cohort of TROPION-PanTumor01 (n=41), datopotamab deruxtecan demonstrated an objective response rate (ORR) of 27% as assessed by blinded independent central review (BICR). All responses were partial (n=11) and 56% of patients achieved stable disease (n=23). The disease control rate (DCR) was 85% and median progression-free survival (PFS) was 8.3 months (95% confidence interval [CI], 5.5-11.1). With median follow-up of 13.7 months, the median duration of response (DoR) and the median overall survival (OS) had not been reached with 59% of patients alive for more than one year.
Approximately 70% of breast cancer tumours are considered HR-positive and HER2-low or negative.1 For patients with HR-positive, HER2-low or negative metastatic breast cancer that progress on or are not suitable candidates for endocrine therapy, the current standard of care is single-agent chemotherapy.2
Funda Meric-Bernstam, Chair, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, and investigator in the TROPION-PanTumor01 trial, said: “Patients with HR-positive, HER2-low or negative metastatic breast cancer who are not eligible for endocrine therapy or have exhausted treatment options have a poor prognosis. These preliminary results with datopotamab deruxtecan in patients with heavily pretreated HR-positive, HER2-low or negative metastatic breast cancer are encouraging and warrant further evaluation in this setting.”
Cristian Massacesi, Chief Medical Officer and Oncology Chief Development Officer, AstraZeneca, said: “Many of these patients with metastatic breast cancer in TROPION-PanTumor01 had exhausted most of their available treatment options, having received a striking median of five prior regimens including a CDK4/6 inhibitor for nearly all patients. These promising results with datopotamab deruxtecan in such a heavily pretreated patient population support our strong belief that this TROP2-directed antibody drug conjugate has the potential to improve outcomes for patients with HR-positive, HER2-low or negative breast cancer in this, and possibly earlier settings.”
Mark Rutstein, Global Head, Oncology Clinical Development, Daiichi Sankyo, said: “These results add to the growing body of data demonstrating the potential of datopotamab deruxtecan to treat certain types of metastatic breast cancer. We look forward to the continued evaluation of our TROP2-directed antibody drug conjugate, including comparisons to standard therapy in earlier lines of treatment for HR-positive, HER2-low or negative metastatic breast cancer through our ongoing TROPION-Breast01 Phase III trial.”
Patients in the TROPION-PanTumor01 trial were heavily pretreated, receiving a median of five lines of prior regimens in the metastatic setting (range 3-10). Prior treatments included CDK4/6 inhibitors (95%), capecitabine (83%), taxanes (59%), anthracyclines (54%), neoadjuvant chemotherapy (37%), mTOR inhibitors (29%) and PI3KCA inhibitors (20%). As of data cut-off on 22 July 2022, five patients remained on study treatment.
The safety profile of datopotamab deruxtecan was consistent with previous data with no new safety signals identified. The most common Grade 3 or higher treatment-emergent adverse events (TEAEs) were decreased lymphocyte count (15%), stomatitis (10%), anaemia (7%), dyspnoea (2%) and fatigue (2%). Serious TEAEs were observed in six patients (15%), including one death due to dyspnoea that was not considered treatment-related. Treatment discontinuations due to an adverse event occurred in five patients (12%). No cases of Grade 3 or higher diarrhoea or febrile neutropenia were observed. One case of Grade 3 interstitial lung disease was adjudicated as treatment-related.
AstraZeneca and Daiichi Sankyo have a broad clinical development programme for datopotamab deruxtecan in breast cancer, including the ongoing pivotal TROPION-Breast01 Phase III trial evaluating datopotamab deruxtecan in patients with HR-positive, HER2-low or negative, inoperable or metastatic breast cancer previously treated with chemotherapy.
Notes
HR-positive breast cancer
Breast cancer is the most common cancer and one of the leading causes of cancer-related deaths worldwide.3 More than two million breast cancer cases were diagnosed in 2020, with nearly 685,000 deaths globally.3
HR-positive breast cancer (expressing estrogen or progesterone receptors, or both) is the most common subtype of breast cancer with approximately 70% of breast cancer tumours considered HR-positive and HER2-low or negative.1
The growth of HR-positive breast cancer cells is often driven by estrogen receptors (ER), and endocrine therapies that target ER-driven disease are widely used as 1st-line treatment in the advanced setting, and often paired with cyclin-dependent kinase (CDK) 4/6 inhibitors.4-6 However, resistance to CDK4/6 inhibitors and current endocrine therapies develops in many patients with advanced disease.6 Once this occurs, the treatment options are limited – with chemotherapy being the current standard of care – and survival rates are low with 30% of patients anticipated to live beyond five years after diagnosis.1,2,6
Optimising endocrine therapy and overcoming resistance for patients with ER-driven disease at all stages of treatment as well as identifying new therapies for those who no longer have ER-driven disease are active areas of focus for breast cancer research.
TROP2 (trophoblast cell-surface antigen 2) is a transmembrane glycoprotein that is broadly expressed in several types of solid tumours, including HR-positive, HER2-low or negative breast cancer.7-8 TROP2 expression is an unfavourable prognostic factor for overall survival in all types of breast cancer.7
TROPION-PanTumor01
TROPION-PanTumor01 is a first-in-human, open-label, two-part, multicentre Phase I trial evaluating the safety and preliminary efficacy of datopotamab deruxtecan in patients with advanced solid tumours that have relapsed or are refractory to standard treatment or for which no standard treatment is available. The dose escalation portion of the trial enrolled patients with non-small cell lung cancer (NSCLC) to assess the safety and efficacy of datopotamab deruxtecan to determine the recommended dose for expansion (6mg/kg). The dose expansion part of TROPION-PanTumor01 is enrolling several different cohorts including patients with NSCLC, triple-negative breast cancer (TNBC), HR-positive, HER2-low or negative breast cancer, small cell lung cancer, urothelial, gastric, pancreatic, castration-resistant prostrate and esophageal cancer.
Safety endpoints include dose-limiting toxicities and serious adverse events. Efficacy endpoints include ORR, DoR, time to response, PFS and OS. Pharmacokinetic, biomarker and immunogenicity endpoints also are being evaluated.
Datopotamab deruxtecan (Dato-DXd)
Datopotamab deruxtecan (Dato-DXd) is an investigational TROP2-directed ADC. Designed using Daiichi Sankyo’s proprietary DXd ADC technology, datopotamab deruxtecan is one of three leading ADCs in the oncology pipeline of Daiichi Sankyo, and one of the most advanced programmes in AstraZeneca’s ADC scientific platform. Datopotamab deruxtecan is comprised of a humanized anti-TROP2 IgG1 monoclonal antibody, developed in collaboration with Sapporo Medical University, attached to a number of topoisomerase I inhibitor payloads, an exatecan derivative, via tetrapeptide-based cleavable linkers.
A comprehensive development programme called TROPION is underway globally with more than 10 trials evaluating the efficacy and safety of datopotamab deruxtecan across multiple TROP2-targetable tumours, including TNBC, HR-positive, HER2-low or negative breast cancer and NSCLC. Trials in combination with other anticancer treatments, such as immunotherapy, are also underway.
AstraZeneca and Daiichi Sankyo collaboration
AstraZeneca and Daiichi Sankyo entered into a global collaboration to jointly develop and commercialise datopotamab deruxtecan in July 2020, except in Japan where Daiichi Sankyo maintains exclusive rights. Daiichi Sankyo is responsible for the manufacturing and supply of datopotamab deruxtecan.
AstraZeneca in breast cancer
Driven by a growing understanding of breast cancer biology, AstraZeneca is starting to challenge, and redefine, the current clinical paradigm for how breast cancer is classified and treated to deliver even more effective treatments to patients in need – with the bold ambition to one day eliminate breast cancer as a cause of death.
AstraZeneca has a comprehensive portfolio of approved and promising compounds in development that leverage different mechanisms of action to address the biologically diverse breast cancer tumour environment.
With Enhertu (trastuzumab deruxtecan), a HER2-directed ADC, AstraZeneca and Daiichi Sankyo are aiming to improve outcomes in previously treated HER2-positive and HER2-low metastatic breast cancer and are exploring its potential in earlier lines of treatment and in new breast cancer settings.
In HR-positive breast cancer, AstraZeneca continues to improve outcomes with foundational medicines Faslodex (fulvestrant) and Zoladex (goserelin) and aims to reshape the HR-positive space with next-generation oral selective estrogen receptor degrader (ngSERD) and potential new medicine camizestrant as well as a potential first-in-class AKT kinase inhibitor, capivasertib. AstraZeneca is also collaborating with Daiichi Sankyo to explore the potential of TROP2-directed ADC, datopotamab deruxtecan, in this setting.
PARP inhibitor Lynparza (olaparib) is a targeted treatment option that has been studied in early and metastatic breast cancer with an inherited BRCA mutation. AstraZeneca with MSD (Merck & Co., Inc. in the US and Canada) continue to research Lynparza in these settings and to explore its potential in earlier disease.
To bring much-needed treatment options to patients with TNBC, an aggressive form of breast cancer, AstraZeneca is evaluating the potential of datopotamab deruxtecan alone and in combination with immunotherapy Imfinzi (durvalumab), capivasertib in combination with chemotherapy, and Imfinzi in combination with other oncology medicines, including Lynparza and Enhertu.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the ambition to provide cures for cancer in every form, following the science to understand cancer and all its complexities to discover, develop and deliver life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers. It is through persistent innovation that AstraZeneca has built one of the most diverse portfolios and pipelines in the industry, with the potential to catalyse changes in the practice of medicine and transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day, eliminate cancer as a cause of death.
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca, Daiichi Sankyo's drug shows promise in heavily pretreated breast cancer patients in trial
Dec. 09, 2022 4:52 AM ET
AstraZeneca PLC (AZN), DSKYF, DSNKY
By: Ravikash, SA News Editor
AstraZeneca (NASDAQ:AZN) and Daiichi Sankyo (OTCPK:DSKYF) (OTCPK:DSNKY) said on Thursday that their medicine datopotamab deruxtecan (Dato-DXd) showed durable efficacy in patients with a type of breast cancer in an early stage study.
AstraZeneca PLC (AZN), DSKYF, DSNKY
December 09, 2022
R&D
Capivasertib Plus FASLODEX® (fulvestrant)
IBI110 (anti-LAG-3 mAb) in combination with Sintilimab (anti-PD-1 mAb)
Capivasertib Plus FASLODEX® (fulvestrant)
Capivasertib plus Faslodex reduced the risk of disease progression or death by 40% versus Faslodex in advanced HR-positive breast cancer
PUBLISHED 8 December 2022
8 December 2022 13:30 GMT
CAPItello-291 Phase III trial results presented at SABCS 2022
show potential of capivasertib as first-in-class AKT inhibitor
Detailed results from the CAPItello-291 Phase III trial showed AstraZeneca’s capivasertib in combination with Faslodex (fulvestrant) demonstrated a statistically significant and clinically meaningful improvement in progression-free survival (PFS) versus placebo plus Faslodex in patients with hormone receptor (HR)-positive, HER2-low or negative, locally advanced or metastatic breast cancer, following recurrence or progression on, or after, endocrine therapy (with or without a CDK4/6 inhibitor).1 Results will be presented today in an oral presentation at the 2022 San Antonio Breast Cancer Symposium (SABCS).
Results showed capivasertib in combination with Faslodex demonstrated a 40% reduction in the risk of disease progression or death versus placebo plus Faslodex in the overall trial population (based on a hazard ratio [HR] of 0.60, 95% confidence interval [CI] 0.51-0.71; p=<0.001; median 7.2 versus 3.6 months).1 In the AKT pathway biomarker-altered population, capivasertib plus Faslodex reduced the risk of disease progression or death by 50% versus placebo plus Faslodex (HR of 0.50, 95% CI 0.38-0.65; p=<0.001; median 7.3 versus 3.1 months).1 Alterations within the AKT pathway (PI3K/AKT/PTEN) occur frequently in breast cancer, affecting up to 50% of patients with advanced HR-positive breast cancer.2-4
Nicholas Turner, MD, PhD, Professor of Molecular Oncology at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, London, UK, and principal investigator in the CAPItello-291 Phase III trial, said: “These data demonstrate the practice-changing potential of capivasertib as a new treatment option for patients with advanced HR-positive breast cancer. Critically, this potentially first-in-class treatment has shown it delays disease progression for those who have progressed on, or become resistant to, endocrine therapies and CDK4/6 inhibitors.”
Susan Galbraith, Executive Vice President, Oncology R&D, AstraZeneca, said: “Capivasertib brings important progress to an area with persistent treatment gaps as the first therapy of its kind shown to be effective in a Phase III trial in patients with advanced HR-positive, HER2-low or negative breast cancer. We believe these results which showed benefit in all-comers and biomarker positive populations can reshape HR-positive breast cancer treatment, and that capivasertib can become an important new option for patients.”
Summary of results: CAPItello-2911
Capivasertib plus Faslodex
n=355
Placebo plus Faslodex
n=353
Median PFS in overall population (months)
7.2
3.6
HR (95% CI)
0.60 (0.51-0.71)
p-value
p=<0.001
Median PFS in the biomarker-altered population (months)
7.3
3.1
HR (95% CI)
0.50 (0.38-0.65)
p-value
p=<0.001
ORR in overall population
22.9%
12.2%
ORR in biomarker-altered population
28.8%
9.7%
HR, hazard ratio; CI, confidence interval; PFS, progression-free survival; ORR, objective response rate
Confirmed objective response rate (ORR) was 22.9% for the capivasertib plus Faslodex arm versus 12.2% for the placebo plus Faslodex arm in the overall trial population, and 28.8% versus 9.7%, respectively, in the biomarker-altered population.1 Although the overall survival (OS) data were immature at the time of the analysis, early data are encouraging.1 The trial will continue to assess OS as a key secondary endpoint.
The safety profile of capivasertib plus Faslodex was similar to that observed in previous trials evaluating this combination.1 In the overall trial population, the most frequent any grade adverse events (AEs) with capivasertib plus Faslodex occurring in 20% or more of patients were diarrhoea (72.4%), nausea (34.6%), rash (group term including rash, rash macular, maculo-papular rash, rash papular and rash pruritic; 38%) fatigue (20.8%) and vomiting (20.6%).1 The most frequent Grade 3 or higher AEs occurring in 5% or more of patients were diarrhoea (9.3%) and rash (12.1%).1
Notes
HR-positive breast cancer
Breast cancer is the most common cancer and is one of the leading causes of cancer-related deaths worldwide.5 More than two million patients were diagnosed with breast cancer in 2020, with nearly 685,000 deaths globally.5
HR-positive breast cancer (expressing estrogen or progesterone receptors, or both), is the most common subtype of breast cancer with approximately 70% of breast cancer tumours considered HR-positive and HER2-low or negative.6
The growth of HR-positive breast cancer cells is often driven by estrogen receptors (ER),7 and endocrine therapies that target ER-driven disease are widely used as 1st-line treatment in the advanced setting, and often paired with cyclin-dependent kinase (CDK) 4/6 inhibitors.8,9 However, resistance to CDK4/6 inhibitors and current endocrine therapies develops in many patients with advanced disease.9 Once this occurs, treatment options are limited9 – with chemotherapy being the current standard of care10 – and survival rates are low with 30% of patients anticipated to live beyond five years after diagnosis.6
Optimising endocrine therapy and overcoming resistance for patients with ER-driven disease at all stages of treatment as well as identifying new therapies for those who no longer have ER-driven disease are active areas of focus for breast cancer research.
CAPItello-291
CAPItello-291 is a Phase III, double-blind, randomised trial that is part of a larger clinical programme focused on capivasertib, an investigational AKT (serine/threonine kinase) inhibitor. CAPItello-291 is evaluating the efficacy of capivasertib in combination with Faslodex versus placebo plus Faslodex for the treatment of locally advanced (inoperable) or metastatic HR-positive, HER2-low or negative breast cancer.
The global trial enrolled 708 adult patients with histologically confirmed HR-positive, HER2-low or negative breast cancer whose disease has recurred or progressed during or after aromatase inhibitor therapy, with or without a CDK4/6 inhibitor, and up to one line of chemotherapy for advanced disease. The trial has dual primary endpoints of PFS in the overall patient population and in a population of patients whose tumours have qualifying alterations in the AKT pathway (PIK3CA, AKT1 or PTEN genes). In the trial, approximately 40% of tumours had these alterations.
Capivasertib
Capivasertib is an investigational oral treatment currently in Phase III trials for the treatment of multiple subtypes of breast cancer, prostate cancer and a Phase II trial for haematologic malignancies. A potent, selective adenosine triphosphate (ATP)-competitive inhibitor of all three AKT isoforms (AKT1/2/3), capivasertib is being evaluated as a monotherapy and in combination with existing therapies in tumours harbouring alterations in the AKT pathway (PI3K/AKT/PTEN), and in tumours reliant on signalling via this pathway for survival. Capivasertib 400 mg is administered twice daily according to an intermittent dosing schedule of four days on and three days off. This was chosen in early phase trials based on tolerability and the degree of target inhibition.
The capivasertib clinical research programme is investigating the safety and efficacy of capivasertib when used alone and in combination with established treatment regimens.
Capivasertib was discovered by AstraZeneca subsequent to a collaboration with Astex Therapeutics (and its collaboration with the Institute of Cancer Research and Cancer Research Technology Limited).
AstraZeneca in breast cancer
Driven by a growing understanding of breast cancer biology, AstraZeneca is starting to challenge, and redefine, the current clinical paradigm for how breast cancer is classified and treated to deliver even more effective treatments to patients in need – with the bold ambition to one day eliminate breast cancer as a cause of death.
AstraZeneca has a comprehensive portfolio of approved and promising compounds in development that leverage different mechanisms of action to address the biologically diverse breast cancer tumour environment.
With Enhertu (trastuzumab deruxtecan), a HER2-directed ADC, AstraZeneca and Daiichi Sankyo are aiming to improve outcomes in previously treated HER2-positive and HER2-low metastatic breast cancer and are exploring its potential in earlier lines of treatment and in new breast cancer settings.
In HR-positive breast cancer, AstraZeneca continues to improve outcomes with foundational medicines Faslodex (fulvestrant) and Zoladex (goserelin) and aims to reshape the HR-positive space with next-generation SERD and potential new medicine camizestrant as well as a potential first-in-class AKT kinase inhibitor, capivasertib. AstraZeneca is also collaborating with Daiichi Sankyo to explore the potential of TROP2-directed ADC, datopotamab deruxtecan, in this setting.
PARP inhibitor Lynparza (olaparib) is a targeted treatment option that has been studied in early and metastatic breast cancer with an inherited BRCA mutation. AstraZeneca with MSD (Merck & Co., Inc. in the US and Canada) continue to research Lynparza in these settings and to explore its potential in earlier disease.
To bring much-needed treatment options to patients with triple-negative breast cancer, an aggressive form of breast cancer, AstraZeneca is evaluating the potential of datopotamab deruxtecan alone and in combination with immunotherapy Imfinzi (durvalumab), capivasertib in combination with chemotherapy, and Imfinzi in combination with other oncology medicines, including Lynparza and Enhertu.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the ambition to provide cures for cancer in every form, following the science to understand cancer and all its complexities to discover, develop and deliver life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers. It is through persistent innovation that AstraZeneca has built one of the most diverse portfolios and pipelines in the industry, with the potential to catalyse changes in the practice of medicine and transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day, eliminate cancer as a cause of death.
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca says adding to capivasertib to Faslodex reduces breast cancer progression
Dec. 08, 2022 3:18 PM ET
By: Jonathan Block, SA News Editor
- Adding AstraZeneca's (NASDAQ:AZN) experimental cancer drug capivasertib to Faslodex (fulvestrant) led to a 40% reduction in the risk of disease progression or death compared to Faslodex alone.
- https://seekingalpha.com/news/3915462-astrazeneca-says-adding-to-capivasertib-to-faslodex-reduces-breast-cancer-progression
- AstraZeneca PLC (AZN)
Iptacopan
Darovasertib Combination Therapy with Crizotinib
Capivasertib Plus FASLODEX® (fulvestrant)
Novartis investigational iptacopan provides clinically meaningful increases in hemoglobin levels in complement-inhibitor-naïve patients with PNH
Dec 08, 2022
- Phase III APPOINT-PNH study of investigational oral monotherapy iptacopan met its primary endpoint; second positive Phase III topline readout for iptacopan in paroxysmal nocturnal hemoglobinuria (PNH)1
- Topline APPOINT-PNH data were consistent with APPLY-PNH readout and showed a significant proportion of complement-inhibitor-naïve patients treated with iptacopan achieved clinically meaningful increases in hemoglobin levels vs. baseline without the need for blood transfusions1
- PNH has a significant unmet need not addressed by anti-C5 therapies; despite treatment with anti-C5s, a large proportion of people with PNH remain anemic, fatigued and dependent on blood transfusions2-5
- APPOINT-PNH data to be presented at upcoming medical meeting and included in iptacopan PNH global regulatory 2023 submissions
Basel, December 8, 2022 —
Novartis today announced the Phase III APPOINT-PNH study (NCT04820530) of investigational oral monotherapy iptacopan in complement-inhibitor-naïve (including anti-C5 therapies) adults with PNH met its primary endpoint1. Topline results showed a significant proportion of patients treated with iptacopan (200 mg twice daily) achieved clinically meaningful hemoglobin-level increases of 2 g/dL or more from baseline without the need for blood transfusions at 24 weeks1.
In the study, the safety profile of iptacopan monotherapy was consistent with previously reported data1,6,7. Detailed data will be presented at an upcoming medical meeting and included as part of global regulatory submissions in 2023.
“We are very encouraged by the results of the complement-inhibitor-naïve data from the Phase III APPOINT-PNH trial,” said David Soergel, M.D., Global Head, Cardiovascular, Renal and Metabolism Development Unit, Novartis. “This second iptacopan readout for PNH underscores the robust potential for this therapy, enabling us to submit a broad regulatory package with the goal of iptacopan potentially becoming the first oral monotherapy for PNH.”
Topline results for the pivotal Phase III APPLY-PNH study were recently announced8. It met its two primary endpoints, with iptacopan demonstrating superiority over anti-C5 therapies (eculizumab or ravulizumab) in adults with PNH experiencing residual anemia despite prior anti-C5 treatment8. The study showed a statistically significant and clinically meaningful increase in the proportion of iptacopan-treated patients achieving 2 g/dL or more hemoglobin-level increases from baseline, and 12 g/dL or more hemoglobin levels, both without the need for blood transfusions at 24 weeks, compared to anti-C5 therapies8.
Novartis is grateful to the patients and clinical investigators whose time, trust and commitment made this PNH research possible, and is excited to continue to explore the potential of iptacopan as the first oral monotherapy option for patients with PNH.
Iptacopan is also being investigated in Phase III studies for the complement-mediated kidney diseases (CMKDs) C3 glomerulopathy (APPEAR-C3G [NCT04817618]), IgA nephropathy (APPLAUSE-IgAN [NCT04578834]), and atypical hemolytic uremic syndrome (APPELHUS [NCT04889430]), as well as in a number of additional indications in Phase II9-11.
Following presentation of the Phase III APPLY-PNH iptacopan data at ASH, Novartis will host an investor conference call on December 13, 2022 at 18:30 CET / 12:30 ET. A simultaneous webcast may be accessed by visiting the Novartis website at https://www.novartis.com/investors/event-calendar, and a replay will be available after the call.
About the study
APPOINT-PNH (NCT04820530) is a Phase III, multinational, multicenter, open-label, single-arm study to evaluate the efficacy and safety of twice-daily, oral iptacopan monotherapy (200 mg) in adult PNH patients who are naïve to complement inhibitor therapy, including anti-C5 therapies (e.g., eculizumab or ravulizumab)12.
The primary endpoint was to assess the proportion of participants achieving an increase in hemoglobin levels from baseline of 2 g/dL or more in the absence of red blood cell (RBC) transfusions at 24 weeks12. Secondary endpoints include the proportion of participants achieving sustained hemoglobin levels of 12 g/dL or more in the absence of RBC transfusions, transfusion avoidance defined as the proportion of participants who remain free from transfusions, average change in hemoglobin levels, average percent change in lactate dehydrogenase (LDH) levels, rate of breakthrough hemolysis, average change in absolute reticulocyte counts, change in fatigue, and rates of major adverse vascular events12.
About paroxysmal nocturnal hemoglobinuria (PNH)
PNH is a rare, chronic and serious complement-mediated blood disorder2. People with PNH have an acquired mutation in some of their hematopoietic stem cells (which are located in the bone marrow and can grow and develop into RBCs, white blood cells and platelets) that causes them to produce RBCs that are susceptible to premature destruction by the complement system2,3. This leads to intravascular hemolysis (destruction of RBCs within blood vessels) and extravascular hemolysis (destruction of RBCs mostly in the spleen and liver), which cause anemia (low levels of circulating RBCs), thrombosis (formation of blood clots), fatigue and other debilitating symptoms that can impact people’s quality of life2,3.
It is estimated that approx. 10-20 people per million worldwide live with PNH2. Although PNH can develop at any age, it is often diagnosed in people between 30-40 years old13,14.
PNH has a significant unmet need not addressed by anti-C5 therapies (eculizumab or ravulizumab): despite treatment with anti-C5s, a large proportion of people with PNH remain anemic, fatigued and dependent on blood transfusions2-5.
About iptacopan
Iptacopan is an investigational first-in-class, orally administered targeted factor B inhibitor of the alternative complement pathway6,7,15. It acts upstream of the C5 terminal pathway, preventing not only intravascular but also extravascular hemolysis in PNH6,7,15. In doing so, iptacopan targets a key part of the biology responsible for PNH while offering an oral monotherapy option6,7,15.
Discovered at the Novartis Institutes for BioMedical Research, iptacopan is currently in development for a number of other complement-mediated diseases (CMDs) where significant unmet needs exist, including kidney diseases C3G, IgAN, atypical hemolytic uremic syndrome (aHUS), membranous nephropathy (MN), lupus nephritis (LN), and blood disorders immune thrombocytopenic purpura (ITP) and cold agglutinin disease (CAD).
Based on disease prevalence, unmet need and data from Phase II studies, iptacopan has received FDA Breakthrough Therapy Designation in PNH, orphan drug designations from the FDA and EMA in PNH and C3G, EMA PRIME designation for C3G, and EMA orphan drug designation in IgAN16-19.
About Novartis
Novartis is reimagining medicine to improve and extend people’s lives. We deliver high-value medicines that alleviate society’s greatest disease burdens through technology leadership in R&D and novel access approaches. In our quest to find new medicines, we consistently rank among the world’s top companies investing in research and development. About 108,000 people of more than 140 nationalities work together to bring Novartis products to nearly 800 million people around the world. Find out more at https://www.novartis.com
Novartis is on Twitter. Sign up to follow @Novartis at https://twitter.com/novartisnews
For Novartis multimedia content, please visit https://www.novartis.com/news/media-library
For questions about the site or required registration, please contact media.relations@novartis.com
Novartis iptacopan comes out successful in 2nd phase 3 trial rare blood disorder
Dec. 08, 2022 5:05 AM ET
By: Ravikash, SA News Editor
Novartis (NYSE:NVS) said its oral drug iptacopan met the main goal of a phase 3 trial in certain patients with paroxysmal nocturnal hemoglobinuria (PNH) in a phase 3 trial.
https://www.novartis.com/clinicaltrials
Zuranolone (SAGE-217/BIIB125)
Darovasertib Combination Therapy with Crizotinib
Darovasertib Combination Therapy with Crizotinib
December 6, 2022
Sage Therapeutics and Biogen Complete Rolling Submission of New Drug Application for Zuranolone in the Treatment of Major Depressive Disorder and Postpartum Depression
Zuranolone is being evaluated as a short course, rapid-acting, oral medication for major depressive disorder (MDD) and postpartum depression (PPD)
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Dec. 6, 2022-- Sage Therapeutics, Inc. (Nasdaq: SAGE) and Biogen Inc. (Nasdaq: BIIB) announced the completion of the rolling submission of a New Drug Application (NDA) to the U.S. Food and Drug Administration (FDA) for zuranolone in the treatment of major depressive disorder (MDD) and postpartum depression (PPD). Zuranolone is an investigational drug being evaluated as a rapid-acting, once-daily, 14-day oral short course treatment in adults with MDD and PPD. The submission completes the NDA filing that was initiated earlier this year.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20221205005815/en/
In the clinical development program to date, zuranolone showed rapid and sustained improvement of depressive symptoms with a generally well-tolerated and consistent safety profile. Zuranolone, a neuroactive steroid, has a novel mechanism of action as a positive allosteric modulator of GABA-A receptors. In people with depression, it may help to rapidly rebalance dysregulated neuronal networks to help restore brain function. Zuranolone targets brain networks responsible for functions such as mood, arousal, behavior, and cognition.
“Based on the data in the LANDSCAPE and NEST programs, we believe that zuranolone has the potential to be a meaningful new therapy for depression,” said Priya Singhal, M.D., M.P.H., Head of Global Safety and Regulatory Sciences and Interim Head of R&D at Biogen. “We look forward to working with the FDA as this filing progresses.”
“Mental health is a highly underserved area with an urgent unmet need for innovative therapies. We need to rethink how MDD and PPD are treated. Existing treatments often take weeks to months to provide symptom relief, and patients may need to cycle through multiple treatment options to fully address their symptoms. People with MDD and PPD deserve better,” said Laura Gault, M.D., Ph.D., Chief Medical Officer at Sage. “We believe that zuranolone, if approved, could evolve the way depression is treated and this submission brings us one step closer to that goal.”
The NDA submission includes data from the LANDSCAPE and NEST development programs for zuranolone. The LANDSCAPE program includes five studies of zuranolone in adults with MDD (MDD-201B, MOUNTAIN, SHORELINE, WATERFALL, and CORAL Studies). The NEST program includes two studies of zuranolone in adult women with PPD (ROBIN and SKYLARK Studies).
Zuranolone was granted Fast Track Designation by the FDA in 2017 and Breakthrough Therapy in 2018 for MDD. The FDA also granted Fast Track Designation for PPD in 2022.
About zuranolone
Zuranolone (SAGE-217/BIIB125) is a once-daily, 14-day, investigational drug in development for the treatment of major depressive disorder (MDD) and postpartum depression (PPD). Zuranolone is an oral neuroactive steroid (NAS) GABA-A receptor positive allosteric modulator (PAM). The GABA system is the major inhibitory signaling pathway of the brain and central nervous system and contributes to regulating brain function. Zuranolone has been granted Fast Track and Breakthrough Therapy Designation for MDD and Fast Track Designation for PPD by the U.S. Food & Drug Administration.
Zuranolone is being evaluated in the LANDSCAPE and NEST clinical development programs. The two development programs include multiple studies examining use of zuranolone in several thousand people with a variety of dosing, clinical endpoints, and treatment paradigms. The LANDSCAPE program includes five studies of zuranolone in people with MDD (MDD-201B, MOUNTAIN, SHORELINE, WATERFALL, and CORAL Studies). The NEST program includes two placebo-controlled studies of zuranolone in women with PPD (ROBIN and SKYLARK Studies). Additionally, Shionogi completed a Phase 2 study of zuranolone in Japan in people with MDD.
About Sage Therapeutics
Sage Therapeutics is a biopharmaceutical company fearlessly leading the way to create a world with better brain health. Our mission is to pioneer solutions to deliver life-changing brain health medicines, so every person can thrive. For more information, please visit www.sagerx.com.
About Biogen
As pioneers in neuroscience, Biogen discovers, develops, and delivers worldwide innovative therapies for people living with serious neurological diseases as well as related therapeutic adjacencies. One of the world’s first global biotechnology companies, Biogen was founded in 1978 by Charles Weissmann, Heinz Schaller, Sir Kenneth Murray, and Nobel Prize winners Walter Gilbert and Phillip Sharp. Today, Biogen has a leading portfolio of medicines to treat multiple sclerosis, has introduced the first approved treatment for spinal muscular atrophy, and developed the first and only approved treatment to address a defining pathology of Alzheimer’s disease. Biogen is also commercializing biosimilars and focusing on advancing one of the industry’s most diversified pipelines in neuroscience that will transform the standard of care for patients in several areas of high unmet need.
We routinely post information that may be important to investors on our website at www.biogen.com. Follow us on social media - Twitter, LinkedIn, Facebook, YouTube.
View source version on businesswire.com: https://www.businesswire.com/news/home/20221205005815/en/
Source: Sage Therapeutics, Inc.
Sage, Biogen complete rolling filing with FDA for depression therapy zuranolone
Dec. 06, 2022 7:20 AM ET
By: Ravikash, SA News Editor
- Sage Therapeutics (NASDAQ:SAGE) and Biogen (NASDAQ:BIIB) completed a rolling submission of a new drug application (NDA) with the U.S. Food and Drug Administration (FDA) for approval of zuranolone to treat major depressive disorder (MDD) and postpartum depression (PPD).
- https://seekingalpha.com/news/3914235-sage-biogen-complete-rolling-filing-with-fda-for-depression-therapy-zuranolone
- Biogen Inc. (BIIB), SAGE
- https://www.sagerx.com/
- https://www.sagerx.com/programs-research/pipeline
Darovasertib Combination Therapy with Crizotinib
Darovasertib Combination Therapy with Crizotinib
Darovasertib Combination Therapy with Crizotinib
IDEAYA Biosciences Receives Fast Track Designation for Darovasertib Combination Therapy with Crizotinib for the Treatment of Metastatic Uveal Melanoma
- Fast Track designation granted by U.S. FDA for evaluation of darovasertib in combination with crizotinib in adult patients being treated for metastatic uveal melanoma (MUM)
- Enables darovasertib / crizotinib development program to access expedited regulatory review processes, including potential eligibility for accelerated approval / priority review
SOUTH SAN FRANCISCO, Calif., Dec. 5, 2022 /PRNewswire/ --
IDEAYA Biosciences, Inc. (NASDAQ: IDYA), a synthetic lethality focused precision medicine oncology company committed to the discovery and development of targeted therapeutics, announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation to IDEAYA's development program investigating darovasertib, a potential first-in-class protein kinase C (PKC) inhibitor, for use in combination with crizotinib, an investigational cMET inhibitor, for the treatment of adult patients with metastatic uveal melanoma.
"We are extremely pleased to receive the U.S. FDA Fast Track designation as we prepare to initiate a potential Phase 2/3 registrational trial to evaluate the darovasertib and crizotinib combination in patients with MUM. The Fast Track designation acknowledges MUM as a serious condition and the potential for the darovasertib / crizotinib combination to treat this unmet medical need," said Dr. Darrin Beaupre, Senior Vice President and Chief Medical Officer at IDEAYA Biosciences.
Fast Track is a U.S. FDA process designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need. Under the Fast Track designation, the darovasertib / crizotinib development program in MUM is eligible for various expedited regulatory review processes, including generally more frequent FDA interactions (e.g., meetings, written communications), potential eligibility for rolling review of a New Drug Application (NDA) and potential accelerated approval and priority review of an NDA.
Darovasertib was previously also designated as an Orphan Drug by the U.S. FDA in Uveal Melanoma (UM), including in MUM, entitling IDEAYA to certain potential tax credits, exemptions from user fees, and statutory marketing exclusivity.
IDEAYA is targeting initiation of a potential registration-enabling trial for the darovasertib and crizotinib combination in MUM in Q1 2023, subject to FDA feedback and guidance.
IDEAYA is also planning to initiate a company-sponsored Phase 1 clinical trial in Q4 2022 to evaluate darovasertib monotherapy in neoadjuvant UM patients. The preliminary development approach contemplates clinical endpoints such as organ preservation and/or vision preservation proximal to primary interventional treatments. Additional information on the company's plans to evaluate darovasertib, including scientific insights and clinical development opportunities in the neoadjuvant setting, will be highlighted in an Investor R&D Day webcast being hosted by IDEAYA on December 12, 2022, at 8:00 am - 9:30 am ET. Registration is available at https://ir.ideayabio.com/events or https://lifescievents.com/event/ideaya-rd-day/.
About IDEAYA Biosciences
IDEAYA is a synthetic lethality-focused precision medicine oncology company committed to the discovery and development of targeted therapeutics for patient populations selected using molecular diagnostics. IDEAYA's approach integrates capabilities in identifying and validating translational biomarkers with drug discovery to select patient populations most likely to benefit from its targeted therapies. IDEAYA is applying its early research and drug discovery capabilities to synthetic lethality – which represents an emerging class of precision medicine targets.
SOURCE IDEAYA Biosciences, Inc.
IDEAYA wins FDA fast track status for melanoma treatment
Dec. 05, 2022 6:37 AM ET
IDEAYA Biosciences, Inc. (IDYA)PFE
By: Dulan Lokuwithana, SA News Editor
- Oncology-focused biotech IDEAYA Biosciences (NASDAQ:IDYA) announced Monday that the FDA granted Fast Track designation for its experimental drug darovasertib in metastatic uveal melanoma (MUM) as a combination therapy.
- Accordingly, the regulatory benefits related to FDA’s Fast Track designation will be applicable for darovasertib, a protein kinase C inhibitor, in combination with Pfizer’s (PFE) lung cancer therapy crizotinib as a treatment for adults with MUM.
- https://seekingalpha.com/news/3913825-idya-stock-on-watch-after-fda-fast-track-status-for-melanoma-treatment
- IDEAYA Biosciences, Inc. (IDYA)PFE
- https://www.ideayabio.com/pipeline/
biotecHOPE™ 2022
ANAVEX®2-73 (BLARCAMESINE)
ANAVEX®2-73 (BLARCAMESINE)
ANAVEX®2-73 (BLARCAMESINE)
ANAVEX®2-73 (BLARCAMESINE) PHASE 2B/3 STUDY MET PRIMARY AND KEY SECONDARY ENDPOINTS,
SHOWING STATISTICALLY SIGNIFICANT REDUCTION OF CLINICAL DECLINE IN GLOBAL CLINICAL STUDY OF PATIENTS WITH EARLY ALZHEIMER’S DISEASE
- Robust, Statistically Significant and Clinically Meaningful Absolute Improvement in Cognitive Function as Measured by ADAS-Cog and ADCS-ADL
- Key Secondary Endpoint CDR-SB Also Met, Demonstrating Statistically Significant Results
- Plan to Meet with Regulatory Authorities to Determine Next Steps
NEW YORK –December 1, 2022
Anavex Life Sciences Corp. (“Anavex” or the “Company”) (Nasdaq: AVXL), a clinical-stage biopharmaceutical company developing differentiated therapeutics for the treatment of neurodegenerative and neurodevelopmental disorders including Alzheimer’s disease, Parkinson’s disease, Rett syndrome and other central nervous system (CNS) disorders, today announced positive topline results from its Phase 2b/3 ANAVEX®2-73-AD-004 clinical trial of oral ANAVEX®2-73 (blarcamesine) for the treatment of mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) and mild AD (collectively known as early AD). ANAVEX®2-73 met the primary endpoints ADAS-Cog[1] and ADCS-ADL[2] and key secondary endpoint CDR-SB[3] with statistically significant results. Next step, in light of this data, is meeting with regulatory authorities to discuss this data in the context of ongoing development with an aim to bring this therapy to patients in Europe, Asia-Pacific, and the U.S.
ANAVEX®2-73 (blarcamesine) is an orally available, small-molecule activator of the sigma-1 receptor (SIGMAR1), which, data suggest, is pivotal to restoring neural cell homeostasis and promoting neuroplasticity.[4]
ANAVEX®2-73-AD-004 was a randomized, double-blind, multicenter, placebo-controlled 509 patient Phase 2b/3 study (randomized 1:1:1 to mid or high dose of ANAVEX®2-73 or placebo), for the treatment of early Alzheimer’s disease over 48 weeks. Top line data will be presented later today in the late breaking oral communication presentation at the Clinical Trials on Alzheimer’s Disease (CTAD) Congress 2022, December 1, 2022, at 4:30pm PT in San Francisco, CA. Further analysis of the data remains ongoing, and the Company plans to submit the data for publication in a peer-reviewed medical journal. The open-label extension study ATTENTION-AD will continue to follow participants over a 96 week period.
ANAVEX®2-73 treatment met the primary endpoints and reduced clinical decline on the global cognitive and functional scales over 48 weeks in the analysis of the Intent-to-treat (ITT) population.
ANAVEX®2-73 demonstrated visible improvement in patients with Alzheimer’s disease. Patients treated with ANAVEX®2-73 were 84% more likely, to have improved cognition by ADAS-Cog score change of -0.50 points or better from baseline to end of treatment than patients on placebo, Odds Ratio = 1.84 (p = 0.015). On average, patients, who improved cognitively with ANAVEX®2-73 treatment, improved by ADAS-Cog cognition score of -4.03 points. ANAVEX®2-73 treatment was 167% more likely to improve function compared with placebo, at a clinically meaningful improvement of ADCS-ADL score change of +3.5 points or better, Odds Ratio = 2.67 (p=0.0255). This reflects a robust improved and clinically meaningful outcome in cognition and function from baseline.
Additionally, treatment with ANAVEX®2-73 statistically significantly reduced cognitive decline, measured with ADAS-Cog, compared to placebo at end of treatment by 45%, representing a treatment difference in mean score change of -1.85 points (p=0.033).
ANAVEX®2-73 treatment also met the secondary endpoint of reduction in clinical decline of cognition and function assessed by the Clinical Dementia Rating Scale Sum of Boxes (CDR-SB) compared to placebo, by a treatment difference in mean score change of -0.42 points (p=0.040), representing 27% reduction in the ITT population.
ANAVEX®2-73 (blarcamesine) was generally safe and well tolerated. The incidence of treatment emergent adverse events (TEAEs) was similar in the active and placebo arms with dizziness being the most common TEAE. TEAEs ≥7.5% threshold were predominantly mild or moderate. No clinically significant changes in vital signs, laboratory values and ECG parameters in active and placebo arms were observed. Safety findings in the study were consistent with the known safety profile of ANAVEX®2-73.
In addition to safety and efficacy demonstrated on the primary and key secondary endpoints, a pre-specified analysis of patients without SIGMAR1 gene mutation provides further confidence of the robustness of the SIGMAR1 activation in the treatment of neurodegenerative diseases. Approximately 80% of the total worldwide population lack a SIGMAR1 gene mutation.[5] ANAVEX®2-73 was more efficacious in this pre-specified population. This effect is consistent with prior clinical trials of ANAVEX®2-73.[6]
“People living with Alzheimer’s disease desperately need new therapies and I am truly impressed with the outcome of this study, which demonstrated reversal of cognitive decline,” said A/Professor Stephen Macfarlane, FRANZCP, Head of Clinical Services at the Dementia Centre, HammondCare and Principal Investigator. “These results complement and are consistent with findings from the previously completed Alzheimer’s disease Phase 2a ANAVEX®2-73 trial, which also demonstrated therapeutic effect on cognition and function. ANAVEX®2-73 might be a very much needed solution for many patients with Alzheimer’s disease.”
“We are very pleased to see such positive clinical data in patients with Alzheimer’s disease, which is otherwise a progressive disease, thereby emphasizing the potentially significant implications these findings have for patients, caregivers, and healthcare systems worldwide,” said Edward R Hammond, MD, PhD, MPH, Chief Medical Officer of Anavex. “We intend to discuss these findings with regulatory authorities in the context of the ongoing clinical development of ANAVEX®2-73 in this indication, with the goal of providing a much-needed treatment to the millions of patients living with Alzheimer’s disease.”
“The successful results of the ANAVEX®2-73-AD-004 clinical trial would not be possible without the truly motivated and dedicated study participants, their families and caregivers and the clinical investigators around the world. We thank all the people involved in the study for their invaluable contributions,” said Christopher U. Missling, PhD, President and Chief Executive Officer of Anavex. “These clinical study findings confirm the robustness of the ANAVEX precision medicine platform, and we look forward to advancing ANAVEX®2-73 as a potential new treatment option for Alzheimer’s disease while we continue to focus on the effect of ANAVEX®2-73 leveraging this approach to drug development to provide intelligent solutions beyond many traditional neurology trials in disease areas with high unmet needs.”
Economic Burden of Alzheimer's Disease[7]
Alzheimer's disease is the most common cause of dementia and the fifth leading cause of death in adults older than 65 years. The estimated total healthcare costs for the treatment of Alzheimer's disease in 2020 were estimated at $305 billion, with the cost expected to increase to more than $1 trillion as the population ages. Most of the direct costs of care for Alzheimer's disease are attributed to skilled nursing care, home healthcare, and hospice care. Indirect costs of care, including quality of life and informal caregiving, are likely underestimated, and are associated with significant negative societal and personal burdens.
About Anavex Life Sciences Corp.
Anavex Life Sciences Corp. (Nasdaq: AVXL) is a publicly traded biopharmaceutical company dedicated to the development of novel therapeutics for the treatment of neurodegenerative and neurodevelopmental disorders, including Alzheimer's disease, Parkinson's disease, Rett syndrome, and other central nervous system (CNS) diseases, pain, and various types of cancer. Anavex's lead drug candidate, ANAVEX®2-73 (blarcamesine), has successfully completed a Phase 2a clinical trial for Alzheimer's disease, a Phase 2 proof-of-concept study in Parkinson's disease dementia, and both a Phase 2 and a Phase 3 study in adult patients with Rett syndrome. ANAVEX®2-73 is an orally available drug candidate that restores cellular homeostasis by targeting sigma-1 and muscarinic receptors. Preclinical studies demonstrated its potential to halt and/or reverse the course of Alzheimer's disease. ANAVEX®2-73 also exhibited anticonvulsant, anti-amnesic, neuroprotective, and anti-depressant properties in animal models, indicating its potential to treat additional CNS disorders, including epilepsy. The Michael J. Fox Foundation for Parkinson's Research previously awarded Anavex a research grant, which fully funded a preclinical study to develop ANAVEX®2-73 for the treatment of Parkinson's disease. ANAVEX®3-71, which targets sigma-1 and M1 muscarinic receptors, is a promising clinical stage drug candidate demonstrating disease-modifying activity against the major hallmarks of Alzheimer's disease in transgenic (3xTg-AD) mice, including cognitive deficits, amyloid, and tau pathologies. In preclinical trials, ANAVEX®3-71 has shown beneficial effects on mitochondrial dysfunction and neuroinflammation. Further information is available at www.anavex.com. You can also connect with the company on Twitter, Facebook, Instagram, and LinkedIn.

Anavex's drug improves cognitive function in Alzheimer's patients, meets main goal of trial
Dec. 02, 2022 6:53 AM ET
Anavex Life Sciences Corp. (AVXL)
By: Ravikash, SA News Editor12 Comments
Anavex Life Sciences (NASDAQ:AVXL) said its oral drug ANAVEX2-73 (blarcamesine) met the main goal of improvement in cognitive function in patients with early Alzheimer's disease (AD) in a phase 2B/3 trial.
Anavex Life Sciences Corp. (AVXL)
https://www.anavex.com/therapeutic-candidates
Donanemab
ANAVEX®2-73 (BLARCAMESINE)
ANAVEX®2-73 (BLARCAMESINE)
Lilly Shares Positive Donanemab Data in First Active Comparator Study in Early Symptomatic Alzheimer's Disease
November 30, 2022
- Brain amyloid clearance (<24.1 Centiloids) was achieved in 37.9% of donanemab-treated participants compared with 1.6% of Aduhelm® (aducanumab-avwa)-treated patients at 6 months
- Donanemab reduced brain amyloid plaque levels vs. baseline by 65.2% compared with 17.0% for Aduhelm® at 6 months
SAN FRANCISCO, Nov. 30, 2022 /PRNewswire/ -- Eli Lilly and Company (NYSE: LLY) has announced that donanemab met all primary and secondary endpoints for the 6-month primary outcome analysis in the Phase 3 TRAILBLAZER-ALZ 4 study, providing the first active comparator data on amyloid plaque clearance in patients with early symptomatic Alzheimer's disease treated with amyloid-targeting therapies. These data comparing donanemab to Aduhelm® * (aducanumab-avwa) to assess superiority on amyloid plaque reduction were shared at the 15th Clinical Trials on Alzheimer's Disease (CTAD) conference. Donanemab is an investigational antibody that targets a modified form of beta amyloid plaque called N3pG.
Through the FDA's accelerated approval pathway, the FDA has recognized that the reduction of amyloid beta plaque is a biomarker reasonably likely to predict clinical benefit in the treatment of early Alzheimer's disease.
"The purpose of this first ever active comparator trial of amyloid lowering agents was to answer important questions about potential differences in amyloid plaque reduction," said Mark Mintun, M.D., group vice president of pain and neurodegeneration research and development, Eli Lilly and Company. "These data reinforce our confidence in donanemab's unique mechanism of action based on reductions in key biomarkers of Alzheimer's disease, amyloid plaque and plasma phosphorylated tau (P-tau). Importantly, this was also the first study to obtain ARIA rates side by side using identical methods for ARIA assessment in the same patient population, demonstrating the ability to disconnect rate of plaque clearance from rate of ARIA incidence."
In the co-primary outcomes, brain amyloid plaque clearance, defined as achieving brain amyloid plaque levels of <24.1 Centiloids, was achieved in 37.9% of donanemab-treated participants (25 of 66) compared with 1.6% of Aduhelm-treated patients (1 of 64) at 6 months; in the intermediate tau subpopulation, 38.5% of donanemab-treated participants (10 of 26) reached brain amyloid clearance compared with 3.8% of Aduhelm-treated participants (1 of 26) by 6 months. In a key secondary outcome, donanemab reduced brain amyloid levels vs. baseline by 65.2% compared with 17.0% for Aduhelm at 6 months. In an exploratory outcome, donanemab, but not aducanumab-avwa, treatment significantly reduced plasma P-tau217 at 6 months compared to baseline.
The safety profile of both treatments was consistent with their previously published studies. ARIA was the most common treatment emergent adverse event in both groups. In the aducanumab-avwa group, the incidence of total ARIA was 26.1% with 4.3% being symptomatic. In the donanemab group, the incidence of total ARIA was 25.4% with 2.8% being symptomatic. For both treatments, all symptomatic cases were related to ARIA-E.
"It is encouraging to see that donanemab produced significant reduction of amyloid build up in the brain and P-tau in the blood after 6 months. This suggests that this treatment modified the biology of Alzheimer's disease early on in treatment," said Stephen Salloway, MD, associate director of the Center for Alzheimer's Disease Research at Brown University, who presented the findings. "It is also notable in TRAILBLAZER-ALZ 4 that the higher amyloid clearance by donanemab compared to aducanumab-avwa at 6 months was not associated with a higher rate of ARIA."
TRAILBLAZER-ALZ 4 is ongoing and will have 12-month and 18-month secondary analyses. The study is one of five studies that comprise the clinical program to evaluate the efficacy and safety of donanemab. In August, Lilly announced that the FDA accepted the donanemab application for review, with Priority Review designation, for Alzheimer's disease under the accelerated approval pathway.
About TRAILBLAZER-ALZ 4 Study
TRAILBLAZER-ALZ 4 (LY3002813) is a multicenter, randomized, open-label Phase 3 study of that enrolled 148 patients aged 50 to 85 with early symptomatic AD who met entry criteria including a Clinical Dementia Rating (CDR)-Global Score of 0.5 or 1 and gradual and progressive change in memory function for more than six months, among other criteria. Donanemab and Aduhelm are administered via intravenous infusions every four weeks for up to 18 months. Donanemab is administered until evidence of plaque clearance via positron emission tomography (PET) at 6, 12, or 18 months. Aduhelm is administered through the duration of the study according to its approved label. The studies' co-primary endpoints are superiority on, as measured by PET scan: the percentage of participants who reach complete amyloid plaque clearance and the percentage of participants who reach complete amyloid plaque clearance in the intermediate tau subpopulation at 6 months.
Lilly previously announced and published in the New England Journal of Medicine (NEJM) results from the Phase 2 TRAILBLAZER-ALZ study in March 2021. In June 2021, Lilly announced that the FDA had granted Breakthrough Therapy designation for donanemab based on the TRAILBLAZER-ALZ data.
About Alzheimer's Disease
Alzheimer's disease is a fatal illness that causes progressive decline in memory and other aspects of cognition. Dementia due to Alzheimer's disease is the most common form of dementia, accounting for 60 to 80 percent of all cases1. There are currently over 55 million people living with dementia around the world, with numbers expected to increase to nearly 139 million by 20502. Over 10 million new cases of dementia are diagnosed each year worldwide, implying one new case every 3.2 seconds, and a significant increase in the caregiving burden placed on society and families. In the US alone, there was an increase of nearly 10 million new caregivers from 2015 to 20203. The current annual societal and economic cost of dementia is estimated at $1.3 trillion, an amount that is expected to double by 2030 unless we find a way to slow the disease2.
About Lilly
Lilly unites caring with discovery to create medicines that make life better for people around the world. We've been pioneering life-changing discoveries for nearly 150 years, and today our medicines help more than 47 million people across the globe. Harnessing the power of biotechnology, chemistry and genetic medicine, our scientists are urgently advancing new discoveries to solve some of the world's most significant health challenges, redefining diabetes care, treating obesity and curtailing its most devastating long-term effects, advancing the fight against Alzheimer's disease, providing solutions to some of the most debilitating immune system disorders, and transforming the most difficult-to-treat cancers into manageable diseases. With each step toward a healthier world, we're motivated by one thing: making life better for millions more people. That includes delivering innovative clinical trials that reflect the diversity of our world and working to ensure our medicines are accessible and affordable. To learn more, visit Lilly.com and Lilly.com/newsroom or follow us on Facebook, Instagram, and LinkedIn. P-LLY
© Lilly USA, LLC 2022. ALL RIGHTS RESERVED.

View original content to download multimedia:https://www.prnewswire.com/news-releases/lilly-shares-positive-donanemab-data-in-first-active-comparator-study-in-early-symptomatic-alzheimers-disease-301690725.html
SOURCE Eli Lilly and Company
Lilly posts Phase 3 data to compare its Alzheimer’s drug vs. Biogen’s
Dec. 01, 2022 7:15 AM ET
Eli Lilly and Company (LLY), BIIB, ESALF, ESALY
By: Dulan Lokuwithana, SA News Editor
Eli Lilly (NYSE:LLY) shared data from a Phase 3 trial for its Alzheimer's disease donanemab, comparing its performance against Aduhelm, an FDA-approved Alzheimer's therapy developed by Biogen (NASDAQ:BIIB) and Eisai (OTCPK:ESALF) (OTCPK:ESALY)
Eli Lilly and Company (LLY), BIIB, ESALF, ESALY
https://www.clinicaltrials.gov/ct2/show/NCT05508789
November 30, 2022
VLA15
ANAVEX®2-73 (BLARCAMESINE)
batiraxcept (AVB-500)
Valneva and Pfizer Report Six-Month Antibody Persistence Data in Children and Adults for Lyme Disease Vaccine Candidate
December 1, 2022
- Antibody levels remained above baseline six months after completion of a three-dose (Month 0-2-6) or a two-dose (Month 0-6) vaccination schedule
- Higher antibody levels were observed in the three-dose vaccination schedule versus the two-dose vaccination schedule, further validating the use of this schedule in the ongoing Phase 3 study
- There were no safety concerns observed in this six-month observational follow up
New York & Saint-Herblain (France), December 1, 2022 – Pfizer Inc. (NYSE: PFE) and Valneva SE (Nasdaq: VALN; Euronext Paris: VLA) today reported antibody persistence data six months after the completion of a three-dose (Month 0-2-6) or a two-dose (Month 0-6) vaccination schedule with their Lyme disease vaccine candidate, VLA15 in both children and adults. This is the first time antibody persistence data are reported in pediatric populations for this vaccine candidate.
Following positive immunogenicity and safety data for Phase 2 study VLA15-221 in April 2022[1], Valneva and Pfizer evaluated the persistence of antibodies six months after the Month 0-2-6 and the Month 0-6 vaccination schedule with VLA15 in healthy adults and pediatric participants (5 to 65 years of age). Data were collected in 96 healthy adults and 81 pediatric participants (5-17 years of age) for the Month 0-2-6 vaccination schedule and in 84 healthy adults and 78 pediatric participants (5-17 years of age) for the Month 0-6 schedule.
As observed in previous clinical studies with VLA15, antibody levels declined over time in all study groups but remained above baseline, confirming their persistence six months after completion of both vaccination schedules. Overall, antibody levels remained higher with the three-dose vaccination schedule compared to the two-dose schedule. Geometric mean fold rise (GMFRs) compared to baseline were 1.9-fold for Serotype 1 (ST1) to 3.2-fold Serotype 2 (ST2) across all age groups in the Month 0-2-6 vaccination schedule. The highest GMFRs were reported in the 5 to 11 years old age group, with GMFR levels at 2.8-fold (ST1) to 6.6-fold (ST2).
These results further validate the use of the three-dose vaccination schedule which is also included in the Phase 3 protocols for all participants.
No vaccine-related serious adverse events (SAEs) and no safety concerns were observed in this six-month observational follow up.
Juan Carlos Jaramillo M.D., Chief Medical Officer of Valneva, said, “We are pleased with these antibody persistence data that further validate the use of the three-dose vaccination schedule in our ongoing Phase 3 study and the acceptable safety and tolerability profiles of our vaccine candidate. Lyme disease continues to spread, representing a high unmet medical need that impacts the lives of many in the Northern Hemisphere, and each new report of positive data takes us a step closer to potentially bringing this vaccine to both adults and children who could benefit from it.”
Earlier this year, Pfizer and Valneva initiated a Phase 3 clinical study, Vaccine Against Lyme for Outdoor Recreationists (VALOR) (NCT05477524), to investigate the efficacy, safety and immunogenicity of VLA15[2]. Approximately 6,000 participants 5 years of age and older will receive three doses of VLA15 180 µg or saline placebo as a primary vaccination series followed by one booster dose of VLA15 or saline placebo (1:1 ratio). Enrollment is ongoing in Europe and the United States and expected to be completed in the second quarter of 2023. To learn more, visit www.pfizerclinicaltrials.com/nct05477524. To achieve the required pediatric safety database, Pfizer and Valneva are planning to initiate a complementary Phase 3 clinical study in early December 2022 to collect additional VLA15 safety data in participants 5 to 17 years of age.
“Rates of Lyme disease continue to increase globally, underscoring the importance of a vaccine that may help protect both adults and children,” said Annaliesa Anderson, Ph.D., Senior Vice President and Chief Scientific Officer of Vaccine Research & Development at Pfizer. “These six-month antibody persistence data are encouraging, and we hope that the data generated from the Phase 3 studies will further support the positive evidence for VLA15 to date.”
Pending successful completion of the Phase 3 studies, Pfizer could potentially submit a Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA) and Marketing Authorisation Application (MAA) to the European Medicines Agency (EMA) in 2025.
About VLA15
VLA15 is the only Lyme disease vaccine candidate currently in clinical development. This investigational multivalent protein subunit vaccine uses an established mechanism of action for a Lyme disease vaccine that targets the outer surface protein A (OspA) of Borrelia burgdorferi, the bacteria that cause Lyme disease. OspA is a surface protein expressed by the bacteria when present in a tick. Blocking OspA inhibits the bacterium’s ability to leave the tick and infect humans. The vaccine covers the six most common OspA serotypes expressed by the Borrelia burgdorferi sensu lato species that are prevalent in North America and Europe. VLA15 has demonstrated a strong immune response and satisfactory safety profile in pre-clinical and clinical studies so far. Valneva and Pfizer entered into a collaboration agreement in April 2020 to co-develop VLA15, with updates to the terms within this agreement made in June 2022.3,4 The terms of the collaboration agreement include a $25 million milestone payment made to Valneva upon Pfizer’s initiation of the Phase 3 study. The program was granted Fast Track designation by the U.S. FDA in July 2017.5
About Clinical Study VLA15-221
VLA15-221 is a randomized, observer-blind, placebo-controlled Phase 2 study. It is the first clinical study with VLA15 which enrolled a pediatric population (5-17 years old).
585 healthy participants received VLA15 at two different immunization schedules (month 0-2-6 [N=190] or month 0-6 [N=187]) or three doses of placebo (month 0-2-6 [N=208]). Vaccine recipients received VLA15 at a dose of 180 µg, which was selected based on data generated in the two previous Phase 2 studies. The main safety and immunogenicity readout was performed one month after the primary vaccination series. A subset of participants will receive a booster dose of VLA15 or placebo at month 18 (booster phase) and will be followed for three additional years to monitor antibody persistence.
VLA15 is tested as an alum-adjuvanted formulation and administered intramuscularly. The study is being conducted at U.S. sites located in areas where Lyme disease is endemic and has enrolled both volunteers with a cleared past infection with Borrelia burgdorferi as well as Borrelia burgdorferi-naïve volunteers.
About Lyme Disease
Lyme disease is a systemic infection caused by Borrelia burgdorferi bacteria transmitted to humans by infected Ixodes ticks.6 It is considered the most common vector-borne illness in the Northern Hemisphere.7 While the true incidence of Lyme disease is unknown, it is estimated to annually affect approximately 476,000 people in the United States and 130,000 people in Europe.8,9 Early symptoms of Lyme disease (such as a gradually expanding erythematous rash called Erythema migrans or more nonspecific symptoms like fatigue, fever, headache, mild stiff neck, arthralgia or myalgia) are often overlooked or misinterpreted. Left untreated, the disease can disseminate and cause more serious complications affecting the joints (arthritis), the heart (carditis) or the nervous system.9 The medical need for vaccination against Lyme disease is steadily increasing as the geographic footprint of the disease widens.8
About Valneva SE
Valneva is a specialty vaccine company focused on the development and commercialization of prophylactic vaccines for infectious diseases with significant unmet medical need. The Company takes a highly specialized and targeted approach to vaccine development and then applies its deep understanding of vaccine science to develop prophylactic vaccines addressing these diseases. Valneva has leveraged its expertise and capabilities both to commercialize three vaccines and to rapidly advance a broad range of vaccine candidates into and through the clinic, including candidates against Lyme disease and the chikungunya virus.
Pfizer, Valneva Lyme disease vaccine shows antibodies even 6-month after vaccination
Dec. 01, 2022 6:16 AM ET
By: Ravikash, SA News Editor1 Comment
Pfizer (NYSE:PFE) and Valneva (NASDAQ:VALN) said their Lyme disease vaccine VLA15 showed antibody levels remained above baseline six months after vaccination in a phase 2 trial.
https://valneva.com/research-development/lyme-disease/
https://clinicaltrials.gov/ct2/show/NCT04801420
batiraxcept (AVB-500)
batiraxcept (AVB-500)
batiraxcept (AVB-500)
Press Release
Nov 29, 2022
Aravive Announces Fast Track Designation of Batiraxcept for Treatment of ccRCC
FDA decision based on new Phase 1b data: Objective Response Rate (ORR) of 57% and median Progression-Free Survival (PFS) of 11.4 months in patients with advanced or metastatic clear cell renal cell carcinoma (ccRCC) who have progressed after 1 or 2 prior lines of immuno-oncology (IO)- and vascular endothelial growth factor tyrosine kinase inhibitor (VEGF-TKI)-based therapies
HOUSTON, Nov. 29, 2022 (GLOBE NEWSWIRE) -- Aravive, Inc. (Nasdaq: ARAV, “the Company”), a late clinical-stage oncology company developing targeted therapeutics to treat metastatic disease, today announced the U.S. Food and Drug Administration (FDA) has granted Fast Track Designation to the company’s lead program, batiraxcept, for treatment of patients with advanced or metastatic clear cell renal cell carcinoma (ccRCC) who have progressed after 1 or 2 prior lines of systemic therapy that include both immuno-oncology (IO)-based and vascular endothelial growth factor tyrosine kinase inhibitor (VEGF-TKI)-based therapies (either in combination or sequentially).
Fast Track is a process designed to facilitate the development and expedite the review of investigational drugs to treat serious conditions and fill an unmet medical need. Drugs that receive Fast Track designation may be eligible for more frequent communications and meetings with the FDA to discuss the drug's development plan, including the design of the proposed clinical trials, use of biomarkers and the extent of data needed to support approval. Drugs with Fast Track Designation may also qualify for accelerated and priority review of new drug applications if relevant criteria are met.
The Fast Track Designation was based on new data submitted to the agency from the P1b clear cell renal cell cancer (ccRCC) study (AVB500-RCC-003; NCT04300140). As of September 26, 2022, 26 previously treated (second line or greater) patients with ccRCC have been treated with batiraxcept in the Phase 1b portion of a Phase 1b/2 trial at doses of 15 mg/kg (n=16) and 20 mg/kg (n=10), plus cabozantinib 60 mg daily. There were no dose limiting toxicities observed at either dose. Clinical data from this study demonstrate that batiraxcept has the potential to increase the clinical activity of cabozantinib in patients with metastatic ccRCC who have progressed following IO- and VEGF-TKI-based therapies (N=14 of the 26 patients) as the Objective Response Rate (ORR) was 57% and median Progression-Free Survival (PFS) was 11.4 months in this population.
“The majority of patients with kidney cancer develop resistance to frontline treatment and there is a clinical need for novel agents to improve upon treatment options in the refractory setting,” said Kathryn Beckermann, M.D., Ph.D., Assistant Professor, Division of Hematology and Oncology, Vanderbilt University Medical Center, and lead investigator for the trial. “Response rates to single agent targeted kinase inhibitors are approximately 30% with a PFS of approximately 7 months. The early data seen with batiraxcept including biomarker development, response rate, and progression-free survival are promising.”
“A review of the literature suggests that the clinical activity of cabozantinib is lower in those patients who have progressed following a VEGF-TKI-based therapy compared to patients who have progressed on IO or IO/IO therapy. Since preclinical data published by Xiao in 20191 observed that batiraxcept may restore TKI sensitivity, it makes sense that the combination of batiraxcept and cabozantinib may exhibit its greatest impact in those patients who have failed prior VEGF-TKI therapies,” said Gail McIntyre, Ph.D., DABT, Chief Executive Officer of Aravive. “Understanding the P1b ccRCC data has allowed us to identify the most appropriate patient population in which to evaluate batiraxcept in combination with cabozantinib and potentially the quickest path to approval in this population with an unmet medical need.”
_______________
1 Cancer Res 2019;79:5758–68
About Aravive
Aravive, Inc. is a late clinical-stage oncology company developing targeted therapeutics to treat metastatic disease. Our lead product candidate, batiraxcept (formerly AVB-500), is an ultra-high affinity decoy protein that binds to GAS6, the sole ligand that activates AXL, thereby inhibiting metastasis and tumor growth, and restoring sensitivity to anti-cancer agents. Batiraxcept has been granted Fast Track Designation by the U.S. FDA and Orphan Drug Designation by the European Commission in platinum-resistant recurrent ovarian cancer. Batiraxcept is in an active registrational Phase 3 trial in platinum resistant ovarian cancer (NCT04729608), a Phase 1b/2 trial in clear cell renal cell carcinoma (NCT04300140), and a Phase 1b/2 trial in pancreatic adenocarcinoma (NCT04983407). The Company is based in Houston, Texas and received a Product Development Award from the Cancer Prevention & Research Institute of Texas (CPRIT) in 2016. Additional information at www.aravive.com.
Aravive gains on FDA Fast Track status for lead program
Nov. 29, 2022 7:42 AM ET
By: Dulan Lokuwithana, SA News Editor
- Clinical-stage oncology company Aravive, Inc. (NASDAQ:ARAV) added ~7% pre-market Tuesday after announcing that the FDA granted Fast Track Designation to its lead program, batiraxcept, as a treatment for certain kidney cancer patients.
- https://seekingalpha.com/news/3911854-arav-stock-gains-on-fda-fast-track-status-for-lead-program
- Aravive, Inc. (ARAV)
- https://aravive.com/pipeline/
- https://aravive.com/
XENLETA® (lefamulin)
batiraxcept (AVB-500)
XENLETA® (lefamulin)
Nabriva Therapeutics Announces Positive Topline Results from Phase 1 Trial of XENLETA® (lefamulin) in Adult Patients with Cystic Fibrosis
November 28, 2022 at 7:01 AM EST
- PK Data and Safety Profile Consistent with Previous Studies in Healthy Subjects –
- Results Support Potential Utility of Lefamulin in Patients with Cystic Fibrosis -
DUBLIN, Ireland and FORT WASHINGTON, Pa., Nov. 28, 2022 (GLOBE NEWSWIRE) -- Nabriva Therapeutics plc (NASDAQ: NBRV), a biopharmaceutical company engaged in the commercialization and development of innovative anti-infective agents to treat serious infections, announced positive topline results from their Phase 1 clinical trial that assessed the safety and pharmacokinetics (PK) of oral and intravenous (IV) XENLETA® (lefamulin) in adult patients with cystic fibrosis (CF).
“We are excited to share positive topline results from this important study of XENLETA in patients with CF,” said Christine Guico-Pabia, M.D., MBA, MPH, Nabriva’s Chief Medical Officer. “The data indicate that the PK of XENLETA in CF patients is consistent with that observed in previous single-dose healthy volunteer studies evaluating the approved oral and IV dosing for adults with community-acquired bacterial pneumonia (CABP). In addition, XENLETA was well-tolerated and the adverse event profile in CF patients was consistent with that described across our clinical program.
Dr. Guico-Pabia added, “XENLETA has been demonstrated to be a potent anti-staphylococcal antibiotic in in vitro and clinical studies, including against methicillin-resistant S. aureus (MRSA). There are limited treatment options for the management of bacterial exacerbations in CF patients caused by S. aureus and the results of this study support the potential utility of XENLETA in this difficult to treat patient population. We would like to thank the study participants, investigators, and the Cystic Fibrosis Foundation for their support of this important study and look forward to sharing the complete results with the medical community in the first half of 2023.”
About the Trial
The Phase 1 trial is an open-label, randomized, single-dose, crossover study to assess the safety and pharmacokinetics of oral (600 mg) and IV (150 mg) XENLETA in adult patients with cystic fibrosis. The dosing utilized in this study is consistent with the FDA approved dosage for the treatment of adults with CABP.
More information can be found at ClinicalTrials.gov -NCT05225805.
About Nabriva Therapeutics plc
Nabriva Therapeutics is a biopharmaceutical company engaged in the commercialization and development of innovative anti-infective agents to treat serious infections. Nabriva Therapeutics received U.S. Food and Drug Administration approval for XENLETA® (lefamulin injection, lefamulin tablets), the first systemic pleuromutilin antibiotic for community-acquired bacterial pneumonia (CABP). Nabriva Therapeutics is also developing CONTEPO™ (fosfomycin) for injection, a potential first-in-class epoxide antibiotic for complicated urinary tract infections (cUTI), including acute pyelonephritis. Nabriva entered into an exclusive agreement with subsidiaries of Merck & Co. Inc., Kenilworth, N.J., USA to market, sell and distribute SIVEXTRO® (tedizolid phosphate) in the United States and certain of its territories.
About XENLETA
XENLETA (lefamulin) is a first-in-class semi-synthetic pleuromutilin antibiotic for systemic administration in humans discovered and developed by the Nabriva Therapeutics team. It is designed to inhibit the synthesis of bacterial protein, which is required for bacteria to grow. XENLETA’s binding occurs with high affinity, high specificity and at molecular sites that are different than other antibiotic classes. Efficacy of XENLETA was demonstrated in two multicenter, multinational, double-blind, double-dummy, non-inferiority trials assessing a total of 1,289 patients with CABP. In these trials, XENLETA was compared with moxifloxacin and in one trial, moxifloxacin with and without linezolid. Patients who received XENLETA had similar rates of efficacy as those taking moxifloxacin alone or moxifloxacin plus linezolid. The most common adverse reactions associated with XENLETA included diarrhea, nausea, reactions at the injection site, elevated liver enzymes, and vomiting. For more information, please visit www.XENLETA.com.
Indication and Important Safety Information
Indication
XENLETA is a pleuromutilin antibacterial indicated for the treatment of adults with community-acquired bacterial pneumonia (CABP) caused by the following susceptible microorganisms: Streptococcus pneumoniae, Staphylococcus aureus (methicillin-susceptible isolates), Haemophilus influenzae, Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydophila pneumoniae.
Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of XENLETA and other antibacterial drugs, XENLETA should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria.
Important Safety Information
CONTRAINDICATIONS
XENLETA is contraindicated in patients with known hypersensitivity to XENLETA or pleuromutilins.
XENLETA tablets are contraindicated for use with CYP3A4 substrates that prolong the QT interval.
Please see Full Prescribing Information for XENLETA at www.XENLETA.com.
Source: Nabriva Therapeutics US, Inc
Nabriva gains after announcing Phase 1 data for cystic fibrosis candidate
Nov. 28, 2022 10:07 AM ET
Nabriva Therapeutics plc (NBRV)
By: Dulan Lokuwithana, SA News Editor
- Ireland-based pharma Nabriva Therapeutics (NASDAQ:NBRV) rose ~15% on Monday morning after announcing results from a Phase 1 trial for its antibiotic Xenleta in adults with cystic fibrosis (CF).
- https://seekingalpha.com/news/3911601-nbrv-stock-gains-after-announcing-phase-1-data-for-cystic-fibrosis-candidate
- Nabriva Therapeutics plc (NBRV)
- https://www.xenleta.com/
- https://www.nabriva.com/
axs-05
batiraxcept (AVB-500)
XENLETA® (lefamulin)
axsome therapeutics announces axs-05 achieves primary endpoint in the accord phase 3 trial in alzheimer’s disease agitation
November 28, 2022
AXS-05 statistically significantly delayed time to relapse of Alzheimer’s disease agitation versus placebo (p=0.014, primary endpoint)
AXS-05 statistically significantly prevented relapse of Alzheimer’s disease agitation versus placebo (p=0.018, key secondary endpoint)
Statistically significant improvement in Alzheimer’s disease agitation, as measured by the CMAI total score, starting at Week 1 with open-label AXS-05 (p<0.001 vs baseline, all timepoints)
Improvement in Alzheimer’s disease agitation, assessed by the modified Alzheimer’s Disease Cooperative Study-CGIC scale, achieved by 66% of patients at 2 weeks and 86% at 5 weeks
Improvement in Alzheimer’s disease agitation, assessed by the PGI-C scale, achieved by 68% of patients at 2 weeks and 89% at 5 weeks
No treatments are currently approved for Alzheimer’s disease agitation
NEW YORK, Nov. 28, 2022 (GLOBE NEWSWIRE) -- Axsome Therapeutics, Inc. (NASDAQ: AXSM), a biopharmaceutical company developing and delivering novel therapies for the management of central nervous system (CNS) disorders, today announced that AXS-05, a novel, oral, investigational NMDA receptor antagonist with multimodal activity, met the primary and key secondary endpoints in the ACCORD (Assessing Clinical Outcomes in Alzheimer’s Disease Agitation) Phase 3 trial, by substantially and statistically significantly delaying the time to relapse and preventing relapse of agitation in patients with Alzheimer’s disease, as compared to placebo. The ACCORD study was a double-blind, placebo-controlled, multi-center, randomized withdrawal, U.S. trial which treated 178 patients with Alzheimer’s disease agitation. Patients achieving a sustained clinical response after open-label treatment with AXS-05 were randomized (n=108) in a 1:1 ratio to continue treatment with AXS-05 or to discontinue AXS-05 and switch to placebo. AXS-05 has been granted Breakthrough Therapy designation by the U.S. Food and Drug Administration (FDA) for the treatment of Alzheimer’s disease agitation. There are currently no FDA-approved treatments for Alzheimer’s disease agitation.
AXS-05 met the primary endpoint by substantially and statistically significantly delaying the time to relapse of agitation symptoms as compared to placebo, with a hazard ratio for time to relapse of 0.275 (p=0.014), representing a 3.6-fold lower risk of relapse compared to placebo. AXS-05 also met the key secondary endpoint of relapse prevention, based on the rates of relapse during the double-blind treatment period (7.5% of AXS-05 patients vs. 25.9% of placebo patients, p=0.018). Relapse was defined as a ≥10-point worsening in the CMAI total score from randomization or a CMAI total score greater than that at study entry; or hospitalization or other institutionalization due to agitation associated with Alzheimer’s disease.
With open-label treatment with AXS-05, patients experienced rapid, substantial, and statistically significant improvement compared to baseline in agitation symptoms. Statistically significant improvement on the Cohen Mansfield Agitation Inventory (CMAI) was seen with open-label AXS-05 treatment at all timepoints starting at Week 1 (p<0.001), with mean reductions from baseline of 11.0 points at Week 2 (p<0.001), and 20.6 points at Week 5 (p<0.001). Improvements were also significant with open-label AXS-05 treatment on all CMAI subscales including the Physically Aggressive subscale at all timepoints (p<0.001).
Jeffrey Cummings, MD, ScD, Director Emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health, and Chambers Professor of Brain Science at the University of Nevada Las Vegas said, “Agitation is one of the most troubling and consequential aspects of Alzheimer’s disease for patients and their caregivers as it is associated with early nursing home placement, accelerated cognitive decline, and increased mortality. The results of the ACCORD trial demonstrate convincing clinical activity for AXS-05 on agitation associated with Alzheimer’s disease based on both a significant delay in symptom relapse as well as a reduction of relapse compared to placebo. Treatment with AXS-05 during the open-label period in a large cohort of patients resulted in rapid and clinically meaningful improvements in Alzheimer’s disease agitation. The improvements were especially notable since they were seen on the aggressive symptom subscales of the agitation measures. Agitation occurs in the majority of patients with Alzheimer’s disease and there are currently no treatments approved for this condition. AXS-05 could potentially fill this high unmet medical need for patients and their caregivers, if approved, based on the observed positive efficacy and favorable safety and tolerability results.”
Rapid and substantial improvement in Alzheimer’s disease agitation was reported by both clinicians and caregivers on global measures. Clinicians reported improvement in agitation in 66.3% of patients at Week 2 and 86.3% at Week 5 after treatment with AXS-05, as assessed using the modified Alzheimer’s Disease Cooperative Study-Clinical Global Impression of Change for Agitation (mADCS-CGIC). Caregivers reported improvement in agitation in 67.5% of patients at Week 2 and 89.3% at Week 5 after treatment with AXS-05, as assessed using the Patient Global Impression of Change (PGI-C) rated by the caregiver.
Caregiver distress and burden, patient quality of life, and depressive symptoms were all statistically significantly improved compared to baseline after patients were treated with open-label AXS-05. Caregiver distress was assessed using the NPI Agitation and Aggression Caregiver Distress score (p<0.001, at Weeks 4 and 8). Caregiver burden was assessed using the Zarit Burden Interview (ZBI) (p=0.006 at Week 4, p=0.003 at Week 8). Patient quality of life was assessed using the caregiver rated Quality of Life Alzheimer’s Disease (QoL-AD) scale (p<0.001 at Week 4, p=0.013 at Week 8). Depressive symptoms were assessed using the Cornell Scale for Depression in Dementia (CSDD) (p<0.001, at Weeks 4 and 8).
Herriot Tabuteau, MD, Chief Executive Officer of Axsome said, “With the positive results from ACCORD, AXS-05 has now demonstrated efficacy in the treatment of Alzheimer’s disease agitation in two well-controlled trials. In addition to the strong results versus placebo in the double-blind period, results from the open-label period evidenced rapid, substantial, and significant improvements in Alzheimer’s disease agitation versus baseline with AXS-05 treatment. The ACCORD results complement, and are consistent with, those from the previously completed positive ADVANCE-1 trial. We intend to discuss these findings with the FDA in the context of the ongoing clinical development of AXS-05 in this indication, with the goal of providing a much needed treatment to the millions of patients living with Alzheimer’s disease agitation and their caregivers.”
The rates of adverse events observed in the double-blind period were 28.3% in the AXS-05 group and 22.2% in the placebo group. Discontinuations in the double-blind period due to adverse events were low (0% for AXS-05 and 1.9% for placebo). One serious adverse event was reported in the AXS-05 group (faecaloma), which was determined by the investigator to be not related to study medication, and 2 serious adverse events were reported in the placebo group (cardiac arrest, femur fracture). Falls were reported in 4 patients in the AXS-05 group, none of which were associated with serious adverse events and all of which were determined by the investigators to be not related to study medication, and in 2 patients in the placebo group, one of which was associated with a femur fracture. One death was reported in the placebo group. There was no evidence of cognitive decline for patients treated with AXS-05 as shown by the Mini-Mental State Examination (MMSE), a widely utilized measure of general cognitive function. Treatment with AXS-05 was not associated with sedation.
AXS-05 was granted Breakthrough Therapy designation for the treatment of Alzheimer's disease agitation by the FDA in June 2020. The FDA Breakthrough Therapy designation was supported by the positive results of the ADVANCE-1 trial. A Breakthrough Therapy designation is granted to potentially expedite development and review timelines for a promising investigational medicine when preliminary clinical evidence indicates it may demonstrate substantial improvement on one or more clinically significant endpoints over available therapies for a serious or life-threatening condition.
Open-label Period Results Summary
A total of 178 patients were treated with open-label AXS-05 for up to 9 weeks and assessed for efficacy. The primary timepoint for open-label efficacy assessments was 5 weeks, and the key secondary timepoint was 2 weeks. P-values were calculated versus baseline.
- The mean CMAI total score was 70.9 at baseline.
- Treatment with AXS-05 was associated with a mean reduction from baseline in the CMAI total score of 6.7 points at Week 1, 11.0 points at Week 2, and 20.6 points at Week 5 (p<0.001 for all).
- Clinical response on the CMAI (defined as ≥30% reduction from baseline) after treatment with AXS-05 was achieved by 21.8% of patients at Week 1, 40.4% of patients at Week 2, and 70.0% of patients at Week 5.
- Treatment with AXS-05 was also associated with improvements on all CMAI subscales including the Physically Aggressive subscale at all timepoints (p<0.001).
- Improvement in Alzheimer’s disease agitation, assessed using the clinician rated mADCS-CGIC, was achieved by 47.1% of patients at Week 1, 66.3% of patients at Week 2, and 86.3% of patients at Week 5, after treatment with AXS-05.
- Improvement in Alzheimer’s disease agitation, assessed using the caregiver rated PGI-C, was achieved by 51.2% of patients at Week 1, 67.5% of patients at Week 2, and 89.3% of patients at Week 5, after treatment with AXS-05.
- Caregiver distress, assessed using the NPI Agitation and Aggression Caregiver Distress score, was significantly reduced after treatment with AXS-05 (p<0.001, at Weeks 4 and 8).
- Caregiver burden, assessed using the ZBI, was significantly reduced after treatment with AXS-05 (p=0.006 at Week 4, p=0.003 at Week 8).
- Patient quality of life, assessed using the caregiver rated QoL-AD scale, was significantly improved after treatment with AXS-05 (p<0.001 at Week 4, p=0.013 at Week 8).
- Depressive symptoms, assessed using the CSDD, were significantly reduced after treatment with AXS-05 (p<0.001, at Weeks 4 and 8).
Double-blind Period Results Summary
A total of 108 patients were randomized, 53 to continued treatment with AXS-05, and 55 switched to placebo. The mean CMAI total scores at randomization were 43.7 and 44.9 for the AXS-05 and placebo groups respectively.
- AXS-05 met the primary endpoint by substantially and statistically significantly delaying the time to relapse of Alzheimer’s disease agitation as compared to placebo (hazard ratio for time to relapse of 0.275, p=0.014), demonstrating a 3.6-fold lower risk of relapse compared to placebo.
- AXS-05 met the key secondary endpoint by preventing relapse of Alzheimer’s disease agitation as compared to placebo, with 7.5% of AXS-05 patients relapsing versus 25.9% of patients switched to placebo (p=0.018).
- The rates of adverse events in the double-blind period were 28.3% in the AXS-05 group and 22.2% in the placebo group. Discontinuations in the double-blind period due to adverse events were low (0% for AXS-05 and 1.9% for placebo).
About the ACCORD Study
ACCORD (Assessing Clinical Outcomes in Alzheimer’s Disease Agitation) was a Phase 3, randomized, double-blind, placebo-controlled, multi-center trial to evaluate efficacy and safety of AXS-05 in patients with Alzheimer’s disease (AD) agitation. Patients with a diagnosis of probable Alzheimer’s disease and clinically meaningful agitation associated with their disease were enrolled into a 9-week, open-label period, during which they were treated with AXS-05 and monitored for a sustained clinical response. Sustained clinical response was defined as a ≥30% improvement from baseline in the Cohen-Mansfield Agitation Inventory (CMAI) total score and improvement on the PGI-C (score of ≤3) that are both maintained for at least 4 consecutive weeks.
Patients who experienced a sustained clinical response during the open-label treatment period were then randomized in a 1:1 ratio, to continue treatment with AXS-05 or to switch to placebo treatment, in a double-blind fashion for up to 26 weeks. Treatment was continued until either a relapse of agitation symptoms or the end of the 26-week double-blind period, whichever occurred first. Relapse was defined as a ≥10-point worsening in the CMAI total score from randomization or a CMAI total score greater than that at study entry; or hospitalization or other institutionalization due to agitation associated with Alzheimer’s disease.
A total of 178 patients were enrolled into the open-label period and treated with AXS-05, and 108 patients were randomized to continue on AXS-05 (n=53) or to switch to placebo (n=55). The mean Cohen-Mansfield Agitation Inventory (CMAI) total score at baseline study entry was 70.9. The mean CMAI total scores at randomization were 43.7 (AXS-05) and 44.9 (placebo). The minimum score on the CMAI is 29, corresponding to the total absence of symptoms, with higher scores corresponding to greater agitation. The primary endpoint in the study was time from randomization to relapse of Alzheimer’s disease agitation calculated by the Kaplan-Meier estimates and the hazard ratio. The key secondary endpoint, to assess relapse prevention, was the percentage of patients who relapsed. The primary timepoint for open-label efficacy assessments was Week 5 and the key secondary timepoint was Week 2. P-values for the open-label period were calculated versus baseline.
About AXS-05
AXS-05 (dextromethorphan-bupropion) is a novel, oral, patent protected, investigational N-methyl-D-aspartate (NMDA) receptor antagonist with multimodal activity under development for the treatment of Alzheimer’s disease (AD) agitation and other central nervous system (CNS) disorders. AXS-05 utilizes a proprietary formulation and dose of dextromethorphan and bupropion, and Axsome’s metabolic inhibition technology, to modulate the delivery of the components. The dextromethorphan component of AXS-05 is an uncompetitive NMDA receptor antagonist, also known as a glutamate receptor modulator, and a sigma-1 receptor agonist. The bupropion component of AXS-05 serves to increase the bioavailability of dextromethorphan, and is a norepinephrine and dopamine reuptake inhibitor. AXS-05 is covered by a robust patent estate extending out at least to 2037-2040. AXS-05 was granted FDA Breakthrough Therapy designation for the treatment of Alzheimer’s disease agitation in June 2020. AXS-05 is not approved by the FDA for the treatment of AD agitation.
About Axsome Therapeutics, Inc.
Axsome Therapeutics, Inc. is a biopharmaceutical company developing and delivering novel therapies for central nervous system (CNS) conditions that have limited treatment options. Through development of therapeutic options with novel mechanisms of action, we are transforming the approach to treating CNS conditions. At Axsome, we are committed to developing products that meaningfully improve the lives of patients and provide new therapeutic options for physicians. For more information, please visit the Company’s website at axsome.com. The Company may occasionally disseminate material, nonpublic information on the company website.
Source: Axsome Therapeutics, Inc.
Axsome says candidate for Alzheimer’s agitation met main goal in late-stage trial
Nov. 28, 2022 7:22 AM ET
Axsome Therapeutics, Inc. (AXSM)
By: Dulan Lokuwithana,
SA News Editor3 Comments
Axsome Therapeutics (NASDAQ:AXSM) jumped ~20% pre-market Monday after the neurology-focused biopharma announced that its candidate for Alzheimer’s disease (AD) agitation AXS-05 met the main goal in a Phase 3 trial.
Axsome Therapeutics, Inc. (AXSM)
https://www.axsome.com/axs-portfolio/pipeline/about-axs-05
SRP-9001
tetravalent dengue vaccine candidate (TAK-003)
tetravalent dengue vaccine candidate (TAK-003)
Sarepta Therapeutics Announces That U.S. FDA has Accepted for Filing and Granted Priority Review for the Biologics License Application for SRP-9001, Sarepta’s Gene Therapy for the Treatment of Ambulant Individuals with Duchenne Muscular Dystrophy
11/28/22 7:00 AM EST
– Regulatory action date of May 29, 2023
– SRP-9001 would be the first gene therapy for Duchenne, a one-time treatment designed to treat the underlying cause of DMD by delivering a functional shortened dystrophin to muscle
CAMBRIDGE, Mass., Nov. 28, 2022 (GLOBE NEWSWIRE) -- Sarepta Therapeutics, Inc. (NASDAQ:SRPT), the leader in precision genetic medicine for rare diseases, today announced that the U.S. Food and Drug Administration (FDA) has accepted the Company's Biologics License Application (BLA) seeking accelerated approval of SRP-9001 (delandistrogene moxeparvovec) for the treatment of ambulant individuals with Duchenne muscular dystrophy. SRP-9001 has been granted Priority Review by the FDA, with a regulatory action date of May 29, 2023.
“We are delighted to announce that the FDA has accepted Sarepta’s BLA for SRP-9001 for filing and priority review,” said Doug Ingram, president and chief executive officer, Sarepta Therapeutics. “Duchenne is a relentlessly degenerative and invariably fatal disease, robbing children of muscle and function hourly and daily. Our BLA submission for an accelerated approval, along with the FDA’s acceptance of that BLA for filing and review, is a tremendously important milestone in our effort to bring a potentially life-changing gene therapy to Duchenne patients as rapidly as possible and we look forward to working with the FDA through the review process.”
SRP-9001 is an investigational gene therapy for Duchenne being developed in partnership with Roche. Duchenne is characterized by a mutation in the dystrophin gene that results in the lack of dystrophin, which acts as a shock absorber for muscle at the membrane. SRP-9001 is designed to treat the proximate cause of Duchenne by delivering to muscle a gene that codes for a shortened, functional form of dystrophin. In addition to a wealth of pre-clinical evidence, the BLA for SRP-9001 included efficacy and safety data from Study SRP-9001-103 (also known as ENDEAVOR), as well as from Studies SRP-9001-101 and SRP-9001-102, and an integrated analysis across these three clinical studies comparing functional results to a propensity-score-weighted external control (EC). In clinical results from more than 80 treated patients, SRP-9001 has demonstrated positive results at multiple time points, including one-, two- and up to four-years after treatment, in addition to demonstrating a consistent safety profile.
In addition to Studies SRP-9001-101, SRP-9001-102 and SRP-9001-103, SRP-9001 is also being studied in EMBARK (Study SRP-9001-301), a global, randomized, double-blind, placebo-controlled clinical trial of SRP-9001 which has recruited 125 participants with Duchenne between the ages of 4 to 7. EMBARK is fully enrolled with results expected by the end of 2023. Sarepta has proposed EMBARK as the post-marketing confirmatory trial for SRP-9001.
About SRP-9001 (delandistrogene moxeparvovec)
SRP-9001 (delandistrogene moxeparvovec) is an investigational gene transfer therapy intended to deliver SRP-9001 to muscle tissue for the targeted production of functional components of dystrophin. Sarepta is responsible for global development and manufacturing for SRP-9001 and plans to commercialize SRP-9001 in the United States upon receiving FDA approval. In December 2019, Roche partnered with Sarepta to combine Roche’s global reach, commercial presence and regulatory expertise with Sarepta’s gene therapy candidate for Duchenne to accelerate access to SRP-9001 for patients outside the United States.
About Sarepta Therapeutics
Sarepta is on an urgent mission: engineer precision genetic medicine for rare diseases that devastate lives and cut futures short. We hold leadership positions in Duchenne muscular dystrophy (DMD) and limb-girdle muscular dystrophies (LGMDs), and we currently have more than 40 programs in various stages of development. Our vast pipeline is driven by our multi-platform Precision Genetic Medicine Engine in gene therapy, RNA and gene editing. For more information, please visit www.sarepta.com or follow us on Twitter, LinkedIn, Instagram and Facebook.
Sarepta/Roche gene therapy for Duchenne gets FDA priority review
Nov. 28, 2022 7:43 AM ET
Sarepta Therapeutics, Inc. (SRPT), RHHBY, RHHBF
By: Dulan Lokuwithana, SA News Editor
- Sarepta Therapeutics (NASDAQ:SRPT) announced Monday that the FDA accepted its marketing application for gene therapy candidate SRP-9001 it develops with Roche (OTCQX:RHHBY) (OTCQX:RHHBF) under the agency’s priority review.
- https://seekingalpha.com/news/3911535-sareptaroche-gene-therapy-for-duchenne-gets-fda-priority-review
- Sarepta Therapeutics, Inc. (SRPT), RHHBY, RHHBF
- https://www.sarepta.com/products-pipeline/pipeline
tetravalent dengue vaccine candidate (TAK-003)
tetravalent dengue vaccine candidate (TAK-003)
tetravalent dengue vaccine candidate (TAK-003)
Takeda’s Biologics License Application (BLA) for Dengue Vaccine Candidate (TAK-003) Granted Priority Review by U.S. Food and Drug Administration
November 22, 2022
- TAK-003 is Being Evaluated for the Prevention of Dengue Disease Caused by Any Dengue Virus Serotype in Individuals 4 Years Through 60 Years of Age
OSAKA, Japan and CAMBRIDGE, Massachusetts, November 22, 2022 – Takeda (TSE:4502/NYSE:TAK) today announced that the U.S. Food and Drug Administration (FDA) has accepted and granted priority review of the Biologics License Application (BLA) for TAK-003, the company’s investigational dengue vaccine candidate. In the U.S., TAK-003 is being evaluated for the prevention of dengue disease caused by any dengue virus serotype in individuals 4 years through 60 years of age.
Dengue is a mosquito-borne virus endemic in more than 125 countries, including the U.S. territories of Puerto Rico, the U.S. Virgin Islands and American Samoa.1,2 Incidence of dengue has increased globally over the past two decades and is a leading cause of fever among travelers returning from Latin America, the Caribbean and Southeast Asia.3
“If approved, we believe TAK-003 has the potential to become an important dengue prevention option for healthcare providers, and we continue to be encouraged by our discussions with the FDA,” said Gary Dubin, M.D., president of the Global Vaccine Business Unit at Takeda. “This year, of the 888 dengue infections in the U.S., 96% were a result of travel to dengue endemic areas. Of the 316 dengue infections in U.S. endemic territories, 97% were locally transmitted.4 At Takeda, we are guided by our commitment to serving these affected populations and are fully committed to working with the FDA to advance this filing.”
The TAK-003 BLA is supported by safety and efficacy data from the pivotal Phase 3 Tetravalent Immunization against Dengue Efficacy Study (TIDES) trial, where the dengue vaccine candidate met its primary endpoint by preventing 80.2% of symptomatic dengue cases at 12 months.5,6 In addition, TAK-003 met its secondary endpoint by preventing 90.4% of hospitalizations at 18 months, and in an exploratory analysis, it demonstrated protection against dengue fever through 4.5 years (54 months) after vaccination. The TIDES exploratory analyses showed that throughout the 4.5-year study follow-up, TAK-003 prevented 84% of hospitalized dengue cases and 61% of symptomatic dengue cases in the overall population, including both seropositive and seronegative individuals.
Currently, TAK-003 has not been approved by the FDA or any other health authority outside of Indonesia. Following the approval of TAK-003 in Indonesia, Takeda will continue to progress regulatory filings in other dengue-endemic and non-endemic countries. In October 2022, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) recommended the approval of Takeda’s dengue vaccine candidate, TAK-003, for the prevention of dengue disease caused by any serotype in individuals four years of age and older in Europe and in dengue-endemic countries participating in the parallel EU-M4all procedure. The final step in the path to approval in Europe is a Marketing Authorization decision from the EMA, which is expected in the coming months. Regulatory reviews will also progress in dengue-endemic countries in Latin America and Asia.
About TAK-003
Takeda's tetravalent dengue vaccine candidate (TAK-003) is based on a live-attenuated dengue serotype 2 virus, which provides the genetic “backbone” for all four vaccine viruses.7 Clinical Phase 2 data in children and adolescents showed that TAK-003 induced immune responses against all four dengue serotypes, in both seropositive and seronegative participants, which persisted through 48 months after vaccination.8 The pivotal Phase 3 TIDES trial met its primary endpoint of overall vaccine efficacy (VE) against virologically confirmed dengue (VCD) at 12 months follow-up and all secondary endpoints at 18 months follow-up for which there were a sufficient number of dengue cases, including VE against hospitalized dengue and VE in baseline seropositive and baseline seronegative individuals. Safety results from the studies' integrated analysis showed that the rates of Serious Adverse Events (SAEs) were 6.21% in the TAK-003 Group, and 7.56% in the Placebo Group.9 Most frequent unsolicited AEs were nasopharyngitis, upper respiratory tract infection, viral upper respiratory tract infection, viral infection, and pyrexia.
About the Phase 3 TIDES (DEN-301) Trial
The double-blind, randomized, placebo-controlled Phase 3 TIDES trial is evaluating the safety and efficacy of two doses of TAK-003 in the prevention of laboratory-confirmed symptomatic dengue fever of any severity and due to any of the four dengue virus serotypes in children and adolescents.10 Study participants were randomized 2:1 to receive two doses of TAK-003 0.5 mL or placebo on months 0 and 3, administered subcutaneously. The study is comprised of five parts. Part 1 and the primary endpoint analysis evaluated vaccine efficacy (VE) and safety through 12 months after the second dose. Part 2 continued for an additional six months to complete the assessment of the secondary endpoints of VE by serotype, baseline serostatus and disease severity, including VE against hospitalized dengue. Part 3 evaluated VE and long-term safety by following participants for an additional two and a half to three years, as per World Health Organization (WHO) recommendations.5 Part 4 will evaluate efficacy and safety for 13 months following booster vaccination, and Part 5 will evaluate long-term efficacy and safety for one year after completion of Part 4.
The trial is taking place at sites in dengue-endemic areas in Latin America (Brazil, Colombia, Panama, the Dominican Republic and Nicaragua) and Asia (Philippines, Thailand and Sri Lanka) where there are unmet needs in dengue prevention and where severe dengue is a leading cause of serious illness and death among children.5 Baseline blood samples were collected from all individuals participating in the trial to allow for evaluation of safety and efficacy based on serostatus. Takeda and an independent Data Monitoring Committee of experts are actively monitoring safety on an ongoing basis.
About Takeda
Takeda is a global, values-based, R&D-driven biopharmaceutical leader headquartered in Japan, committed to discover and deliver life-transforming treatments, guided by our commitment to patients, our people and the planet. Takeda focuses its R&D efforts on four therapeutic areas: Oncology, Rare Genetics and Hematology, Neuroscience, and Gastroenterology (GI). We also make targeted R&D investments in Plasma-Derived Therapies and Vaccines. We are focusing on developing highly innovative medicines that contribute to making a difference in people’s lives by advancing the frontier of new treatment options and leveraging our enhanced collaborative R&D engine and capabilities to create a robust, modality-diverse pipeline. Our employees are committed to improving quality of life for patients and to working with our partners in health care in approximately 80 countries and regions. For more information, visit https://www.takeda.com.
Takeda dengue vaccine gets FDA priority review
Nov. 23, 2022 7:16 AM ET
Takeda Pharmaceutical Company Limited (TAK)
By: Dulan Lokuwithana, SA News Editor
- Takeda (NYSE:TAK) announced that the U.S. Food and Drug Administration (FDA) accepted and granted the priority review for the Biologics License Application (BLA) it submitted for the investigational dengue vaccine candidate TAK-003.
- A live-attenuated vaccine, TAK-003, is currently undergoing the FDA review for the prevention of dengue disease in those aged 4 - 60 years.
- https://seekingalpha.com/news/3910929-takeda-dengue-vaccine-gets-fda-priority-review
- Takeda Pharmaceutical Company Limited (TAK)
- https://www.takeda.com/what-we-do/research-and-development/our-pipeline/
- https://www.takeda.com/
ARV-471
tetravalent dengue vaccine candidate (TAK-003)
Epcoritamab (DuoBody®-CD3xCD20)
Arvinas Announces ARV-471 Achieves a Clinical Benefit Rate of 38% in Evaluable Patients and Continues to Show a Favorable Tolerability Profile in its Phase 2 Expansion Trial (VERITAC)
November 22, 2022
ARV-471 continues to show activity in heavily pre-treated patients with locally advanced or metastatic ER+/HER2- breast cancer
Median progression free survival of 3.7 months in all patients and 5.7 months in patients with ESR1 mutant tumors support the initiation of two Phase 3 registrational trials
NEW HAVEN, Conn., Nov. 22, 2022 (GLOBE NEWSWIRE) -- Arvinas, Inc. (Nasdaq: ARVN) today announced initial results from the Phase 2 cohort expansion portion (VERITAC) of a phase 1/2 study with ARV-471, a novel PROTAC® estrogen receptor (ER) protein degrader. ARV-471 is being co-developed with Pfizer Inc. (NYSE: PFE) for the treatment of patients with locally advanced or metastatic ER positive / human epidermal growth factor receptor 2 (HER2) negative (ER+/HER2-) breast cancer.
This disclosure was originally planned for December 8, 2022. However, on November 21, 2022, the 2022 San Antonio Breast Cancer Symposium (SABCS) incorrectly published the abstract, omitting a key safety data table, and inadvertently released the corresponding full data presentation on the SABCS website. These full data are scheduled to be presented on December 8, 2022 at 9:00 a.m. CT in an oral presentation titled “ARV-471, a PROTAC® estrogen receptor (ER) degrader in advanced ER-positive/human epidermal growth factor receptor 2 (HER2)-negative breast cancer: phase 2 expansion (VERITAC) of a phase 1/2 study.”
As a result of the early release of the full data presentation, Arvinas will host a conference call and webcast today, November 22, 2022, at 4:30 p.m. ET to discuss these data. Those wishing to examine the data in more detail are welcome to access our 8K filed last evening located here.
In the VERITAC trial, ARV-471 shows a favorable tolerability profile and demonstrates a clinical benefit rate of 38% (total n=71) (CBR: rate of confirmed complete response, confirmed partial response, or stable disease > 24 weeks), the primary endpoint in the trial. These results are consistent with the Phase 1 portion of this trial.
Patients in VERITAC had a median of four lines of prior therapies, in a population where 100% of patients were treated with prior cyclin-dependent kinase (CDK4/6) inhibitors, 79% with prior fulvestrant, and 73% with prior chemotherapy.
At the time of data cutoff (June 6, 2022), ARV-471 administered at 200 mg (n=35) and 500 mg (n=36) demonstrated:
- Antitumor activity in 100% CDK4/6 inhibitor-pretreated patients, as measured by a CBR of 38% (total n=71) in all patients and 51.2% in patients with mutant ESR1 tumors (n=41).
- Preliminary median progression-free survival (mPFS) of 3.7 months, a key secondary endpoint, in all evaluable patients and 5.7 months in patients with mutant ESR1 tumors (n=41).
- A favorable tolerability profile, with the majority of treatment-related adverse events (TRAEs) reported as Grade 1 or 2.
“I’m gratified to see the continued differentiated profile of ARV-471 and its potential to become an important new standard of care for patients with ER+/HER2- breast cancer,” said John Houston, Ph.D., President and Chief Executive Officer at Arvinas. “The positive VERITAC results, in a heavily pre-treated population in which 100% of the patients received at least one prior CDK4/6 inhibitor and many who had progressed on or after chemotherapy, and fulvestrant, reinforce our confidence in ARV-471 as we prepare to initiate two pivotal trials, with the goal of working to give patients and physicians a potential new option in the fight against breast cancer.”
“These data validate the early data which led us to enter into the collaboration with Arvinas and give us the confidence needed to initiate two Phase 3 registrational trials," said Chris Boshoff, M.D., Ph.D., Chief Development Officer, Oncology and Rare Disease, Pfizer Global Product Development.
ARV-471 Clinical Update
Study Design
VERITAC is the Phase 2 cohort expansion portion of a Phase 1/2 single-arm trial of ARV-471 alone and in combination with palbociclib in patients with ER+/HER2- locally advanced or metastatic breast cancer (mBC) (NCT04072952). In VERITAC, patients were treated with either 200 mg or 500 mg ARV-471 with a primary endpoint of CBR (CR, PR or SD > 24 weeks). Secondary endpoints include ORR, DOR, PFS and OS as well as safety (AEs) and pharmacokinetics.
Enrollment
As of the data cut-off date of June 6, 2022, 71 patients with locally advanced or metastatic ER+/HER2- breast cancer in the VERITAC expansion cohort were treated once-daily with oral doses of ARV-471 at 200 mg (n=35) or 500 mg (n=36).
- 100% of patients were previously treated with CDK 4/6 inhibitors
- 79% of patients were previously treated with fulvestrant
- 73% of patients were previously treated with chemotherapy
- 45% received chemotherapy in the metastatic setting
Efficacy Data
Clinical benefit rate (the primary endpoint, defined as a confirmed complete response, partial response, or stable disease ≥ 24 weeks) in all patients (n=71) and in patients with tumors harboring ESR1 mutations (n=41):
- All patients (200 mg and 500 mg, n=71): 38%
- Patients with tumors harboring ESR1 mutations (n=41): 51.2%
- Patients with ESR1 wild-type tumors (n=25): 20%
- All patients at 200 mg (n=35): 37.1%
- Patients with tumors harboring ESR1 mutations (n=19): 47%
- All patients at 500 mg (n=36): 39%
- Patients with tumors harboring ESR1 mutations (n=22): 55%
Progression free survival
- All patients receiving 200 mg or 500 mg qd ARV-471 (n=71): median 3.7 months
- Patients with mutant ESR1 tumors (n=41): median 5.7 months
- Patients receiving 200 mg qd ARV-471 (n=35): median 3.5 months
- Patients with mutant ESR1 tumors (n=19): median 5.5 months
- At the time of the data cutoff, data for 500 mg cohort were immature and therefore not included in a separate analysis
About ARV-471
ARV-471 is an investigational, orally-bioavailable PROTAC® protein degrader designed to specifically target and degrade the estrogen receptor (ER) for the treatment of patients with locally advanced or metastatic ER+/HER2- breast cancer.
In preclinical studies, ARV-471 demonstrated near-complete ER degradation in tumor cells, induced robust tumor shrinkage when dosed as a single agent in multiple ER-driven xenograft models, and showed superior anti-tumor activity when compared to a standard of care agent, fulvestrant, both as a single agent and in combination with a CDK4/6 inhibitor. In July 2021, Arvinas announced a global collaboration with Pfizer for the co-development and co-commercialization of ARV-471; Arvinas and Pfizer will equally share worldwide development costs, commercialization expenses, and profits.
About Arvinas
Arvinas is a clinical-stage biotechnology company dedicated to improving the lives of patients suffering from debilitating and life-threatening diseases through the discovery, development, and commercialization of therapies that degrade disease-causing proteins. Arvinas uses its proprietary PROTAC® Discovery Engine platform to engineer proteolysis targeting chimeras, or PROTAC® targeted protein degraders, that are designed to harness the body’s own natural protein disposal system to selectively and efficiently degrade and remove disease-causing proteins. In addition to its robust preclinical pipeline of PROTAC® protein degraders against validated and “undruggable” targets, the company has three investigational clinical-stage programs: bavdegalutamide (ARV-110) and ARV-766 for the treatment of men with metastatic castration-resistant prostate cancer; and ARV-471 for the treatment of patients with locally advanced or metastatic ER+/HER2- breast cancer. For more information, visit www.arvinas.com.
Pfizer, Arvinas breast cancer therapy hits 38% clinical benefit in Phase 2 trial
Nov. 22, 2022 8:17 AM ET
By: Dulan Lokuwithana, SA News Editor
Arvinas, Inc (NASDAQ:ARVN) announced Tuesday early results from its Phase 2 cohort expansion portion of a Phase 1/2 study for protein degrader ARV-471 it co-develops with Pfizer (NYSE:PFE), indicating a clinical benefit rate of 38% among breast cancer patients.
https://clinicaltrials.gov/ct2/show/NCT04072952
https://www.arvinas.com/research-and-development/
Epcoritamab (DuoBody®-CD3xCD20)
ELAHERE™ (mirvetuximab soravtansine-gynx)
Epcoritamab (DuoBody®-CD3xCD20)
Genmab Announces U.S. Food and Drug Administration Accepts for Priority Review Biologics License Application (BLA) for Epcoritamab (DuoBody®-CD3xCD20) for the Treatment of Relapsed/Refractory Large B-Cell Lymphoma (LBCL)
Nov 21, 2022 at 2:00 PM CET
Media Release
COPENHAGEN, Denmark; November 21, 2022
- Epcoritamab BLA accepted for FDA Priority review; FDA action date is May 21, 2023
- Epcoritamab could become the first subcutaneous bispecific antibody approved for the treatment of LBCL
- BLA submission supported by positive EPCORE™ NHL-1 trial results
Genmab A/S (Nasdaq: GMAB) today announced that the U.S. Food and Drug Administration (FDA) has accepted for Priority Review the Biologics License Application (BLA) for subcutaneous epcoritamab (DuoBody®-CD3xCD20), an investigational bispecific antibody, for the treatment of patients with relapsed/refractory large B-cell lymphoma (LBCL) after two or more lines of systemic therapy. Under the Prescription Drug User Fee Act (PDUFA), the FDA has set a target action date of May 21, 2023.
The BLA submission is based on safety and preliminary efficacy data from the LBCL cohort of the pivotal EPCORE™ NHL-1 open-label, multi-center phase 2 clinical trial evaluating epcoritamab in patients with relapsed, progressive or refractory CD20+ mature B-cell non-Hodgkin lymphoma (B-NHL). These results were presented in a late-breaking oral presentation as a part of the Presidential Symposium at the 27th Annual Meeting of the European Hematology Association (EHA2022), in Vienna, Austria.
“We are pleased that the BLA for epcoritamab has been accepted for Priority Review by the FDA, accelerating the pathway for approval and bringing us one step closer to potentially delivering a novel treatment option to relapsed and refractory LBCL patients who are in need of additional treatment options,” said Jan van de Winkel, Ph.D., Chief Executive Officer of Genmab. “Together with our partner, AbbVie, we recognize the unmet need for safe, effective and accessible treatments for patients with B-cell malignancies and we believe that epcoritamab has the potential to become a core therapy in this patient population.”
Epcoritamab is being co-developed by Genmab and AbbVie as part of the companies' oncology collaboration. The companies will share commercial responsibilities in the U.S. and Japan, with AbbVie responsible for further global commercialization. The companies are committed to evaluating epcoritamab as a monotherapy, and in combination, across lines of therapy in a range of hematologic malignancies, including an ongoing phase 3, open-label, randomized clinical trial evaluating epcoritamab as a monotherapy in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) (NCT: 04628494) and a phase 3, open-label clinical trial evaluating epcoritamab in combination in patients with relapsed/refractory follicular lymphoma (FL) (NCT: 05409066).
In October 2022, the European Medicines Agency validated for review a Marketing Authorization Application (MAA) for epcoritamab for the treatment of patients with relapsed/refractory DLBCL– a major subtype of LBCL – after two or more lines of systemic therapy.
Based on the existing agreement, this milestone triggers a USD 80 million milestone payment from AbbVie. The milestone payment will not impact Genmab’s 2022 financial guidance provided on November 9, 2022.
About the EPCORE™ NHL-1 Trial
EPCORE™ NHL-1 is an open-label, multi-center safety and preliminary efficacy trial of epcoritamab including a phase 1 first-in-human, dose escalation part; a phase 2 expansion part; and an optimization part. The trial was designed to evaluate subcutaneous epcoritamab in patients with relapsed, progressive or refractory CD20+ mature B-NHL, including LBCL and DLBCL. Data from the dose escalation part of the study, which determined the recommended phase 2 dose, were published in The Lancet in 2021. In the phase 2 expansion part, additional patients are treated with epcoritamab to further explore the safety and efficacy of epcoritamab in patients with different types of relapsed/refractory B-NHLs who had limited therapeutic options.
The primary endpoint of the phase 2 expansion part was overall response rate (ORR) as assessed by an IRC. Secondary efficacy endpoints included duration of response, complete response rate, progression-free survival, overall survival, time to response, time to next therapy, and rate of minimal residual disease negativity.
About Epcoritamab
Epcoritamab is an investigational IgG1-bispecific antibody created using Genmab's proprietary DuoBody technology. Genmab's DuoBody-CD3 technology is designed to direct cytotoxic T cells selectively to elicit an immune response towards target cell types. Epcoritamab is designed to simultaneously bind to CD3 on T cells and CD20 on B-cells and induces T cell mediated killing of CD20+ cells.4 CD20 is expressed on B-cells and a clinically validated therapeutic target in many B-cell malignancies, including diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma and chronic lymphocytic leukemia.5,6
About Genmab
Genmab is an international biotechnology company with a core purpose to improve the lives of people with cancer. For more than 20 years, Genmab’s vision to transform cancer treatment has driven its passionate, innovative and collaborative teams to invent next-generation antibody technology platforms and leverage translational research and data sciences, fueling multiple differentiated cancer treatments that make an impact on people’s lives. To develop and deliver novel therapies to patients, Genmab has formed 20+ strategic partnerships with biotechnology and pharmaceutical companies. Genmab’s proprietary pipeline includes bispecific T-cell engagers, next-generation immune checkpoint modulators, effector function enhanced antibodies and antibody-drug conjugates.
Genmab is headquartered in Copenhagen, Denmark with locations in Utrecht, the Netherlands, Princeton, New Jersey, U.S. and Tokyo, Japan. For more information, please visit Genmab.com and follow us on Twitter.com/Genmab.
GENMAB_FDA Submission Acceptance Release_FINAL
AbbVie, Genmab lymphoma therapy goes under FDA priority review
Nov. 21, 2022 9:29 AM ET
By: Dulan Lokuwithana, SA News Editor
- Danish biotech Genmab A/S (GMAB) announced Monday that the U.S. FDA accepted its marketing application and granted priority review for lymphoma therapy epcoritamab, a bispecific antibody it co-develops with AbbVie (NYSE:ABBV).
- https://seekingalpha.com/pr/19029717-genmab-announces-u-s-food-and-drug-administration-accepts-for-priority-review-biologics
- Genmab A/S (GMAB), ABBV
- https://www.genmab.com/research-innovation/antibody-technology-platforms/
- https://www.genmab.com/
INBRX-109
ELAHERE™ (mirvetuximab soravtansine-gynx)
ELAHERE™ (mirvetuximab soravtansine-gynx)
Inhibrx Announces Updated Efficacy and Safety Data from the Expansion Cohorts in the Phase 1 Trial of INBRX-109 for the Treatment of Chondrosarcoma
SAN DIEGO, Nov. 16, 2022 /
PRNewswire/ -- Inhibrx, Inc. (Nasdaq: INBX), a clinical-stage biopharmaceutical company dedicated to the development of therapeutics for oncology and rare diseases, today announced updated efficacy and safety data from the ongoing Phase 1 INBRX-109 expansion cohorts for the treatment of chondrosarcoma. Inhibrx presented this dataset as of May 2022 at the Annual Connective Tissue Oncology Society (CTOS) Conference today, which included matured data on the original chondrosarcoma cohort and initial data from an additional cohort of chondrosarcoma patients with the isocitrate dehydrogenase (IDH) mutation. Additionally, Inhibrx announced further updated results from this dataset as of November 2022.
Among the 33 patients evaluable as of November 8, 2022, the observed disease control rate was 87.9%, or 29 out of 33 patients as measured by RECISTv1.1, with two patients achieving partial responses (6.1%) and 27 patients achieving stable disease (81.8%). Disease control was observed in patients with and without IDH1/IDH2 mutations. Of those achieving stable disease 55.6% had decreases from baseline in tumor size. Clinical benefit was durable, 14 of 33 patients (42.4%) who achieved disease control had a clinical benefit lasting greater than 6 months, and the longest duration of stable disease is 20 months. To date, the median progression-free survival (PFS) is 7.6 months, and five patients remain on study.
Treatment-related adverse events (AEs) were reported in less than 5% of the patients with the most common being increased alanine aminotransferase (ALT), increased aspartate aminotransferase (AST), and increased blood bilirubin and fatigue. There were no grade 4 or 5 events reported among patients with treatment-related AEs.
About INBRX-109
INBRX-109 is a precision-engineered, tetravalent death receptor 5 (DR5) agonist antibody designed to exploit the tumor-biased cell death induced by DR5 activation.
In 2021, the FDA granted Fast Track designation to INBRX-109 for the treatment of patients with unresectable or metastatic conventional chondrosarcoma and orphan-drug designation to INBRX-109 for chondrosarcoma in the United States.
In June 2021, Inhibrx initiated a randomized, blinded, placebo-controlled, potential registration-enabling Phase 2 trial of INBRX-109 in conventional chondrosarcoma, which is currently ongoing.
About Inhibrx, Inc.
Inhibrx is a clinical-stage biotechnology company focused on developing a broad pipeline of novel biologic therapeutic candidates in oncology and orphan diseases. Inhibrx utilizes diverse methods of protein engineering to address the specific requirements of complex target and disease biology, including its proprietary sdAb platform. Inhibrx has collaborations with 2seventy bio (formerly bluebird bio), Bristol-Myers Squibb and Chiesi, among others. For more information, please visit www.inhibrx.com.
SOURCE Inhibrx Inc.
Inhibrx's drug for rare bone cancer shows promise in ongoing phase 1 study
Nov. 16, 2022 9:37 AM ET
By: Ravikash, SA News Editor
Inhibrx (NASDAQ:INBX) on Wednesday reported updated data from an ongoing phase 1 trial of INBRX-109 expansion groups to treat chondrosarcoma.
https://inhibrx.com/inbrx-109/
ELAHERE™ (mirvetuximab soravtansine-gynx)
ELAHERE™ (mirvetuximab soravtansine-gynx)
ELAHERE™ (mirvetuximab soravtansine-gynx)
ImmunoGen Announces FDA Accelerated Approval of ELAHERE™ (mirvetuximab soravtansine-gynx) for the Treatment of Platinum-Resistant Ovarian Cancer
November 14, 2022 at 4:30 PM EST
ELAHERE is the First ADC Approved by FDA for Platinum-Resistant Ovarian Cancer
Indication Covers Patients with One to Three Prior Systemic Treatment Regimens, Regardless of Prior Avastin® Use
VENTANA FOLR1 (FOLR1-2.1) RxDx Assay, the Companion Diagnostic to Identify Ovarian Cancer Patients Eligible for ELAHERE, Contemporaneously Approved by FDA
Approval Transitions ImmunoGen to a Fully-Integrated Oncology Company
Conference Call to be Held Tomorrow at 8:00 AM ET
WALTHAM, Mass.--(BUSINESS WIRE)--Nov. 14, 2022-- ImmunoGen Inc. (Nasdaq: IMGN), a leader in the expanding field of antibody-drug conjugates (ADCs) for the treatment of cancer, today announced that the US Food and Drug Administration (FDA) has granted accelerated approval for ELAHERE™ (mirvetuximab soravtansine-gynx) for the treatment of adult patients with folate receptor alpha (FRα)-positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer, who have received one to three prior systemic treatment regimens. ELAHERE was approved under FDA's accelerated approval program based on objective response rate (ORR) and duration of response (DOR) data from the pivotal SORAYA trial. Continued approval may be contingent upon verification and description of clinical benefit in a confirmatory trial. ELAHERE is a first-in-class ADC directed against FRα, a cell-surface protein highly expressed in ovarian cancer, and is the first FDA approved ADC for platinum-resistant disease.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20221104005657/en/
"The approval of ELAHERE is significant for patients with FRα-positive platinum-resistant ovarian cancer, which is characterized by limited treatment options and poor outcomes," said Ursula Matulonis, MD, Chief of the Division of Gynecologic Oncology at the Dana-Farber Cancer Institute, Professor of Medicine at the Harvard Medical School, and SORAYA Co-Principal Investigator. “ELAHERE’s impressive anti-tumor activity, durability of response, and overall tolerability observed in SORAYA demonstrate the benefit of this new therapeutic option, and I look forward to treating patients with ELAHERE."
"With an indication for use regardless of prior treatment with Avastin, we believe ELAHERE is positioned to become the new standard of care for patients with FRα-positive platinum-resistant ovarian cancer,” said Mark Enyedy, ImmunoGen’s President and Chief Executive Officer. “ELAHERE’s accelerated approval is a testament to the decades of work dedicated to developing the next generation of ADCs and marks ImmunoGen’s transition to a fully-integrated oncology company and the start of an exciting new chapter for us as a leader in the development and commercialization of innovative oncology products. With a highly experienced commercial and medical team in place, we are well prepared to support a successful launch and deliver ELAHERE rapidly to patients across the US."
ELAHERE was evaluated in the pivotal SORAYA trial, a single-arm study in 106 patients with platinum-resistant ovarian cancer whose tumors expressed high levels of FRα and who had been treated with one to three prior systemic treatment regimens – at least one of which included Avastin® (bevacizumab). The primary endpoint was confirmed ORR as assessed by investigator and the key secondary endpoint was DOR. Per the label, ELAHERE demonstrated an ORR by investigator of 31.7% (95% confidence interval [CI]: 22.9, 41.6), including five complete responses (CRs). The median DOR was 6.9 months (95% CI: 5.6, 9.7) as assessed by investigator. The safety of ELAHERE has been evaluated in a pooled analysis from three studies among a total of 464 patients with FRα-positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer who received at least one dose of ELAHERE (6 mg/kg adjusted ideal body weight (AIBW) administered intravenously once every 3 weeks).
The prescribing information for ELAHERE includes a boxed warning for ocular toxicity, including visual impairment, keratopathy, dry eye, photophobia, eye pain, and uveitis. The most common adverse reactions (greater than or equal to 20% of patients), including laboratory abnormalities, were vision impairment, fatigue, increased aspartate aminotransferase, nausea, increased alanine aminotransferase, keratopathy, abdominal pain, decreased lymphocytes, peripheral neuropathy, diarrhea, decreased albumin, constipation, increased alkaline phosphatase, dry eye, decreased magnesium, decreased leukocytes, decreased neutrophils, and decreased hemoglobin.
"Platinum-resistant ovarian cancer is a notoriously challenging disease to treat. Given there have been no new therapies approved by FDA for this indication since 2014, ELAHERE's accelerated approval is a tremendous advance in the ovarian cancer treatment paradigm,” said Anna Berkenblit, MD, Senior Vice President and Chief Medical Officer of ImmunoGen. “We are thrilled with today’s approval and extend our sincere thanks to the patients, families, caregivers, and investigators who helped make this achievement a reality and have supported the broader mirvetuximab development program. As we work to deliver more good days to patients, we look forward to the continued evaluation of mirvetuximab in earlier lines of treatment, in combination, and across a wider range of levels of FRα expression.”
MIRASOL, the confirmatory randomized trial designed to convert the accelerated approval of ELAHERE to full approval, is fully enrolled and top-line data are expected in early 2023. During the Biologics License Application review, FDA requested ImmunoGen submit preliminary ORR and DOR data from both arms of MIRASOL. To maintain data integrity for the ongoing MIRASOL trial, an independent third-party statistician performed the analyses and submitted the outputs directly to FDA.
FDA has also granted approval of the VENTANA FOLR1 (FOLR1-2.1) RxDx Assay, the only companion diagnostic to aid in identifying patients eligible for treatment with ELAHERE, developed by Roche. Approximately 35-40% of ovarian cancer patients express high levels of FRα, which is defined as greater than or equal to 75% tumor cells staining with 2+ intensity. Testing can be done on fresh or archived tissue; newly diagnosed patients can test at diagnosis to determine if ELAHERE will be an option for them at the time of progression to platinum resistance. Testing is now available in the US through four centralized laboratories and is expected to expand to additional laboratories over time. For the current list of US laboratories that offer testing, please visit https://usinfo.Roche.com/folr1ihc.html.
ImmunoGen is committed to helping eligible platinum-resistant ovarian cancer patients gain access to treatment with ELAHERE and is providing support through our ELAHERE Support Services program. For more information, call 1-833-ELAHERE or visit www.elahere.com.
ABOUT ELAHERE (MIRVETUXIMAB SORAVTANSINE-GYNX)
ELAHERE (mirvetuximab soravtansine-gynx) is a first-in-class ADC comprising a folate receptor alpha-binding antibody, cleavable linker, and the maytansinoid payload DM4, a potent tubulin inhibitor designed to kill the targeted cancer cells.
Indication and Usage
ELAHERE™ is indicated for the treatment of adult patients with folate receptor-alpha (FRα) positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer, who have received one to three prior systemic treatment regimens. Select patients for therapy based on an FDA-approved test.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
Please see full Prescribing Information, including Boxed Warning for ELAHERE.
ABOUT IMMUNOGEN
ImmunoGen is developing the next generation of antibody-drug conjugates (ADCs) to improve outcomes for cancer patients. By generating targeted therapies with enhanced anti-tumor activity and favorable tolerability profiles, we aim to disrupt the progression of cancer and offer our patients more good days. We call this our commitment to TARGET A BETTER NOW™.
Learn more about who we are, what we do, and how we do it at www.immunogen.com.
AVASTIN® is a trademark of Genentech, a member of the Roche Group. ELAHERE™ is a trademark of ImmunoGen, Inc.
View source version on businesswire.com: https://www.businesswire.com/news/home/20221104005657/en/
Source: ImmunoGen Inc.
ImmunoGen wins FDA approval of antibody-drug conjugate Elahere for ovarian cancer
Nov. 14, 2022 5:16 PM ET
By: Jonathan Block, SA News Editor4 Comments
- The US FDA has granted accelerated approval to ImmunoGen (NASDAQ:IMGN) for Elahere (mirvetuximab soravtansine), an antibody-drug conjugate ("ADC") for platinum-resistant ovarian cancer.
- https://seekingalpha.com/news/3907530-immunogen-wins-fda-approval-of-antibody-drug-conjugate-elahere-for-ovarian-cancer
- ImmunoGen, Inc. (IMGN)
- https://www.immunogen.com/what-we-do/our-pipeline/
biotecHOPE™ 2022
PT027
IgA Nephropathy (IgAN)
IgA Nephropathy (IgAN)
PT027 recommended by FDA Advisory Committee as new rescue treatment for asthma
PUBLISHED9 November 2022
9 November 2022 07:00 GMT
First and only rescue medication recommended for US approval that has been shown to reduce severe exacerbations
The Food and Drug Administration’s (FDA) Pulmonary-Allergy Drugs Advisory Committee (PADAC) has voted 16 to 1 that the data support a favourable benefit risk assessment for the use of PT027 (albuterol/budesonide) for the treatment of asthma in people aged 18 years and older. In adolescents aged 12 to 17 years, the Committee voted 9 to 8 that the data do not support a favourable benefit risk assessment for the use of PT027 for the treatment of asthma. In children aged 4 to 11 years, the Committee voted 16 to 1 that the data do not support a favourable benefit risk assessment for the use of PT027 for the treatment of asthma.
PT027 is a potential first-in-class, pressurised metered-dose inhaler (pMDI), fixed-dose combination rescue medication in the US containing albuterol, a short-acting beta2-agonist (SABA), and budesonide, an anti-inflammatory inhaled corticosteroid (ICS). It is being developed by AstraZeneca and Avillion.
In the first half of 2022, the FDA accepted the New Drug Application (NDA) for PT027 and set a Prescription Drug User Fee Act date for the first half of 2023.
Bradley E. Chipps, Past President of the American College of Allergy, Asthma & Immunology and Medical Director of the Capital Allergy & Respiratory Disease Center in Sacramento, US, said: “Millions of people with asthma rely on their albuterol rescue inhaler to alleviate acute symptoms, but this does not treat the underlying inflammation, leaving patients at risk of severe asthma exacerbations, regardless of their disease severity or level of control. If approved, PT027 could transform the current rescue treatment approach.”
Mene Pangalos, Executive Vice President, BioPharmaceuticals R&D, AstraZeneca, said: “We are pleased that the Pulmonary-Allergy Drugs Advisory Committee has recognised the potential for PT027 to deliver important benefits for people with asthma, as a first-in-class treatment option in the US. We look forward to working with our partner Avillion and the FDA to progress the application and discuss next steps, including for adolescents and children.”
Asthma is a chronic, inflammatory, variable respiratory disease that affects as many as 339 million people worldwide,1 including over 25 million in the US.2 Globally, more than 176 million asthma attacks are experienced each year.3
The NDA submission was based on results from the MANDALA, DENALI and TYREE Phase III trials.4-7 In MANDALA, PT027 significantly reduced the risk of severe exacerbations compared to albuterol in patients with moderate to severe asthma when used as an as-needed rescue medication in response to symptoms.4,5 In DENALI, PT027 significantly improved lung function compared to the individual components, albuterol and budesonide, in patients with mild to moderate asthma.6
The safety and tolerability of PT027 in these trials were consistent with the known profiles of the components.4-7
Results from the MANDALA trial were published in the New England Journal of Medicine in May 2022.4
PADAC reviews and evaluates available data concerning the safety and effectiveness of marketed and investigational human drug products for use in the treatment of pulmonary disease and diseases with allergic and/or immunologic mechanisms and makes appropriate recommendations to the Commissioner of Food and Drugs.
Notes
Asthma
Asthma is a chronic, inflammatory, variable respiratory disease that affects as many as 339 million adults and children worldwide,1 including over 25 million in the US.2
Patients with asthma experience recurrent breathlessness and wheezing, which varies over time, and in severity and frequency.8 These patients are at risk of severe exacerbations regardless of their disease severity, adherence to treatment or level of control.9,10
There are an estimated 176 million asthma exacerbations globally per year,3 including more than 10 million in the US;2 these are physically threatening and emotionally significant for many patients11 and can be fatal.1,12
Inflammation is central to both asthma symptoms8 and exacerbations.13 Many patients experiencing asthma symptoms use a SABA (e.g. albuterol) as a rescue medicine;14-16 however, taking a SABA alone does not address inflammation, leaving patients at risk of severe exacerbations,17 which can result in impaired quality of life,18 hospitalisation19 and frequent oral corticosteroid (OCS) use.19 Treatment of exacerbations with as few as 1-2 short courses of OCS are associated with an increased risk of adverse health conditions including type 2 diabetes, depression/anxiety, renal impairment, cataracts, cardiovascular disease, pneumonia and fracture.8,20,21 International recommendations from the Global Initiative for Asthma no longer recommend SABA alone as the preferred rescue therapy.8
MANDALA
MANDALA4,22 was a Phase III, randomised, double-blind, multicentre, parallel-group, event-driven trial evaluating the efficacy and safety of PT027 compared to albuterol on the risk of experiencing a severe asthma exacerbation in 3,132 adults, adolescents, and children (aged 4–11 years) with moderate to severe asthma taking ICS alone or in combination with a range of asthma maintenance therapies, including long-acting beta2-agonists (LABA), leukotriene receptor antagonists (LTRA), long-acting muscarinic antagonists (LAMA) or theophylline. The trial comprised a two-to-four-week screening period, at least a 24-week treatment period and a two-week post-treatment follow-up period.
Patients were randomly assigned to one of the following three treatment groups in a 1:1:1 ratio: PT027 180/160mcg (excluding children aged 4–11 years), PT027 180/80mcg or albuterol 180mcg, taken as an as-needed rescue medicine. PT027 and the albuterol comparator were delivered in a pressurised metered-dose inhaler (pMDI) using AstraZeneca’s Aerosphere delivery technology. The primary efficacy endpoint was the time to first severe asthma exacerbation during the treatment period. Secondary endpoints included severe exacerbation rate (annualised), total systemic corticosteroid exposure (annualised), asthma control and health-related quality of life.
Full results from the positive MANDALA Phase III trial showed that PT027 (albuterol/budesonide) demonstrated a statistically significant reduction in the risk of a severe exacerbation versus albuterol rescue in patients with moderate to severe asthma. Compared with albuterol rescue, PT027 at the 180mcg albuterol/160mcg budesonide dose reduced the risk of a severe exacerbation by 27% (p<0.001) in adults and adolescents.4,5
Primary and secondary endpoint results in adults and adolescents4,5
(pre-planned on-treatment efficacy analysis)
Treatment Group
Comparison versus albuterol 180mcg
Time to first severe exacerbation
n
Number (%) of Patients with a Severe Exacerbation a, b
Hazard Ratio
(95% CI)
p value (2‑sided)
PT027 180/160mcg
1013
207 (20.4)
0.73 (0.61, 0.88)
<0.001
Albuterol 180mcg
1014
266 (26.2)
Annualised severe exacerbation rate (rate ratio)
n
Number of Severe Exacerbations a, b
Annualised rate
(95% CI)
Rate Ratio
(95% CI)
PT027 180/160mcg
1013
334
0.45 (0.34, 0.60)
0.76 (0.62, 0.93)
Albuterol 180mcg
1014
413
0.59 (0.44, 0.78)
Annualised total SCS dose (mg/year)
n
Mean (SD) b
% reduction in mean
p-valuec (2-sided) c
PT027 180/160mcg
1012
86.2 (262.86)
33.4%
0.002
Albuterol 180mcg
1011
129.3 (657.19)
aDeterioration of asthma requiring use of SCS for ≥3 days, or inpatient hospitalisation, or emergency room visit, that required SCS. bBefore discontinuation of randomised treatment or change in maintenance therapy. cWilcoxon rank sum test
CI, confidence interval; SCS, systemic corticosteroid; SD, standard deviation
Primary endpoint results in adults, adolescents, and children4,5
Treatment Group
Comparison versus albuterol 180mcg
Time to first severe exacerbation
n
Number (%) of Patients with a Severe Exacerbation a, b
Hazard Ratio
(95% CI)
p value (2‑sided)
PT027 180/80mcg
1054
241 (22.9)
0.83 (0.70, 0.99)
0.041
Albuterol 180mcg
1056
276 (26.1)
aDeterioration of asthma requiring use of SCS for ≥3 days, or inpatient hospitalisation, or emergency room visit, that required SCS. bBefore discontinuation of randomised treatment or change in maintenance therapy.
CI, confidence interval
Adverse events (AEs) were similar across the treatment groups in the trial and were consistent with the known safety profiles of the individual components, with the most common AEs including nasopharyngitis and headache.4,5
DENALI
DENALI6,23,24 was a Phase III, randomised, double-blind, placebo-controlled, multicentre, parallel-group trial evaluating the efficacy and safety of PT027 compared to its components, albuterol and budesonide, on improvement in lung function in 1,001 adults, adolescents, and children aged 4–11 years with mild to moderate asthma previously treated either with SABA as-needed alone or in addition to regular low-dose ICS maintenance therapy. The trial comprised a two-to-four-week screening period, a 12-week treatment period and a two-week post-treatment follow-up period.
Patients were randomly assigned to one of the following five treatment groups in a 1:1:1:1:1 ratio: PT027 180/160mcg four times daily (excluding children aged 4–11 years), PT027 180/80mcg four times daily, albuterol 180mcg four times daily, budesonide 160mcg four times daily (excluding children aged 4–11 years) and placebo four times daily. PT027, the albuterol and budesonide comparators and placebo were delivered in a pMDI using AstraZeneca’s Aerosphere delivery technology. The dual primary efficacy endpoints were change from baseline in FEV1 area under the curve 0-6 hours over 12 weeks of PT027 compared to budesonide to assess the effect of albuterol and change from baseline in trough FEV1 at Week 12 of PT027 compared to albuterol to assess the effect of budesonide. Secondary endpoints included the time to onset and duration of response on day one, the number of patients who achieved a clinically meaningful improvement in asthma control from baseline at Week 12 and trough FEV1 at Week 1.
In the trial, PT027 demonstrated a statistically significant improvement in lung function measured by forced expiratory volume in one second (FEV1), compared to the individual components, albuterol and budesonide, and compared to placebo in patients with mild to moderate asthma aged 12 years or older. Onset of action and duration of effect were similar for PT027 and albuterol. The safety and tolerability of PT027 in DENALI was consistent with the known profiles of the components.
PT027
PT027 is a potential first-in-class SABA/ICS rescue treatment for asthma in the US, to be taken as needed. It is an inhaled, fixed-dose combination rescue medication containing albuterol (also known as salbutamol), a SABA, and budesonide, a corticosteroid, and is being developed in a pMDI using AstraZeneca’s Aerosphere delivery technology.
AstraZeneca and Avillion collaboration
In March 2018, AstraZeneca and Avillion signed an agreement to advance PT027 through a global clinical development programme for the treatment of asthma. Under the terms of the agreement, Avillion became the trial sponsor responsible for executing and funding the multicentre, global clinical trial programme for PT027 through NDA filing to a regulatory decision in the US. Following the successful approval of PT027, AstraZeneca has the option, upon certain financial payments, to commercialise the medicine in the US.
AstraZeneca in Respiratory and Immunology
Respiratory & Immunology, part of BioPharmaceuticals, is one of AstraZeneca’s main disease areas and is a key growth driver for the Company.
AstraZeneca is an established leader in respiratory care with a 50-year heritage. The Company aims to transform the treatment of asthma and COPD by focusing on earlier biology-led treatment, eliminating preventable asthma attacks, and removing COPD as a top-three leading cause of death. The Company’s early respiratory research is focused on emerging science involving immune mechanisms, lung damage and abnormal cell-repair processes in disease and neuronal dysfunction.
With common pathways and underlying disease drivers across respiratory and immunology, AstraZeneca is following the science from chronic lung diseases to immunology-driven disease areas. The Company’s growing presence in immunology is focused on five mid- to late-stage franchises with multi-disease potential, in areas including rheumatology (including systemic lupus erythematosus), dermatology, gastroenterology, and systemic eosinophilic-driven diseases. AstraZeneca’s ambition in Respiratory & Immunology is to achieve disease modification and durable remission for millions of patients worldwide.
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca's inhaled asthma therapy gets FDA panel nod for use in adults but not for kids
Nov. 09, 2022 4:35 AM ET
By: Ravikash, SA News Editor
A committee of the U.S. Food and Drug Administration (FDA) recommended the approval of AstraZeneca's (NASDAQ:AZN) inhaled asthma therapy PT027 in people aged 18 years and older but stopped short of giving it a greenlight for use in children and adolescents.
The British pharma giant said that the FDA's Pulmonary-Allergy Drugs Advisory Committee (PADAC) voted 16 to 1 that the data support a favorable benefit risk assessment for the use of PT027 (albuterol/budesonide) to treat asthma in people aged 18 years and older.
https://seekingalpha.com/symbol/AZN
IgA Nephropathy (IgAN)
IgA Nephropathy (IgAN)
IgA Nephropathy (IgAN)
Ionis presents positive Phase 2 data in patients with IgA Nephropathy at American Society of Nephrology's Kidney Week 2022
November 7, 2022 at 7:05 AM EST
– IONIS-FB-LRx achieved a 44% mean reduction in proteinuria in patients treated for 6 months
– Roche to advance IONIS-FB-LRx into Phase 3 development in H1 2023
CARLSBAD, Calif., Nov. 7, 2022 /PRNewswire/ -- Ionis Pharmaceuticals, Inc. (Nasdaq: IONS) today presented positive results from a Phase 2 clinical study of IONIS-FB-LRx in patients with immunoglobulin A nephropathy (IgAN). Results from the study were presented in a poster session at the American Society of Nephrology's (ASN) Kidney Week 2022.
In the Phase 2 study, IONIS-FB-LRx met its primary endpoint of change in 24-hour urinary protein, demonstrating a 44% mean reduction in proteinuria from baseline to week 29. Kidney function, as measured by estimated glomerular filtration rate (eGFR), was maintained in all patients in the study. IONIS-FB-LRx achieved robust and sustained reductions in plasma complement Factor B (CFB), Alternative Pathway Activity (AH50), and urinary complement fragment Ba (Factor Ba). IONIS-FB-LRx also demonstrated a favorable safety and tolerability profile in this study.
"We are extremely pleased with the results from this proof-of-concept Phase 2 study of IONIS-FB-LRx, which demonstrated the potential to treat IgAN by inhibiting complement Factor B," said Richard Geary, Ph.D., executive vice president, drug development, at Ionis. "IgAN can lead to chronic kidney disease and kidney failure and has few treatment options. Given the significant unmet medical need, we are particularly pleased that Roche is moving expeditiously to advance IONIS-FB-LRx into Phase 3 development for IgAN in the first half of next year."
About the IONIS-FB-LRx Study
IONIS-FB-LRx is being evaluated in an ongoing open-label, single arm, Phase 2 clinical study in up to 25 participants with IgAN in two dose cohorts treated sequentially (NCT04014335). The first dose cohort included 10 patients treated for 29 weeks. The primary endpoint in the study is the change in 24-hour urine protein excretion from baseline to week 29. The study is also evaluating reduction in plasma complement Factor B, measures of kidney function and safety and tolerability of monthly dosing of IONIS-FB-LRx.
About IgA Nephropathy (IgAN)
Immunoglobulin A nephropathy (IgAN) is an important cause of chronic kidney disease and renal failure. Also known as Berger's disease, IgAN is characterized by deposition of IgA and Complement 3 (C3) activation products in the glomerular mesangium of the kidneys, resulting in inflammation and tissue damage. Although IgAN may occur at any age, it generally presents in the second or third decade of life. The clinical presentation, disease progression and histologic findings are highly variable among affected individuals. Current therapies are aimed at reduction of protein levels in the urine with administration of angiotensin inhibitors and control of blood pressure. Sometimes immunosuppressive therapies are given; however, this practice is not universally accepted.
About Ionis Pharmaceuticals, Inc.
For more than 30 years, Ionis has been the leader in RNA-targeted therapy, pioneering new markets and changing standards of care with its novel antisense technology. Ionis currently has three marketed medicines and a premier late-stage pipeline highlighted by industry-leading cardiovascular and neurological franchises. Our scientific innovation began and continues with the knowledge that sick people depend on us, which fuels our vision of becoming a leading, fully integrated biotechnology company.
To learn more about Ionis, visit www.ionispharma.com and follow us on Twitter @ionispharma.
Cision View original content to download multimedia:https://www.prnewswire.com/news-releases/ionis-presents-positive-phase-2-data-in-patients-with-iga-nephropathy-at-american-society-of-nephrologys-kidney-week-2022-301669838.html
SOURCE Ionis Pharmaceuticals, Inc.
Ionis Pharmaceuticals Investor Contact: 760-603-2331; Ionis Pharmaceuticals Media Contact: 760-603-4679
Ionis, Roche kidney disease drug meets main goal in mid-stage study
Nov. 07, 2022 7:30 AM ET
Ionis Pharmaceuticals, Inc. (IONS), RHHBY, RHHBF
By: Ravikash, SA News Editor1 Comment
- Ionis Pharmaceuticals (NASDAQ:IONS) said a phase 2 trial of IONIS-FB-LRx in patients with immunoglobulin A nephropathy (IgAN) met its main goal.
- IgAN is a kidney disease which occurs when an antibody called immunoglobulin A (IgA) builds up in the kidneys causing inflammation.
- https://seekingalpha.com/news/3902491-ionis-roche-kidney-disease-drug-meets-main-goal-in-mid-stage-study
- https://seekingalpha.com/symbol/IONS
- https://seekingalpha.com/symbol/RHHBY
- https://seekingalpha.com/symbol/RHHBF
- https://www.ionispharma.com/
- https://www.ionispharma.com/ionis-innovation/pipeline/
OLPASIRAN
IgA Nephropathy (IgAN)
OLPASIRAN
AMGEN PRESENTS NEW PHASE 2 DATA THAT SHOW OLPASIRAN DELIVERS SIGNIFICANT REDUCTION IN LIPOPROTEIN(A) LEVELS
Olpasiran Reduced Lipoprotein(a) Levels by More Than 95% in Patients With Established ASCVD
Amgen is Initiating a Phase 3 Cardiovascular Outcomes Trial Based on These Results
Data Simultaneously Published in the New England Journal of Medicine
THOUSAND OAKS, Calif. , Nov. 6, 2022 /PRNewswire/ -- Amgen (NASDAQ:AMGN) today presented end-of-treatment data from its Phase 2 OCEAN(a)-DOSE study of investigational olpasiran (formerly AMG 890) in adults with elevated lipoprotein(a) [Lp(a)] levels (>150 nmol/L) and a history of atherosclerotic cardiovascular disease (ASCVD). The study was designed to assess safety, tolerability and optimal dose of olpasiran in adults with established ASCVD to reduce Lp(a).1 These data were presented during the Nov. 6 Late-Breaking Science Session of the American Heart Association (AHA) Scientific Sessions 2022 in Chicago, Illinois, and simultaneously published in the New England Journal of Medicine.
OCEAN(a)-DOSE is a multicenter, randomized, double-blind, placebo-controlled dose-finding study of olpasiran in 281 patients with established ASCVD and Lp(a) levels >150 nmol/L. Patients were randomized to one of four doses of olpasiran (10 mg Q12 weeks, 75 mg Q12 weeks, 225 mg Q12 weeks or 225 mg Q24 weeks) or placebo, given subcutaneously.2 Across cohorts, the median baseline Lp(a) concentration was 260.3 nmol/L. Patients who received 75 mg or higher every 12 weeks had a 95% or greater reduction in Lp(a) compared to placebo at week 36. At these doses (75 mg or higher), more than 98% of patients achieved an Lp(a) level of 125 nmol/L or less at week 36.2 Overall, the rates of adverse events were similar in the olpasiran and placebo arms. The most common treatment-related adverse events were injection site reactions, primarily pain.2
"Epidemiological research has shown us that Lp(a) is an independent risk factor and is primarily genetically determined. It has been estimated that up to 20% of people worldwide are living with elevated levels, which are linked to a higher risk for heart disease, stroke and the potential significant burden on patients with cardiovascular disease,"5 said David M. Reese, M.D., executive vice president of Research and Development at Amgen. "Our Phase 2 data for olpasiran presented at AHA continue to demonstrate a significant reduction in Lp(a) and provide strong evidence supporting its potential for patients with ASCVD. We look forward to studying this treatment further in Phase 3 clinical trials, which we expect to begin enrolling in December 2022."
At week 36, Lp(a) increased by a mean of 3.6% in the placebo arm, whereas there were substantial reductions of Lp(a) levels in all of the olpasiran arms. Placebo-adjusted mean percent reductions were 70.5% for 10 mg every 12 weeks, 97.4% for 75 mg every 12 weeks, 101.1% for 225 mg every 12 weeks and 100.5% for 225 mg every 24 weeks .2
"Currently, there are no approved medicines that can consistently achieve marked or sustained reductions in Lp(a) concentration," said Michelle L. O'Donoghue M.D., MPH, Senior Investigator, TIMI Study Group at Brigham and Women's Hospital and OCEAN(a)-DOSE trial Global Principal Investigator. "RNA interference with olpasiran is a promising treatment approach that led to a profound and sustained reduction in Lp(a) concentration in this Phase 2 study."
About Lp(a)
Lp(a) is genetically determined3-5 and a presumed independent risk factor for cardiovascular disease (CVD). Although an agreed upon threshold for elevated Lp(a) is not firmly established, approximately 20% of adults have Lp(a) >125 nmol/L (or approximately 50 mg/dL).3 Evidence has emerged from pathophysiological, epidemiologic, and genetic studies on the potential role of elevated Lp(a) in contributing to myocardial infarction, stroke, and peripheral arterial disease.5
About OCEAN(a)
The OCEAN(a) (Olpasiran Trials of Cardiovascular Events And LipoproteiN(a) Reduction) clinical program for Amgen's investigational olpasiran is designed to treat patients with atherosclerotic cardiovascular disease (ASCVD) and elevated Lp(a) levels to reduce the risk of cardiovascular events.
The OCEAN(a)-DOSE trial is a multicenter, randomized, double-blind, placebo-controlled dose-finding Phase 2 study in 281 patients with ASCVD and Lp(a) >150 nmol/L. Patients were randomly assigned to one of four active subcutaneous doses of olpasiran (10 mg Q12 weeks, 75 mg Q12 weeks, 225 mg Q12 weeks or 225 mg Q24 weeks) or placebo. The primary endpoint is percent change from baseline in Lp(a) at 36 weeks. A secondary endpoint is percent change from baseline in Lp(a) at 48 weeks.
A prespecified exploratory endpoint was the percent change in Lp(a) from baseline at each scheduled visit for the 225 mg Q24 week dose group.
About Amgen
Amgen is committed to unlocking the potential of biology for patients suffering from serious illnesses by discovering, developing, manufacturing and delivering innovative human therapeutics. This approach begins by using tools like advanced human genetics to unravel the complexities of disease and understand the fundamentals of human biology.
Amgen focuses on areas of high unmet medical need and leverages its expertise to strive for solutions that improve health outcomes and dramatically improve people's lives. A biotechnology pioneer since 1980, Amgen has grown to be one of the world's leading independent biotechnology companies, has reached millions of patients around the world and is developing a pipeline of medicines with breakaway potential.
Amgen is one of the 30 companies that comprise the Dow Jones Industrial Average and is also part of the Nasdaq-100 index. In 2022, Amgen was named one of the "World's Best Employers" by Forbes and one of "America's 100 Most Sustainable Companies" by Barron's.
For more information, visit Amgen.com and follow us on Twitter, LinkedIn, Instagram, TikTok and YouTube.

View original content to download multimedia:https://www.prnewswire.com/news-releases/amgen-presents-new-phase-2-data-that-show-olpasiran-delivers-significant-reduction-in-lipoproteina-levels-301669146.html
SOURCE Amgen
Amgen's olpasiran cuts cholesterol levels by 95% in heart disease patients in trial
Nov. 07, 2022 5:15 AM ET
By: Ravikash, SA News Editor1 Comment
Amgen (NASDAQ:AMGN) said its drug olpasiran helped reduce a type of 'bad cholesterol' by more than 95% in patients with atherosclerotic cardiovascular disease (ASCVD) in a phase 2 trial.
https://seekingalpha.com/symbol/AMGN
EB-101
SARCONEOS (BIO101)
OLPASIRAN
Abeona Therapeutics Announces Positive Topline Results with Both Co-Primary Endpoints Met in Pivotal Phase 3 VIITAL™ Study of EB-101
Abeona Therapeutics Announces Positive Topline Results with Both Co-Primary Endpoints Met in Pivotal Phase 3 VIITAL™ Study of EB-101
November 03, 2022
Co-primary endpoint measuring >50% wound healing, other endpoints measuring >75% and complete wound healing at six months all met
Co-primary endpoint measuring pain reduction at six months met; greater magnitude of pain reduction benefit was observed in post-hoc analysis of EB-101 treated wounds with severe baseline pain
EB-101 was well-tolerated with no serious treatment-related adverse events, consistent with past clinical experience
Plans to submit Biologics License Application (BLA) to U.S. FDA
Conference call on November 3, 2022 at 8:30 a.m. EDT
NEW YORK and CLEVELAND, Nov. 03, 2022 (GLOBE NEWSWIRE) -- Abeona Therapeutics Inc. (Nasdaq: ABEO) today announced positive topline data from its pivotal Phase 3 VIITAL™ study assessing the safety and efficacy of EB-101 for the treatment of patients with recessive dystrophic epidermolysis bullosa (RDEB). The VIITAL™ study met its two co-primary efficacy endpoints demonstrating statistically significant, clinically meaningful improvements in wound healing and pain reduction in large chronic RDEB wounds.
“We are very pleased with the topline results from our pivotal VIITAL™ study, which reinforce the strong value proposition of EB-101 as a potential one-time therapy to both significantly improve wound healing and reduce pain for the most disabling, challenging to treat wounds in patients with RDEB,” said Vish Seshadri, Chief Executive Officer of Abeona. “The VIITAL™ study is differentiated from any other pivotal study in RDEB by the co-primary endpoint measuring patient-reported pain. We believe the significant result in this endpoint supports EB-101’s potential for improving the daily life of RDEB patients. Based on the efficacy and safety profile of EB-101 in VIITAL™, we are looking forward to sharing the VIITAL™ study results with the FDA and progressing toward submission of a BLA. We are grateful to the patients, their families, caregivers, and the patient advocacy groups for their support of this study, and are also thankful for the clinical investigators, study site personnel, and the entire Abeona team who collectively contributed to this milestone achievement.”
Summary of Topline Results: All Evaluated Endpoints Successfully Achieved
The pivotal Phase 3 VIITAL™ study evaluated the efficacy, safety and tolerability of EB-101 in 43 large chronic wound pairs in 11 subjects with RDEB. The large chronic wounds randomized and treated in VIITAL™ measured greater than 20 cm2 of surface area and had remained open for a minimum of six months and a maximum of 21 years (mean 6.2 years). The co-primary endpoints of the study were: 1) the proportion of RDEB wound sites with greater than or equal to 50% healing from baseline, comparing randomized treated with matched untreated (control) wound sites at the six-month timepoint, as determined by direct investigator assessment; and 2) pain reduction associated with wound dressing change assessed by the mean differences in scores of the Wong-Baker FACES scale between randomized treated and matched untreated (control) wounds at the six-month timepoint. The study allowed for wounds not included in the randomized primary efficacy analysis to receive EB-101 treatment (n=14 non-randomized wounds). The tables below summarize the topline primary efficacy results:
EB-101 was shown to be well-tolerated with no serious treatment-related adverse events observed, consistent with past clinical experience. There were no deaths or instances of positive replication-competent retrovirus (RCR) results, and no systemic immunologic responses were reported during the study, as well as no squamous cell carcinoma (SCC) at treatment sites after application of EB-101. Two subjects reported at least one serious adverse event (SAE) unrelated to EB-101. Four subjects reported related treatment emergent adverse events (TEAEs), including procedural pain, muscle spasms and pruritis. Infections unrelated to EB-101 were observed in eight patients.
Abeona anticipates submitting results from this study, including further details with additional exploratory endpoints and the Week 12 results, for presentation at future medical meetings and for publication in a peer-reviewed journal. The Week 12 results are similar to Week 24 results, achieving statistical significance for pain reduction and wound healing at all levels.
Jean Tang, M.D., Ph.D., Professor of Dermatology, Stanford University School of Medicine and Principal Investigator of the EB-101 pivotal Phase 3 VIITAL™ study said, “Large chronic RDEB wounds are the toughest to treat and often associated with intense chronic pain that significantly impacts the quality of life of RDEB patients, necessitating frequent use of opioids. In the Phase 3 VIITAL™ study, EB-101 has been shown to both heal such large chronic wounds and significantly reduce pain. And we continue to see durable clinical benefit of EB-101 with up to eight years of follow-up in our Phase 1/2a study.”
Brett Kopelan, Executive Director, debra of America, and father to Rafi, a 15-year-old with RDEB, said, “I am incredibly enthused to see new clinical evidence of EB-101’s potential to treat the more difficult chronic and large wounds. Our patient community needs options to address not only the healing of wounds but also the chronic pain and the acute treatment related pain of daily wound care associated with these wounds. Today’s standard of care comprises hours of brutal and painful wound care, and EB-101’s promise to be a transformational option for RDEB patients is truly exciting.”
About EB-101
EB-101 is an autologous, engineered cell therapy currently being developed for the treatment of recessive dystrophic epidermolysis bullosa (RDEB), a rare connective tissue disorder without an approved therapy. The EB-101 VIITAL™ study is a randomized clinical trial with target enrollment of at least 10 to 15 RDEB patients with approximately 36 large, chronic wound sites treated in total. Treatment with EB-101 involves using gene transfer to deliver the COL7A1 gene into a patient’s own skin cells (keratinocytes and its progenitors) and transplanting those cells back to the patient. EB-101 is being investigated for its ability to enable normal Type VII collagen expression and to facilitate wound healing. The U.S. FDA has granted Rare Pediatric Disease designation for EB-101. Abeona produces EB-101 for the VIITAL™ study at its fully integrated gene and cell therapy manufacturing facility in Cleveland, Ohio. EB-101 is an investigational product not yet approved by the FDA.
About Abeona Therapeutics
Abeona Therapeutics Inc. is a clinical-stage biopharmaceutical company developing cell and gene therapies for serious diseases. Abeona’s lead clinical program is EB-101, its investigational autologous, engineered cell therapy currently in development for recessive dystrophic epidermolysis bullosa. The Company’s development portfolio also features AAV-based gene therapies for ophthalmic diseases with high unmet medical need. Abeona’s novel, next-generation AAV capsids are being evaluated to improve tropism profiles for a variety of devastating diseases. Abeona’s fully integrated cell and gene therapy cGMP manufacturing facility produces EB-101 for the pivotal Phase 3 VIITAL™ study and is capable of clinical and potential commercial production of AAV-based gene therapies. For more information, visit www.abeonatherapeutics.com.
Source: Abeona Therapeutics Inc.
Released November 3, 2022
Abeona says phase 3 trial of EB-101 cell therapy for rare skin disorder meets main goals
Nov. 03, 2022 9:32 AM ET
Abeona Therapeutics Inc. (ABEO)
By: Anuron Mitra, SA News Editor
- Abeona Therapeutics (NASDAQ:ABEO) on Thursday said a phase 3 trial of its cell therapy EB-101 for the treatment of recessive dystrophic epidermolysis bullosa (RDEB) met its main goals.
- https://seekingalpha.com/news/3901011-abeona-says-phase-3-trial-of-eb-101-cell-therapy-for-rare-skin-disorder-meets-main-goals
- https://seekingalpha.com/symbol/ABEO
- https://clinicaltrials.gov/ct2/show/NCT04227106
- https://www.abeonatherapeutics.com/
SARCONEOS (BIO101)
SARCONEOS (BIO101)
SARCONEOS (BIO101)
NOVEMBER 03, 2022
BIOPHYTIS REPORTS POSITIVE POST-HOC ANALYSIS OF THE PHASE 2-3 COVA CLINICAL STUDY STRONGLY SUPPORTING THERAPEUTIC POTENTIAL OF SARCONEOS (BIO101) IN COVID-19
Biophytis released the full results from its phase 2-3 COVA clinical study evaluating Sarconeos (BIO101) in the treatment of COVID-19-related respiratory failure.
- A reduction in the risk of early death or respiratory failure at day 28 of 45% in the Intent-To-Treat (ITT) population and 53% in the Per Protocol (PP) population
- A reduction in the risk of death at day 90 of 43% in the ITT population and 70% in the PP population
- The start of regulatory development of Sarconeos (BIO101) targeting conditional and emergency use marketing authorisations in 2023
Biophytis reports positive post-hoc analysis of the phase 2-3
COVA clinical study strongly supporting therapeutic
potential of Sarconeos (BIO101) in COVID-19
• A reduction in the risk of early death or respiratory failure at day 28 of
45% in the Intent-To-Treat (ITT) population and 53% in the Per Protocol
(PP) population
• A reduction in the risk of death at day 90 of 43% in the ITT population
and 70% in the PP population
• The start of regulatory development of Sarconeos (BIO101) targeting
conditional and emergency use marketing authorisations in 2023
Paris (France), Cambridge (Massachusetts, U.S.), November 3rd, 2022, 8am CET – Biophytis
SA (NasdaqCM: BPTS, Euronext Growth Paris: ALBPS) (the “Company” or “Biophytis”), a clinical-
stage biotechnology company focused on the development of therapeutics that slow the
degenerative processes associated with aging, including severe respiratory failure in patients suffering from COVID-19, today released the full results from its phase 2-3 COVA clinical study
evaluating Sarconeos (BIO101) in the treatment of COVID-19-related respiratory failure.
The objective of the study was to investigate the efficacy and safety of Sarconeos (BIO101), 350
mg BID in hospitalized COVID-19 patients with hypoxemia, at risk of respiratory failure requiring
high flow oxygen or mechanical ventilation, and death. The proportion and time to onset of
these negative events were studied at 28 days in the primary analysis, corresponding to the
maximum treatment period, with follow-up of mortality and safety for at least 90 days.
The 233 treated patients (ITT population) were 63 years old on average, 64% of the patients
were male, recruited in centers in Europe, the US and Brazil between Q3 2020 and Q1 2022,
infected with the main SARS-Cov-2 variants. The trial ended early before reaching the 310
patients originally planned, due to stalled recruitment. The sub-population of patients without
major protocol deviations (PP sub-population) included 180 patients with similar baseline
demographics and disease characteristics as the ITT population. Since the top line results of the
study were reported and because the study was underpowered, post-hoc statistical analyses
have been performed to re-estimate the effect of Sarconeos (BIO101) on the risk of early death
or respiratory failure at day 28 (primary endpoint of the study) and death at day 90 in the ITT
and PP populations.
On respiratory failure or early death, post-hoc Kaplan-Meier analyses show a significant
reduction with Sarconeos (BIO101) in the risk of early death or respiratory failure at day 28 by
45% (p=0.037) in the ITT population and by 53% (p=0.051) in the PP population. These post-
hoc analyses strongly strengthen the primary analysis that had shown significant differences
over 28 days in the Kaplan Meier curves for BIO101 versus placebo, (p=0.034, see figure below),
and a strong trend when testing for difference at day 28 by using the pre-defined statistical
model (primary end-point,Cochran-Mantel-Haenszel test, p=0.071).
On mortality follow-up over 90 days, post hoc Kaplan-Meier analysis of the risk of death at day
90 was reduced with Sarconeos (BIO101) by 43% in the ITT population (p=0.076) and by 70% in
the PP population (p=0.016). These analysis strongly strengthen the trend shown in the primary
analysis with similar reduction of risk of death at day 28 which was not significant. The reduction
in the risk of death at day 90 reflects the effect of Sarconeos (BIO101) on early death and
respiratory failure during the maximum 28 days treatment period that translates efficiently and
in the same proportion into a reduction in the risk of death later on.
Sarconeos (BIO101) has a good safety profile, with a lower proportion of patients with adverse
events compared to placebo (57% vs. 64%), in particular a lower frequency of serious, mostly
respiratory, adverse events (25% vs. 31%).
Time (days)
Proportion
Proportion without respiratory failure or early death, Kaplan-Meier Analysis, ITT population
Time (days)
Proportion
Proportion without death, Kaplan-Meier Analysis, ITT population
The Company aims to present the results in detail as soon as possible during upcoming scientific
conferences in the first half of 2023 and in a peer-reviewed scientific journal.
Stanislas Veillet, CEO of Biophytis, said: "These post-hoc analyses strongly support the
therapeutic potential of Sarconeos (BIO101) in the treatment of hospitalized patients with
severe COVID-19. The reduction in the risk of respiratory failure and death by more than 40% is
impressive. These results exceed expectations about the effect size of BIO101 (expected 37.5%
relative reduction vs. placebo) used in the sample size calculation of the study and commit us to
further develop Sarconeos (BIO101) in this indication, giving hospitalized patients a therapeutic
option while COVID-19 is becoming endemic. We will start sharing these results in the coming
months with regulatory agencies and health authorities, particularly in Europe, the US and
Brazil. The aim is to file for conditional marketing authorisation (Europe) and emergency use
authorization (USA, Brazil) as soon as possible in 2023. I would like to sincerely thank all the patients, caregivers, employees, and finally the shareholders of Biophytis for their work, trust and dedication, throughout this study."
Convinced of the therapeutic potential of Sarconeos (BIO101), Biophytis intends to offer this
new therapeutic solution to hospitalized patients with severe COVID-19 as soon as possible.
Biophytis will first amend and extend the Early Access Programme (EAP) to make Sarconeos
(BIO101) available as soon as possible to hospitalized COVID-19 patients at risk of respiratory
failure and death. An EAP has already been approved in the first half of 2022 in Brazil to treat
intensive care patients, and applications will be made in other territories including the US and
Europe. Biophytis will also start to prepare for filing in 2023 for Emergency Use Authorization
(EUA) in the United States and Brazil and conditional marketing authorisation in Europe,
depending on COVID-19 evolution.
About the COVA study
As a reminder, the COVA clinical study (identifier clinicaltrials.gov: NCT04472728) is an
international, multi-centre, double-blind, placebo-controlled, group-sequential and adaptive
two-part study. It is a phase 2-3 study evaluating Sarconeos (BIO101) in patients aged 45 years
and older, hospitalised with severe respiratory manifestations of COVID-19. Part 1 of the COVA
study is an exploratory Phase 2 proof-of-concept study designed to provide preliminary data
on the safety, tolerability and efficacy of Sarconeos (BIO101) in 50 hospitalised patients with
severe respiratory failure in patients suffering from COVID-19. Part 2 of the COVA study is a
randomised phase 3 study investigating the safety and efficacy of Sarconeos (BIO101) on
respiratory function in patients. Due to the evolution of the pandemia, the company decided
in April 2022 to stop enrolment at 237 enrolled patients, below the originally planned number
of 310.
About BIOPHYTIS
Biophytis SA is a clinical-stage biotechnology company specialized in the development of
therapeutics that are aimed at slowing the degenerative processes associated with aging and
improving functional outcomes for patients suffering from age-related diseases, including
severe respiratory failure in patients suffering from COVID-19. Sarconeos (BIO101), our leading
drug candidate, is a small molecule, administered orally, planned to be developed as a
treatment for sarcopenia in upcoming Phase 3 clinical trials in the United States, Brazil and
Europe (SARA-31 and SARA-32). It has also been studied in a clinical two-part Phase 2-3 study
(COVA) for the treatment of severe respiratory manifestations of COVID-19 in Europe, Latin
America, and the US. A pediatric formulation of Sarconeos (BIO101) is being developed for the
treatment of Duchenne Muscular Dystrophy (DMD). The Company is based in Paris, France, and
Cambridge, Massachusetts. The Company's ordinary shares are listed on Euronext Growth
(Ticker: ALBPS -ISIN: FR0012816825) and ADSs (American Depositary Shares) are listed on
Nasdaq Capital Market (Ticker BPTS – ISIN: US09076G1040). For more information visit
www.biophytis.com
Biophytis surges 32 % as COVID drug cuts risk of early death in trial
Nov. 03, 2022 5:29 AM ET
By: Ravikash, SA News Editor
Biophytis (NASDAQ:BPTS) said its medicine Sarconeos help cut the risk of early death or respiratory failure in patients with COVID-19 in a post-hoc analysis of a phase 2-3 trial.
https://seekingalpha.com/symbol/BPTS
https://www.biophytis.com/en/our-science/sarcopenie/
OTX-2002
SARCONEOS (BIO101)
SARCONEOS (BIO101)
OMEGA THERAPEUTICS RECEIVES ORPHAN DRUG DESIGNATION FOR OTX-2002 FOR THE TREATMENT OF HEPATOCELLULAR CARCINOMA
Nov 02, 2022 PDF Version
Phase 1/2 MYCHELANGELO™ I Clinical Trial Underway to Evaluate Safety, Tolerability and Preliminary Antitumor Activity of OTX-2002
CAMBRIDGE, Mass., Nov. 2, 2022 /PRNewswire/ -- Omega Therapeutics, Inc. ("Omega"), a clinical-stage biotechnology company pioneering the first systematic approach to use mRNA therapeutics as a new class of programmable epigenetic medicines, today announced that the U.S. Food and Drug Administration (FDA) has granted Orphan Drug Designation for OTX-2002, the company's first-in-class epigenomic controller engineered to downregulate c-Myc (MYC), for the treatment of hepatocellular carcinoma (HCC).
The company recently announced that the first patient had been dosed in its Phase 1/2 MYCHELANGELO™ I clinical trial investigating the safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary antitumor activity of OTX-2002 as a monotherapy and in combination with standard of care therapies in patients with relapsed or refractory HCC and other solid tumor types known for association with the MYC oncogene.
"HCC is a devastating illness that often develops resistance to current standard of care therapeutics. The FDA's decision to grant orphan drug designation for OTX-2002 underscores the need for novel therapies to address HCC and the potential of epigenomic programming to transform the treatment landscape," said Mahesh Karande, President and Chief Executive Officer of Omega Therapeutics. "We look forward to continuing to work with clinical investigators, patients and the FDA as we advance our MYCHELANGELO clinical program and evaluate the potential of OTX-2002 to bring a new treatment option to the liver cancer patient community."
About OTX-2002
OTX-2002 is a first-in-class Omega Epigenomic Controller™ in development for the treatment of hepatocellular carcinoma (HCC). OTX-2002 is an mRNA therapeutic delivered via lipid nanoparticles (LNPs) and is designed to downregulate MYC expression pre-transcriptionally through epigenetic modulation while potentially overcoming MYC autoregulation. MYC is a master transcription factor that regulates cell proliferation, differentiation and apoptosis and plays a significant role in more than 50% of all human cancers. OTX-2002 is currently being evaluated in the Phase 1/2 MYCHELANGELO™ I trial in patients with relapsed or refractory HCC and other solid tumor types known for association with the MYC oncogene; visit clinicaltrials.gov (NCT05497453) for more details.
About Omega Therapeutics
Omega Therapeutics, founded by Flagship Pioneering, is a clinical-stage biotechnology company pioneering the first systematic approach to use mRNA therapeutics as a new class of programmable epigenetic medicines. The company's OMEGA Epigenomic Programming™ platform harnesses the power of epigenetics, the mechanism that controls gene expression and every aspect of an organism's life from cell genesis, growth, and differentiation to cell death. Using a suite of technologies, paired with Omega's process of systematic, rational, and integrative drug design, the OMEGA platform enables control of fundamental epigenetic processes to correct the root cause of disease by returning aberrant gene expression to a normal range without altering native nucleic acid sequences. Omega's modular and programmable mRNA medicines, Omega Epigenomic Controllers™, target specific epigenomic loci within insulated genomic domains, EpiZips™, from amongst thousands of unique, mapped, and validated genome-wide DNA-sequences, with high specificity to durably tune single or multiple genes to treat and cure diseases through Precision Genomic Control™. Omega is currently advancing a broad pipeline of development candidates spanning a range of disease areas, including oncology, regenerative medicine, multigenic diseases including immunology, and select monogenic diseases, including alopecia.
For more information, visit omegatherapeutics.com, or follow us on Twitter and LinkedIn.
Cision View original content to download multimedia:https://www.prnewswire.com/news-releases/omega-therapeutics-receives-orphan-drug-designation-for-otx-2002-for-the-treatment-of-hepatocellular-carcinoma-301665321.html
SOURCE Omega Therapeutics
Omega liver cancer drug OTX-2002 gets FDA orphan drug status
Nov. 02, 2022 8:18 AM ET
Omega Therapeutics, Inc. (OMGA)
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted orphan drug designation to Omega Therapeutics' (NASDAQ:OMGA) OTX-2002 to treat hepatocellular carcinoma (HCC), a type of liver cancer.
- https://seekingalpha.com/news/3899540-omega-liver-cancer-drug-otx-2002-gets-fda-orphan-drug-status
- https://seekingalpha.com/symbol/OMGA
- https://omegatherapeutics.com/our-portfolio/#pipeline
Iomab-B
Epcoritamab (DuoBody®-CD3xCD20)
Epcoritamab (DuoBody®-CD3xCD20)
Actinium Announces Positive Top-line Results from Pivotal Phase 3 SIERRA Trial of Iomab-B in Patients with Active Relapsed or Refractory Acute Myeloid Leukemia
OCTOBER 31, 2022
- Iomab-B met the primary endpoint of durable complete remission of 6-months following initial complete remission after HCT with a p-value of <0.0001
NEW YORK, Oct. 31, 2022 /PRNewswire/ -- Actinium Pharmaceuticals, Inc. (NYSE AMERICAN: ATNM) (Actinium or the Company), a leader in the development of targeted radiotherapies, today announced positive top-line results from the pivotal Phase 3 trial for its lead product candidate Iomab-B. The SIERRA (Study of Iomab-B in Elderly Relapsed or Refractory AML) trial was conducted in patients 55 years of age or older who had active disease (relapsed or refractory AML). The SIERRA trial is a randomized, multi-center, controlled study which compared Iomab-B as a conditioning regimen prior to a Bone Marrow Transplant (BMT) versus a control arm which allowed all current means of conventional care with the intent to transplant these patients. The SIERRA trial met its primary endpoint of durable complete remission or dCR of 6 months post initial remission after a BMT in Iomab-B arm compared to conventional care arm demonstrating statistical significance p<0.0001.

Dr. Avinash Desai, Actinium's Chief Medical Officer, added, "We are excited that the randomized, controlled, multi-center, pivotal SIERRA trial has delivered these results for patients that need new treatment options. Our goal is to increase access to BMT and improve patient outcomes with Iomab-B, and these topline results move us in this direction given their statistical significance. We will continue to work on our Biologics License Application (BLA) submission to the US Food and Drug Administration (FDA) for approval of Iomab-B. On behalf of Actinium, I'd like to thank the patients who took the leap of faith and enrolled in the SIERRA trial, their families and caregivers who supported them and the investigators who contributed their efforts and advice who made this trial possible. Without them it would not have been possible to yield these results that will enable us to continue to develop Iomab-B."
Sandesh Seth, Actinium's Chairman and CEO, said, "This is a significant milestone in Actinium's lifecycle and a testimony to the quality of our team who undertook a pioneering study in a patient population that is considered largely futile to treat. Despite being perennially under-staffed and under resourced, their passion and perseverance has yielded a clinically meaningful dividend. Our recently strengthened team is executing to enable our mission to disrupt the field of bone marrow conditioning with Iomab-B, first in r/r AML and then by building upon its robust prior clinical results in several hematological diseases. We look forward to sharing additional clinical data from the SIERRA trial by year end."
About Iomab-B and the Pivotal Phase 3 SIERRA Trial
Iomab-B is a first-in-class targeted radiotherapy intended to improve patient access to potentially curative BMT by simultaneously and rapidly depleting blood cancer, immune and bone marrow stem cells that uniquely express CD45. Multiple studies have demonstrated increased survival in patients receiving BMT, however, an overwhelming majority of patients with blood cancers do not receive BMT as current approaches do not produce a remission, which is needed to advance to BMT, or are too toxic. Studied in over 400 patients, prior studies with Iomab-B have demonstrated nearly universal access to BMT, increased survival and tolerability in multiple clinical trials including the recently completed pivotal Phase 3 SIERRA trial in patients with active (leukemic blasts >5%), relapsed or refractory acute myeloid leukemia (r/r AML) age 55 and above. The SIERRA trial produced positive topline results, meeting its primary endpoint of durable Complete Remission (dCR) of 6 months with statistical significance (p<0.0001). Actinium intends to submit a Biologics License Application (BLA) seeking approval for Iomab-B to address patients age 55+ with r/r AML who cannot access BMT with currently available therapies. Iomab-B has been granted Orphan Drug Designation from the U.S. Food and Drug Administration (FDA) and has patent protection into 2037.
The pivotal Phase 3 SIERRA (Study of Iomab-B in Elderly relapsed or refractory AML) is a 153-patient, randomized, multi-center clinical trial, studying Iomab-B compared to the control arm of physician's choice of salvage therapy. Control arm options included chemotherapies like cytarabine and daunorubicin and targeted agents such as a Bcl-2 inhibitor (Venetoclax), FLT3 inhibitors and IDH 1/2 inhibitors. The SIERRA control arm reflects real-world treatment of r/r AML patients with over 20 single agents or combination of agents as no standard of care exists for this patient population. Data from full patient enrollment presented at the Transplantation & Cellular Therapy Tandem Meetings in April 2022 showed that 100% of patients receiving Iomab-B accessed BMT and engrafted without delay. Iomab-B was also shown to be well tolerated given its targeted nature, consistent with its previous clinical data. The SIERRA trial enrolled patients at 24 leading transplant centers in the United States and Canada that perform over 30% of AML BMTs.
Developed at the Fred Hutchinson Cancer Research Center, a pioneer in the field of BMT, Iomab-B is supported by data in six disease indications including leukemias, lymphomas and multiple myeloma, which afflict over 100,000 patients annually. Actinium intends to pursue additional indications for Iomab-B beyond AML. Actinium also intends to pursue international regulatory approvals independently and through partnerships. In April 2022, Actinium licensed the European, Middle East and North African commercial rights for Iomab-B to Immedica AB, a fully-fledged independent pharmaceutical company headquartered in Sweden. In exchange, Actinium received an upfront payment of $35 million USD with the potential for an additional $417 million USD in regulatory and sales milestones and mid-twenty percent royalties. Europe represents a commercial opportunity double the size of the United States by number of patients with AML receiving BMT. Iomab-B has been granted Orphan Drug Designation by the European Medicines Agency (EMA) and has received positive Scientific Advice from the Committee for Medicinal Products for Human Use (CHMP) of the EMA indicating that the Phase 3 SIERRA trial design, primary endpoint and planned statistical analysis are acceptable as the basis for a Marketing Authorization Application.
About Actinium Pharmaceuticals, Inc.
Actinium Pharmaceuticals, Inc. is a clinical-stage biopharmaceutical company developing targeted radiotherapies to deliver cancer-killing radiation with cellular level precision to treat patients with high unmet needs. Actinium's clinical pipeline is led by radiotherapies that are being applied to targeted conditioning, which is intended to selectively deplete a patient's disease or cancer cells and certain immune cells prior to a bone marrow transplant (BMT), gene therapy or adoptive cell therapy, such as CAR-T, to enable engraftment of these transplanted cells with minimal toxicities. Our lead product candidate, I-131 apamistamab (Iomab-B) has been studied in over four hundred patients in six disease indications including acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), acute lymphoblastic leukemia (ALL), hodgkin's lymphoma, non-hodgkin's lymphoma (NHL) and multiple myeloma across twelve clinical trials including the pivotal Phase 3 Study of Iomab-B in Elderly Relapsed or Refractory Acute Myeloid Leukemia (SIERRA) trial for BMT conditioning. Iomab-B targets CD45, a cell surface protein expressed on blood cancer cells, normal nucleated immune cells and bone marrow stem cells. Actinium licensed the world-wide exclusive rights to Iomab-B from the Fred Hutchinson Cancer Research Center, a noble prize-winning institution that pioneered the field of bone marrow transplant. Data. Data from the pivotal Phase 3 SIERRA trial has been presented at multiple international medical conferences such as the annual meeting of the American Society of Hematology (ASH) with recent topline data submitted for presentation at this year's meeting, the Tandem Meetings, Transplantation & Cellular Therapy Meetings of the American Society for Transplantation and Cellular Therapy (ASTCT) and the Center for International Blood & Marrow Transplant Research (CIBMTR), and the annual meeting of the Society of Hematologic Oncology (SOHO), where it was awarded honorable distinction in 2019. Post successful topline results, the Company expects to release a more comprehensive set of results by year-end 2022 and is working toward a BLA filing in 2023. Iomab-ACT, low dose I-131 apamistamab, is being studied as a targeted conditioning agent in a Phase 1 study with a CD19 CAR T-cell Therapy with Memorial Sloan Kettering Cancer Center with NIH funding. Iomab-ACT employs a lower dose of I-131 and is being developed to be a single-infusion, out-patient administered therapy that can transiently lymphodeplete patients prior to receiving their CAR-T cellular therapy. Actimab-A, our second most advanced product candidate has been studied in approximately 150 patients with Acute Myeloid Leukemia or AML, including in ongoing combination trials with the chemotherapy regimen CLAG-M and with venetoclax, a targeted therapy. Actimab-A or lintuzumab-Ac225 is an Actinium-225 based antibody radiation conjugate targeting CD33, a validated target in AML. Actinium is a pioneer and leader in the field of Actinium-225 alpha therapies with an industry leading technology platform comprising over 195 patents and patent applications including methods of producing the radioisotope AC-225. Our technology and expertise have enabled collaborative research partnerships with Astellas Pharma, Inc. for solid tumor theranostics, with AVEO Oncology Inc. to create an Actinium-225 HER3 targeting radiotherapy for solid tumors, and with EpicentRx, Inc. to create targeted radiotherapy combinations with their novel, clinical stage small molecule CD47-SIRPα inhibitor. More information is available on Actinium's website: https://www.actiniumpharma.com/.
View original content to download multimedia:https://www.prnewswire.com/news-releases/actinium-announces-positive-top-line-results-from-pivotal-phase-3-sierra-trial-of-iomab-b-in-patients-with-active-relapsed-or-refractory-acute-myeloid-leukemia-301662998.html
SOURCE Actinium Pharmaceuticals, Inc.
Released October 31, 2022
Actinium climbs 23% as lead asset meets main goal in Phase 3 leukemia trial
Oct. 31, 2022 6:50 AM ET
Actinium Pharmaceuticals, Inc. (ATNM)
By: Dulan Lokuwithana, SA News Editor1 Comment
- Actinium Pharmaceuticals (NYSE:ATNM), a biotech focused on targeted radiotherapies, jumped ~23% pre-market Monday after announcing that its lead product candidate Iomab-B met the primary endpoint in a pivotal Phase 3 trial involving patients with acute myeloid leukemia (AML).
- https://seekingalpha.com/news/3897617-atnm-stock-climbs-as-lead-asset-meets-main-goal-in-phase-3-leukemia-trial
- https://seekingalpha.com/symbol/ATNM
- https://www.actiniumpharma.com/
Epcoritamab (DuoBody®-CD3xCD20)
Epcoritamab (DuoBody®-CD3xCD20)
Epcoritamab (DuoBody®-CD3xCD20)
October 28, 2022
AbbVie Announces Submissions of Regulatory Applications for Epcoritamab (DuoBody®-CD3xCD20) for the Treatment of Relapsed/Refractory Diffuse Large B-Cell Lymphoma (DLBCL) and Large B-Cell Lymphoma (LBCL)
- European Medicines Agency (EMA) validates AbbVie's Marketing Authorization Application; Genmab submits Biologics License Application to U.S. Food and Drug Administration (FDA)
- The submissions are supported by the EPCORE™ NHL-1 open-label, multi-center Phase 2 trial evaluating the safety and preliminary efficacy of subcutaneous epcoritamab in adult patients with relapsed, progressive or refractory CD20+ mature B-cell non-Hodgkin's lymphoma (NHL)
NORTH CHICAGO, Ill., Oct. 28, 2022 /PRNewswire/ -- AbbVie (NYSE: ABBV) today announced that the European Medicines Agency (EMA) has validated a Marketing Authorization Application (MAA) for epcoritamab (DuoBody®-CD3xCD20), an investigational subcutaneous bispecific antibody, for the treatment of adult patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL) after two or more lines of systemic therapy. Additionally, Genmab has submitted a Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA) for epcoritamab for the treatment of adult patients with R/R large B-cell lymphoma (LBCL) after two or more lines of systemic therapy.
The regulatory submissions are supported by previously announced results from the LBCL cohort of the EPCORE™ NHL-1 open-label, multi-center Phase 2 trial evaluating the safety and preliminary efficacy of investigational epcoritamab in adult patients with relapsed, progressive or refractory CD20+ mature B-cell non-Hodgkin's lymphoma (NHL), including DLBCL.
LBCL and its major subtype, DLBCL, are fast-growing types of NHL, a cancer that develops in the lymphatic system and affects B-cell lymphocytes, a type of white blood cell.1 DLBCL is the most common type of NHL worldwide and accounts for approximately 30 percent of all NHL cases globally.1 Because NHL affects B-cell lymphocytes, the disease and its subtypes are classified as B-cell malignancies.
"The regulatory submissions for epcoritamab exemplify our pursuit to deliver innovative care for people living with large B-cell lymphoma and diffuse large B-cell lymphoma who have limited treatment options," said Mohamed Zaki, M.D., Ph.D., vice president and head, global oncology development, AbbVie. "This achievement represents an initial step in our commitment to scientific research and providing an important treatment option with the potential to become a core therapy for people living with B-cell malignancies such as LBCL and DLBCL."
Epcoritamab is being co-developed by AbbVie and Genmab as part of the companies' oncology collaboration. The companies will share commercial responsibilities in the U.S. and Japan, with AbbVie responsible for further global commercialization. The companies are committed to evaluating epcoritamab as a monotherapy, and in combination, across lines of therapy in a range of hematologic malignancies, including an ongoing Phase 3, open-label, randomized trial evaluating epcoritamab as a monotherapy in patients with R/R DLBCL (NCT: 04628494).
About Diffuse Large B-cell Lymphoma (DLBCL)
DLBCL is a fast-growing type of non-Hodgkin's lymphoma (NHL) that affects B-cell lymphocytes, a type of white blood cell.1 It is the most common type of NHL worldwide and accounts for approximately 30 percent of all NHL cases.1 DLBCL can arise in lymph nodes, as well as in organs outside of the lymphatic system.1 The disease occurs more commonly in the elderly and is slightly more prevalent in men.1
About the EPCORE™ NHL-1 Trial
EPCORE™ NHL-1 is an open-label, multi-center safety and preliminary efficacy trial of epcoritamab that includes a Phase 1 first-in-human, dose escalation part; a Phase 2 expansion part; and an optimization part. The trial was designed to evaluate subcutaneous epcoritamab in patients with relapsed, progressive or refractory CD20+ mature B-cell NHL, including LBCL and DLBCL. Data from the dose escalation part of the study, which determined the recommended Phase 2 dose, were published in The Lancet in 2021. In the Phase 2 expansion part, additional patients were treated with epcoritamab to further explore the safety and efficacy of epcoritamab in three cohorts of patients with different types of relapsed/refractory B-cell NHLs who had limited therapeutic options.
The primary endpoint of the Phase 2 expansion part was overall response rate (ORR) as assessed by an independent review committee (IRC). Secondary efficacy endpoints included duration of response, complete response rate, progression-free survival, overall survival, time to response, time to next therapy, and rate of minimal residual disease negativity.
About Epcoritamab
Epcoritamab is an investigational IgG1-bispecific antibody created using Genmab's proprietary DuoBody® technology. Genmab's DuoBody®-CD3 technology is designed to direct cytotoxic T-cells selectively to elicit an immune response toward target cell types. Epcoritamab is designed to simultaneously bind to CD3 on T-cells and CD20 on B-cells, and induces T-cell mediated killing of CD20+ cells.2 CD20 is expressed on B-cells and is a clinically validated therapeutic target in many B-cell malignancies, including diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma and chronic lymphocytic leukemia.3,4 Epcoritamab is being co-developed by AbbVie and Genmab as part of the companies' oncology collaboration.
About AbbVie in Oncology
At AbbVie, we are committed to transforming standards of care for multiple blood cancers while advancing a dynamic pipeline of investigational therapies across a range of cancer types. Our dedicated and experienced team joins forces with innovative partners to accelerate the delivery of potential breakthrough medicines. We are evaluating more than 20 investigational medicines in over 300 clinical trials across some of the world's most widespread and debilitating cancers. As we work to have a remarkable impact on people's lives, we are committed to exploring solutions to help patients obtain access to our cancer medicines. For more information, please visit http://www.abbvie.com/oncology.
About AbbVie
AbbVie's mission is to discover and deliver innovative medicines that solve serious health issues today and address the medical challenges of tomorrow. We strive to have a remarkable impact on people's lives across several key therapeutic areas: immunology, oncology, neuroscience, eye care, virology, women's health and gastroenterology, in addition to products and services across its Allergan Aesthetics portfolio. For more information about AbbVie, please visit us at www.abbvie.com. Follow @abbvie on Twitter, Facebook, Instagram, YouTube and LinkedIn.
SOURCE AbbVie
Genmab files for approval of blood cancer drug in US, AbbVie gets review in EU
Oct. 28, 2022 9:29 AM ET
By: Ravikash, SA News Editor
- Genmab (GMAB) on Friday said it filed an application to the U.S. Food and Drug Administration (FDA) seeking approval of subcutaneous epcoritamab to treat patients with relapsed/refractory (R/R) large B-cell lymphoma (LBCL) who have received two or more lines of systemic therapy.
- Meanwhile, the European Medicines Agency (EMA) validated AbbVie's (NYSE:ABBV) marketing authorization application (MAA) for subcutaneous epcoritamab (DuoBody-CD3xCD20) to treat adult patients with R/R diffuse large B-cell lymphoma (DLBCL) after two or more lines of systemic therapy.
- https://seekingalpha.com/news/3897259-genmab-files-for-approval-of-blood-cancer-drug-in-us-abbvie-gets-review-in-eu
- https://seekingalpha.com/symbol/ABBV
- https://seekingalpha.com/symbol/GMAB
- https://www.abbvie.com/our-science/pipeline/gen-3013.html
- https://www.abbvie.com/
NERLYNX® (neratinib) tablets
Epcoritamab (DuoBody®-CD3xCD20)
NERLYNX® (neratinib) tablets
2022 News Releases
Download:
Oct. 27, 2022 - SUMMIT: EGFR Exon 18-mutant NSCLC Poster
Puma Biotechnology Presents Updated Findings from the Phase II SUMMIT Basket Trial of Neratinib in EGFR Exon 18-Mutant NSCLC at the 2022 EORTC/NCI/AACR Symposium
LOS ANGELES, Calif., Oct. 27, 2022 - Puma Biotechnology, Inc. (NASDAQ: PBYI), a biopharmaceutical company, presented updated findings from the Phase II SUMMIT basket trial of neratinib for EGFR exon 18-mutant non-small cell lung cancer (NSCLC) patients at the EORTC/NCI/AACR Molecular Targets and Cancer Therapeutics Symposium that is taking place in Barcelona, Spain. The poster, entitled, "Neratinib efficacy in patients with EGFR exon 18-mutant non-small cell lung cancer: findings from the SUMMIT basket trial,” was presented by Alejandro Martínez Bueno, Head of Medical Oncology Service, Hospital Quirón Deuxes, Barcelona, Spain, on October 27 beginning at 10:00 a.m. CEST.
The Phase II SUMMIT ‘basket’ trial is an open-label, multicenter, multi-national study evaluating the safety and efficacy of neratinib administered daily to patients who have solid tumors with activating, EGFR exon 18 or HER2 mutations. In the EGFR exon 18-mutant cohort, patients with lung cancer with single or complex EGFR exon 18 mutations, who were EGFR tyrosine kinase inhibitor (TKI) naïve or were previously exposed to EGFR TKI, were enrolled into this study and received 240 mg of neratinib monotherapy once daily. Anti-diarrheal prophylaxis with loperamide was required for the first 2 cycles.
This cohort of 29 patients had received 1-6 prior lines of therapy in the metastatic setting before entering the trial. Twenty-three patients (79%) had been previously treated with an EGFR-targeted TKI (e.g., afatinib, osimertinib).
The interim efficacy results showed that the objective response rate (ORR) was 35% overall, 30% in patients pretreated with TKIs, and 50% in patients not pretreated with TKIs. Response or stable disease lasting for ≥ 48 weeks was observed in 7 patients (6 PR, 1 SD). Final data will be presented at a later date.
The safety profile observed in the cohort of patients with EGFR exon 18-mutant NSCLC showed that for the 31 patients who received at least one dose of neratinib, diarrhea, constipation, and nausea were the most commonly reported adverse events. There were no reports of grade 4 diarrhea, 3 patients (10%) reported grade 3 diarrhea, and 1 patient (3%) permanently discontinued neratinib due to diarrhea.
Dr. Martínez, an investigator of the study from Hospital Quirón Deuxes, said, “We are very excited about these interim study results in patients with EGFR exon 18-mutant lung cancer, for whom treatment options are limited. This study shows that neratinib has the potential to be an efficacious and safe option to treat their disease, even following treatment with other TKIs and chemotherapy.”
Alan H. Auerbach, CEO and President of Puma Biotechnology, added, “We are very pleased to observe that treatment with neratinib led to meaningful responses in patients with EGFR exon 18- mutated NSCLC. Improving the lives of our cancer patients is our foremost goal, and we are pleased to see the benefit that was provided to these patients in the SUMMIT trial.”
About Puma Biotechnology
Puma Biotechnology, Inc. is a biopharmaceutical company with a focus on the development and commercialization of innovative products to enhance cancer care. Puma in-licenses the global development and commercialization rights to PB272 (neratinib, oral), PB272 (neratinib, intravenous) and PB357. Neratinib, oral was approved by the U.S. Food and Drug Administration in 2017 for the extended adjuvant treatment of adult patients with early stage HER2- overexpressed/amplified breast cancer, following adjuvant trastuzumab-based therapy, and is marketed in the United States as NERLYNX® (neratinib) tablets. In February 2020, NERLYNX was also approved by the FDA in combination with capecitabine for the treatment of adult patients with advanced or metastatic HER2-positive breast cancer who have received two or more prior anti- HER2-based regimens in the metastatic setting. NERLYNX was granted marketing authorization by the European Commission in 2018 for the extended adjuvant treatment of adult patients with early stage hormone receptor-positive HER2-overexpressed/amplified breast cancer and who are less than one year from completion of prior adjuvant trastuzumab-based therapy. NERLYNX is a registered trademark of Puma Biotechnology, Inc.
In September 2022, Puma entered into an exclusive license agreement for the development and commercialization of the anti-cancer drug alisertib, a selective, small molecule, orally administered inhibitor of aurora kinase A. Initially, Puma intends to focus the development of alisertib on the treatment of small cell lung cancer and breast cancer.
Further information about Puma Biotechnology may be found at www.pumabiotechnology.com.
To help ensure patients have access to NERLYNX, Puma has implemented the Puma Patient Lynx support program to assist patients and healthcare providers with reimbursement support and referrals to resources that can help with financial assistance. More information on the Puma Patient Lynx program can be found at https://www.NERLYNX.com or 1-855-816-5421.
INDICATIONS: NERLYNX® (neratinib) tablets, for oral use, is a kinase inhibitor indicated:
- As a single agent, for the extended adjuvant treatment of adult patients with early stage HER2-positive breast cancer, to follow adjuvant trastuzumab-based therapy.
- In combination with capecitabine, for the treatment of adult patients with advanced or metastatic HER2-positive breast cancer, who have received two or more prior anti-HER2 based regimens in the metastatic setting.
Please see Full Prescribing Information for additional safety information.
https://nerlynx.com/
Puma's Nerlynx shows promise in lung cancer patients in phase 2 trial
Oct. 27, 2022 7:05 AM ET
Puma Biotechnology, Inc. (PBYI)
By: Ravikash, SA News Editor
Puma Biotechnology (NASDAQ:PBYI) reported updated data from a phase 2 basket trial called SUMMIT of neratinib to treat patients with EGFR exon 18-mutant non-small cell lung cancer (NSCLC).
https://seekingalpha.com/symbol/PBYI
https://www.pumabiotechnology.com/index.html
Capivasertib plus Faslodex
TissueCypher® Barrett’s Esophagus Test
NERLYNX® (neratinib) tablets
Capivasertib plus Faslodex significantly improved progression-free survival vs. Faslodex in CAPItello-291 Phase III trial in advanced HR-positive breast cancer
PUBLISHED26 October 2022
26 October 2022 07:00 BST
Capivasertib, a potential first-in-class AKT inhibitor, combined with Faslodex could
become a new option for patients in this setting regardless of biomarker status
Positive high-level results from the CAPItello-291 Phase III trial showed that AstraZeneca’s capivasertib in combination with Faslodex (fulvestrant) demonstrated a statistically significant and clinically meaningful improvement in progression-free survival (PFS) versus placebo plus Faslodex in patients with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-low or negative locally advanced or metastatic breast cancer, following recurrence or progression on or after endocrine therapy (with or without a CDK4/6 inhibitor).
The trial met both primary endpoints, improving PFS in the overall patient population and in a prespecified biomarker subgroup of patients whose tumours had qualifying alterations in the PIK3CA, AKT1 or PTEN genes. Although the overall survival (OS) data were immature at the time of the analysis, early data are encouraging. The trial will continue to assess OS as a key secondary endpoint.
The safety profile of capivasertib plus Faslodex was similar to that observed in previous trials evaluating this combination.
Breast cancer is the most common cancer worldwide, with an estimated 2.3 million patients diagnosed in 2020.1 Approximately 70% of breast cancer tumours are considered HR-positive and HER2-low or negative.2 Endocrine therapies are widely used for the treatment of HR-positive breast cancer, but many patients with advanced disease develop resistance to 1st-line CDK4/6 inhibitors and estrogen receptor-targeting therapies, underscoring the need for additional options.3
Nicholas Turner, MD, PhD, Professor of Molecular Oncology at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, London, UK, and principal investigator in the CAPItello-291 Phase III trial, said: “The CAPItello-291 Phase III trial results show capivasertib offers a clinically meaningful improvement in progression free survival for patients with HR-positive breast cancer. This potential new medicine could give people more time with their cancer under control, which is a priority for patients and their families.”
Susan Galbraith, Executive Vice President, Oncology R&D, AstraZeneca, said: “These exciting data in an all-comers population indicate that capivasertib could become a new first-in-class treatment option for patients with HR-positive breast cancer. These patients often experience tumour progression on, or resistance to, available endocrine therapies for advanced disease and urgently need new therapies that extend the effectiveness of endocrine-based treatment approaches.”
The data will be presented at a forthcoming medical meeting and shared with global health authorities.
AstraZeneca has a comprehensive portfolio of approved and potential new medicines in development for patients with breast cancer. In addition to these results, the Company is also announcing today results from the SERENA-2 Phase II trial of camizestrant, the next-generation oral selective estrogen receptor degrader (ngSERD) in advanced estrogen receptor (ER)-positive breast cancer.
Notes
HR-positive breast cancer
HR-positive breast cancer (expressing estrogen or progesterone receptors, or both), is the most common subtype of breast cancer, and the growth of HR-positive breast cancer cells is often driven by ER.2,4,5 Endocrine therapies that target ER-driven disease are widely used as 1st-line treatment for this form of breast cancer in the advanced setting, and often paired with cyclin-dependent kinase (CDK) 4/6 inhibitors. However, resistance to CDK4/6 inhibitors and current endocrine therapies develops in many patients with advanced disease and treatment options are limited.3 Optimising endocrine therapy and overcoming resistance for patients with ER-driven disease at all stages of treatment are active areas of focus for breast cancer research.
CAPItello-291
CAPItello-291 is a Phase III, double-blind, randomised trial that is part of a larger clinical programme focused on capivasertib, an investigational AKT (serine/threonine kinase) inhibitor. CAPItello-291 is evaluating the efficacy of capivasertib in combination with Faslodex versus placebo plus Faslodex for the treatment of locally advanced (inoperable) or metastatic HR-positive, HER2-low or negative breast cancer.
The global trial enrolled 708 adult patients with histologically confirmed HR-positive, HER2-low or negative breast cancer whose disease has recurred or progressed during or after aromatase inhibitor therapy, with or without a CDK4/6 inhibitor, and up to one line of chemotherapy for advanced disease. The trial has dual primary endpoints of PFS in the overall patient population and in a subgroup of patients whose tumours have qualifying alterations in the PIK3CA, AKT1 or PTEN genes. In the trial, approximately 40% of tumours had PI3K/AKT/PTEN alterations.
Capivasertib
Capivasertib is an investigational oral treatment currently in Phase III trials for the treatment of multiple subtypes of breast cancer, prostate cancer and a Phase II trial for haematologic malignancies. A potent, selective adenosine triphosphate (ATP)-competitive inhibitor of all three AKT isoforms (AKT1/2/3), capivasertib is being evaluated in combination with existing therapies in tumours harbouring alterations in the PI3K/AKT/PTEN pathway, and in tumours reliant on signalling via this pathway for survival. Capivasertib is dosed according to an intermittent schedule, which consists of four days on and three days off. This was chosen in early phase trials based on tolerability and the degree of target inhibition.
The capivasertib clinical research programme is investigating the safety and efficacy of capivasertib when used in combination with established treatment regimens.
Capivasertib was discovered by AstraZeneca subsequent to a collaboration with Astex Therapeutics (and its collaboration with the Institute of Cancer Research and Cancer Research Technology Limited).
AstraZeneca in breast cancer
Driven by a growing understanding of breast cancer biology, AstraZeneca is starting to challenge, and redefine, the current clinical paradigm for how breast cancer is classified and treated to deliver even more effective treatments to patients in need – with the bold ambition to one day eliminate breast cancer as a cause of death.
AstraZeneca has a comprehensive portfolio of approved and promising compounds in development that leverage different mechanisms of action to address the biologically diverse breast cancer tumour environment.
With Enhertu (trastuzumab deruxtecan), a HER2-directed ADC, AstraZeneca and Daiichi Sankyo are aiming to improve outcomes in previously treated HER2-positive and HER2-low metastatic breast cancer and are exploring its potential in earlier lines of treatment and in new breast cancer settings.
In HR-positive breast cancer, AstraZeneca continues to improve outcomes with foundational medicines Faslodex (fulvestrant) and Zoladex (goserelin) and aims to reshape the HR-positive space with ngSERD and potential new medicine camizestrant as well as a potential first-in-class AKT kinase inhibitor, capivasertib. AstraZeneca is also collaborating with Daiichi Sankyo to explore the potential of TROP2-directed ADC, datopotamab deruxtecan, in this setting.
PARP inhibitor Lynparza (olaparib) is a targeted treatment option that has been studied in early and metastatic breast cancer patients with an inherited BRCA mutation. AstraZeneca with MSD (Merck & Co., Inc. in the US and Canada) continue to research Lynparza in metastatic breast cancer patients with an inherited BRCA mutation and are exploring new opportunities to treat these patients earlier in their disease.
To bring much-needed treatment options to patients with triple-negative breast cancer, an aggressive form of breast cancer, AstraZeneca is testing immunotherapy Imfinzi (durvalumab) in combination with other oncology medicines, including Lynparza and Enhertu, evaluating the potential of capivasertib in combination with chemotherapy, and datopotamab deruxtecan.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the ambition to provide cures for cancer in every form, following the science to understand cancer and all its complexities to discover, develop and deliver life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers. It is through persistent innovation that AstraZeneca has built one of the most diverse portfolios and pipelines in the industry, with the potential to catalyse changes in the practice of medicine and transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day, eliminate cancer as a cause of death.
AstraZeneca
AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on Twitter @AstraZeneca.
AstraZeneca's capivasertib shows survival benefit, meets main goals of breast cancer study
Oct. 26, 2022 5:28 AM ET
By: Ravikash, SA News Editor
AstraZeneca (NASDAQ:AZN) said its drug capivasertib in combination with Faslodex showed survival benefit in certain patients with breast cancer cancer in a phase 3 trial and become a new option for patients in this setting regardless of biomarker status.
The study called CAPItello-291 enrolled 708 adult patients.
https://seekingalpha.com/symbol/AZN
TECVAYLI™ (teclistamab-cqyv)
TissueCypher® Barrett’s Esophagus Test
TissueCypher® Barrett’s Esophagus Test
U.S. FDA Approves TECVAYLI (teclistamab-cqyv), the First Bispecific T-cell Engager Antibody for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
Oct 25, 2022United States
TECVAYLI™, an off-the-shelf, subcutaneous therapy, is an important new medicine for patients with incurable blood cancer who face limited treatment options
HORSHAM, Pa., October 25, 2022 – The Janssen Pharmaceutical Companies of Johnson & Johnson announced today that the U.S. Food and Drug Administration (FDA) approved TECVAYLI™ (teclistamab-cqyv) for the treatment of adult patients with relapsed or refractory multiple myeloma, who previously received four or more prior lines of therapy, including a proteasome inhibitor, immunomodulatory drug and anti-CD38 monoclonal antibody.[1] TECVAYLI™ is a first-in-class, bispecific T-cell engager antibody that is administered as a subcutaneous treatment.1 This off-the-shelf (or ready to use) therapy uses innovative science to activate the immune system by binding to the CD3 receptor expressed on the surface of T-cells and to the B-cell maturation antigen (BCMA) expressed on the surface of multiple myeloma cells and some healthy B-lineage cells.1
This indication is approved under accelerated approval based on response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s).1
TECVAYLI™ is Janssen’s fourth approved treatment for multiple myeloma, further diversifying the company’s industry-leading oncology portfolio and deepening its commitment to discovering and developing therapies for this rare blood cancer.
“We are greatly encouraged by the FDA’s approval of teclistamab and Janssen’s commitment to the multiple myeloma community,” said Michael Andreini, President and CEO of the Multiple Myeloma Research Foundation. “Multiple myeloma is a life-threatening disease with considerable unmet need, and teclistamab is an important new treatment option for patients who have faced multiple relapses.”
The pivotal Phase 2 MajesTEC-1 clinical trial included patients who had received a median of five prior lines of therapy (n=110).1 An overall response rate (ORR) of 61.8 percent (95 percent Confidence Interval [CI]: 52.1 percent, 70.9 percent) was achieved, notably with 28.2 percent of patients achieving a complete response (CR) or better (CR or stringent complete response [sCR]).1 The median time to first response was 1.2 months (range 0.2 to 5.5 months). With a median follow-up of 7.4 months, the estimated duration of response (DOR) rate was 90.6 percent (95 percent CI: 80.3 percent, 95.7 percent) at six months and 66.5 percent (95 percent CI: 38.8 percent, 83.9 percent) at nine months.1 The study included heavily pretreated patients, and 78 percent of patients received four or more prior lines of therapy.1 All patients were triple-class exposed (to a proteasome inhibitor, an immunomodulatory agent and an anti-CD38 monoclonal antibody), and 76 percent were triple-class refractory (to a proteasome inhibitor, an immunomodulatory agent and an anti-CD38 monoclonal antibody).1
“Today’s achievement, which marks an important addition to our diverse and growing oncology portfolio, strengthens our resolve to discover and develop much-needed cancer treatments for patients and physicians,” said Peter Lebowitz, M.D., Ph.D., Global Therapeutic Area Head, Oncology, Janssen Research & Development, LLC. “The approval of TECVAYLI, which demonstrated an overall response rate of more than 60 percent in heavily pretreated patients, underscores our commitment to translate science into medicines as we strive toward our goal of one day eliminating this disease.”
The Safety Information for TECVAYLI™ includes a boxed warning for Cytokine Release Syndrome (CRS) and Neurologic Toxicity including immune effector cell-associated neurotoxicity syndrome in addition to warnings and precautions for hepatotoxicity, infections, neutropenia, hypersensitivity and other administrative reactions and embryo-fetal toxicity.1 The most common adverse reactions (>20%) in the safety population of MajesTEC-1 (n=165) were pyrexia, CRS, musculoskeletal pain, injection site reaction, fatigue, upper respiratory tract infection, nausea, headache, pneumonia, and diarrhea.1 The most common Grade 3 to 4 laboratory abnormalities (>20%) were decreased lymphocytes, decreased neutrophils, decreased white blood cells, decreased hemoglobin and decreased platelets.1 TECVAYLI™ is available only through a restricted program called the TECVAYLI™ Risk Evaluation and Mitigation Strategy.1 Details of the Important Safety Information are included below. TECVAYLI™ is supplied as 30mg/3mL and 153mg/1.7mL single-dose vials.1
“In the pivotal teclistamab study, we have continued to observe positive results in heavily pretreated patients with relapsed or refractory multiple myeloma,” said Ajai Chari, M.D., Professor of Medicine, Division of Hematology and Medical Oncology at the Icahn School of Medicine at Mount Sinai and study investigator.‡ “As a clinician and researcher, I see first-hand the human toll of this incurable disease. The approval of teclistamab, as the first bispecific antibody in relapsed or refractory multiple myeloma, is a meaningful step in helping many of these hard-to-treat patients.”
About the MajesTEC-1 Study1
MajesTEC-1 (NCT04557098, NCT03145181), is a Phase 1/2 single-arm, open-label, multicohort, multicenter dose-escalation study to evaluate the safety and efficacy of TECVAYLI™ in adults with relapsed or refractory multiple myeloma who received three or more prior lines of therapy.
Phase 1 of the study (NCT03145181) was conducted in two parts: dose escalation (Part 1) and dose expansion (Part 2). It evaluated safety, tolerability, pharmacokinetics and preliminary efficacy of TECVAYLI™ in adult participants with relapsed or refractory multiple myeloma. Study criteria excluded patients who had stroke, seizure, allogenic stem cell transplantation within the past six months, Eastern Cooperative Oncology Group (ECOG) performance score of 2 or higher, known active CNS involvement or clinical signs of meningeal involvement of multiple myeloma, or active or documented history of autoimmune disease, with the exception of vitiligo, Type 1 diabetes, and prior autoimmune thyroiditis.
Phase 2 of the study (NCT04557098) evaluated the efficacy of TECVAYLI™ at the recommended phase 2 dose (RP2D), established at subcutaneous 1.5 mg/kg weekly, as measured by ORR. During week one, participants received step-up doses of TECVAYLI™ subcutaneous (0.06 and 0.3 mg/kg). Subsequently, participants received weekly treatment doses of TECVAYLI™ subcutaneous 1.5 mg/kg until disease progression or unacceptable toxicity. Efficacy was established based on ORR as determined by the Independent Review Committee (IRC) assessment using International Myeloma Working Group (IMWG) 2016 criteria.
The primary endpoint was overall response rate or unacceptable toxicity. Secondary endpoints included duration of response, very good partial response, complete response, stringent complete response, time to response, minimal residual disease status, progression-free survival, overall survival, safety, pharmacokinetics, immunogenicity and patient-reported outcomes.
TECVAYLI™ Important Safety Information
WARNING: CYTOKINE RELEASE SYNDROME and NEUROLOGIC TOXICITY including IMMUNE EFFECTOR CELL-ASSOCIATED NEUROTOXICITY SYNDROME
Cytokine release syndrome (CRS), including life-threatening or fatal reactions, can occur in patients receiving TECVAYLI™. Initiate treatment with TECVAYLI™ step-up dosing schedule to reduce risk of CRS. Withhold TECVAYLI™ until CRS resolves or permanently discontinue based on severity.
Neurologic toxicity, including Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) and serious and life-threatening reactions, can occur in patients receiving TECVAYLI™. Monitor patients for signs or symptoms of neurologic toxicity, including ICANS, during treatment and treat promptly. Withhold TECVAYLI™ until neurologic toxicity resolves or permanently discontinue based on severity.
TECVAYLI™ is available only through a restricted program called the TECVAYLI™ Risk Evaluation and Mitigation Strategy (REMS).
Please read full Prescribing Information including Boxed Warning for TECVAYLI™.
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we’re creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular, Metabolism, & Retina; Immunology; Infectious Diseases & Vaccines; Neuroscience; Oncology; and Pulmonary Hypertension.
Learn more at www.janssen.com. Follow us at @JanssenGlobal and @JanssenUS. Janssen Research & Development, LLC and Janssen Biotech, Inc. are part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
Johnson & Johnson wins FDA approval for multiple myeloma therapy
Oct. 25, 2022 4:01 PM ET
By: Dulan Lokuwithana, SA News Editor
- The Janssen Pharmaceutical unit of Johnson & Johnson (NYSE:JNJ) announced Tuesday that the FDA granted accelerated approval for Tecvayli as a treatment for adult patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy.
- https://seekingalpha.com/news/3895052-johnson-johnson-wins-fda-approval-for-multiple-myeloma-therapy
- https://seekingalpha.com/symbol/JNJ
- https://www.jnj.com/
TissueCypher® Barrett’s Esophagus Test
TissueCypher® Barrett’s Esophagus Test
TissueCypher® Barrett’s Esophagus Test
New Data Demonstrate that the Utilization of TissueCypher® Barrett’s Esophagus Test Results Can Significantly Improve the Management of Low-Grade Dysplasia in Patients with Barrett’s Esophagus over the Standard of Care Alone
10/25/2022
Data presented at the 2022 American College of Gastroenterology (ACG 2022) Annual Scientific Meeting
FRIENDSWOOD, Texas--(BUSINESS WIRE)-- Castle Biosciences, Inc. (Nasdaq: CSTL), a company improving health through innovative tests that guide patient care, today announced new data showing that the use of TissueCypher® Barrett’s Esophagus Test results can significantly improve management decisions for Barrett’s esophagus (BE) patients with low-grade dysplasia (LGD)to improve health outcomes. TissueCypher is Castle’s precision medicine test designed to predict future development of high-grade dysplasia (HGD) and/or esophageal adenocarcinoma (EAC) within five years for patients diagnosed with BE.
Overall, the study results suggest that TissueCypher may be used to standardize the management of BE patients with LGD to improve health outcomes, by helping ensure that patients at a high risk of progression receive earlier interventions and by potentially reducing unnecessary use of endoscopic eradication therapy (EET) and endoscopies for lower risk patients.
“A diagnosis of low-grade dysplasia in Barrett’s esophagus warrants expert pathology review, as these patients may have a significant risk of developing esophageal cancer. However, expert pathology review lacks standard criteria, is highly variable and is fraught with logistical challenges,” said Lucas C. Duits, M.D., Ph.D., Department of Gastroenterology and Hepatology at University Medical Center in Amsterdam, The Netherlands. “The use of TissueCypher test results can reduce inconsistencies in management decisions for Barrett’s esophagus patients with low-grade dysplasia. We believe there are potential implications to this finding, including a reduction in the incidence and mortality of esophageal cancer and a reduction in the use of unnecessary clinical treatments, when appropriate.”
The study results were shared in a podium presentation at the 2022 American College of Gastroenterology (ACG2022) Annual Scientific Meeting, being held Oct. 21-26 in Charlotte, North Carolina. The presentation was titled “An Objective Spatialomics Test Standardizes Management Decisions with Potential to Improve Outcomes for Barrett’s Esophagus Patients,” and was given by Lucas C. Duits, M.D., Ph.D.
The study involved a cohort of 154 real patients with known outcomes who were followed prospectively as part of the SURF trial. Twenty-four of these patients progressed to HGD/EAC within five years. Each patient’s baseline specimens were independently reviewed by 30 pathologists from five countries and also tested with TissueCypher in a blinded manner. Management decision simulations were performed, where each patient's baseline specimens were first evaluated by a generalist pathologist, and then referred to an expert pathologist from the same country for any diagnoses of LGD. In one arm of the study, management for the patients was determined by the current standard of care, which includes pathology review of tissue samples and management according to current guidelines. In the other arm, patients were managed by the current standard of care with additional guidance from TissueCypher test results. The percentage of patients receiving appropriate management per their known outcome was compared between the two study arms, with appropriate management defined as:
- Three- to five-year surveillance for patients who did not progress to HGD/EAC during surveillance; and
- Either surveillance in less than one year or EET for patients who did progress to HGD/EAC during surveillance.
The study results showed the following:
- Using TissueCypher test results to guide patient management decisions significantly increased the likelihood of BE patients with LGD receiving appropriate management per their known outcome (p=0.0007). 58.4% of patients had a 100% chance of receiving appropriate management when TissueCypher test results were used to guide decisions despite different pathologists reviewing their baseline specimens, compared to 9.1% of patients who were managed according to the standard of care pathology review alone.
- Use of TissueCypher test results improved the consistency of management decisions for BE patients with LGD by reducing the impact of variable pathology review (p<0.0001). 57.1% of patients whose care was guided with the addition of TissueCypher test results had no deviation in management decisions when different pathologists reviewed their baseline specimens, compared to 7.1% of patients whose management was guided only by the current standard of care.
About TissueCypher® Barrett’s Esophagus Test
The TissueCypher Barrett’s Esophagus test is Castle’s precision medicine test designed to predict future development of high-grade dysplasia (HGD) and/or esophageal cancer in patients with Barrett’s esophagus (BE). TissueCypher is indicated for use in patients with endoscopic biopsy confirmed BE that is graded non-dysplastic (ND), indefinite for dysplasia (IND) or low-grade dysplasia (LGD); its clinical performance has been supported by nine peer-reviewed publications of BE progressor patients with leading clinical centers around the world. The TissueCypher Barrett’s Esophagus Assay is a proprietary Laboratory Developed Test with its own unique CPT PLA code (0108U) and has been on the Medicare Clinical Laboratory Fee Schedule since January 2021. Additionally, the test received Advanced Diagnostic Laboratory Test (ADLT) status from the Centers for Medicare & Medicaid Services (CMS) in March 2022.
About Castle Biosciences
Castle Biosciences (Nasdaq: CSTL) is a leading diagnostics company improving health through innovative tests that guide patient care. The Company aims to transform disease management by keeping people first: patients, clinicians, employees and investors.
Castle’s current portfolio consists of tests for skin cancers, uveal melanoma, Barrett’s esophagus and mental health conditions. Additionally, the Company has active research and development programs for tests in other diseases with high clinical need, including its test in development to predict systemic therapy response in patients with moderate-to-severe psoriasis, atopic dermatitis and related conditions. To learn more, please visit www.CastleBiosciences.com and connect with us on LinkedIn, Facebook, Twitter and Instagram.
DecisionDx-Melanoma, DecisionDx-CMSeq, DecisionDx-SCC, MyPath Melanoma, DiffDx-Melanoma, DecisionDx-UM, DecisionDx-PRAME, DecisionDx-UMSeq, TissueCypher and IDgenetix are trademarks of Castle Biosciences, Inc.
Source: Castle Biosciences, Inc.
Castle Biosciences rises on new data for TissueCypher esophageal cancer test
Oct. 25, 2022 1:45 PM ET
Castle Biosciences, Inc. (CSTL)
By: Dulan Lokuwithana, SA News Editor
Castle Biosciences, Inc. (NASDAQ:CSTL), a cancer-focused diagnostics company, added ~8% on Tuesday after announcing new data supporting its TissueCypher test, which is designed to predict high-grade dysplasia (HGD) and/or esophageal cancer in patients with Barrett’s esophagus (BE).
https://seekingalpha.com/symbol/CSTL
https://castlebiosciences.com/
biotecHOPE™ 2022
VAX-24
Quizartinib
Quizartinib
Vaxcyte Reports Positive Topline Data from Phase 1/2 Proof-of-Concept Study of its 24-Valent Pneumococcal Conjugate Vaccine Candidate Being Investigated for the Prevention of Invasive Pneumococcal Disease in Adults Aged 18-64
October 24, 2022PDF Version
-- In the Study, VAX-24 Demonstrated a Safety and Tolerability Profile Similar to Prevnar 20™ (PCV20) at All Doses Studied --
-- All 24 Serotypes of VAX-24 at Conventional 2.2mcg PCV Dose Met or Exceeded Regulatory Immunogenicity Standards --
-- All 20 VAX-24 Serotypes Common with PCV20 Met Standard OPA Response Non-Inferiority Criteria, of Which 16 Achieved Higher Immune Responses, at 2.2mcg VAX-24 Dose --
-- All 4 Serotypes Unique to VAX-24 Exceeded Standard Superiority Criteria --
-- Vaxcyte to Advance Potential Best-in-Class VAX-24 Clinical Program in Adult and Pediatric Populations --
-- Company to Host Webcast/Conference Call Today at 8:00 a.m. ET / 5:00 a.m. PT --
SAN CARLOS, Calif., Oct. 24, 2022 (GLOBE NEWSWIRE) -- Vaxcyte, Inc. (Nasdaq: PCVX), a clinical-stage vaccine innovation company engineering high-fidelity vaccines to protect humankind from the consequences of bacterial diseases, today announced positive topline results from the Phase 1/2 clinical proof-of-concept study evaluating the safety, tolerability and immunogenicity of VAX-24, the Company’s investigational 24-valent pneumococcal conjugate vaccine (PCV), in healthy adults aged 18-64. In this study, VAX-24 met the primary safety and tolerability objectives, demonstrating a safety profile similar to Prevnar 20TM (PCV20) for all doses studied.
In the study, VAX-24 met or exceeded the established regulatory immunogenicity standards for all 24 serotypes at the conventional 2.2mcg dose, which the Company intends to move forward into a Phase 3 program. At this dose, VAX-24 met the standard opsonophagocytic activity (OPA) response non-inferiority criteria for all 20 serotypes common with PCV20, of which 16 achieved higher immune responses. Additionally, at all three doses, VAX-24 met the standard superiority criteria for all four serotypes unique to VAX-24. These four incremental serotypes cover 10-15 percent of strains causing invasive pneumococcal disease (IPD) over the current standard-of-care in adults.
“We are thrilled with these positive topline results from our Phase 1/2 proof-of-concept study, which met all of our objectives. The findings indicate a potential best-in-class profile for VAX-24 and validate our carrier-sparing approach to enable the development of broader-spectrum PCVs,” said Grant Pickering, Chief Executive Officer and Co-Founder of Vaxcyte. “The study results demonstrate that VAX-24 has the potential to provide broader coverage and better immune responses relative to the standard-of-care. We believe this presents an opportunity to set a new bar for immunogenicity standards for pneumococcal vaccines.”
Key Topline Study Results
Safety and Tolerability Findings:
- VAX-24 demonstrated a safety and tolerability profile similar to PCV20 at all doses studied.
- Frequently reported local and systemic reactions were generally mild-to-moderate, resolving within several days of vaccination, with no difference observed across the cohorts. No serious adverse events or new onset chronic illnesses were considered to be related to study vaccines.
- The full six-month safety follow-up is ongoing for the Phase 2 portion of the study.
Immunogenicity Findings:
- VAX-24 demonstrated robust OPA and immunoglobulin G (IgG) immune responses for all 24 serotypes at all doses studied (1.1mcg, 2.2mcg, 2.2mcg/4.4mcg), each of which could advance into Phase 3.
- The VAX-24 2.2mcg dose met or exceeded the established regulatory immunogenicity standards for all 24 serotypes and is the dose the Company expects to advance into Phase 3.
- At the 2.2mcg dose, VAX-24 met the standard OPA response non-inferiority criteria(1) for all 20 serotypes common with PCV20, of which 16 serotypes (3, 4, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 23F and 33F) achieved higher immune responses and four serotypes (9V, 18C, 19F and 33F) reached statistical significance.
- At all three doses, VAX-24 met the standard superiority criteria(2) for all four serotypes (2, 9N, 17F and 20B) unique to VAX-24.
“We are very excited to share these strong clinical results from our proof-of-concept study, which validate the potential for VAX-24 to improve upon the standard-of-care for adults by potentially providing 10-15 percent incremental protection for this serious disease. The 24 serotypes included in VAX-24 cover a significant portion of the IPD currently in circulation and are associated with high case-fatality rates, antibiotic resistance and meningitis,” said Jim Wassil, Executive Vice President and Chief Operating Officer of Vaxcyte. “On behalf of our team at Vaxcyte, we would like to gratefully acknowledge the efforts of everyone involved in this program, especially the trial investigators, trial sites and study participants.”
About the Phase 1/2 Clinical Proof-of-Concept Study
The VAX-24 Phase 1/2 clinical proof-of-concept study is a randomized, observer-blind, dose-finding, controlled study designed to evaluate the safety, tolerability and immunogenicity of VAX-24 in healthy adults 18-64 years of age.
The Phase 1 portion of the study evaluated the safety and tolerability of a single injection of VAX-24 at three dose levels, 1.1mcg, 2.2mcg and 2.2mcg/4.4mcg, and compared to PCV20 in 64 healthy adults 18 to 49 years of age.
The Phase 2 portion evaluated the safety, tolerability and immunogenicity of a single injection of VAX-24 at the same three dose levels and compared to a single injection of PCV20 in 771 healthy adults 50 to 64 years of age. The immunogenicity objectives of the Phase 2 portion of the study include an assessment of the induction of antibody responses, using OPA and IgG, at each of the three VAX-24 doses and compared to PCV20, and for the additional four serotypes contained in VAX-24 (and Pneumovax® 23), but not in PCV20, the percentage of subjects that experience a four-fold rise in antibody titers. Participants in the study will be evaluated for safety through six months after vaccination. Additional information about the study can be found at www.clinicaltrials.gov under the identifier NCT05266456.
VAX-24 Adult Program
- Topline safety, tolerability and immunogenicity data from the Phase 2 study in adults 65 and older are anticipated in the first half of 2023.
- Final results with the 6-month safety data of the Phase 2 adult studies are anticipated in the first half of 2023.
- Regulatory interactions to inform the Phase 3 program are anticipated in the second half of 2023.
- Topline safety, tolerability and immunogenicity data from the Phase 3 non-inferiority study in adults are expected in 2025.
VAX-24 Pediatric Program
- The infant Investigational New Drug (IND) application submission and the Phase 2 study initiation are both anticipated in first half of 2023.
- Topline safety, tolerability and immunogenicity data from the infant Phase 2 study primary 3-dose immunization series are expected by 2025.
VAX-XP Adult Program
- The IND application submission for VAX-XP, Vaxcyte’s PCV candidate with 31 strains, is anticipated in the second half of 2023.
- Topline safety, tolerability and immunogenicity data from a Phase 1/2 study in adults are expected in 2024.
About VAX-24
VAX-24 is an investigational 24-valent PCV candidate designed to prevent IPD, which can be most serious for infants, young children, older adults and those with immune deficiencies or certain chronic health conditions. The public health community continues to affirm the need for vaccines that offer broader protection to prevent IPD. VAX-24 is intended to improve upon the standard-of-care PCVs for both children and adults by covering the serotypes that are responsible for most of the pneumococcal disease currently in circulation. Vaxcyte aims to efficiently create and deliver high-fidelity, broad-spectrum vaccines, such as VAX-24, by using modern synthetic techniques, including advanced chemistry and the XpressCFTM cell-free protein synthesis platform. Vaxcyte is deploying this approach with VAX-24 in order to add more pneumococcal strains without compromising the overall immune response.
In August 2022, the FDA granted Fast Track Designation to VAX-24 for the adult indication. The Fast Track designation is an FDA process that has been designed to expedite the development and review of drugs, including vaccines, that treat or prevent serious conditions and fill an important unmet medical need.
About Vaxcyte
Vaxcyte is a vaccine innovation company engineering high-fidelity vaccines to protect humankind from the consequences of bacterial diseases. The Company is developing broad-spectrum conjugate and novel protein vaccines to prevent or treat bacterial infectious diseases. Vaxcyte’s lead candidate, VAX-24, is a 24-valent, broad-spectrum pneumococcal conjugate vaccine being developed for the prevention of IPD. Vaxcyte is re-engineering the way highly complex vaccines are made through modern synthetic techniques, including advanced chemistry and the XpressCFTM cell-free protein synthesis platform, exclusively licensed from Sutro Biopharma, Inc. Unlike conventional cell-based approaches, the Company’s system for producing difficult-to-make proteins and antigens is intended to accelerate its ability to efficiently create and deliver high-fidelity vaccines with enhanced immunological benefits. Vaxcyte’s pipeline also includes VAX-XP, a PCV with coverage of 31 strains; VAX-A1, a prophylactic vaccine candidate designed to prevent Group A Strep infections; and VAX-PG, a therapeutic vaccine candidate designed to slow or stop the progression of periodontal disease. Vaxcyte is driven to eradicate or treat invasive bacterial infections, which have serious and costly health consequences when left unchecked. For more information, visit www.vaxcyte.com.
Vaxcyte climbs 70% after pneumococcal vaccine data
Oct. 24, 2022 1:45 PM ET
By: Dulan Lokuwithana, SA News Editor2 Comments
- Vaxcyte (NASDAQ:PCVX) added ~70% intraday on Monday to reach the highest level since November 2020 after the clinical-stage vaccine developer announced promising data from a Phase 1/2 clinical study for its experimental 24-valent pneumococcal vaccine (PCV), VAX-24.
- https://seekingalpha.com/news/3894235-pcvx-stock-climbs-after-pneumococcal-vaccine-data
- https://seekingalpha.com/symbol/PCVX
- https://vaxcyte.com/pipeline/
Quizartinib
Quizartinib
Quizartinib
Quizartinib Granted Priority Review in the U.S. for Patients with Newly Diagnosed FLT3-ITD Positive Acute Myeloid Leukemia • Submission based on QuANTUM-First results showing quizartinib plus chemotherapy significantly improved overall survival compared to chemotherapy alone Tokyo and Basking Ridge, NJ – (October 24, 2022) – Daiichi Sankyo (TSE: 4568) received notification of acceptance by the U.S. Food and Drug Administration (FDA) of the New Drug Application (NDA) of quizartinib in combination with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and as continuation monotherapy following consolidation, for the treatment of adult patients with newly diagnosed acute myeloid leukemia (AML) that is FLT3-ITD positive. The application has been granted Priority Review. The FDA grants Priority Review to applications for medicines that, if approved, would offer significant improvements over available options by demonstrating safety or efficacy improvements, preventing serious conditions or enhancing patient compliance. The Prescription Drug User Fee Act date (PDUFA), the FDA action date for their regulatory decision, is April 24, 2023. The Priority Review follows receipt of Fast Track Designation, granted by the FDA in March 2022 for quizartinib in newly diagnosed FLT3-ITD positive AML. AML is one of the most common forms of leukemia in adults.1 An estimated 20,050 new cases of AML will be diagnosed in the U.S. in 2022, and the five-year overall survival rate is reported at 30.5%. 1,2 Of all newly diagnosed cases of AML, approximately 25% have the FLT3-ITD mutation, which is associated with particularly unfavorable prognosis including increased risk of relapse and shorter overall survival.3 “There is a need for new targeted therapy options for patients with acute myeloid leukemia and the results of the QuANTUM-First trial showed that quizartinib in combination with standard chemotherapy has potential to change the current standard of care for newly diagnosed patients with the historically difficultto-treat FLT3-ITD subtype,” said Ken Takeshita, MD, Global Head, R&D, Daiichi Sankyo. “The FDA’s prioritization of this application reflects the importance of the data, and we will continue to work with the FDA and other global regulatory authorities to support the review of quizartinib for the treatment of patients with newly diagnosed FLT3-ITD positive acute myeloid leukemia.” 2 The NDA is based on data from the QuANTUM-First phase 3 trial presented at the Presidential Symposium of the European Hematology Association (EHA) 2022 Congress. In QuANTUM-First, quizartinib combined with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and continued as monotherapy following consolidation, demonstrated a statistically significant and clinically meaningful improvement in overall survival in adult patients with newly diagnosed FLT3-ITD positive AML compared to chemotherapy alone. The safety of quizartinib combined with intensive chemotherapy and as continuation monotherapy in QuANTUM-First was generally manageable with no new safety signals observed. The incidence of grade ≥3 QT prolongation events was low, with uncommon ventricular arrythmia events. Overall, the risk of QT prolongation was manageable with ECG monitoring, quizartinib dose modification and correction/elimination of additional risk factors. About QuANTUM-First QuANTUM-First is a randomized, double-blind, placebo-controlled global phase 3 study evaluating quizartinib in combination with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and as continuation monotherapy following consolidation, in adult patients aged 18-75 with newly diagnosed FLT3-ITD positive AML. Patients were randomized 1:1 into two treatment groups to receive quizartinib or placebo combined with anthracycline- and cytarabine-based regimens. Eligible patients, including those who underwent hematopoietic stem cell transplant (HSCT), continued with quizartinib or placebo for up to 36 cycles. The primary study endpoint was overall survival. Secondary endpoints include event-free survival, postinduction rates of complete remission (CR) and composite complete remission (CRc), and the percentage of patients who achieve CR or CRc with FLT3-ITD minimal residual disease negativity. Safety and pharmacokinetics, along with exploratory efficacy and biomarker endpoints, also were evaluated. QuANTUM-First enrolled 539 patients at 193 study sites across Asia, Europe, North America, Oceania and South America. For more information, visit ClinicalTrials.gov. About Acute Myeloid Leukemia More than 474,500 new cases of leukemia were reported globally i
About FLT3-ITD FLT3 (FMS-like tyrosine kinase 3) is a tyrosine kinase receptor protein normally expressed by hematopoietic stem cells that plays an important role in cell development, promoting cell survival, growth and differentiation through various signaling pathways. 3 Mutations of the FLT3 gene, which occur in approximately 30% of AML patients, can drive oncogenic signaling.3 FLT3-ITD (internal tandem duplication) is the most common type of FLT3 mutation in AML, occurring in about 25% of all newly diagnosed patients, and is associated with increased risk of relapse and shorter overall survival.3 About Quizartinib Quizartinib is an oral, highly potent and selective type II FLT3 inhibitor currently in clinical development for treatment of FLT3-ITD positive AML.3 In addition to QuANTUM-First, the quizartinib development program includes a phase 1/2 trial in pediatric and young adult patients with relapsed/refractory FLT3-ITD positive AML in Europe and North America. Several phase 1/2 combination studies with quizartinib also are underway at The University of Texas MD Anderson Cancer Center as part of a strategic research collaboration focused on accelerating development of Daiichi Sankyo pipeline therapies for AML. In addition to U.S. FDA Priority Review, quizartinib has received Fast Track Designation from the FDA for the treatment of adult patients with newly diagnosed AML that is FLT3-ITD positive, in combination with standard cytarabine and anthracycline induction and cytarabine consolidation chemotherapy. Orphan Drug Designation has been granted to quizartinib for the treatment of AML in Europe, Japan and the U.S. Regulatory applications are currently under review in Europe and Japan for quizartinib in the treatment of adult patients with newly diagnosed AML that is FLT3-ITD positive, in combination with standard cytarabine and anthracycline induction and cytarabine consolidation chemotherapy, and as continuation monotherapy following consolidation, based on the results of the QuANTUM-First trial. Quizartinib is currently approved for use in Japan for the treatment of adult patients with relapsed/refractory FLT3-ITD AML, as detected by an approved test. Quizartinib is an investigational medicine in all countries outside of Japan. 4 About Daiichi Sankyo Daiichi Sankyo is dedicated to creating new modalities and innovative medicines by leveraging our worldclass science and technology for our purpose “to contribute to the enrichment of quality of life around the world.” In addition to our current portfolio of medicines for cancer and cardiovascular disease, Daiichi Sankyo is primarily focused on developing novel therapies for people with cancer as well as other diseases with high unmet medical needs. With more than 100 years of scientific expertise and a presence in more than 20 countries, Daiichi Sankyo and its 16,000 employees around the world draw upon a rich legacy of innovation to realize our 2030 Vision to become an “Innovative Global Healthcare Company Contributing to the Sustainable Development of Society.” For more information, please visit: www.daiichisankyo.com.
Daiichi Sankyo's quizartinib gets FDA priority review to treat blood cancer subtype
Oct. 24, 2022 8:57 AM ET
Daiichi Sankyo Company, Limited (DSNKY), DSKYF
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted priority review to Daiichi Sankyo's (OTCPK:DSKYF) (OTCPK:DSNKY) quizartinib to treat certain patients with a type of blood cancer.
- https://seekingalpha.com/news/3894071-daiichi-sankyos-quizartinib-gets-fda-priority-review-to-treat-blood-cancer-subtype
- https://seekingalpha.com/symbol/DSKYF
- https://seekingalpha.com/symbol/DSNKY
- https://www.daiichisankyo.com/rd/pipeline/
- https://www.daiichisankyo.com/
VPO-227
Quizartinib
BBP-398 in Combination with LUMAKRAS® (sotorasib)
Vanda Pharmaceuticals Announces Orphan Drug Designation Granted for VPO-227, a Novel Candidate for the Treatment of Cholera
October 21, 2022 WASHINGTON, Oct. 21, 2022 /PRNewswire/ -- Vanda Pharmaceuticals Inc. (Vanda) (Nasdaq: VNDA) today announced the U.S. Food and Drug Administration (FDA) has granted Orphan Drug Designation for VPO-227 for the treatment of cholera. While the incidence of cholera in the U.S. is low, cholera is a widespread infectious diarrheal disease with estimated 1.4 to 4 million cases worldwide, resulting in 21,000 to 143,000 deaths annually.1 Many of these deaths occur in children, as diarrheal diseases are the second leading cause of death globally among children under 5 years of age.2 Cholera remains a major public health challenge and recognized unmet medical need despite decades-long public health efforts. "This designation is an important milestone in the development of VPO-227 and highlights the need for potential new treatment options for patients who suffer from cholera and other conditions of water hyper-excretion," said Mihael H. Polymeropoulos, M.D., Vanda's President, CEO and Chairman of the Board. VPO-227 is a small-molecule with a novel mechanism of action which blocks the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) ion channel. CFTR plays a pivotal role in cholera-induced intestinal fluid loss as it is affected by the cholera toxin. VPO-227, therefore, has the potential to be an orally administered treatment for cholera. In a recent publication in the journal Toxins, the authors showed that oral VPO-227 protects animals from a lethal cholera challenge using two separate cholera strains.3 Orphan Drug Designation is granted by the FDA to investigational therapies addressing rare medical conditions and provides benefits to drug developers, including assistance in the drug development process, tax credits for clinical costs, exemptions from certain FDA fees and the potential for seven years of post-approval marketing exclusivity. Additionally, in order to incentivize development in tropical diseases, including cholera, the FDA has established the Tropical Disease Priority Review Voucher Program, which grants a transferable Priority Review Voucher to sponsors of eligible new drug applications for products treating tropical diseases. Vanda expects to submit an Investigational New Drug (IND) application to the FDA for VPO-227 in 2023.
About Vanda Pharmaceuticals Inc. Vanda is a leading global biopharmaceutical company focused on the development and commercialization of innovative therapies to address high unmet medical needs and improve the lives of patients. For more on Vanda Pharmaceuticals Inc., please visit www.vandapharma.com and follow us on Twitter @vandapharma. About VPO-227 VPO-227 (formerly BPO-27) is a small molecule CFTR inhibitor in development for the treatment of secretory disorders, including cholera. Vanda entered into a license agreement with University of California, San Francisco (UCSF) in 2017, under which Vanda acquired an exclusive worldwide license from UCSF to develop and commercialize a portfolio of CFTR activators and inhibitors, including the activator VPO-227. CFTR activators and inhibitors may have broad applicability in addressing a number of disorders, including chronic dry eye, constipation, polycystic kidney disease, cholestasis, and secretory diarrheas.
View original content:https://www.prnewswire.com/news-releases/vanda-pharmaceuticals-announces-orphan-drug-designation-granted-for-vpo227-a-novel-candidate-for-the-treatment-of-cholera-301656345.html SOURCE Vanda Pharmaceuticals Inc.
Vanda granted FDA’s Orphan Drug Designation for cholera therapy
Oct. 21, 2022 2:34 PM ET
Vanda Pharmaceuticals Inc. (VNDA)
By: Dulan Lokuwithana, SA News Editor
- Commercial-stage biotech Vanda Pharmaceuticals (NASDAQ:VNDA) announced Friday that the FDA issued Orphan Drug Designation for VPO-227, an experimental therapy for cholera.
- https://seekingalpha.com/news/3893804-vnda-stock-gain-as-fda-grants-orphan-drug-designation-for-cholera-therapy
- https://seekingalpha.com/symbol/VNDA
- https://www.vandapharma.com/
- https://www.vandapharma.com/pipeline/
BBP-398 in Combination with LUMAKRAS® (sotorasib)
BBP-398 in Combination with LUMAKRAS® (sotorasib)
BBP-398 in Combination with LUMAKRAS® (sotorasib)
BridgeBio Pharma Announces First Lung Cancer Patient Dosed in Phase 1/2 Trial and US FDA Fast Track Designation for SHP2 inhibitor BBP-398 in Combination with Amgen’s LUMAKRAS® (sotorasib)
– BBP-398, an investigational SHP2 inhibitor, is a potentially optimal agent for use in combination therapies given its continuous, once-daily dosing in addition to synergistic activity with other agents to treat cancers driven by KRAS G12C mutations
– The combination of investigational therapy BBP-398 and LUMAKRAS, if successful, has the potential to address the serious unmet need for patients with KRAS G12C-mutated non-small cell lung cancer (NSCLC).
– This combination trial is designed to target NSCLC driven by a KRAS G12C mutation, one of the most common oncogenic mutations in the United States (US) and European Union (EU); 13% of NSCLC tumors have a KRAS G12C mutation with approximately 30,000 people diagnosed in the US each year
– Preclinical findings demonstrated synergistic efficacy for the combination of the two therapies in a KRAS G12C-mutated NSCLC cell line-derived xenograft model
PALO ALTO, Calif., Oct. 11, 2022 (GLOBE NEWSWIRE) — BridgeBio Pharma, Inc., (Nasdaq: BBIO) (BridgeBio), a commercial-stage biopharmaceutical company focused on genetic diseases and cancers, today announced that the first patient with non-small cell lung cancer (NSCLC) has been dosed in its Phase 1/2 clinical trial of BBP-398, an investigational SHP2 inhibitor, with Amgen Inc.’s (Amgen) LUMAKRAS® (sotorasib), the first and only currently approved targeted treatment for patients with KRAS G12C-mutated locally advanced or metastatic NSCLC, in advanced solid tumors with the KRAS G12C mutation.
Approximately 30,000 people are diagnosed with KRAS G12C-mutated NSCLC in the US each year and the KRAS G12C mutation is one of the most frequent oncogenic mutations in the US and Europe. By combining SHP2 inhibition with KRAS G12C inhibition in patients with the KRAS G12C mutation, there is potential to prevent oncogenesis and overactive cellular proliferation.
“The survival rate following a diagnosis of NSCLC with a KRAS mutation is extremely poor. We are hopeful that by launching this clinical trial with Amgen, we may be able to fill the current gap in unmet medical need for these cancer patients,” said Frank McCormick, Ph.D., chairman of oncology at BridgeBio. “We are grateful the FDA has granted our program Fast Track designation and are hopeful it will allow us to address the needs of these patients more quickly following diagnosis.”
The Phase 1/2 study will include a dose escalation period followed by dose expansion and optimization, and is designed to evaluate the safety, tolerability, pharmacokinetics, pharmacodynamics and preliminary efficacy of BBP-398 in combination with LUMAKRAS. The dose escalation period will enroll patients with all solid tumors with a KRAS G12C mutation and participants will be eligible regardless of previous exposure to a KRAS G12C inhibitor. The dose expansion period will enroll patients with NSCLC with a KRAS G12C mutation who have not previously been exposed to a KRAS G12C inhibitor. Initial data is expected by the end of 2024.
Additionally, the US Food and Drug Administration (FDA) granted Fast Track designation for the investigation of BBP-398 in combination with LUMAKRAS for adult patients with previously treated, KRAS G12C-mutated, metastatic NSCLC. The FDA’s Fast Track designation is designed to drive the development and expedite the review process for medicines under investigation for serious conditions with unmet medical needs.
“To date, preclinical data for SHP2 inhibition has shown promise in unlocking possible combination strategies to treat patients suffering from a range of cancers, including NSCLC. By combining SHP2 inhibition with KRAS G12C inhibition, there is potential for this therapeutic arsenal to be impactful for patients since it could prevent overactive cellular proliferation and oncogenesis. I am extremely pleased to see that work from our group and others has now reached the clinic, where we will be able to study the benefit it could have for cancer patients with KRAS G12C mutations,” said Benjamin G. Neel, M.D., Ph.D., Co-founder of Navire Pharma Inc. (Navire), a BridgeBio company, and Director of the L/I Perlmutter Cancer Center at NYU Langone and Professor of Medicine at NYU Grossman SoM.1
“People with metastatic NSCLC with a KRAS mutation often do not respond well to standard chemotherapy and immunotherapy options. They might have a worse prognosis than patients without a KRAS mutation and it is essential to deliver better therapeutic options to people with this difficult-to-treat cancer. I am hopeful that by partnering with BridgeBio on this study we may be able to provide substantial relief for patients with a serious unmet need,” said Rohit Joshi, M.D., Director for Cancer Research SA (CRSA) and Associate Professor at the University of Adelaide.
In May 2022, BridgeBio entered into an exclusive license agreement with Bristol Myers Squibb to develop and commercialize BBP-398 in oncology worldwide, except for in mainland China and other Asian markets. These territories are part of BridgeBio’s separate strategic collaboration with LianBio announced in 2020. The 2022 agreement with Bristol Myers Squibb expands upon the earlier agreement between the companies signed in 2021 to investigate the combination of BBP-398 with OPDIVO® (nivolumab) in patients with advanced solid tumors with KRAS mutations.
BridgeBio has a non-exclusive clinical collaboration with Amgen to evaluate the combination of BBP-398 with LUMAKRAS in patients with advanced solid tumors with the KRAS G12C mutation.
BBP-398, as a monotherapy or in combination with other targeted therapies, could potentially be a promising therapy for patients with the KRAS G12C mutation. Initial Phase 1 data from the ongoing BBP-398 trial is expected in 2023.
OPDIVO® (nivolumab) is a trademark of Bristol-Myers Squibb Company.
About BBP-398
BBP-398 is a SHP2 inhibitor that is being developed for difficult-to-treat cancers and was founded through a collaboration with The University of Texas MD Anderson Cancer Center’s Therapeutics Discovery division. SHP2 is a protein-tyrosine phosphatase that links growth factor, cytokine and integrin signaling with the downstream RAS/ERK MAPK pathway to regulate cellular proliferation and survival. In May 2022, BridgeBio entered an exclusive license with Bristol Myers Squibb to develop and commercialize BBP-398, a potentially best-in-class SHP2 inhibitor. Additionally, BridgeBio has a strategic collaboration with LianBio for clinical development and commercialization of BBP-398 in combination with various agents in solid tumors such as non-small cell lung cancer, colorectal and pancreatic cancer, in mainland China and other Asian markets and clinical collaborations; with Bristol Myers Squibb for combination with OPDIVO® (nivolumab) in patients with advanced solid tumors with KRAS mutations; and with Amgen for combination with LUMAKRAS® (sotorasib), Amgen’s KRAS G12C inhibitor, in patients with advanced solid tumors with KRAS G12C mutations.
About BridgeBio Pharma, Inc.
BridgeBio Pharma (BridgeBio) is a commercial-stage biopharmaceutical company founded to discover, create, test and deliver transformative medicines to treat patients who suffer from genetic diseases and cancers with clear genetic drivers. BridgeBio’s pipeline of development programs ranges from early science to advanced clinical trials. BridgeBio was founded in 2015 and its team of experienced drug discoverers, developers and innovators are committed to applying advances in genetic medicine to help patients as quickly as possible. For more information visit bridgebio.com and follow us on LinkedIn and Twitter.
BridgeBio stock rises as BBP-398, Lumakras combo for lung cancer gets FDA fast track status
Oct. 11, 2022 1:49 PM ET
BridgeBio Pharma, Inc. (BBIO), AMGNBMY, LIAN
By: Ravikash, SA News Editor1 Comment
- BridgeBio Pharma (NASDAQ:BBIO) stock rose ~4% on Oct. 11 after the company said the U.S. Food and Drug Administration (FDA) granted fast track designation to BBP-398 in combination with Amgen's (NASDAQ:AMGN) Lumakras for adult patients with previously treated, KRAS G12C-mutated, metastatic non-small cell lung cancer (NSCLC).
- https://seekingalpha.com/news/3890439-bridgebio-stock-rises-as-bbp-398-lumakras-combo-gets-fda-fast-track-status
- https://seekingalpha.com/symbol/BBIO
- https://seekingalpha.com/symbol/AMGN
- https://seekingalpha.com/symbol/BMY
- https://seekingalpha.com/symbol/LIAN
- https://bridgebio.com/navire-rtk-cancer/
- https://bridgebio.com/pipeline/
TREMFYA® (guselkumab) & SIMPONI® (golimumab)
BBP-398 in Combination with LUMAKRAS® (sotorasib)
TREMFYA® (guselkumab) & SIMPONI® (golimumab)
Results of Novel Clinical Study of Guselkumab and Golimumab Combination Therapy Show Adults with Moderately to Severely Active Ulcerative Colitis Maintained Higher Rates of Clinical, Histologic, and Endoscopic Remission at Week 38
Oct 10, 2022United States
The rate of clinical remission was 47.9 percent in patients who received combination induction therapy with guselkumab and golimumab compared with either treatment alone (31.0 percent and 20.8 percent, respectively) at 38 weeks1
SPRING HOUSE, PENNSYLVANIA, October 10, 2022 – The Janssen Pharmaceutical Companies of Johnson & Johnson today announced data from an ongoing analysis of a Phase 2a clinical trial showing adults with moderately to severely active ulcerative colitis (UC) who received 12 weeks of combination induction therapy with guselkumab and golimumab, followed by a transition to guselkumab alone for maintenance, achieved a clinical remission ratea (based on the modified Mayo score [mMayo])b at week 38 of 47.9 percent, a higher rate than induction and maintenance treatment with either guselkumab alone (31.0 percent) or golimumab alone (20.8 percent).1,2 Patients had comparable rates of adverse events (AEs) across the treatment groups.1 Guselkumab alone, or the combination of guselkumab and golimumab are under clinical investigation and not approved for the treatment of adults with UC in the U.S.
The VEGA study is the first randomized controlled trial to evaluate the efficacy and safety of combination therapy with an interleukin (IL)-23p19 subunit antagonist (guselkumab) and a tumor necrosis factor-alpha (TNFα) antagonist (golimumab) in UC.3,4 Detailed results were presented today as an oral presentation (OP087) at the United European Gastroenterology (UEG) Week 2022 congress taking place in-person in Vienna, Austria and virtually from October 8-11.1
“Exploring combinations of advanced therapies is an important step in continuing to innovate for the many patients living with ulcerative colitis,” said Bruce E. Sands, M.D., M.S., Chief of the Dr. Henry D. Janowitz Division of Gastroenterology at Mount Sinai, Professor of Medicine at the Icahn School of Medicine at Mount Sinai, and VEGA Steering Committee member.c “These new data from the VEGA trial build upon and affirm our initial 12-week findings showing the potential clinical benefit of combining guselkumab and golimumab in treating adults with moderately to severely active ulcerative colitis.”
In the VEGA study, patients with moderately to severely active UC were randomized (1:1:1) to receive combination therapy with guselkumab and golimumab, guselkumab monotherapy, or golimumab monotherapy.1 After endpoints were evaluated at week 12, patients in the monotherapy groups continued their initially assigned treatment, while patients randomized to the combination therapy group transitioned to guselkumab alone as a maintenance therapy.1 Patients remained blinded and received their respective therapies through the final efficacy assessment at week 38. Clinical remissiona,d was assessed based on the modified Mayo score (mMayo),b as well as the total Mayo score.e Symptomatic remission,f endoscopic improvement,g endoscopic remission,h histologic remission,i and composite histologic-endoscopic endpointsg,i were also assessed at week 38 in an exploratory analysis.1 Safety was evaluated through week 50 (16 weeks after the final dose of study intervention at week 34).1
Patients who received combination therapy with guselkumab and golimumab followed by maintenance treatment with guselkumab achieved clinical remissiona (mMayob) at week 38 (47.9 percent [34/71]) versus 31.0 percent (22/71) and 20.8 percent (15/72) of patients who received guselkumab or golimumab alone, respectively (nominal p=<0.05).1
Rates of clinical remissiond as defined by the total Mayo scoree at week 38 were similar to those based on the mMayo,a,b with 43.7 percent (31/71) in the combination therapy followed by guselkumab group achieving this endpoint, compared to either the guselkumab or golimumab monotherapy groups, (31.0 percent [22/71] and 22.2 percent [16/72], respectively).1
Also, patients receiving combination therapy followed by guselkumab had the following outcomes at week 38:1
- Endoscopic improvementg and the composite histologic-endoscopic endpointg,i were higher in patients who received combination therapy followed by treatment with guselkumab compared to patients who received guselkumab or golimumab alone.
- Endoscopic remissionh and histologic remissioni were higher in patients who received combination therapy followed by treatment with guselkumab compared to patients who received golimumab alone.
Patients receiving combination therapy followed by maintenance treatment with guselkumab and patients receiving treatment only with guselkumab monotherapy achieved the same rate of symptomatic remissionf of 69 percent at week 38, which was greater than the golimumab monotherapy group of 59.7 percent.1
Rates of AEs were comparable through week 50 of the study.1 Respectively, the combination therapy followed by guselkumab, guselkumab alone, and golimumab alone groups had AE rates of 63.4, 64.8, and 76.4 percent and infection rates of 31.0, 23.9, and 31.9 percent.1 All groups had the same serious AE rates of 5.6 percent and the same serious infection rates of 2.8 percent.1 Overall, 13.1 percent of patients discontinued their treatment prior to the final dose of study intervention.1
“The 38-week VEGA data suggest the potential that guselkumab and golimumab combination therapy has in patients with moderately to severely active ulcerative colitis for whom previous conventional treatments have inadequately managed their disease or improved their well-being,” said Jan Wehkamp, M.D., Ph.D., Vice President, Gastroenterology Disease Area Leader, Janssen Research & Development, LLC. “We thank the patients who participated in the VEGA study, as their contribution helps us get closer to our goal of developing therapies that will bring meaningful improvements to patients with ulcerative colitis.”
Janssen previously announced the 12-week data of patient outcomes from the VEGA study at the 17th Congress of the European Crohn's and Colitis Organisation on February 19, 2022.2
About VEGA (NCT03662542; EudraCT 2018-001510-15)
VEGA was a randomized, double-blind, active-controlled, parallel group, global multicenter Phase 2a proof-of-concept study evaluating the efficacy and safety of combination induction therapy with guselkumab and golimumab, followed by a transition to guselkumab monotherapy for maintenance, in patients with moderately to severely active UC as defined by a Mayo score of 6 to 12 inclusive and an endoscopy subscore of 2 or greater as determined by central read.3,4
Study participants were naïve to TNFα, IL-12/23, and IL-23p19 antagonists and had to be refractory or intolerant to conventional therapy (e.g. immunosuppressants and/or corticosteroids).1 Participants were randomly assigned 1:1:1 to receive guselkumab monotherapy dosed at 200 milligrams (mg) intravenously (IV) at weeks 0, 4, and 8 followed by 100 mg every 8 weeks (q8w) subcutaneous (SC) (n=71); golimumab SC monotherapy dosed at 200 mg at week 0 followed by 100 mg SC at weeks 2, 6, and 10 followed by 100 mg every 4 weeks SC monotherapy (n=72); or a combination of 200 mg IV guselkumab plus 200 mg SC golimumab at week 0, 100 mg SC golimumab at weeks 2, 6, and 10, and 200 mg IV guselkumab at weeks 4 and 8 (n=71) followed by 100 mg guselkumab SC q8w thereafter.1 After week 12, participants in the monotherapy groups continued their initially assigned treatment, while patients randomized to the combination group transitioned to guselkumab 100 mg SC q8w as a maintenance therapy.1 The participants received their respective therapies through week 34 with final efficacy assessments at week 38.1
The primary endpoint was clinical response at week 12, defined as a decrease from baseline in the Mayo score by 30 percent or more and 3 or more points, with either a decrease in rectal bleeding subscore of 1 or more or rectal bleeding subscore of 0 or 1. The trial’s major secondary endpoint was clinical remission at week 12, defined as Mayo score less than or equal to 2, with no individual subscore more than 1. No adjustments were made for multiple comparisons.2,3 Other key endpoints evaluated at week 12 were clinical remission (based on components of the mMayo score), symptomatic remission, endoscopic improvement, endoscopic remission, histologic remission, composite histologic-endoscopic endpoints, and biomarker outcomes.1
About guselkumab
Developed by Janssen, guselkumab (which is marketed under the brand name TREMFYA®) is the first approved fully human monoclonal antibody that selectively binds to the p19 subunit of IL-23 and inhibits its interaction with the IL-23 receptor.9 TREMFYA is approved in the U.S., Canada, Japan, and a number of other countries worldwide for the treatment of adults with moderate to severe plaque psoriasis (PsO) who may benefit from taking injections or pills (systemic therapy) or phototherapy (treatment using ultraviolet light), and for the treatment of adult patients with active psoriatic arthritis (PsA).9 It is also approved in the EU for the treatment of moderate to severe plaque PsO in adults who are candidates for systemic therapy and for the treatment of active PsA in adult patients who have had an inadequate response or who have been intolerant to a prior disease-modifying antirheumatic drug therapy.9
The Janssen Pharmaceutical Companies of Johnson & Johnson maintain exclusive worldwide marketing rights to TREMFYA®.
Please read the full Prescribing Information, including Medication Guide for TREMFYA®, and discuss any questions that you have with your doctor.
About golimumab10
- Golimumab (marketed as SIMPONI®) is a prescription medicine for adults with:
- Moderate to severe rheumatoid arthritis (RA), with the medicine methotrexate (MTX)
- Active PsA, alone or with the medicine MTX
- Active ankylosing spondylitis
- Moderately to severely active UC when certain other UC medicines have not worked well enough or cannot be tolerated, or if it is necessary to continue taking steroid medicines
- Please read the full Prescribing Information and Medication Guide for SIMPONI® and discuss any questions you have with your doctor.
- https://www.simponiariahcp.com/
Learn more at www.janssen.com.
Follow us at www.twitter.com/JanssenGlobal.
Janssen Research & Development, LLC is part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
J&J says Tremfya, Simponi combination effective for ulcerative colitis
Oct. 10, 2022 1:35 PM ET
By: Jonathan Block, SA News Editor
- New research indicates that a combination of Johnson & Johnson's (NYSE:JNJ) Tremfya (guselkumab) + Simponi (golimumab) led to a better clinical remission rate than with either treatment alone for ulcerative colitis (UC).
- https://seekingalpha.com/news/3890091-johnson-johnson-says-tremfya-simponi-combination-effective-for-ulcerative-colitis
- https://seekingalpha.com/symbol/JNJ
- https://www.simponiariahcp.com/
- https://www.tremfya.com/
- https://www.janssen.com/
Sotatercept
BBP-398 in Combination with LUMAKRAS® (sotorasib)
TREMFYA® (guselkumab) & SIMPONI® (golimumab)
Merck Announces Positive Top-line Results from Pivotal Phase 3 STELLAR Trial Evaluating Sotatercept for the Treatment of Adults with Pulmonary Arterial Hypertension (PAH)
October 10, 2022 6:45 am ET
Sotatercept demonstrated significant improvement in exercise capacity and key secondary outcome measures compared to placebo when added to background therapy
RAHWAY, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced positive top-line results from the pivotal Phase 3 STELLAR trial evaluating the safety and efficacy of sotatercept, an investigational activin receptor type IIA-Fc (ActRIIA-Fc) fusion protein being evaluated as an add-on to stable background therapy for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1). The trial met its primary efficacy outcome measure, demonstrating a statistically significant and clinically meaningful improvement in 6-minute walk distance (6MWD, which measures how far patients can walk in 6 minutes) from baseline at 24 weeks. Eight of nine secondary efficacy outcome measures achieved statistical significance, including the outcome measure of proportion of participants achieving multicomponent improvement (defined as improvement in 6MWD, improvement in N-terminal pro-B-type natriuretic peptide (NT-proBNP) level, and either improvement in WHO FC or maintenance of WHO FC II), and the outcome measure of time to death or the first occurrence of a clinical worsening event (TTCW). The Cognitive/Emotional Impacts domain score of PAH-SYMPACT®, which was assessed as the ninth and final secondary outcome measure, did not achieve statistical significance. The overall safety profile of sotatercept in STELLAR was in general consistent with what has been observed in Phase 2. Results from the study will be presented at an upcoming scientific congress.
“In the Phase 3 STELLAR study, sotatercept added to currently approved background therapy showed a profound effect on the primary efficacy outcome measure of improvement from baseline to 24 weeks in six-minute walk distance. The results from the secondary efficacy outcomes, including a favorable benefit seen in patients’ time to a clinical-worsening event, are especially noteworthy,” said Dr. Dean Y. Li, president, Merck Research Laboratories. “We believe that in totality, the results observed in the STELLAR study suggest that sotatercept has the potential to transform the treatment of patients with PAH. We are moving with urgency on our regulatory applications to bring this investigational therapy to these patients.”
About STELLAR
STELLAR (NCT04576988) is a pivotal Phase 3, randomized, double-blind, placebo-controlled, multicenter, parallel-group study designed to evaluate the safety and efficacy of sotatercept compared to placebo, as an add-on to background therapy for the treatment of adults with pulmonary arterial hypertension (WHO Group 1). The primary endpoint is exercise capacity, as measured by 6-minute walk distance (6MWD) 24 weeks following initiation of treatment. Nine secondary outcome measures were assessed: proportion of participants achieving multicomponent improvement (consisting of improvement in 6MWD, improvement in N-terminal pro-B-type natriuretic peptide (NT-proBNP) level, and either improvement in WHO FC or maintenance of WHO FC II); change from baseline in pulmonary vascular resistance (PVR); change from baseline in NT-proBNP levels; proportion of participants who improved in WHO FC; time to death or the first occurrence of a clinical worsening event (TTCW); proportion of participants who maintained or achieved a low risk score using the simplified French Risk score calculator; change from baseline in the Physical Impacts domain score of PAH; change from baseline in the Cardiopulmonary Symptoms domain score of PAH-SYMPACT®; and change from baseline in the Cognitive/Emotional Impacts domain score of PAH-SYMPACT®.
About sotatercept
Sotatercept is an investigational, potential first-in-class activin receptor type IIA-Fc (ActRIIA-Fc) fusion protein in development for the treatment of adult patients with pulmonary arterial hypertension (WHO Group 1). Sotatercept was designed to rebalance pro-proliferative (ActRIIA/Smad2/3-mediated) and anti- proliferative (BMPRII/Smad1/5/8-mediated) signaling associated with pulmonary arterial wall and right ventricular remodeling.
Sotatercept has been granted Breakthrough Therapy designation by the U.S. Food and Drug Administration (FDA), as well as Priority Medicines designation by the European Medicines Agency for the treatment of PAH.
Merck acquired exclusive rights to sotatercept in the pulmonary hypertension field through the acquisition of Acceleron Pharma Inc. Sotatercept is the subject of a licensing agreement with Bristol Myers Squibb.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit www.merck.com and connect with us on Twitter, Facebook, Instagram, YouTube and LinkedIn.
Source: Merck & Co., Inc.
Merck's Acceleron buy shows results as sotatercept meets main goal in trial to treat high pressure in lungs
Oct. 10, 2022 7:35 AM ET
By: Ravikash, SA News Editor
Merck (NYSE:MRK) said sotatercept met the main goal of showing statistically significant improvement in 6-minute walk distance (6MWD) in a phase 3 trial in patients with pulmonary arterial hypertension (PAH).
https://seekingalpha.com/symbol/MRK
RGX-314
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) (AMX0035)
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) (AMX0035)
REGENXBIO ANNOUNCES ADDITIONAL POSITIVE INTERIM DATA FROM TRIALS OF RGX-314 FOR THE TREATMENT OF WET AMD
October 3, 2022 at 7:05 AM EDT
- Company announced positive interim data from and the expansion of Phase II AAVIATE® trial of RGX-314 for the treatment of wet AMD using suprachoroidal delivery
- RGX-314 continues to be well tolerated in 85 patients from Cohorts 1-5 with no drug-related serious adverse events
- Meaningful reduction in treatment burden at six months across all dose levels, 85% reduction in treatment burden observed at third dose level
- 67% of patients in Cohort 4 were injection-free
- No meaningful differences in outcomes at six months for patients who are NAb positive
- Phase II trial expanded to include new cohort at third dose level with short-course prophylactic ocular steroids following RGX-314 administration
- Positive interim data presented at the AAO Annual Meeting from the Phase I/IIa Long-term Follow-up study of RGX-314 for the treatment of wet AMD using subretinal delivery
- RGX-314 continues to be well-tolerated and demonstrates long-term, durable treatment effect up to four years
- Two pivotal trials, ATMOSPHERE® and ASCENT™, are active and enrolling patients
- Pivotal trials are expected to support BLA submission in 2024
- New interim data from Phase II ALTITUDE® trial of RGX-314 for the treatment of diabetic retinopathy using suprachoroidal delivery expected at the Retina Society 55th Annual Scientific Meeting in November
- Conference call Monday, October 3 at 8:30 a.m. ET
ROCKVILLE, Md, Oct. 3, 2022 (PRNewswire) – REGENXBIO Inc. (Nasdaq: RGNX) today announced a program update from its ongoing clinical investigation of RGX-314 for the treatment of wet AMD, a leading cause of vision loss globally.
REGENXBIO announced positive interim data from the Phase II AAVIATE® trial of RGX-314 for the treatment of wet AMD using suprachoroidal delivery. REGENXBIO also presented positive interim data from the Phase I/IIa long-term follow-up (LTFU) study of RGX-314 for the treatment of wet AMD using subretinal delivery at the American Academy of Ophthalmology (AAO) annual meeting this past weekend in Chicago.
"Today's announcements come nearly a year into our collaboration with AbbVie to advance RGX-314 in wet AMD and other retinal diseases. These new subretinal and suprachoroidal data highlight the potential impact of RGX-314 for the millions of patients facing vision loss from wet AMD," said Kenneth T. Mills, President and Chief Executive Officer of REGENXBIO. "I am pleased with the continued progress on and momentum for these programs. We remain on track to submit a BLA for RGX-314 in 2024, and we expect to provide an update on the ALTITUDE trial of RGX-314 for the treatment of diabetic retinopathy using suprachoroidal delivery at the upcoming Retina Society Meeting in November."
Data Summary and Safety Update for the Phase II AAVIATE Trial of RGX-314 using Suprachoroidal Delivery
The Phase II AAVIATE trial of RGX-314 for the treatment of wet AMD using in-office suprachoroidal delivery continues to show positive interim results. AAVIATE is a multi-center, open-label, randomized, active-controlled, dose-escalation trial that is evaluating the efficacy, safety and tolerability of suprachoroidal delivery of RGX-314. The primary endpoint of the trial is mean change in vision in patients dosed with RGX-314, as measured by best corrected visual acuity (BCVA) at Week 40 from baseline, compared to patients receiving monthly injections of ranibizumab. Other endpoints include mean change in central retinal thickness (CRT) and number of anti-vascular endothelial growth factor (anti-VEGF) intravitreal injections received following administration of RGX-314.
As of August 1, 2022, RGX-314 suprachoroidal delivery was reported to be well tolerated across 85 patients dosed in Cohorts 1-5. Fifteen SAEs were reported, none of which were considered related to RGX-314. For the total group of Cohorts 1-4 (n=65), all common treatment emergent adverse events (TEAEs) through 6 months in the study eye were mild or moderate and included conjunctival hemorrhage, increased intraocular pressure, episcleritis, and conjunctival hyperemia. Mild intraocular inflammation was reported at similar incidence in the first and second dose levels, with an increase in incidence in mild to moderate inflammation seen at the third dose level (Cohort 4). All intraocular inflammation resolved with topical corticosteroids.
Patients treated in the RGX-314 arms and the ranibizumab control arm both continue to demonstrate stable BCVA and CRT at 6 months. In addition, a meaningful reduction in anti-VEGF treatment burden following administration of RGX-314 compared to mean annualized injection rate during the 12 months prior to administration was observed and ranged from -63.8% to -84.7% across all cohorts. The highest reduction in treatment burden was observed in the third dose level, with patients receiving a mean of 1.3 injections over six months following administration of RGX-314, which represents an 84.7% reduction in anti-VEGF treatment burden. Ten out of 15 patients (67%) in the third dose level received no anti-VEGF injections over six months following RGX-314 administration. In these patients, visual acuity and CRT was observed to be stable over six months.
Additionally, the interim data from the second dose level (Cohorts 2 and 3) suggests there is no meaningful difference in safety and vision outcomes for patients who are neutralizing antibody (NAb) positive.
Phase II AAVIATE Trial Expansion to Cohort 6
REGENXBIO announced today that the AAVIATE study has expanded, and an additional cohort (Cohort 6) will be enrolled to evaluate RGX-314 at the third dose level of 1x1012 GC/eye with a short course of prophylactic ocular steroids to evaluate the ability to prevent or reduce the occurrence of the mild to moderate intraocular inflammation seen to date. Patients will be enrolled in Cohort 6 regardless of NAb status.
"We are pleased to share updated data from the AAVIATE trial, including new 6-month data from Cohorts 1-4 which provides continued evidence of the emerging clinical profile of RGX-314 for the treatment of wet AMD using suprachoroidal delivery," said Steve Pakola, M.D., Chief Medical Officer of REGENXBIO. "RGX-314 continues to be well tolerated, with emerging evidence of treatment effect, including meaningful reduction in anti-VEGF treatment burden at all dose levels. We look forward to expanding this trial to further explore the third dose level."
Data Summary from Phase I/IIa Long-term Follow-up Study of RGX-314 using Subretinal Delivery
The Phase I/IIa study evaluated RGX-314 in 42 patients with wet AMD using subretinal delivery and was designed as an open label, dose escalation study evaluating five doses of RGX-314 over two years. Dose dependent increases in treatment effect were observed, and doses similar to those used in Cohort 3 and Cohort 4 of the Phase I/IIa trial were advanced into the ongoing pivotal trials, ATMOSPHERE and ASCENT. After the Phase I/IIa study's completion, patients were encouraged to enroll into a long-term follow-up study for up to five years after RGX-314 administration. Data presented at AAO highlights the results of the 16 (out of 18) patients from Cohorts 3 and 4 who enrolled in the LTFU study, with data now out to 4 years and 3 years, respectively. Data from this study demonstrating that RGX-314 continues to be well-tolerated with long-term, durable treatment effect up to four years is expected to support the anticipated BLA filing for RGX-314 in 2024.
As of August 29, 2022, RGX-314 continues to be generally well-tolerated in the long-term follow-up study (n=37). A total of nine serious adverse events (SAEs) were reported in four patients, none of which were considered related to RGX-314. No new drug-related ocular AEs were reported in the long-term follow-up study for Cohorts 3 and 4. One patient in Cohort 5 experienced a significant decrease of vision during the long-term follow-up study who had macular pigmentary changes after a superior bleb in the Phase I/IIa trial.
Patients treated with RGX-314 continue to demonstrate a long-term, durable treatment effect in Cohort 3 up to 4 years and Cohort 4 up to three years. Stable to improved visual acuity was observed, with a mean BCVA of +12 letters from baseline at four years for Cohort 3 patients and -5 letters from baseline at three years for Cohort 4 patients following RGX-314 administration.
Patients also demonstrated meaningful long-term reductions in anti-VEGF treatment burden following administration of RGX-314. Patients in Cohort 3 received a mean annualized rate of 2.4 injections through 4 years following administration of RGX-314 (versus 6.8 injections in the 12 months prior to treatment), representing a 67.0% reduction in mean annualized injection rate. Patients in Cohort 4 received a mean annualized rate of 4.4 injections through 3 years following administration of RGX-314 (versus 10.2 injections in the 12 months prior to treatment), representing a 58.4% reduction in mean annualized injection rate.
"These positive interim data from the long-term follow-up and AAVIATE trials continue to reinforce the potential clinical benefit of a one-time administration of RGX-314 in the overall management of patients with neovascular AMD," said Arshad M. Khanani, M.D., M.A., FASRS, Director of Clinical Research at Sierra Eye Associates, Reno, NV. "I am extremely encouraged by this long-term data up to four years showing durable treatment effect and the potential of RGX-314 to meaningfully reduce injection burden for patients while maintaining vision outcomes. I look forward to the further investigation of RGX-314 in Cohort 6 of the AAVIATE trial, as in-office suprachoroidal delivery has the potential to be an important treatment option for patients."
These study findings are available under the Presentations & Publications page in the Media section of REGENXBIO's website located at www.regenxbio.com.
About the AAVIATE® Trial
The multi-center, open-label, randomized, active-controlled, dose-escalation Phase II AAVIATE trial is evaluating the efficacy, safety and tolerability of suprachoroidal delivery of RGX-314 in patients with wet AMD using the Clearside SCS Microinjector®. Twenty patients in Cohort 1 were randomized to receive RGX-314 at a dose level of 2.5x1011 genomic copies per eye (GC/eye) through one injection versus monthly 0.5 mg ranibizumab intravitreal injection at a 3:1 ratio. Twenty patients in Cohort 2 were randomized to receive RGX-314 at a dose level of 5x1011 GC/eye through two injections versus monthly 0.5 mg ranibizumab intravitreal injection at a 3:1 ratio. Cohort 3 is evaluating RGX-314 at the same dose level as Cohort 2 in 20 patients who are NAb positive. Cohort 4 is evaluating RGX-314 in 15 patients at a dose level of 1x1012 GC/eye and Cohort 5 is evaluating the same dose level of RGX-314 in 20 patients who are NAb positive. Cohort 6 is evaluating patients at the same dose level as Cohorts 4 and 5 and includes a short course of prophylactic steroids following administration of RGX-314.
About RGX-314
RGX-314, being developed in collaboration with AbbVie, is being investigated as a potential one-time treatment for wet AMD, diabetic retinopathy, and other chronic retinal conditions. RGX-314 consists of the NAV® AAV8 vector, which encodes an antibody fragment designed to inhibit vascular endothelial growth factor (VEGF). RGX-314 is believed to inhibit the VEGF pathway by which new, leaky blood vessels grow and contribute to the accumulation of fluid in the retina.
REGENXBIO is advancing research in two separate routes of administration of RGX-314 to the eye, through a standardized subretinal delivery procedure as well as delivery to the suprachoroidal space. REGENXBIO has licensed certain exclusive rights to the SCS Microinjector® from Clearside Biomedical, Inc. to deliver gene therapy treatments to the suprachoroidal space of the eye.
https://regenxbio.com/rgx-314/
About REGENXBIO Inc.
REGENXBIO is a leading clinical-stage biotechnology company seeking to improve lives through the curative potential of gene therapy. REGENXBIO's NAV Technology Platform, a proprietary adeno-associated virus (AAV) gene delivery platform, consists of exclusive rights to more than 100 novel AAV vectors, including AAV7, AAV8, AAV9 and AAVrh10. REGENXBIO and its third-party NAV Technology Platform Licensees are applying the NAV Technology Platform in the development of a broad pipeline of candidates, including late-stage and commercial programs, in multiple therapeutic areas. REGENXBIO is committed to a "5x'25" strategy to progress five AAV Therapeutics from our internal pipeline and licensed programs into pivotal-stage or commercial products by 2025.
Cision View original content to download multimedia:
SOURCE REGENXBIO Inc.
REGENXBIO says additional phase 2 data bolsters RGX-314 for wet macular degeneration
Oct. 03, 2022 10:55 AM ET
By: Jonathan Block, SA News Editor
- Additional interim data from the Phase II AAVIATE trial of REGENXBIO's (NASDAQ:RGNX) RGX-314 for the treatment of wet age-related macular degeneration provided additional support for the candidate.
- https://seekingalpha.com/news/3887986-regenxbio-says-additional-phase-2-data-bolsters-rgx-314-for-wet-macular-degeneration
- https://seekingalpha.com/symbol/RGNX
- https://regenxbio.com/rgx-314/
- https://regenxbio.com/
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) (AMX0035)
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) (AMX0035)
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) (AMX0035)
AMYLYX PHARMACEUTICALS ANNOUNCES FDA APPROVAL OF RELYVRIO™ FOR THE TREATMENT OF ALS
September 29, 2022 at 6:30 PM EDT
- RELYVRIO (previously known as AMX0035 in the U.S.) is an oral, fixed-dose combination therapy for the treatment of adults with ALS
- RELYVRIO significantly slowed loss of physical function in a randomized, placebo-controlled clinical trial in ALS
- Detailed data from the CENTAUR clinical trial were published in the New England Journal of Medicine, Muscle & Nerve, and the Journal of Neurology, Neurosurgery and Psychiatry
- Amylyx to host investor conference call tomorrow, September 30 at 8:00 a.m. ET
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Sep. 29, 2022--
Amylyx Pharmaceuticals, Inc. (NASDAQ: AMLX) (“Amylyx” or the “Company”) today announced that the U.S. Food and Drug Administration (FDA) has approved RELYVRIO™ (sodium phenylbutyrate and taurursodiol) for the treatment of adults with amyotrophic lateral sclerosis (ALS). RELYVRIO (previously known as AMX0035 in the U.S.) significantly slowed the loss of physical function in people living with ALS in a randomized, placebo-controlled clinical trial. RELYVRIO can be taken as a monotherapy or with existing approved treatments.
“Today’s FDA approval of RELYVRIO is an exciting milestone for the ALS community and is a major step toward achieving our mission to one day end the suffering caused by neurodegenerative diseases,” said Joshua Cohen and Justin Klee, Co-CEOs of Amylyx. “We want to give a heartfelt thank you to the broader ALS community, including healthcare professionals and those living with ALS, for their guidance, support of our clinical programs, and for sharing their experiences with us. Their stories inspired us and helped our team to better understand the ALS clock, instilling in us a deep sense of urgency that will continue to drive us forward. This is just the beginning and there is much more to be done.”
ALS is a relentlessly progressive and fatal neurodegenerative disorder caused by motor neuron death in the brain and spinal cord. Motor neuron loss in ALS leads to deteriorating muscle function, the inability to move and speak, respiratory paralysis and eventually, death. More than 90% of people with ALS have sporadic disease, showing no clear family history. ALS affects approximately 29,000 people in the U.S.
Leading U.S. ALS advocacy organizations including The ALS Association, Answer ALS Foundation, I AM ALS, Les Turner ALS Foundation and Team Gleason said in a statement, “Our organizations have been on a mission to create a world free of ALS. With today’s approval, we are encouraged that RELYVRIO can offer people living with ALS and their families the potential of more time with functional independence. This is especially important for a rapidly progressive disease with a median survival time from diagnosis of just two to three years. This is significant for people living with ALS, their loved ones, caregivers, clinicians, researchers, and advocacy, as we now have a new treatment option that could be a big step forward for the future of ALS care.”
The approval of RELYVRIO is based on data from CENTAUR, a multicenter Phase 2 clinical trial in 137 participants with ALS encompassing a 6-month randomized, placebo-controlled phase and an open-label extension (OLE) long-term follow-up phase. Detailed data from CENTAUR were published in the New England Journal of Medicine, Muscle & Nerve, and the Journal of Neurology, Neurosurgery, and Psychiatry.
The most common adverse events occurring with RELYVRIO (at least 15% and at least 5% greater than placebo) were diarrhea, abdominal pain, nausea, and upper respiratory tract infection. Gastrointestinal-related adverse reactions occurred throughout the study but were more frequent during the first three weeks of treatment.
“Any time we have a new tool to slow the progression of this disease represents an important milestone in how we battle ALS. The published data on both function and survival in a randomized trial – and what this means for people living with ALS – are a step forward for the ALS community,” said Sabrina Paganoni, M.D., Ph.D., principal investigator of the CENTAUR trial, investigator at the Sean M. Healey & AMG Center for ALS at Massachusetts General Hospital, and Associate Professor of Physical Medicine and Rehabilitation at Harvard Medical School and Spaulding Rehabilitation Hospital.
“The approval of a new treatment that helps slow the progression of ALS, preserve physical function and potentially extend survival has the potential to greatly impact the hundreds of people living with ALS who I currently treat,” said Merit Cudkowicz, M.D., co-principal investigator of the CENTAUR trial and co-founder of the Northeast ALS Consortium, Chief of Neurology and the Director of the Healey & AMG Center for ALS and Chief of Neurology at Massachusetts General Hospital, and the Julieanne Dorn Professor of Neurology at Harvard Medical School. “There are too few options to target this uniformly fatal and rapid illness, and I am encouraged at this outcome and what it represents for my patients and their families.”
“Our priority now is to ensure that adults living with ALS in the U.S. whose doctors have prescribed RELYVRIO can access it as quickly as possible,” said Margaret Olinger, Global Head of Commercial and Chief Commercial Officer of Amylyx. “Physicians will be able to prescribe immediately, and we anticipate specialty pharmacies will be able to start to fill prescriptions and ship RELYVRIO to people with ALS in the next four to six weeks.”
After considering the input of many stakeholders throughout the ALS community in the U.S., Amylyx made the decision to price RELYVRIO below the latest FDA-approved product available to people with ALS. To ensure that every eligible person who can benefit from RELYVRIO will have access, Amylyx will provide support to healthcare professionals, people living with ALS, and their loved ones through the Amylyx Care Team (ACT) Support Program. ACT provides people living with ALS who have been prescribed RELYVRIO, and their loved ones, with a dedicated, single point of contact to guide their treatment journey. ACT works tirelessly to aid with navigating through insurance in an effort to overcome potential barriers to access. ACT helps confirm coverage and provides financial assistance options to eligible individuals with out-of-pocket costs. ACT also provides education, support, and resources to help adults living with ALS get started and continue with RELYVRIO treatment, as prescribed by their healthcare provider. People with ALS, their caregivers, and healthcare professionals in the U.S. can now call 1-866-318-2989 or email amylyxcareteam@amylyx.com to speak with an ACT team member.
About the CENTAUR Trial
CENTAUR was a multicenter Phase 2 clinical trial in 137 participants with ALS encompassing a 6-month randomized placebo-controlled phase and an open-label extension (OLE) long-term follow-up phase. The trial met its primary efficacy endpoint.
Detailed safety and functional efficacy data from CENTAUR were published in the New England Journal of Medicine. Data from additional analyses from the CENTAUR trial were published in Muscle & Nerve in 2020 and 2022, and the Journal of Neurology, Neurosurgery and Psychiatry in 2022.
The CENTAUR trial was funded, in part, by the ALS ACT grant and the ALS Ice Bucket Challenge, and was supported by The ALS Association, ALS Finding a Cure (a program of The Leandro P. Rizzuto Foundation), the Northeast ALS Consortium, and the Sean M. Healey & AMG Center for ALS at Mass General.
About RELYVRIO™ (previously known as AMX0035 in the U.S.)
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) is an oral, fixed-dose medication approved to treat amyotrophic lateral sclerosis (ALS) in adults in the U.S. and approved with conditions as ALBRIOZA™ for the treatment of ALS in Canada. Additionally, the European Medicines Agency (EMA) is reviewing the Company’s Marketing Authorisation Application for AMX0035 for the treatment of ALS in Europe. AMX0035 is being explored for the potential treatment of other neurodegenerative diseases.
INDICATION AND IMPORTANT SAFETY INFORMATION FOR RELYVRIO (sodium phenylbutyrate/taurursodiol), for oral suspension
INDICATION
RELYVRIO is indicated for the treatment of amyotrophic lateral sclerosis (ALS) in adults.
Please click here to read the full Prescribing Information for RELYVRIO™.
About Amylyx Pharmaceuticals
Amylyx Pharmaceuticals, Inc. is committed to supporting and creating more moments for the neurodegenerative community through the discovery and development of innovative new treatments. Amylyx is headquartered in Cambridge, Massachusetts and has operations in Canada and EMEA. For more information, visit amylyx.com and follow us on LinkedIn and Twitter. For investors, please visit investors.amylyx.com.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220929005962/en/
Source: Amylyx Pharmaceuticals, Inc.
Amylyx wins FDA approval of ALS drug Relyvrio; shares up 12% after hours
Sep. 29, 2022 5:40 PM ET
Amylyx Pharmaceuticals, Inc. (AMLX)
By: Jonathan Block, SA News Editor2 Comments
The US FDA approved Amylyx Pharmaceuticals (NASDAQ:AMLX) Relyvrio for the treatment of amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig's disease.
https://seekingalpha.com/symbol/AMLX
https://www.amylyx.com/pipeline
CFT1946
RELYVRIO™ (sodium phenylbutyrate and taurursodiol) (AMX0035)
Lecanemab
C4 Therapeutics Receives Study May Proceed Letter from U.S. FDA to Initiate Phase 1/2 Clinical Trial of CFT1946, an Orally Bioavailable BiDAC™ Degrader, in BRAF-V600 Mutant Solid Cancers
Phase 1/2 Clinical Trial Will Study CFT1946 in BRAF-V600 Mutant Solid Cancers Including Lung, Colorectal and Melanoma; Trial Initiation Expected by Year End 2022
WATERTOWN, Mass., Sept. 29, 2022 (GLOBE NEWSWIRE) -- C4 Therapeutics, Inc. (C4T) (Nasdaq: CCCC), a clinical-stage biopharmaceutical company dedicated to advancing targeted protein degradation science to develop a new generation of small-molecule medicines and transform how disease is treated, today announced it has received a Study May Proceed Letter from the United States Food and Drug Administration (FDA) to begin a Phase 1/2 trial for CFT1946, an orally bioavailable mutant-selective BiDAC™ degrader for the treatment of BRAF-V600 mutant solid tumors.
“The Study May Proceed Letter from the FDA, which marks C4T’s third successful oncology investigational new drug application in less than two years, demonstrates the power of our TORPEDO platform to build an exciting portfolio of degrader medicines that have the potential to transform how diseases are treated,” said Andrew Hirsch, president and chief executive officer of C4 Therapeutics. “We designed CFT1946 to be a potent and selective degrader of mutant BRAF-V600, which accounts for approximately 50,000 cancer diagnoses annually. We believe our innovative therapeutic candidate may overcome some limitations of BRAF inhibitor treatments to offer cancer patients the potential for deeper and more durable responses.”
The Phase 1/2 clinical trial will primarily investigate safety, tolerability, and anti-tumor activity, with secondary and exploratory objectives to characterize the pharmacokinetic and pharmacodynamic profile of CFT1946. The initial arm of the Phase 1 portion of the study will evaluate CFT1946 as a single agent in patients with BRAF-V600 mutant solid tumors. As the Phase 1 trial progresses, an additional arm of the trial will evaluate CFT1946 in combination with trametinib in patients with BRAF-V600 mutant solid tumors. Following the identification of the recommended dose, the Phase 2 portion of the trial is expected to expand to three investigational arms to evaluate: (1) CFT1946 monotherapy in patients with V600 mutant melanoma or non-small cell lung cancer (NSCLC) after prior BRAF inhibitor treatment; (2) CFT1946 in combination with trametinib in patients with V600 mutant melanoma or NSCLC after prior BRAF inhibitor treatment; and (3) CFT1946 in combination with trametinib in patients with V600 mutant NSCLC who have not previously been treated with a BRAF inhibitor.
About C4 Therapeutics
C4 Therapeutics (C4T) (Nasdaq: CCCC) is a clinical-stage biopharmaceutical company dedicated to delivering on the promise of targeted protein degradation science to create a new generation of medicines that transform patients’ lives. C4T is leveraging its TORPEDO® platform to efficiently design and optimize small-molecule medicines that harness the body’s natural protein recycling system to rapidly degrade disease-causing proteins, offering the potential to overcome drug resistance, drug undruggable targets and improve patient outcomes. C4T is advancing multiple targeted oncology programs to the clinic and expanding its research platform to deliver the next wave of medicines for difficult-to-treat diseases. For more information, please visit www.c4therapeutics.com.
About CFT1946
CFT1946 is an orally bioavailable BiDAC degrader designed to be potent and selective against BRAF-V600 mutant targets. In pre-clinical studies, CFT1946 is active in vivo and in vitro in models with BRAF-V600E-driven disease and in the escape mutant BRAF models. C4T is advancing CFT1946 to the clinic to study treatment for BRAF-V600 mutant solid tumors including lung, colorectal or melanoma.
C4 Therapeutics wins FDA nod to study cancer candidate in solid tumors
Sep. 29, 2022 8:14 AM ET
By: Dulan Lokuwithana, SA News Editor
- C4 Therapeutics, Inc. (NASDAQ:CCCC) added ~7% pre-market Thursday after the clinical-stage biotech announced that the FDA issued a Study May Proceed Letter to start a Phase 1/2 trial for its oral solid tumor candidate CFT1946.
- https://seekingalpha.com/news/3887093-cccc-stock-on-watch-after-fda-nod-to-study-cancer-candidate-in-solid-tumors
- https://seekingalpha.com/symbol/CCCC
- https://c4therapeutics.com/pipeline
- https://c4therapeutics.com/
Lecanemab
20-Valent Pneumococcal Conjugate Vaccine
Lecanemab
LECANEMAB CONFIRMATORY PHASE 3 CLARITY AD STUDY MET PRIMARY ENDPOINT, SHOWING HIGHLY STATISTICALLY SIGNIFICANT REDUCTION OF CLINICAL DECLINE IN LARGE GLOBAL CLINICAL STUDY OF 1,795 PARTICIPANTS WITH EARLY ALZHEIMER’S DISEASE
SEPTEMBER 27, 2022 • INVESTOR RELATIONS
- ALL KEY SECONDARY ENDPOINTS ALSO MET, DEMONSTRATING HIGHLY STATISTICALLY SIGNIFICANT RESULTS
- PROFILE OF AMYLOID-RELATED IMAGING ABNORMALITIES (ARIA) INCIDENCE WAS WITHIN EXPECTATIONS
- EISAI AIMS TO FILE FOR TRADITIONAL APPROVAL IN THE U.S., AND TO SUBMIT MARKETING AUTHORIZATION APPLICATIONS IN JAPAN AND EUROPE BY THE END OF EISAI FY2022, WHICH ENDS ON MARCH 31, 2023
TOKYO and CAMBRIDGE, Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, "Eisai") and Biogen Inc. (Nasdaq: BIIB, Corporate headquarters: Cambridge, Massachusetts, CEO: Michel Vounatsos, "Biogen") announced positive topline results from Eisai’s large global Phase 3 confirmatory Clarity AD clinical trial of lecanemab (development code: BAN2401), an investigational anti-amyloid beta (Aβ) protofibril antibody for the treatment of mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) and mild AD (collectively known as early AD) with confirmed presence of amyloid pathology in the brain. Lecanemab met the primary endpoint (CDR-SB: Clinical Dementia Rating-Sum of Boxes*) and all key secondary endpoints with highly statistically significant results. Eisai will discuss this data with regulatory authorities in the U.S., Japan and Europe with the aim to file for traditional approval in the US and for marketing authorization applications in Japan and Europe by the end of Eisai’s FY2022, which ends March 31, 2023. Additionally, Eisai will present the Clarity AD study results on November 29, 2022, at the Clinical Trials on Alzheimer’s Congress (CTAD), and publish the findings in a peer-reviewed medical journal.
* CDR-SB is a numeric scale used to quantify the various severity of symptoms of dementia. Based on interviews of people living with AD and family/caregivers, qualified healthcare professionals assess cognitive and functional performance in six areas: memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care. The total score of the six areas is the score of CDR-SB, and CDR-SB is also used as an appropriate item for evaluating the effectiveness of therapeutic drugs targeting the early stages of AD.
Lecanemab treatment met the primary endpoint and reduced clinical decline on the global cognitive and functional scale, CDR-SB, compared with placebo at 18 months by 27%, which represents a treatment difference in the score change of -0.45 (p=0.00005) in the analysis of Intent-to-treat (ITT) population. Starting as early as six months, across all time points, the treatment showed highly statistically significant changes in CDR-SB from baseline compared to placebo (all p-values are less than 0.01). All key secondary endpoints were also met with highly statistically significant results compared with placebo (p<0.01). Key secondary endpoints were the change from baseline at 18 months compared with placebo of treatment in amyloid levels in the brain measured by amyloid positron emission tomography (PET), the AD Assessment Scale-cognitive subscale14 (ADAS-cog14), AD Composite Score (ADCOMS) and the AD Cooperative Study-Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
The incidence of amyloid-related imaging abnormalities-edema/effusion (ARIA-E), an adverse event associated with anti-amyloid antibodies, was 12.5% in the lecanemab group and 1.7% in the placebo group. The incidence of symptomatic ARIA-E was 2.8% in the lecanemab group and 0.0% in the placebo group. The ARIA-H (ARIA cerebral microhemorrhages, cerebral macrohemorrhages, and superficial siderosis) rate was 17.0% in the lecanemab group and 8.7% in the placebo group. The incidence of symptomatic ARIA-H was 0.7% in the lecanemab group and 0.2% in the placebo group. There was no imbalance in isolated ARIA-H (i.e., ARIA-H in patients who did not also experience ARIA-E) between lecanemab (8.8%) and placebo (7.6%). The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group. Overall, lecanemab’s ARIA incidence profile was within expectations.
Clarity AD was a global confirmatory Phase 3 placebo-controlled, double-blind, parallel-group, randomized study in 1,795 people with early AD. The treatment group was administered a dosage of 10 mg/kg bi-weekly of lecanemab, with participants allocated in a 1:1 ratio to receive either placebo or lecanemab. The baseline characteristics of both placebo and lecanemab groups are similar and well balanced. Eligibility criteria allowed patients with a broad range of comorbidities/comedications: hypertension, diabetes, heart disease, obesity, renal disease and anti-coagulants, etc. Eisai’s recruitment strategy for the Clarity AD clinical trial ensured greater inclusion of ethnic and racial populations in the U.S., resulting in approximately 25% of the total U.S. enrollment including Hispanic and African American persons living with early AD. Due to the inclusive eligibility criteria and the successful recruitment of diverse ethnic and racial populations in the U.S., Clarity AD’s population is generally comparable to the country’s Medicare population.
“Since Eisai launched Aricept in the U.S. and Japan in the late 1990s and obtained its approval in over 100 countries, Eisai has provided the drug to people living with dementia while building empathy for them and their families through disease education efforts and community involvement. The positive result of the lecanemab, an anti-Aβ protofibril antibody, pivotal study after almost 25 years since Aricept’s launch is an important milestone for Eisai in fulfilling our mission to meet the expectations of the Alzheimer’s disease community. Alzheimer’s disease not only presents a great challenge for patients and their families, but it also negatively impacts society, including decreased productivity, increased social costs and disease-related anxiety. We believe that helping to alleviate these burdens will positively impact society as a whole,” said Haruo Naito, Chief Executive Officer at Eisai. “Additionally, the lecanemab Clarity AD study results prove the amyloid hypothesis, in which the abnormal accumulation of Aβ in the brain is one of the main causes of Alzheimer’s disease, when targeted with a protofibril-binding therapy. Eisai believes these findings will create new horizons in the diagnosis and treatment of Alzheimer’s disease as well as further activate innovation for new treatment options. The successful results of the Clarity AD clinical trial would not be possible without the truly inspiring dedication of the study’s participants, their families and caregivers and the clinical investigators around the world. We thank all the people involved in the study for their invaluable contributions.”
“Today’s announcement gives patients and their families hope that lecanemab, if approved, can potentially slow the progression of Alzheimer’s disease, and provide a clinically meaningful impact on cognition and function,” said Michel Vounatsos, Chief Executive Officer at Biogen. “Importantly, the study shows that removal of aggregated amyloid beta in the brain is associated with a slowing of disease in patients at the early stage of the disease. We want to thank the many patients who participated in this groundbreaking global study and want to acknowledge the clinical investigators who worked tirelessly to increase the enrollment of traditionally underrepresented populations. As pioneers in neuroscience, we believe defeating this disease will require multiple approaches and treatment options, and we look forward to continuing the discussion about the significance of these findings with the patient, scientific, and medical communities.”
In July 2022, the U.S. Food and Drug Administration (FDA) accepted Eisai’s Biologics License Application (BLA) for lecanemab under the accelerated approval pathway and granted Priority Review. The Prescription Drugs User Fee Act action date (PDUFA) is set for January 6, 2023. The FDA has agreed that the results of Clarity AD can serve as the confirmatory study to verify the clinical benefit of lecanemab. In an effort to secure traditional FDA approval for lecanemab as soon as possible, Eisai submitted the BLA through the FDA’s Accelerated Approval Pathway so that the agency could complete its review of all lecanemab data with the exception of the data from the confirmatory Clarity AD study.
In March 2022, Eisai began submitting application data, with the exception of Clarity AD data, to Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) under the prior assessment consultation system with the aim of obtaining early approval for lecanemab so that people living with early AD may have access to the therapy as soon as possible.
Eisai serves as the lead of lecanemab development and regulatory submissions globally with both Eisai and Biogen co-commercializing and co-promoting the product and Eisai having final decision-making authority.
2. About Lecanemab
Lecanemab is an investigational humanized monoclonal antibody for AD that is the result of a strategic research alliance between Eisai and BioArctic. Lecanemab selectively binds to neutralize and eliminate soluble, toxic amyloid-beta (Aβ) aggregates (protofibrils) that are thought to contribute to the neurodegenerative process in AD. As such, lecanemab may have the potential to have an effect on disease pathology and to slow down the progression of the disease. Currently, lecanemab is being developed as the only anti- Aβ antibody that can be used for the treatment of early AD without the need for titration. With regard to the results from pre-specified analysis at 18 months of treatment, Study 201 demonstrated reduction of brain Aβ accumulation (P<0.0001) and slowing of disease progression measured by ADCOMS (P<0.05) in early AD subjects. The study did not achieve its primary outcome measure* at 12 months of treatment. The Study 201 open-label extension was initiated after completion of the Core period and a Gap period off treatment of 9-59 months (average of 24 months, n=180 from core study enrolled) to evaluate safety and efficacy, and is underway.
Since July 2020 the Phase 3 clinical study (AHEAD 3-45) for individuals with preclinical AD, meaning they are clinically normal and have intermediate or elevated levels of amyloid in their brains, is ongoing. AHEAD 3-45 is conducted as a public-private partnership between the Alzheimer’s Clinical Trial Consortium that provides the infrastructure for academic clinical trials in AD and related dementias in the U.S, funded by the National Institute on Aging, part of the National Institutes of Health, Eisai and Biogen.
Since January 2022, the Tau NexGen clinical study for Dominantly Inherited AD (DIAD), that is conducted by Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU), led by Washington University School of Medicine in St. Louis, is ongoing.
Furthermore, Eisai has initiated a lecanemab subcutaneous dosing Phase 1 study.
* An 80% or higher estimated probability of demonstrating 25% or greater slowing in clinical decline at 12 months treatment measured by ADCOMS from baseline compared to placebo.
4. About the Collaboration between Eisai and Biogen for AD
Eisai and Biogen have been collaborating on the joint development and commercialization of AD treatments since 2014. Eisai serves as the lead of lecanemab development and regulatory submissions globally with both companies co-commercializing and co-promoting the product and Eisai having final decision-making authority.
5. About the Collaboration between Eisai and BioArctic for AD
Since 2005, Eisai and BioArctic have had a long-term collaboration regarding the development and commercialization of AD treatments. Eisai obtained the global rights to study, develop, manufacture and market lecanemab for the treatment of AD pursuant to an agreement with BioArctic in December 2007. The development and commercialization agreement on the antibody lecanemab back-up was signed in May 2015.
6. About Eisai Co., Ltd.
Eisai’s Corporate Concept is “to give first thought to patients and people in the daily living domain, and to increase the benefits that health care provides.” Under this Concept (also known as human health care (hhc) Concept), we aim to effectively achieve social good in the form of relieving anxiety over health and reducing health disparities. With a global network of R&D facilities, manufacturing sites and marketing subsidiaries, we strive to create and deliver innovative products to target diseases with high unmet medical needs, with a particular focus in our strategic areas of Neurology and Oncology.
In addition, we demonstrate our commitment to the elimination of neglected tropical diseases (NTDs), which is a target (3.3) of the United Nations Sustainable Development Goals (SDGs), with working on various activities together with global partners.
For more information about Eisai, please visit www.eisai.com (for global headquarters: Eisai Co., Ltd.), and connect with us on Twitter @Eisai_SDGs.
7. About Biogen
As pioneers in neuroscience, Biogen discovers, develops, and delivers worldwide innovative therapies for people living with serious neurological diseases as well as related therapeutic adjacencies. As one of the world’s first global biotechnology companies, Biogen was founded in 1978 by Charles Weissmann, Heinz Schaller, Sir Kenneth Murray, and Nobel Prize winners Walter Gilbert and Phillip Sharp. Today, Biogen has a leading portfolio of medicines to treat multiple sclerosis, has introduced the first approved treatment for spinal muscular atrophy, and developed the first and only approved treatment to address a defining pathology of Alzheimer’s disease. Biogen is also commercializing biosimilars and focusing on advancing one of the industry’s most diversified pipelines in neuroscience that will transform the standard of care for patients in several areas of high unmet need.
In 2020, Biogen launched a bold 20-year, $250 million initiative to address the deeply interrelated issues of climate, health, and equity. Healthy Climate, Healthy Lives™ aims to eliminate fossil fuels across the company’s operations, build collaborations with renowned institutions to advance the science to improve human health outcomes, and support underserved communities.
We routinely post information that may be important to investors on our website at www.biogen.com. Follow us on social media - Twitter, LinkedIn, Facebook, YouTube.
Biogen, Eisai drive rally in Alzheimer’s stocks as lecanemab succeeds in late-stage trial
Sep. 28, 2022 6:43 AM ET
Biogen Inc. (BIIB)RHHBY, LLY, SAVA, ESALY, AVXL, ESALF, RHHBF, ANVS, PRTA, ACIU, ABOS, CGTX
By: Dulan Lokuwithana, SA News Editor7 Comments
Biogen (NASDAQ:BIIB) and Japanese drugmaker Eisai (OTCPK:ESALF) (OTCPK:ESALY) announced their experimental Alzheimer's medication lecanemab met the main goal in a large-stage trial, sparking pre-market gains Wednesday in companies with similar drugs in development.
https://seekingalpha.com/symbol/ESALF
https://seekingalpha.com/symbol/ESALY
https://seekingalpha.com/symbol/BIIB
SKYSONA® (elivaldogene autotemcel)
20-Valent Pneumococcal Conjugate Vaccine
20-Valent Pneumococcal Conjugate Vaccine
bluebird bio Receives FDA Accelerated Approval for SKYSONA® Gene Therapy for Early, Active Cerebral Adrenoleukodystrophy (CALD)
SKYSONA is the first FDA approved therapy shown to slow the progression of neurologic dysfunction in boys with this devastating and fatal neurodegenerative disease
Management team to host conference call Monday, September 19, at 8:00 a.m. ET
SOMERVILLE, Mass.--(BUSINESS WIRE)--Sep. 16, 2022-- bluebird bio, Inc. (Nasdaq: BLUE) today announced the U.S. Food and Drug Administration (FDA) has granted Accelerated Approval of SKYSONA® (elivaldogene autotemcel), also known as eli-cel, to slow the progression of neurologic dysfunction in boys 4-17 years of age with early, active cerebral adrenoleukodystrophy (CALD). The Company also confirmed that the previous clinical hold on the eli-cel clinical development program has been lifted.
CALD is a rare, progressive, neurodegenerative disease that primarily affects young boys and causes irreversible, devastating neurologic decline, including major functional disabilities such as loss of communication, cortical blindness, requirement for tube feeding, total incontinence, wheelchair dependence, or complete loss of voluntary movement. Nearly half of patients who do not receive treatment die within five years of symptom onset. Prior to the approval of SKYSONA treatment, effective options were limited to allogeneic hematopoietic stem cell transplant (allo-HSCT), which is associated with the risk of serious potential complications including death, that can increase dramatically in patients without a human leukocyte antigen (HLA) matched donor.
“Children with CALD and their families have been at the heart of bluebird’s mission since the company was founded more than a decade ago,” said Andrew Obenshain, chief executive officer, bluebird bio. “For the ALD community, this long-awaited approval represents significant hope and offers families a new option where, for many, there had been none. We are grateful to every individual who was involved in the development of SKYSONA and are committed to working with providers and payers to make this important treatment option available to patients and their families.”
“The agony of watching your child slip away is something no parent should have to bear,” said Elisa Seeger, co-founder, ALD Alliance. “We have made significant strides in providing children diagnosed with CALD the best chance at life with early identification of ALD through expanded newborn screening. Yet with limited treatment options, early diagnosis is still cause for despair instead of hope for many families. Today, parents whose boys receive a CALD diagnosis can have renewed hope for the future.”
“CALD strikes young boys in the prime of their development, robbing them of core neurologic functions necessary for survival. That is an unimaginable reality for any parent, and as a clinician, it is heartbreaking to have limited treatment options for these children and their families,” said David A. Williams, MD, Chief, Division of Hematology/Oncology, Boston Children’s Hospitali. “After supporting the clinical development of SKYSONA for nearly a decade as a study site, Boston Children’s Hospital is extremely pleased that an FDA-approved therapy is now available for children who urgently need new therapies.”
“As one of the largest and most experienced pediatric gene therapy and stem cell transplant programs in the world, the University of Minnesota is committed to expanding access and advancing care and research for patients with rare diseases like ALD,” said Paul Orchard, MD, a pediatric blood and marrow transplant physician at the University of Minnesota Medical School and M Health Fairview Masonic Children’s Hospital. “It’s crucial for these patients and families to have another therapeutic option for cerebral ALD beyond blood stem cell transplantation utilizing cells from another donor, and we’ve seen firsthand the impact that gene therapy has on our patients. We are encouraged by progress we’re making to treat these rare and devastating diseases.”
As a condition of the SKYSONA Accelerated Approval, bluebird has agreed to provide confirmatory long-term clinical data to the FDA. bluebird anticipates that this will include data from the ongoing long-term follow-up study (LTF-304), which follows patients treated in clinical trials for 15 years, and from commercially treated patients.
bluebird anticipates that commercial product will be available by the end of 2022 through a limited number of Qualified Treatment Centers (QTCs) in the United States, including Boston Children’s Hospital and Children’s Hospital of Philadelphia.
bluebird has set the wholesale acquisition cost of SKYSONA in the U.S. at $3.0M. Additional information is available through bluebird’s patient support program, my bluebird support, which will provide personalized support for patients and their families related to all aspects of the gene therapy journey. Caregivers of patients with CALD can visit mybluebirdsupport.com or call 833-888-NEST (833-888-6378) Monday-Friday between 8 a.m. and 8 p.m. ET to ask questions and enroll.
The SKYSONA Biologics License Application (BLA) was reviewed by the U.S. FDA under Priority Review, and bluebird received a rare pediatric priority review voucher upon approval. SKYSONA was previously granted Orphan Drug designation, Rare Pediatric Disease designation, and Breakthrough Therapy designation.
SKYSONA Clinical Data
The approval of SKYSONA is based on data from bluebird bio’s Phase 2/3 study ALD-102 (Starbeam) (N=32) and Phase 3 ALD-104 (N=35) study.
Both open-label, single-arm studies enrolled patients with early, active CALD who had elevated very long chain fatty acid (VLCFA) values, a Loes score between 0.5 and 9 (inclusive), and gadolinium enhancement on magnetic resonance imaging (MRI) of demyelinating lesions. Additionally, patients were required to have a neurologic function score (NFS) of ≤ 1, indicating limited changes in neurologic function. The efficacy of SKYSONA was compared to a natural history population.
Per protocol, patients treated with SKYSONA were assessed using the NFS and monitored for the emergence of six Major Functional Disabilities (MFDs) associated with CALD progression including loss of communication, cortical blindness, requirement for tube feeding, total incontinence, wheelchair dependence, or complete loss of voluntary movement.
The Accelerated Approval of SKYSONA is based on 24-month MFD-free survival. A post-hoc enrichment analysis in symptomatic patients assessed MFD-free survival from onset of symptoms (NFS ≥ 1) in SKYSONA treated (N=11) and untreated patients (N=7). SKYSONA treated patients had an estimated 72 percent likelihood of MFD-free survival at 24 months from time of first NFS ≥ 1, compared to untreated patients who had only an estimated 43 percent likelihood of MFD-free survival.
The most common non-laboratory adverse reactions (incidence ≥ 20%) are mucositis, nausea, vomiting, febrile neutropenia, alopecia, decreased appetite, abdominal pain, constipation, pyrexia, diarrhea, headache, and rash. The most common Grade 3 or 4 laboratory abnormalities (≥40%) include leukopenia, lymphopenia, thrombocytopenia, neutropenia, anemia, and hypokalemia. Please see SKYSONA Important Safety Information below, including a Boxed Warning for Hematologic Malignancy.
Enrollment is complete and all patients have been treated in both studies; follow-up in ALD-104 is ongoing. All patients who complete 24 months of follow-up in studies ALD-102 or ALD-104 are encouraged to participate in a long-term follow-up study (LTF-304) to continue monitoring safety and efficacy outcomes in boys treated with SKYSONA through 15 years post-treatment. On September 15, 2022, the FDA lifted the clinical hold that was put in place August 2021, prior to the completion of its review of the SKYSONA Biologics License Application.
Indication
SKYSONA is indicated to slow the progression of neurologic dysfunction in boys 4-17 years of age with early, active cerebral adrenoleukodystrophy (CALD). Early, active cerebral adrenoleukodystrophy refers to asymptomatic or mildly symptomatic (neurologic function score, NFS ≤ 1) boys who have gadolinium enhancement on brain magnetic resonance imaging (MRI) and Loes scores of 0.5-9.
This indication is approved under accelerated approval based on 24-month Major Functional Disability (MFD)- free survival. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
Please see full Prescribing Information for SKYSONA, including BOXED WARNING and Medication Guide.
About SKYSONA® (elivaldogene autotemcel), also known as eli-cel
SKYSONA is a one-time gene therapy custom-designed to treat the underlying cause of cerebral adrenoleukodystrophy (CALD). SKYSONA uses ex-vivo transduction with the Lenti-D lentiviral vector (LVV) to add functional copies of the ABCD1 gene into a patient’s own hematopoietic stem cells (HSCs). The addition of the functional ABCD1 gene allows patients to produce the ALD protein (ALDP), which can then participate in the local degradation of very long-chain fatty acids (VLCFAs). This degradation of VLCFAs is believed to slow or possibly prevent further inflammation and demyelination.
About bluebird bio, Inc.
bluebird bio is pursuing curative gene therapies to give patients and their families more bluebird days. With a dedicated focus on severe genetic diseases, bluebird has industry-leading clinical and research programs for sickle cell disease, beta-thalassemia and cerebral adrenoleukodystrophy and is advancing research to apply new technologies to these and other diseases. We custom design each of our therapies to address the underlying cause of disease and have developed in-depth and effective analytical methods to understand the safety of our lentiviral vector technologies and drive the field of gene therapy forward.
Founded in 2010, bluebird has the largest and deepest ex-vivo gene therapy data set in the world—setting the standard for industry. Today, bluebird continues to forge new paths, combining our real-world experience with a deep commitment to patient communities and a people-centric culture that attracts and grows a diverse flock of dedicated birds.
For more information, visit bluebirdbio.com or follow us on social media at @bluebirdbio, LinkedIn, Instagram and YouTube.
SKYSONA and bluebird bio are trademarks of bluebird bio, Inc.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220916005595/en/
Source: bluebird bio, Inc.
Bluebird bio jumps 17% on FDA approval of new gene therapy
Sep. 19, 2022 5:52 AM ET
By: Dulan Lokuwithana, SA News Editor4 Comments
- The commercial-stage biotech bluebird bio, Inc. (NASDAQ:BLUE) added ~17% pre-market Monday after the company announced the FDA approval of its gene therapy Skysona to address the impact of a rare neurodegenerative disease called cerebral adrenoleukodystrophy (CALD).
- https://seekingalpha.com/news/3883642-blue-stock-jumps-on-fda-approval-of-new-gene-therapy
- https://seekingalpha.com/symbol/BLUE
- https://www.bluebirdbio.com/
- https://www.bluebirdbio.com/-/media/bluebirdbio/Corporate%20COM/Files/Skysona/SKYSONA_Medication_Guide.pdf
20-Valent Pneumococcal Conjugate Vaccine
20-Valent Pneumococcal Conjugate Vaccine
20-Valent Pneumococcal Conjugate Vaccine
Pfizer Announces Positive Top-Line Results from Phase 3 Study in 20-Valent Pneumococcal Conjugate Vaccine in Infants in the European Union
Monday, September 19, 2022 - 06:45am
- Positive pivotal top-line data demonstrates 20-valent pneumococcal conjugate vaccine candidate (20vPnC), if approved, can likely help protect against all 20 vaccine serotypes in three-dose series and potentially offer the broadest serotype coverage of any available pneumococcal conjugate vaccine (PCV)
- The safety profile of 20vPnC was favorable and similar to Prevenar 13® (or Prevnar 13® in the U.S.) in this schedule, and concomitant use with common pediatric vaccines was supported and well tolerated
- 20vPnC also showed robust functional antibody responses to the vaccine serotypes post Dose 2 and 3 similar to Prevenar® and Prevenar 13®
- The company intends to file for regulatory approval in the EU in the next few months
NEW YORK--(BUSINESS WIRE)-- Pfizer today announced positive top-line results from its pivotal E.U. Phase 3 study in infants (NCT04546425) evaluating its 20-valent pneumococcal conjugate vaccine candidate (20vPnC) for the prevention of invasive pneumococcal disease (IPD), pneumonia, and acute otitis media caused by the 20 Streptococcus pneumoniae (pneumococcus) serotypes contained in the vaccine for the pediatric population.
The study had three coprimary outcomes, associated with immunogenicity responses one month after the second and third doses of a three-dose vaccination series given at approximately 2, 4, and 11-12 months of age of 20vPnC compared to Prevenar 13®. For the non-inferiority (NI) co-primary objective of immunoglobulin G (IgG) geometric mean concentrations (GMCs) one month after Dose 3 at 11-12 months of age, 19 of the 20 serotypes met the NI criteria with only one serotype narrowly missing. For the NI co-primary objective of IgG GMCs one month after Dose 2, 16 of the 20 serotypes met NI. Finally, for the third NI co-primary objective of the percentage of participants with predefined serotype-specific IgG concentrations one month after Dose 2, nine of the 20 serotypes met the NI criteria. All 20 serotypes showed increased booster responses from post dose 2 to post dose 3 which are indicative of immunological memory and long-term protection. All 20 vaccine serotypes also showed strong functional antibody responses as measured by the opsonophagocytic assay (OPA) post-dose 2 and post dose 3 similar to Prevenar® and Prevenar 13®. The totality of data is therefore directionally consistent with prior clinical experience with Prevenar® and Prevenar 13® after 2 and 3 infant doses, both of which have demonstrated effectiveness in a three-dose schedule against the serotypes contained in the vaccine in post-licensure studies.
In summary, the totality of these positive 20vPnC data, combined with the experience with Prevenar 13® in this schedule, demonstrates that the 20vPnC candidate, if approved, is likely to help protect against all 20 vaccine serotypes in a three-dose vaccine series.
“Today marks another important milestone in the 20vPnC pediatric program, with these data demonstrating 20vPnC’s potential to provide the most comprehensive pneumococcal serotype coverage of any available pneumococcal conjugate vaccine,” said Annaliesa Anderson, Ph.D., Senior Vice President and Chief Scientific Officer, Vaccine Research and Development, Pfizer. “Based on the totality of immunogenicity and safety data, we feel confident that 20vPnC is likely to be protective against all vaccine serotypes in a three-dose series. We are thankful to everyone who worked on or participated in this study, and we look forward to hopefully being able to provide infants with more robust and meaningful protection against more pneumococcal disease-causing serotypes in the near future.”
The safety profile of 20vPnC was similar to Prevenar 13® in this schedule, and concomitant use with common pediatric vaccines were supported.
Pfizer plans to file these data by the end of this year with the European Medicines Agency (EMA). These positive data mark the conclusion of pivotal topline readouts for the 20vPnC pediatric program. Pfizer will also seek to present and publish outcomes from this clinical trial at a future date once safety and immunogenicity data have been fully analyzed.
About the 20vPnC Phase 3 Pediatric Program
In 2020, Pfizer initiated the Phase 3 clinical trial program for the pediatric indication for 20vPnC. Four core Phase 3 pediatric studies will help expand the data on the safety, tolerability, and immunogenicity of 20vPnC. These studies collectively enrolled approximately 4,700 infants and 800 toddlers and children of all ages including:
- A Phase 3 study describing the tolerability and safety and comparing immunogenicity of 20vPnC to Prevenar 13® in infants vaccinated at 2, 4, 6, and 12-15 months of age in the U.S. (NCT04382326)
- A Phase 3 study describing the tolerability and safety of 20vPnC, with Prevenar 13® serving as the control in infants vaccinated at 2, 4, 6, and 12-15 months of age in multiple countries. (NCT04379713)
- A Phase 3 study describing the tolerability and safety and comparing immunogenicity of 20vPnC to Prevenar 13® in infant vaccination at approximately 2, 4, and 11-12 months of age in Europe and Australia (NCT04546425)
- A Phase 3 study in children 15 months through <18 years of age receiving a single dose of 20vPnC in the U.S. (NCT04642079).
About 20vPnC
Pfizer’s 20vPnC pediatric vaccine candidate includes 13 serotypes already included in Prevenar 13® – 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F. The seven new serotypes included in 20vPnC are global causes of invasive pneumococcal disease (IPD), and are associated with high case-fatality rates, antibiotic resistance, and/or meningitis. Together, the 20 serotypes included in 20vPnC are responsible for the majority of currently circulating pneumococcal disease in the EU and globally.
On Feb 14, 2022, the European Commission Decision was adopted for APEXXNAR ® (20vPnC) for the prevention of invasive disease and pneumonia caused by the 20 Streptococcus pneumoniae (pneumococcus) serotypes in the vaccine in adults ages 18 years and older.
INDICATIONS FOR PREVENAR 13®
- Active immunisation for the prevention of invasive disease, pneumonia and acute otitis media caused by Streptococcus pneumoniae in infants, children and adolescents from 6 weeks to 17 years of age.
- Active immunisation for the prevention of invasive disease and pneumonia caused by Streptococcus pneumoniae in adults ≥18 years of age and the elderly.
- The use of Prevenar 13 should be determined on the basis of official recommendations taking into consideration the risk of invasive disease and pneumonia in different age groups, underlying comorbidities as well as the variability of serotype epidemiology in different geographical areas.
INDICATIONS FOR APEXXNAR®
- Active immunisation for the prevention of invasive disease and pneumonia caused by Streptococcus pneumoniae in individuals 18 years of age and older. APEXXNAR ® should be used in accordance with official recommendations.
About Pfizer: Breakthroughs That Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world's premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.Pfizer.com. In addition, to learn more, please visit us on www.Pfizer.com and follow us on Twitter at @Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220919005238/en/
Source: Pfizer Inc.
Pfizer posts topline
data for pneumococcal vaccine from late-stage EU trial for children
Sep. 19, 2022 7:24 AM ET
By: Dulan Lokuwithana, SA News Editor
Pfizer (NYSE:PFE) announced Monday preliminary results from a pivotal EU Phase 3 study designed to evaluate its 20-valent pneumococcal conjugate vaccine candidate 20vPnC for the prevention of invasive pneumococcal disease (IPD), pneumonia, and acute otitis media (inflammation of the middle ear).
https://seekingalpha.com/symbol/PFE
https://prevnar20.pfizerpro.com/
biotecHOPE™ 2022
KT-333
Rigosertib In Combination With Opdivo (Nivolumab)
Rigosertib In Combination With Opdivo (Nivolumab)
Kymera Therapeutics Receives FDA Orphan Drug Designation for KT-333, a First-in-Class, Investigational STAT3 Degrader for the Treatment of Cutaneous T-Cell Lymphoma
Sep 15, 2022
Cutaneous T-Cell Lymphoma is the second orphan drug designation for KT-333
WATERTOWN, Mass., Sept. 15, 2022 (GLOBE NEWSWIRE) -- Kymera Therapeutics, Inc. (NASDAQ: KYMR), a clinical-stage biopharmaceutical company advancing targeted protein degradation to deliver novel small molecule protein degrader medicines, today announced that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation to KT-333 for the treatment of Cutaneous T-cell Lymphoma (CTCL).
KT-333 is a first-in-class degrader of the transcriptional regulator STAT3. Deregulation of STAT3 signaling has been implicated in the pathogenesis of a variety of cancers, including CTCL. There are currently no approved therapies for CTCL that target this pathway. KT-333 received orphan drug designation for the treatment of Peripheral T-cell Lymphoma (PTCL) earlier this year.
“This second orphan drug designation reinforces the potential of KT-333 to impact the lives of a broad range of patients with hematological and solid tumors by targeting STAT3, a protein that has been considered undruggable,” said Nello Mainolfi, Co-Founder, President and CEO of Kymera Therapeutics. “We have a significant opportunity to deliver an important new medicine with this first-in-class heterobifunctional degrader, and we look forward to working with the lymphoma community to rapidly advance KT-333 in CTCL and exploring its potential in other cancers.”
The safety, tolerability and PK/PD of escalating doses of KT-333 are currently being evaluated in an ongoing Phase 1 clinical trial in adult patients with relapsed/refractory liquid and solid tumors, including aggressive lymphomas.
The FDA's Orphan Drug Designation program provides orphan status to drugs defined as those intended for the treatment, diagnosis or prevention of rare diseases that affect fewer than 200,000 people in the United States. Orphan drug designation qualifies the sponsor of the drug for certain development incentives, including tax credits for qualified clinical testing, prescription drug user fee exemptions and seven-year marketing exclusivity upon FDA approval.
About Cutaneous T-Cell Lymphoma
Cutaneous T-cell lymphoma (CTCL) is a general term for non-Hodgkin’s T-cell lymphomas that are primarily characterized by an abnormal accumulation of T-cells in the skin and which account for approximately 25 percent of T-cell lymphomas in the U.S. CTCL can involve the blood, lymph nodes and other internal organs. CTCL is a rare and typically slow-growing cancer with symptoms such as dry skin, potentially severe itching, rashes and enlarged lymph nodes. Since symptoms and skin biopsy findings are similar to other skin conditions, early-stage diagnosis can be difficult.
About Kymera Therapeutics
Kymera Therapeutics (Nasdaq: KYMR) is a biopharmaceutical company pioneering the field of targeted protein degradation, a transformative approach to address disease targets and pathways inaccessible with conventional therapeutics. Kymera’s Pegasus platform is a powerful drug discovery engine, advancing novel small molecule therapies that harness the body’s innate protein recycling machinery to degrade dysregulated, disease-causing proteins. With a focus on undrugged nodes in validated pathways, Kymera is advancing a pipeline of novel therapeutics designed to address the most intractable pathways and provide new treatments for patients. Kymera’s initial programs target IRAK4, IRAKIMiD, and STAT3 within the IL-1R/TLR or JAK/STAT pathways, providing the opportunity to treat patients with a broad range of immune-inflammatory diseases, hematologic malignancies, and solid tumors. For more information, visit www.kymeratx.com.
Founded in 2016, Kymera is headquartered in Watertown, Mass. Kymera has been named a “Fierce 15” biotechnology company by Fierce Biotech and has been recognized by the Boston Business Journal as one of Boston’s “Best Places to Work.” For more information about our people, science, and pipeline, please visit www.kymeratx.com or follow us on Twitter or LinkedIn.
Kymera KT-333 gets FDA orphan drug status for blood cancer subtype
Sep. 15, 2022 8:25 AM ET
Kymera Therapeutics, Inc. (KYMR)
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) granted orphan drug designation to Kymera Therapeutics' (NASDAQ:KYMR) KT-333 to treat Cutaneous T-cell Lymphoma (CTCL).
- https://seekingalpha.com/news/3882983-kymera-kt-333-gets-fda-orphan-drug-status-for-blood-cancer-subtype
- https://seekingalpha.com/symbol/KYMR
- https://www.kymeratx.com/
- https://clinicaltrials.gov/ct2/show/NCT05225584
- https://www.kymeratx.com/wp-content/uploads/2021/12/1865.pdf
Rigosertib In Combination With Opdivo (Nivolumab)
Rigosertib In Combination With Opdivo (Nivolumab)
Rigosertib In Combination With Opdivo (Nivolumab)
Sep 12, 2022
Onconova Therapeutics Announces Updated Data From Investigator-Sponsored Phase 1/2a Trial Evaluating Rigosertib In Combination With Nivolumab In Advanced KRAS-Mutated Non-Small Cell Lung Cancer At The ESMO Congress 2022
- Data show an early signal of efficacy in an extensively pre-treated population with 1 complete response and 2 partial responses achieved in 14 evaluable patients
- Responses achieved in patients with 3 distinct and different KRAS mutations, confirming the MOA of rigosertib being KRAS+ agnostic
- 4 of 14 (29%) evaluable patients demonstrated disease control
- The combination of rigosertib and nivolumab has been well tolerated with no synergistic toxicities observed to-date
NEWTOWN, Pa., Sept. 12, 2022 (GLOBE NEWSWIRE) -- Onconova Therapeutics, Inc. (NASDAQ: ONTX), (“Onconova”), a clinical-stage biopharmaceutical company focused on discovering and developing novel products for patients with cancer, today announced updated data from an investigator-sponsored Phase 1/2a trial of oral rigosertib plus the anti-PD-1 immune checkpoint inhibitor (ICI) nivolumab in advanced KRAS-mutated (KRAS+) non-small cell lung cancer (NSCLC). The data, which are featured in a poster at the European Society for Medical Oncology (ESMO) Congress 2022, show an early and encouraging signal of efficacy in the trial’s extensively pre-treated population. The studied doublet has been well tolerated to-date.
"The emerging data being presented at ESMO are encouraging, as treatment with rigosertib plus nivolumab led to both complete and partial responses in patients with KRAS-mutated lung cancers who failed prior ICI therapy,” said Dr Rajwanth Veluswamy, the principal investigator of the study. “Objective responses showcased rigosertib’s KRAS mutation-agnostic mechanism of action, as each responding patient had a tumor with a different underlying variant. This differentiates rigosertib from agents targeting a single KRAS mutation variant, and positions it to potentially address the unmet needs of a much broader patient population. In addition, the ESMO data demonstrated activity in multiple patients with both low PD-L1 expression at diagnosis and STK11/LKB1 co-mutations, both poor predictive features for current lung cancer treatments."
Key data from the presentation include:
Demographics:
- All enrolled patients failed at least one line of prior therapy with a PD-1 checkpoint inhibitor (includes evaluable and non-evaluable patients)
- 80% of enrolled patients failed at least two lines of prior therapy
Response results (as of August 15th, 2022-data cutoff date):
- 3 of 14 evaluable patients achieved an objective response
- 1 patient achieved a complete response (CR) as per RECIST Criteria, with complete resolution of the primary lung tumor as well as sites of metastatic disease.
- 2 patients achieved a partial response (PR)
- Responses were achieved in patients with 3 distinct KRAS mutations (CR: KRAS G12V; PRs: KRAS G12C/STK11 and Q61H/STK11)
- The mean duration of response is 6.75 months
- 4 of 14 evaluable patients achieved disease control (CR, PR, or stable disease)
About the Investigator-sponsored Phase 1/2a Trial
This Phase 1/2a trial is designed to evaluate the combination of rigosertib and nivolumab in advanced KRAS+ metastatic NSCLC patients who have progressed on standard-of-care with anti-PD-1 monotherapy or anti-PD-1 in combination with chemotherapy. It includes a dose-escalating Phase 1 portion followed by a Phase 2a dose-expansion portion. Patients in the trial receive oral rigosertib twice daily on days 1-21, and intravenous nivolumab on days 1 and 15 of 28-day cycles. The primary endpoints of the trial are safety assessments to determine maximum tolerated dose, and overall response rate. Secondary endpoints include progression-free survival and overall survival. For more information on the trial, see ClinicalTrials.gov Identifier: NCT04263090.
About Onconova Therapeutics, Inc.
Onconova Therapeutics is a clinical-stage biopharmaceutical company focused on discovering and developing novel products for patients with cancer. The Company has proprietary targeted anti-cancer agents designed to disrupt specific cellular pathways that are important for cancer cell proliferation.
Onconova’s novel, proprietary multi-kinase inhibitor narazaciclib (formerly ON 123300) is being evaluated in two separate and complementary Phase 1 dose-escalation and expansion studies. These trials are currently underway in the United States and China.
Onconova’s product candidate rigosertib is being studied in an investigator-sponsored study program, including in a dose-escalation and expansion Phase 1/2a investigator-sponsored study with oral rigosertib in combination with nivolumab for patients with KRAS+ non-small cell lung cancer.
For more information, please visit www.onconova.com.
Onconova rigosertib/Opdivo combo shows promise in advanced lung cancer in trial
Sep. 12, 2022 12:19 PM ET
Onconova Therapeutics, Inc. (ONTX), BMY
By: Ravikash, SA News Editor
Onconova Therapeutics (NASDAQ:ONTX) said updated data from a phase 1/2a trial of oral rigosertib and Bristol-Myers Squibb's (NYSE:BMY) Opdivo (nivolumab) showed early signs of efficacy in certain extensively pre-treated patients with non-small cell lung cancer (NSCLC).
https://seekingalpha.com/symbol/ONTX
https://seekingalpha.com/symbol/BMY
https://www.onconova.com/pipeline/
HyBryte™ (research name SGX301)
Rigosertib In Combination With Opdivo (Nivolumab)
HyBryte™ (research name SGX301)
U.S. Food and Drug Administration Awards $2.6 Million Orphan Products Development Grant for Expanded Study of HyBryte™ in the Treatment of Cutaneous T-Cell Lymphoma
Grant supports study of expanded HyBryte™ treatment, including in the Home Use Setting
PRINCETON, N.J., Sept. 6, 2022 /PRNewswire/ -- Soligenix, Inc. (Nasdaq: SNGX) (Soligenix or the Company), a late-stage biopharmaceutical company focused on developing and commercializing products to treat rare diseases where there is an unmet medical need, announced today that the U.S. Food and Drug Administration (FDA) has awarded an Orphan Products Development grant to support the evaluation of HyBryte™ (synthetic hypericin) for expanded treatment in patients with early-stage CTCL. The grant, totaling $2.6 million over 4 years, was awarded to a prestigious academic institution that was a leading enroller in the recently published positive Phase 3 FLASH (Fluorescent Light Activated Synthetic Hypericin) study in the treatment of early stage cutaneous T-cell lymphoma (CTCL).
"We are pleased the FDA is supporting the HyBryte™ program and giving patients an opportunity to access the therapy in an open-label setting," stated Christopher J. Schaber, President and CEO of Soligenix, Inc. "CTCL is an incredibly difficult to treat orphan disease and remains an area of unmet medical need with a very limited number of safe and effective treatment options. The Phase 3 results provide the basis for our upcoming marketing application and this study will serve to embark on potential home-use of the therapy, augment the safety database as well as provide further real-world evidence into the practical use of HyBryte™ once commercially available."
The clinical study RW-HPN-MF-01, "Assessment of Treatment with Visible Light Activated Synthetic Hypericin Ointment in Mycosis Fungoides Patients" is designed as an open-label, multicenter clinical trial enrolling approximately 50 patients at up to six of the highest enrolling clinical centers that participated in the Phase 3 FLASH study. Patients have the potential to be treated for up to 12 months with twice a week dosing (visible light activation to follow ointment application by 24 ± 6 hours). The primary endpoint for the study will be evaluating the number of treatment successes defined as ≥50% reduction in the cumulative CAILS (Composite Assessment of Index Lesion Severity) score from baseline to end of the treatment. Study initiation is planned for the fourth quarter of 2022.
About HyBryte™
HyBryte™ (research name SGX301) is a novel, first-in-class, photodynamic therapy utilizing safe, visible light for activation. The active ingredient in HyBryte™ is synthetic hypericin, a potent photosensitizer that is topically applied to skin lesions that is taken up by the malignant T-cells, and then activated by visible light 16 to 24 hours later. The use of visible light in the red-yellow spectrum has the advantage of penetrating more deeply into the skin (much more so than ultraviolet light) and therefore potentially treating deeper skin disease and thicker plaques and lesions. This treatment approach avoids the risk of secondary malignancies (including melanoma) inherent with the frequently employed DNA-damaging drugs and other phototherapy that are dependent on ultraviolet exposure. Combined with photoactivation, hypericin has demonstrated significant anti-proliferative effects on activated normal human lymphoid cells and inhibited growth of malignant T-cells isolated from CTCL patients. In a published Phase 2 clinical study in CTCL, patients experienced a statistically significant (p=0.04) improvement with topical hypericin treatment whereas the placebo was ineffective. HyBryte™ has received orphan drug and fast track designations from the FDA, as well as orphan designation from the European Medicines Agency (EMA).
The recently published Phase 3 FLASH trial enrolled a total of 169 patients (166 evaluable) with Stage IA, IB or IIA CTCL. The trial consisted of three treatment cycles. Treatments were administered twice weekly for the first 6 weeks and treatment response was determined at the end of the 8th week of each cycle. In the first double-blind treatment cycle, 116 patients received HyBryte™ treatment (0.25% synthetic hypericin) and 50 received placebo treatment of their index lesions. A total of 16% of the patients receiving HyBryte™ achieved at least a 50% reduction in their lesions (graded using a standard measurement of dermatologic lesions, the CAILS score) compared to only 4% of patients in the placebo group at 8 weeks (p=0.04) during the first treatment cycle (primary endpoint). HyBryte™ treatment in the first cycle was safe and well tolerated.
In the second open-label treatment cycle (Cycle 2), all patients received HyBryte™ treatment of their index lesions. Evaluation of 155 patients in this cycle (110 receiving 12 weeks of HyBryte™ treatment and 45 receiving 6 weeks of placebo treatment followed by 6 weeks of HyBryte™ treatment), demonstrated that the response rate among the 12-week treatment group was 40% (p<0.0001 vs the placebo treatment rate in Cycle 1). Comparison of the 12-week and 6-week treatment groups also revealed a statistically significant improvement (p<0.0001) between the two groups, indicating that continued treatment results in better outcomes. HyBryte™ continued to be safe and well tolerated. Additional analyses also indicated that HyBryte™ is equally effective in treating both plaque (response 42%, p<0.0001 relative to placebo treatment in Cycle 1) and patch (response 37%, p=0.0009 relative to placebo treatment in Cycle 1) lesions of CTCL, a particularly relevant finding given the historical difficulty in treating plaque lesions in particular.
The third (optional) treatment cycle (Cycle 3) was focused on safety and all patients could elect to receive HyBryte™ treatment of all their lesions. Of note, 66% of patients elected to continue with this optional compassionate use / safety cycle of the study. Of the subset of patients that received HyBryte™ throughout all 3 cycles of treatment, 49% of them demonstrated a positive treatment response (p<0.0001 vs patients receiving placebo in Cycle 1). Moreover, in a subset of patients evaluated in this cycle, it was demonstrated that HyBryte™ is not systemically available, consistent with the general safety of this topical product observed to date. At the end of Cycle 3, HyBryte™ continued to be well tolerated despite extended and increased use of the product to treat multiple lesions.
Overall safety of HyBryte™ is a critical attribute of this treatment and was monitored throughout the three treatment cycles (Cycles 1, 2 and 3) and the 6-month follow-up period. HyBryte's™ mechanism of action is not associated with DNA damage, making it a safer alternative than currently available therapies, all of which are associated with significant and sometimes fatal, side effects. Predominantly these include the risk of melanoma and other malignancies, as well as the risk of significant skin damage and premature skin aging. Currently available treatments are only approved in the context of previous treatment failure with other modalities and there is no approved front-line therapy available. Within this landscape, treatment of CTCL is strongly motivated by the safety risk of each product. HyBryte™ potentially represents the safest available efficacious treatment for CTCL. With no systemic absorption, a compound that is not mutagenic and a light source that is not carcinogenic, there is no evidence to date of any potential safety issues.
The Phase 3 CTCL clinical study was partially funded by the National Cancer Institute via a Phase II SBIR grant (#1R44CA210848-01A1) awarded to Soligenix, Inc.
About Soligenix, Inc.
Soligenix is a late-stage biopharmaceutical company focused on developing and commercializing products to treat rare diseases where there is an unmet medical need. Our Specialized BioTherapeutics business segment is developing and moving toward potential commercialization of HyBryte™ (SGX301 or synthetic hypericin) as a novel photodynamic therapy utilizing safe visible light for the treatment of cutaneous T-cell lymphoma (CTCL). With a successful Phase 3 study completed, regulatory approval is being sought and commercialization activities for this product candidate are being advanced initially in the U.S. Development programs in this business segment also include our first-in-class innate defense regulator (IDR) technology, dusquetide (SGX942) for the treatment of inflammatory diseases, including oral mucositis in head and neck cancer, and proprietary formulations of oral beclomethasone 17,21-dipropionate (BDP) for the prevention/treatment of gastrointestinal (GI) disorders characterized by severe inflammation including pediatric Crohn's disease (SGX203).
Our Public Health Solutions business segment includes active development programs for RiVax®, our ricin toxin vaccine candidate, and SGX943, our therapeutic candidate for antibiotic resistant and emerging infectious disease, and our vaccine programs targeting filoviruses (such as Marburg and Ebola) and CiVax™, our vaccine candidate for the prevention of COVID-19 (caused by SARS-CoV-2). The development of our vaccine programs incorporates the use of our proprietary heat stabilization platform technology, known as ThermoVax®. To date, this business segment has been supported with government grant and contract funding from the National Institute of Allergy and Infectious Diseases (NIAID), the Defense Threat Reduction Agency (DTRA) and the Biomedical Advanced Research and Development Authority (BARDA).
For further information regarding Soligenix, Inc., please visit the Company's website at https://www.soligenix.com and follow us on LinkedIn and Twitter at @Soligenix_Inc.
SOURCE Soligenix, Inc.
U.S. FDA awards $2.6M grant for expanded study of Soligenix's HyBryte for skin cancer
Sep. 12, 2022 9:28 AM ET
By: Dania Nadeem, SA News Editor
- Soligenix (NASDAQ:SNGX) is trading 3.2% higher after the U.S. Food and Drug Administration awarded a $2.6M grant to support a study of expanded HyBryte treatment to treat T-cell lymphoma, including at-home usage.
- https://seekingalpha.com/news/3882003-us-fda-awards-26m-grant-for-expanded-study-of-soligenixs-hybryte-for-skin-cancer
- https://seekingalpha.com/symbol/SNGX
- https://www.hybryte.com/
XMT-1660
Sotyktu™ (deucravacitinib)
HyBryte™ (research name SGX301)
Mersana Therapeutics Announces FDA Fast Track Designation Granted to XMT-1660 for the Treatment of Triple-Negative Breast Cancer
September 12, 2022
XMT-1660 currently being studied in a Phase 1 trial enrolling patients with breast, endometrial and ovarian cancers
CAMBRIDGE, Mass., Sept. 12, 2022 (GLOBE NEWSWIRE) -- Mersana Therapeutics, Inc. (NASDAQ: MRSN), a clinical-stage biopharmaceutical company focused on discovering and developing a pipeline of antibody-drug conjugates (ADCs) targeting cancers in areas of high unmet medical need, today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation to XMT-1660 for the treatment of adult patients with advanced or metastatic triple-negative breast cancer (TNBC). XMT-1660 is a B7-H4-directed Dolasynthen antibody drug conjugate with a precise, target-optimized drug-to-antibody ratio (DAR 6) and Mersana’s clinically validated DolaLock microtubule inhibitor payload with controlled bystander effect.
“While breast cancer remains an area of high unmet need, TNBC is associated with particularly poor outcomes and very limited treatment options,” said Anna Protopapas, President and Chief Executive Officer of Mersana Therapeutics. “XMT-1660 has demonstrated promising anti-tumor effects in preclinical studies, and we are excited to have recently initiated our Phase 1 trial to investigate its safety and clinical activity. This Fast Track designation allows for a potentially accelerated regulatory review of XMT-1660 as we seek to offer a new therapy for patients living with a range of B7-H4 expressing tumors.”
Mersana’s ongoing multicenter Phase 1 trial is investigating the safety, tolerability and anti-tumor activity of XMT-1660 in patients with solid tumors, including in breast, endometrial and ovarian cancers. The initial dose escalation portion of this trial will evaluate the safety and tolerability of XMT-1660. The dose expansion portion of the trial will evaluate the safety, tolerability and efficacy of XMT-1660.
The FDA’s Fast Track program is designed to facilitate the development and expedite the review of drug candidates to treat serious conditions and fill an unmet medical need. A product candidate that is granted Fast Track designation may be eligible for several benefits, including more frequent meetings and communications with the FDA and, if certain criteria are met, the potential for Accelerated Approval, Priority Review or Rolling Review of a Biologics License Application (BLA) by the FDA.
About Mersana Therapeutics
Mersana Therapeutics is a clinical-stage biopharmaceutical company using its differentiated and proprietary ADC platforms to rapidly develop novel ADCs with optimal efficacy, safety and tolerability to meaningfully improve the lives of people fighting cancer. Mersana’s lead product candidate, upifitamab rilsodotin (UpRi), is a Dolaflexin ADC targeting NaPi2b that is being studied in UPLIFT, a single-arm registrational trial in patients with platinum-resistant ovarian cancer; UPGRADE, a Phase 1/2 umbrella trial evaluating UpRi in combination with other ovarian cancer therapies; and UP-NEXT, a Phase 3 clinical trial of UpRi as monotherapy maintenance following treatment with platinum doublets in recurrent platinum-sensitive ovarian cancer. Mersana is also advancing XMT-1660, a Dolasynthen ADC targeting B7-H4, and XMT-2056, an Immunosynthen ADC targeting a novel epitope of human epidermal growth factor receptor 2 (HER2), in addition to other earlier-stage assets. In addition, multiple partners are using Mersana’s platforms to advance their ADC pipelines. Mersana Therapeutics was named among the 2021 Top Places to Work in Massachusetts by The Boston Globe. Mersana routinely posts information that may be useful to investors on the “Investors and Media” section of its website at www.mersana.com.
Mersana gains as FDA grants fast track status for breast cancer drug
Sep. 12, 2022 8:22 AM ET
Mersana Therapeutics, Inc. (MRSN)
By: Dulan Lokuwithana, SA News Editor
- Clinical-stage biotech Mersana Therapeutics, Inc. (NASDAQ:MRSN) added ~8% in the pre-market trading on the announcement that the FDA issued its Fast Track designation for the company’s antibody-drug conjugate XMT-1660 as a treatment for adults with triple-negative breast cancer (TNBC).
- https://seekingalpha.com/news/3881943-mrsn-stock-gains-fda-grants-fast-track-status-breast-cancer-drug
- https://seekingalpha.com/symbol/MRSN
- https://www.mersana.com/xmt-1660/
Sotyktu™ (deucravacitinib)
Sotyktu™ (deucravacitinib)
Sotyktu™ (deucravacitinib)
Bristol Myers Squibb Announces New Sotyktu™ (deucravacitinib) Long-Term Data Showing Clinical Efficacy Maintained for Up to Two Years with Continuous Treatment in Moderate-to-Severe Plaque Psoriasis
09/10/2022CATEGORY:
Results add to the growing body of evidence and reinforce the efficacy profile of Sotyktu, a once-daily, oral, selective, allosteric tyrosine kinase 2 (TYK2) inhibitor for the treatment of moderate-to-severe plaque psoriasis
New analysis to be presented at the 2022 European Academy of Dermatology and Venereology Congress as part of 26 company-sponsored scientific presentations, demonstrating ongoing commitment to dermatology research
PRINCETON, N.J.--(BUSINESS WIRE)-- Bristol Myers Squibb (NYSE:BMY) today announced new two-year results from the POETYK PSO long-term extension (LTE) trial demonstrating clinical efficacy was maintained with continuous Sotyktu™ (deucravacitinib) treatment in adult patients with moderate-to-severe plaque psoriasis. This analysis assessed patients from the pivotal POETYK PSO-1 trial who transitioned into the LTE trial. At 112 weeks of Sotyktu treatment, modified non-responder imputation (mNRI) response rates were 82.4% for Psoriasis Area and Severity Index (PASI) 75, 55.2% for PASI 90 and 66.5% for static Physician's Global Assessment (sPGA) 0/1.
These data (Presentation #D3T01.1F) and 25 additional abstracts demonstrating Bristol Myers Squibb’s robust body of research in dermatology are being presented at the European Academy of Dermatology and Venereology (EADV) Congress, taking place September 7-10, 2022.
“The reality we are facing is that dermatologists and individuals with psoriasis alike have identified the need for more effective and tolerable oral therapies, as psoriasis is a chronic, systemic, immune-mediated disease that is associated with serious comorbidities,” said Dr. Mark Lebwohl, MD, Dean of Clinical Therapeutics at the Kimberly and Eric J. Waldman Department of Dermatology at the Icahn School of Medicine, Mount Sinai (New York); Dr. Lebwohl was also a participant in the Publication Steering Committee for this study. “These new long-term results showing durable efficacy through up to two years of continuous treatment further support the use of once-daily Sotyktu for people with moderate-to-severe plaque psoriasis and address the need for more effective oral treatment options.”
Of the 262 Sotyktu patients in the analysis, 171 had achieved PASI 75 at Week 16 of the POETYK PSO-1 trial, and among these patients, efficacy was maintained for up to 112 weeks, including response rates for PASI 75 (Week 16, 100%; Week 52, 90.1%; Week 112, 91.0%), PASI 90 (Week 16, 62.6%; Week 52, 64.9%; Week 112, 63.0%) and sPGA 0/1 (Week 16, 84.2%; Week 52, 73.7%; Week 112, 73.5%).
“These two-year follow-up data demonstrate the durable efficacy offered by Sotyktu and its potential to provide long-term, clinically relevant improvement for individuals with moderate-to-severe plaque psoriasis,” said Jonathan Sadeh, MD, MSc, senior vice president of Immunology and Fibrosis Development, Bristol Myers Squibb. “At Bristol Myers Squibb, we are committed to exploring pathbreaking science to elevate care for people burdened by serious immune-mediated diseases and are focused on continuing our research with Sotyktu and other novel molecules in our deep and differentiated portfolio.”
Bristol Myers Squibb thanks the patients and investigators involved in the POETYK PSO clinical trial program.
About the POETYK PSO Clinical Trial Program
PrOgram to Evaluate the efficacy and safety ofdeucravacitinib, a selective TYK2 inhibitor (POETYK) PSO-1 (NCT03624127) and POETYK PSO-2 (NCT03611751) were global Phase 3 studies designed to evaluate the safety and efficacy of deucravacitinib compared to placebo and Otezla® (apremilast) in patients with moderate-to-severe plaque psoriasis. Both POETYK PSO-1, which enrolled 666 patients, and POETYK PSO-2, which enrolled 1,020 patients, were multi-center, randomized, double-blind trials that evaluated deucravacitinib (6 mg once daily) compared with placebo and Otezla (30 mg twice daily). POETYK PSO-2 included a randomized withdrawal and retreatment period after Week 24.
The co-primary endpoints of both POETYK PSO-1 and POETYK PSO-2 were the percentage of patients who achieved Psoriasis Area and Severity Index (PASI) 75 response and those who achieved static Physician's Global Assessment (sPGA) score of 0 or 1 (clear/almost clear) at Week 16 versus placebo. Key secondary endpoints of the trials included the percentage of patients who achieved PASI 75 and sPGA 0/1 compared to Otezla at Week 16 and other measures evaluating deucravacitinib versus placebo and Otezla.
Following the 52-week POETYK PSO-1 and POETYK PSO-2 trials, patients could enroll in the ongoing POETYK PSO-LTE trial (NCT04036435) and receive open-label deucravacitinib 6 mg once-daily. 1,221 patients enrolled in the long-term extension trial and received at least one dose of deucravacitinib. Efficacy was analyzed utilizing treatment failure rules (TFR) method of imputation, along with sensitivity analyses using modified non-responder imputation and as-observed analysis, which have been used in similar analyses with other agents. In addition to POETYK PSO-1, POETYK PSO-2 and POETYK PSO-LTE, Bristol Myers Squibb has evaluated deucravacitinib in two other Phase 3 studies in psoriasis: POETYK PSO-3 (NCT04167462) and POETYK PSO-4 (NCT03924427).
The Journal of the American Academy of Dermatology recently published primary analysis results from the POETYK PSO-1 study.
About Sotyktu™
Sotyktu™ (deucravacitinib) is a selective, allosteric inhibitor of tyrosine kinase 2 (TYK2). TYK2 is a member of the Janus kinase (JAK) family. Sotyktu binds to the regulatory domain of TYK2, stabilizing an inhibitory interaction between the regulatory and the catalytic domains of the enzyme. This results in allosteric inhibition of receptor-mediated activation of TYK2 and its downstream activation of Signal Transducers and Activators of Transcription (STATs) as shown in cell-based assays. Janus kinases function as pairs of homo- or heterodimers in the JAK-STAT pathways. TYK2 pairs with JAK1 to mediate multiple cytokine pathways and also pairs with JAK2 to transmit signals as shown in cell-based assays. The precise mechanism linking inhibition of TYK2 enzyme to therapeutic effectiveness in the treatment of adults with moderate-to-severe plaque psoriasis is not currently known.
The U.S. Food and Drug Administration approved Sotyktu for the treatment of adults with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy on September 9, 2022. Sotyktu is also under regulatory review by the European Medicines Agency and other health authorities around the world for the treatment of moderate-to-severe plaque psoriasis and by Japan's Ministry of Health, Labour and Welfare for the treatment of adults with moderate-to-severe plaque psoriasis, pustular psoriasis and erythrodermic psoriasis.
INDICATION
SOTYKTU™ (deucravacitinib) is indicated for the treatment of moderate-to-severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
Limitations of Use:
SOTYKTU is not recommended for use in combination with other potent immunosuppressants.
Please see U.S. Full Prescribing Information, including Medication Guide, for SOTYKTU.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose mission is to discover, develop and deliver innovative medicines that help patients prevail over serious diseases. For more information about Bristol Myers Squibb, visit us at BMS.com or follow us on LinkedIn, Twitter, YouTube, Facebook and Instagram.
Source: Bristol Myers Squibb
Bristol Myers stock rises on FDA approval of psoriasis therapy Sotyktu; presents long-term efficacy data
Sep. 12, 2022 6:22 AM ET
Bristol-Myers Squibb Company (BMY)
By: Ravikash, SA News Editor3 Comments
The U.S. Food and Drug Administration (FDA) on Sept. 9 approved Bristol Myers Squibb's (NYSE:BMY) Sotyktu (deucravacitinib) to treat adults with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
https://seekingalpha.com/symbol/BMY
Ritlecitinib
Sotyktu™ (deucravacitinib)
Sotyktu™ (deucravacitinib)
FDA and EMA Accept Regulatory Submission for Pfizer’s Ritlecitinib for Individuals 12 Years and Older with Alopecia Areata
Friday, September 09, 2022 - 06:45am
– Filings based on clinical data demonstrating significant scalp hair regrowth versus placebo –
NEW YORK--(BUSINESS WIRE)-- Pfizer Inc. (NYSE: PFE) announced today that the U.S. Food and Drug Administration (FDA) accepted for filing the New Drug Application (NDA) for ritlecitinib for adults and adolescents 12 years of age and older with alopecia areata. The FDA is expected to make a decision in the second-quarter 2023. The European Medicines Agency (EMA) has also accepted the Marketing Authorization Application (MAA) for ritlecitinib in the same patient population with a decision anticipated in the fourth-quarter 2023. Ritlecitinib is an investigational oral once daily treatment that is the first in a new class of oral highly selective kinase inhibitors that is a dual inhibitor of the TEC family of tyrosine kinases and of Janus kinase 3 (JAK3).
Alopecia areata is an autoimmune disease that has an underlying immuno-inflammatory pathogenesis and develops when the immune system attacks the body’s hair follicles, causing hair to fall out. This hair loss often occurs on the scalp, but it can also affect eyebrows, eyelashes, facial hair and other areas of the body. Alopecia areata affects approximately 6.8 million people in the U.S. and around 147 million people globally.
“Alopecia areata is an autoimmune disease that can impact people of all ages, genders, and ethnicities, often having an impact on day-to-day life that goes beyond the hair loss itself,” said Michael Corbo, PhD, Chief Development Officer, Inflammation & Immunology, Pfizer Global Product Development. “We believe that ritlecitinib, if approved, will be an important new treatment option, and we are continuing to work closely with regulatory authorities to bring ritlecitinib to adults and adolescents in the U.S. and the EU.”
The submissions were based on previously announced topline results from the pivotal and dose-ranging Phase 2b/3 ALLEGRO (NCT03732807) study and an ongoing Phase 3 ALLEGRO-LT (NCT04006457) open-label, long-term study. Results from the ALLEGRO Phase 2b/3 study were presented at the 2021 European Academy of Dermatology and Venereology (EADV) Congress and the 2022 American Academy of Dermatology Annual Meeting. Initial data from the ongoing ALLEGRO-LT study will be presented at the 2022 EADV Congress.
Pfizer has also completed regulatory submissions for ritlecitinib in the United Kingdom, China and Japan, and expects decisions in 2023.
About the ALLEGRO Program
The randomized, placebo-controlled, double-blind ALLEGRO Phase 2b/3 study investigated ritlecitinib in patients 12 years of age and older with alopecia areata (n=718). Patients included in the study had 50% or more scalp hair loss, as measured by the Severity of Alopecia Tool (SALT), including patients with alopecia totalis (complete scalp hair loss) and alopecia universalis (complete scalp, face, and body hair loss), and were experiencing a current episode of alopecia areata that had lasted between six months and ten years. Patients were randomized to receive once daily ritlecitinib 30 mg or 50 mg (with or without one month of initial treatment with once daily ritlecitinib 200 mg), ritlecitinib 10 mg or placebo.
In this study, statistically significantly higher proportions of patients treated with ritlecitinib 30 mg and 50 mg (with or without the loading dose) had 80% or more scalp hair coverage (SALT<=20) after six months of treatment versus placebo. The overall safety data demonstrated that ritlecitinib was well tolerated both in adult and adolescent patients. Adverse events (AEs) and serious AEs (SAEs) through Week 48 were experienced by 82% and 2% of patients, respectively, with similar rates across active treatment groups. The most common AEs were headache, nasopharyngitis, and upper respiratory tract infections. Cases of herpes zoster (8), pulmonary embolism (1), and breast cancer (2) were reported; no cardiac events, deaths or opportunistic infections were reported through Week 48.
More information about the ALLEGRO 2b/3 trial can be found at https://www.clinicaltrials.gov.
ALLEGRO-LT is an ongoing Phase 3 open-label, long-term study to investigate the safety and efficacy of ritlecitinib in adults with alopecia areata with 25% or greater hair loss and adolescents from 12 years of age with alopecia areata with 50% or greater hair loss.
About Pfizer: Breakthroughs That Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world's premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.Pfizer.com. In addition, to learn more, please visit us on www.Pfizer.com and follow us on Twitter at @Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220908006121/en/
Source: Pfizer Inc.
PFE Dividend History
https://www.nasdaq.com/market-activity/stocks/pfe/dividend-history
https://seekingalpha.com/symbol/PFE
UNI-494
Group B Streptococcus (GBS)
Group B Streptococcus (GBS)
Unicycive Reports Key Findings of UNI-494 Efficacy in Preclinical Animal Model of Acute Kidney Injury (AKI)
September 07, 2022 7:00am EDT Download as PDF
Established animal model of AKI showed a statistically significant reduction of a key biomarker of kidney injury when treated with UNI-494
AKI remains a serious unmet medical need with no FDA approved drugs for its treatment
On track to file regulatory submission by year end 2022 to initiate first-in-humans Phase 1 study with UNI-494
LOS ALTOS, Calif., Sept. 07, 2022 (GLOBE NEWSWIRE) -- Unicycive Therapeutics, Inc. (Nasdaq: UNCY), a clinical stage biotechnology company developing therapies for patients with kidney disease, today announced key findings of UNI-494 efficacy from a preclinical study in rodent model of Acute Kidney Injury.
UNI-494 is a mitochondrial ATP sensitive potassium (mitoKATP) channel activator that is in development for the treatment of AKI. The Company evaluated the effect of UNI-494 on ischemia-reperfusion induced acute kidney injury (IR-AKI) in rats. Animals (n=10/group) were divided into 4 groups: sham, vehicle control, low dose of UNI-494 and high dose of UNI-494. Kidney injury was induced by 45-minute ischemia of bilateral kidneys. UNI-494 was administered orally 1-hour before the induction of ischemia and kidney function was monitored by measuring urinary creatinine, total urinary albumin, and β-2 microglobulin (β-2 MG). Treatment of animals with the higher dose of UNI-494 resulted in a statistically significant reduction of β-2 MG levels in urine.
“We are excited to report this key finding from the IR-AKI model showing treatment with UNI-494 significantly reduced this key biomarker of kidney injury that is a well-accepted biomarker of proximal renal tubule damage. We look forward to presenting these data, along with other data from the study, at an upcoming scientific meeting,” said Shalabh Gupta, M.D., Chief Executive Officer of Unicycive. “We remain on track to file a regulatory submission by the end of 2022 that will allow us to initiate our Phase 1 study with UNI-494.”
“These are very encouraging results for UNI-494. The rat IR-AKI model is a widely published model of AKI and β-2 MG is an established clinical biomarker of proximal renal tubule damage in AKI. The ability of UNI-494 to significantly reduce β-2 MG in these animals provides compelling support for the clinical development of this new drug for AKI," said Ravi Mehta, M.D., Prof. Emeritus of Medicine at University of California San Diego School of Medicine, and a world-renowned expert in AKI research.
About UNI-494
UNI-494 is a novel proprietary drug that selectively binds to the SUR2B subunit of the mitochondrial KATP channel and activates it to restore mitochondrial function and reduce oxidative stress. UNI-494 is cleaved by esterase enzymes to form nicorandil which is the active metabolite. Nicorandil has extensive safety and efficacy data from multiple clinical trials including a 5,000-patient randomized controlled trial (IONA Study) and there is a consensus in the literature that the activation of mitoKATP channel is the biological basis for the observed cardio-protection and reno-protection in multiple clinical trials.
Unicycive has completed pharmacokinetic, safety pharmacology, genetic toxicity and ADME studies on UNI-494. Repeat dose toxicity studies in two species are on track to be completed in the third quarter. The Company is on track to file a regulatory submission in the second half of 2022 to initiate the Phase I healthy volunteer study.
While Unicycive’s initial focus is on acute kidney injury (AKI), UNI-494’s novel mechanism of action may also hold promise for indications in which mitochondrial dysfunction is implicated such as chronic kidney disease, liver disease (alcoholic hepatitis, hepatic encephalopathy) and ophthalmic disease (dry AMD, macular degeneration, etc).
UNI-494 is protected by issued patent(s) in the U.S. and Europe and a wide range of patent applications worldwide.
About Unicycive Therapeutics
Unicycive Therapeutics is a biotechnology company developing novel treatments for kidney diseases. Unicycive’s lead drug, Renazorb, is a novel phosphate binding agent being developed for the treatment of hyperphosphatemia. UNI-494 is a patent-protected new chemical entity in late preclinical development for the treatment of acute kidney injury. For more information, please visit www.unicycive.com.
SOURCE: Unicycive Therapeutics, Inc.
Unicycive stock soars 25% as kidney drug UNI-494 shows promise in preclinical study in rats
Sep. 07, 2022 8:01 AM ET
Unicycive Therapeutics, Inc. (UNCY)
By: Ravikash, SA News Editor
- Unicycive Therapeutics (NASDAQ:UNCY) said treatment with UNI-494 showed a statistically significant reduction of a key biomarker of kidney injury in a preclinical study of an animal model of acute kidney injury (AKI).
- https://seekingalpha.com/news/3880758-unicycive-stock-soars-25-as-kidney-drug-uni-494-shows-promise-in-preclinical-study-in-rats
- https://seekingalpha.com/symbol/UNCY
- https://unicycive.com/focus/uni-494/
- https://unicycive.com/
Group B Streptococcus (GBS)
Group B Streptococcus (GBS)
Group B Streptococcus (GBS)
FDA Grants Breakthrough Therapy Designation to Pfizer’s Group B Streptococcus Vaccine Candidate to Help Prevent Infection in Infants Via Immunization of Pregnant Women
Wednesday, September 07, 2022 - 06:45am
NEW YORK--(BUSINESS WIRE)-- Pfizer Inc. (NYSE:PFE) today announced that its investigational Group B Streptococcus (GBS) vaccine candidate, GBS6 or PF-06760805, received Breakthrough Therapy Designation from the U.S. Food and Drug Administration (FDA) for the prevention of invasive GBS disease due to the vaccine serotypes in newborns and young infants by active immunization of their mothers during pregnancy.
The FDA decision is informed by the interim analysis of a placebo-controlled Phase 2 study (NCT03765073), evaluating the safety and immunogenicity of GBS6 in healthy pregnant women aged 18 to 40 years, who were vaccinated during the second or early third trimester of pregnancy. The study remains ongoing, and Pfizer will publish outcomes from this clinical trial when it is completed.
“GBS infections can have a devastating effect on newborns and their families. While prenatal screening and antibiotics during childbirth help provide protection against GBS in developed countries, this approach is not fully protective in the first week of life; presents multiple challenges in low- and middle-income countries; and has not been shown effective in preventing disease globally in infants beyond the first week of life and through the vulnerable first three months of life,” said Annaliesa Anderson, Ph.D., Senior Vice President and Head of Vaccine Research & Development, Pfizer. “If approved for pregnant women, GBS6 could help protect newborns from the serious illnesses caused by this disease like meningitis, pneumonia, and sepsis – fulfilling a critical global public health need. We are encouraged by today’s decision and look forward to discussing GBS6 with the FDA and other regulatory agencies to potentially reduce neonatal deaths and positively impact the existing global disease burden of GBS.”
The FDA’s Breakthrough Therapy Designation is designed to expedite the development and review of drugs and vaccines that are intended to treat or prevent serious conditions, and preliminary clinical evidence indicates that the drug or vaccine may demonstrate substantial improvement over available therapy on a clinically significant endpoint(s).1 This decision follows the FDA’s March 2017 decision to grant Fast Track status to GBS6. Fast Track status is a process designed to facilitate the development and expedite the review of new drugs and vaccines intended to treat or prevent serious conditions and address an unmet medical need.2
About GBS6
Hexavalent anti capsular polysaccharide (CPS) / cross reactive material 197 glycoconjugate (GBS6) is an investigational maternal vaccine being developed to help prevent invasive Group B Streptococcus (GBS) in newborns. GBS6 is designed to offer protection against the six most prominent GBS serotypes, which account for 98% of disease worldwide.3 It is being evaluated in an ongoing Phase 2, placebo-controlled study in pregnant women and their infants in South Africa, U.K., and the U.S. and is assessing the safety and immunogenicity of a single dose administered by intramuscular injection during the second or early third trimester of pregnancy to prevent disease in infants. Pfizer is pursuing a clinical development strategy in high-, middle- and low-income countries with the intent to make a successfully developed vaccine available globally as quickly as possible.
In April 2022, GBS6 was granted PRIME designation by the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP). This designation provides enhanced support for the development of medicines that target an unmet medical need.4
In 2016, Pfizer received a grant from the Bill & Melinda Gates Foundation, which supported the ongoing Phase 2 clinical trial of GBS6 as well as a parallel non-interventional natural history study.
About Group B Streptococcus (GBS)
Group B Streptococcus (GBS) is a common bacterium that can cause potentially devastating diseases in infants, including sepsis, pneumonia and meningitis, during the first three months of life. About one in four pregnant women carry GBS bacteria in their body and may pass it along to their baby during or prior to birth.5 Annually, there are an estimated 410,000 GBS cases worldwide, which cause at least 147,000 stillbirths and infant deaths each year.6
About Pfizer: Breakthroughs That Change Patients’ Lives
At Pfizer, we apply science and our global resources to bring therapies to people that extend and significantly improve their lives. We strive to set the standard for quality, safety and value in the discovery, development and manufacture of health care products, including innovative medicines and vaccines. Every day, Pfizer colleagues work across developed and emerging markets to advance wellness, prevention, treatments and cures that challenge the most feared diseases of our time. Consistent with our responsibility as one of the world's premier innovative biopharmaceutical companies, we collaborate with health care providers, governments and local communities to support and expand access to reliable, affordable health care around the world. For more than 170 years, we have worked to make a difference for all who rely on us. We routinely post information that may be important to investors on our website at www.Pfizer.com. In addition, to learn more, please visit us on www.Pfizer.com and follow us on Twitter at @Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook at Facebook.com/Pfizer.
Source: Pfizer Inc.
Pfizer's GBS vaccine for pregnant women to protect infants gets FDA breakthrough therapy status
Sep. 07, 2022 7:15 AM ET
By: Ravikash, SA News Editor1 Comment
- The U.S. Food and Drug Administration (FDA) granted breakthrough therapy designation to Pfizer's (NYSE:PFE) vaccine candidate GBS6 (PF-06760805) for preventing invasive Group B Streptococcus (GBS) disease in newborns by immunization of their mothers during pregnancy.
- https://seekingalpha.com/news/3880731-pfizers-gbs-vaccine-for-pregnant-women-to-protect-infants-gets-fda-breakthrough-therapy-status
- https://seekingalpha.com/symbol/PFE
- https://www.pfizer.com/
- https://www.cdc.gov/groupbstrep/index.html
Sarconeos (BIO101)
Group B Streptococcus (GBS)
Sarconeos (BIO101)
Biophytis Announces Very Promising Top Line Results of its Phase 2-3 COVA Clinical Study in COVID-19-Related Respiratory Failure
Wednesday, September 7, 2022 2:20 AM
Biophytis
https://www.biophytis.com/en/
Topic:
Company Update
PARIS, FRANCE and CAMBRIDGE, MA / ACCESSWIRE / September 7th, 2022 / Biophytis SA (NasdaqCM:BPTS)(Euronext Growth Paris:ALBPS) (the "Company" or "Biophytis"), a clinical-stage biotechnology company focused on the development of therapeutics that slow the degenerative processes associated with aging, including severe respiratory failure in patients suffering from COVID-19, today released top-line results from its phase 2-3 COVA clinical study evaluating Sarconeos (BIO101) in the treatment of COVID-19-related respiratory failure.
The objective of the study was to investigate the efficacy and safety of Sarconeos (BIO101), 350 mg BID in hospitalized COVID-19 patients with hypoxemia, at risk of respiratory failure requiring high flow oxygen or mechanical ventilation, and death. The proportion and time to onset of these negative events were studied for 28 days in the primary analysis, with follow-up of mortality and safety until 90 days after start of treatment. The 233 treated patients were 63 years old on average, 64% of the patients were male, recruited in centers in Europe, the US and Brazil between Q3 2020 and Q1 2022, infected with the main SARS-Cov-2 variants
In the primary analysis, Sarconeos (BIO101) reduced by 39% the risk of respiratory failure or early death at 28 days (primary endpoint) compared to placebo (15.8% vs 26.0%, adjusted difference 11.8% in favor of treatment, p=0.07). Sarconeos (BIO101) reduced both the proportion of patients with respiratory failure (12.7% vs 21.5%) and early death (0.8% vs 2.8%). Sarconeos (BIO101) also significantly (p=0.03) delayed the progression of respiratory failure or early death over 28 days maximum treatment period:
In addition, in this primary analysis, Sarconeos (BIO101) reduced the risk of death at 28 days compared to placebo, in similar proportion to the observed reduction in the risk of respiratory failure or early death and delayed its occurrence within 90 days. These effects are nonetheless not statistically significant.
Sarconeos (BIO101) presents a good safety profile, with a similar proportion of adverse events compared to placebo, particularly severe adverse events (25% vs 31%). In addition, more patients in the placebo group experienced respiratory adverse events than patients in the Sarconeos (BIO101) group (32.7% vs 22.7%, respectively), supporting the main efficacy results.
Further data analysis is still ongoing. Results of which will be communicated to the market and presented in details during a major international scientific conference in the next months.
Stanislas Veillet, CEO of Biophytis, said: "The results obtained with Sarconeos (BIO101) in the fight against COVID-19 are very encouraging. It is the only innovative drug candidate in Europe or the United States directly targeting respiratory failure that has demonstrated clinical efficacy in hospitalized patients with hypoxemia caused by COVID-19. It could be used in combination with certain anti-viral and/or anti-inflammatory drugs, which are now part of the medical practice. We will be sharing these results in the coming months with regulatory agencies, health authorities and our partners in Europe, the United States and Brazil to determine under what conditions we could pursue the development of Sarconeos (BIO101) in COVID-19. I would like to sincerely thank all the patients, caregivers, advisors, and finally the shareholders and employees of Biophytis for their hard work, trust and dedication throughout this study, the results of which come at a time when the fear of an epidemic rebound this winter is growing".
Dr Girish Balachandran Nair, Associate Professor of Medicine in Respiratory and Critical Care, Beaumont Hospital, Royal Oak, MI, USA and Principal Investigator of the COVA study in the USA, adds: "These results are extremely exciting and of public interest. This is great news for the medical community and the general population at risk, especially elderly patients. Indeed, COVID-19 is becoming endemic and will persist for a long time. Sarconeos (BIO101) could provide a real therapeutic alternative for elderly patients, hospitalized with hypoxemia and at risk of respiratory failure."
Based on these very promising results, the Company intends to make this new therapeutic solution available to COVID-19 hospitalized patients at risk of respiratory failure and early death. Actually, according to the Johns Hopkins Coronavirus Resource Center, during the last month in the US, Brazil and France, 2.6 million, 0.5 million and 0.6 million people respectively were infected by COVID-19 and 13.9 thousand, 4.5 thousand and 1.7 thousand died from it. Beyond COVID-19 infection, other infections such as flu can also generate Acute Respiratory Distress Syndrome (ARDS).
Biophytis is currently evaluating the possibility of amending and continuing the Early Access Program (EAP) to make Sarconeos (BIO101) available as soon as this winter to COVID-19 hospitalized patients and at risk of respiratory failure and death. An EAP has already been authorized in Brazil to treat patients in intensive care and further EAP might be filed in other territories including the USA and Europe. This is a first step towards market authorization, the conditions of which will be discussed in the coming months with the relevant regulatory authorities (FDA, EMA and ANVISA).
About the COVA study
As a reminder, the COVA clinical programme (identifier clinicaltrials.gov: NCT04472728) is an international, multi-centre, double-blind, placebo-controlled, group-sequential and adaptive two-part study. It is a phase 2-3 study evaluating Sarconeos (BIO101) in patients aged 45 years and older, hospitalised with severe respiratory manifestations of COVID-19. Part 1 of the COVA study is an exploratory Phase 2 proof-of-concept study designed to provide preliminary data on the safety, tolerability and efficacy of Sarconeos (BIO101) in 50 hospitalised patients with severe respiratory failure in patients suffering from COVID-19. Part 2 of the COVA study is a randomised phase 3 study investigating the safety and efficacy of Sarconeos (BIO101) on respiratory function in patients. Due to the evolution of the pandemia, the company decided
in April 2022 to stop enrolment at 237 patients.
About BIOPHYTIS
Biophytis SA is a clinical-stage biotechnology company specialized in the development of therapeutics that are aimed at slowing the degenerative processes associated with aging and improving functional outcomes for patients suffering from age-related diseases, including severe respiratory failure in patients suffering from COVID-19. Sarconeos (BIO101), our leading drug candidate, is a small molecule, administered orally, being developed as a treatment for sarcopenia in a Phase 2 clinical trial in the United States and Europe (SARA-INT). It has also been studied in a clinical two-part Phase 2-3 study (COVA) for the treatment of severe respiratory manifestations of COVID-19 in Europe, Latin America, and the US. A pediatric formulation of Sarconeos (BIO101) is being developed for thetreatment of Duchenne Muscular Dystrophy (DMD). The Company is based in Paris, France, and Cambridge, Massachusetts. The Company's ordinary shares are listed on Euronext Growth (Ticker: ALBPS -ISIN: FR0012816825) and ADSs (American Depositary Shares) are listed on Nasdaq Capital Market (Ticker BPTS - ISIN: US09076G1040). For more information visit www.biophytis.com.
SOURCE: Biophytis
Biophytis stock soars 45% as COVID drug cuts risk of death, respiratory failure in trial
Sep. 07, 2022 5:44 AM ET
By: Ravikash, SA News Editor
Biophytis (NASDAQ:BPTS) said its drug Sarconeos was better at reducing the risk of respiratory failure or early death in patients with COVID-19,compared to placebo.
https://seekingalpha.com/symbol/BPTS
https://www.biophytis.com/en/pipeline/covid19-programme-clinique-cova/
https://www.biophytis.com/en/our-science/sarcopenie/
Eplontersen
XenpozymeTM (olipudase alfa-rpcp)
Sarconeos (BIO101)
Ionis presents positive results from Phase 3 NEURO-TTRansform study at International Symposium on Amyloidosis
September 7, 2022 at 2:30 AM EDT
- Ionis and AstraZeneca's eplontersen demonstrated a statistically significant and clinically meaningful change from baseline for co-primary and secondary endpoints at 35 weeks compared to the external placebo group
- Eplontersen achieved an 81.2% reduction in the co-primary endpoint of serum transthyretin (TTR) concentration from baseline, demonstrating reduced TTR protein production
- Eplontersen demonstrated a favorable safety and tolerability profile
CARLSBAD, Calif., Sept. 7, 2022 /PRNewswire/ -- Ionis Pharmaceuticals, Inc. (Nasdaq: IONS) today presented positive results from a planned 35-week interim analysis of the Phase 3 NEURO-TTRansform study of Ionis and AstraZeneca's eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN). In the study, eplontersen demonstrated a statistically significant and clinically meaningful change from baseline for its co-primary and secondary efficacy endpoints compared to the external placebo group. Eplontersen demonstrated a favorable safety and tolerability profile. The study results were presented today at the International Symposium on Amyloidosis (ISA) in Heidelberg, Germany.
In the study, eplontersen achieved an 81.2% (p<0.0001) mean reduction in the co-primary endpoint of serum transthyretin (TTR) concentration compared to baseline, demonstrating reduced TTR protein production. Eplontersen also demonstrated a significant treatment effect on the co-primary endpoint of modified Neuropathy Impairment Score +7 (mNIS+7), a measure of neuropathic disease progression, with a statistically significant difference in mean change from baseline versus the external placebo group (p<0.0001). The study also met its key secondary endpoint of change from baseline in the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy (Norfolk QoL-DN), showing that treatment with eplontersen significantly improved patient-reported quality of life compared to the external placebo group (p<0.0001).
Eplontersen demonstrated a favorable safety and tolerability profile. In the study, the rate of treatment emergent adverse events (TEAEs) in the eplontersen group was either lower or similar compared to placebo across all major categories. There were no TEAEs of special interest leading to drug discontinuation.
The study data are consistent with the clinical profile seen across Ionis' other LICA programs, further validating how the company's LIgand-Conjugated Antisense technology positions Ionis to deliver potentially transformative treatments for a broad range of unmet medical needs.
"Eplontersen showed clinically meaningful improvement in neuropathy impairment and quality of life measures relative to baseline. The significant efficacy, combined with a favorable safety and tolerability profile, indicate that eplontersen has the potential to be an important therapeutic option for patients living with this debilitating and fatal disease," said Teresa Coelho, M.D., a neurologist and neurophysiologist at Hospital Santo António, Centro Hospitalar Universitário do Porto, Portugal and an investigator for the NEURO-TTRansform study. Dr. Coelho presented data from the interim analysis at ISA.
"The promising results from NEURO-TTRansform show that eplontersen had a positive impact on disease progression and improved quality of life in a substantial number of patients. We are excited about the potential for delivering a new treatment option to patients living with this relentless and devastating disease," said Eugene Schneider, M.D., Ionis' executive vice president and chief clinical development officer.
Based on the study results, Ionis and AstraZeneca will seek regulatory approval for eplontersen for ATTRv-PN and plan to file a new drug application with the U.S. Food and Drug Administration this year.
As part of a global development and commercialization agreement with AstraZeneca, eplontersen is being jointly developed and commercialized by both companies in the U.S. and will be developed and commercialized in the rest of the world by AstraZeneca (with the exception of Latin America).
Eplontersen was granted Orphan Drug Designation in the U.S. It is also currently being evaluated in the Phase 3 CARDIO-TTRansform study for amyloid transthyretin cardiomyopathy (ATTR-CM), a systemic, progressive and fatal condition that leads to progressive heart failure and death within four years from diagnosis.
About NEURO-TTRansform (NCT04136184)
NEURO-TTRansform is a global, open-label, randomized study evaluating the efficacy and safety of eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN). The study has enrolled adult patients with stage 1 or stage 2 polyneuropathy and will compare efficacy of eplontersen to the historical placebo arm from the TEGSEDI® (inotersen) NEURO-TTR registrational study that Ionis completed in 2017. The final primary endpoint analysis will be completed at week 66 and all patients will be followed until week 85 when they will have the option to transition into the open label extension study.
About Eplontersen
Eplontersen is an investigational antisense medicine that uses Ionis' advanced LIgand-Conjugated Antisense, or LICA, technology designed to inhibit the production of the transthyretin (TTR) protein at its source. Eplontersen, which is planned to be delivered to patients via a self-administered autoinjector, is in development to treat all types of ATTR, a systemic, progressive and fatal disease.
About Ionis Pharmaceuticals, Inc.
For more than 30 years, Ionis has been the leader in RNA-targeted therapy, pioneering new markets and changing standards of care with its novel antisense technology. Ionis currently has three marketed medicines and a premier late-stage pipeline highlighted by industry-leading cardiovascular and neurological franchises. Our scientific innovation began and continues with the knowledge that sick people depend on us, which fuels our vision of becoming a leading, fully integrated biotechnology company.
To learn more about Ionis, visit www.ionispharma.com and follow us on Twitter @ionispharma.
View original content to download multimedia:https://www.prnewswire.com/news-releases/ionis-presents-positive-results-from-phase-3-neuro-ttransform-study-at-international-symposium-on-amyloidosis-301618729.html
SOURCE Ionis Pharmaceuticals, Inc.
AstraZeneca/Ionis present data for rare disease drug meeting trial's main goal
Sep. 07, 2022 6:47 AM ET
Ionis Pharmaceuticals, Inc. (IONS), AZN
By: Ravikash, SA News Editor2 Comments
AstraZeneca (NASDAQ:AZN) and Ionis Pharmaceuticals (NASDAQ:IONS) presented detailed results from a 35-week interim analysis of a phase 3 trial of eplontersen, which had met its main goal, in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN).
The company presented the data at the International Symposium on Amyloidosis in Germany. Broad results were reported in June.
https://seekingalpha.com/symbol/IONS
https://seekingalpha.com/symbol/AZN
https://www.ionispharma.com/medicines/akcea-ttr-l/
XenpozymeTM (olipudase alfa-rpcp)
XenpozymeTM (olipudase alfa-rpcp)
XenpozymeTM (olipudase alfa-rpcp)
August 31, 2022
Press Release: XenpozymeTM (olipudase alfa-rpcp) approved by FDA as first disease-specific treatment for ASMD (non-CNS manifestations)
Press Release: XenpozymeTM (olipudase alfa-rpcp) approved by FDA as first disease-specific treatment for ASMD (non-CNS manifestations)
XenpozymeTM (olipudase alfa-rpcp) approved by FDA as first disease-specific treatment for ASMD (non-CNS manifestations)
Paris, August 31, 2022. The U.S. Food and Drug Administration (FDA) has approved XenpozymeTM (olipudase alfa-rpcp) for the treatment of non-central nervous system (non-CNS) manifestations of acid sphingomyelinase deficiency (ASMD) in adult and pediatric patients. Xenpozyme is the first therapy indicated specifically for the treatment of ASMD, and is currently the only approved treatment for this disease.
Bill Sibold
Executive Vice President, Head, Specialty Care at Sanofi
“Sanofi teams have been dedicated to bringing hope to patients living with ASMD and their families. This is a devastating and extremely rare disease that affects both children and adults. The approval of Xenpozyme represents the culmination of bold work done in research and development, and our unwavering commitment to this historically overlooked community.”
ASMD, historically known as Niemann-Pick disease types A, A/B, and B, is an extremely rare, progressive genetic disease with significant morbidity and mortality. It has been estimated that there are fewer than 120 patients diagnosed with ASMD in the U.S. Approximately two-thirds of patients with ASMD in the U.S. are pediatric. Signs and symptoms of ASMD can present in infancy, childhood, or adulthood, and may include enlarged spleen or liver, difficulty breathing, lung infections, and unusual bruising or bleeding, among other disease manifestations. Until now, management of ASMD included supportive care to address the impact of individual symptoms and careful monitoring to detect potential disease complications.
David Guy
Parent to Kaila, age 16, living with ASMD
“As young parents, it was initially devastating to me and my wife when our daughter, Kaila, received her diagnosis of ASMD. We faced so many unknowns when we first heard the diagnosis: what does this mean, how will this affect her, and most importantly what hope is there for a treatment option? We were grateful to find hope when we enrolled Kaila in the clinical trials for olipudase alfa.”
In the U.S., Xenpozyme received Breakthrough Therapy designation, which expedites the development and review of drugs intended to treat serious or life-threatening diseases and conditions. The FDA evaluated Xenpozyme under Priority Review, which is reserved for medicines that represent potentially significant improvements in efficacy or safety in treating serious conditions.. In March 2022, Xenpozyme was approved in Japan under the SAKIGAKE (or “pioneer”) designation, marking the first approval for olipudase alfa anywhere in the world. In June 2022, the European Commission (EC) approved Xenpozyme for use in Europe.
ASMD represents a spectrum of disease, with two types that may represent opposite ends of a continuum referred to as ASMD type A and ASMD type B. ASMD type A/B is an intermediate form that includes varying degrees of central nervous system (CNS) involvement.
ASCEND and ASCEND-Peds clinical trials showed that Xenpozyme improved lung function and reduced spleen and liver volumes in adults and children
The approval is based on positive data from the ASCEND and ASCEND-Peds clinical trials, in which Xenpozyme showed clinically relevant improvement in lung function (as measured by diffusing capacity of the lung for carbon monoxide, or DLco) and platelet count, and reduction of spleen and liver volumes, with a demonstrated safety profile.
Melissa Wasserstein
MD, Pediatric Genetic Medicine, Albert Einstein College of Medicine and the Children’s Hospital at Montefiore
“ASMD is an extremely rare, progressive, and potentially fatal genetic disease that impacts children and adults around the world. Until now, those living with ASMD have had no FDA-approved treatment to combat this devastating condition. I’m proud of the work that has been done and look forward to witnessing the impact that this treatment may have on those living with ASMD.”
The ASCEND trial evaluated the efficacy and safety of Xenpozyme; 31 adult patients with ASMD type A/B or type B were randomized to receive Xenpozyme or placebo for 52 weeks (primary analysis). In the trial, Xenpozyme improved lung function, assessed as the percent change from baseline to Week 52 in predicted diffusing capacity of the lung for carbon monoxide (DLco), and reduced spleen volume, evaluated as percent change from baseline in multiples of normal (MN).
- Twelve (12) patients treated with Xenpozyme had a mean change in percent predicted DLco from baseline (49.1%) to Week 52 (59.4%). This change represents a 23.9% relative improvement compared to a 3% improvement in DLco from baseline in the 17 patients from the placebo group (48.5%) to Week 52 (49.9%). The difference between the two arms (20.9%) was nominally statistically significant (p=0.0003).
- Thirteen (13) patients treated with Xenpozyme had a mean reduction in spleen volume by 38.9% from baseline (11.5 MN) to Week 52 (7.2 MN) compared to a mean increase by 0.5% for the 17 patients in the placebo group from baseline (11.2 MN) to Week 52 (11.2 MN). The difference between the two arms (39.4%) was nominally statistically significant (p<0.0001).
- Twelve (12) patients treated with Xenpozyme had a mean reduction in liver volume by 26.5% from baseline (1.4 MN) to Week 52 (1.0 MN) compared to a mean decrease of 1.8% for the 17 patients in the placebo group from baseline (1.6 MN) to Week 52 (1.6 MN). The difference between the two arms (24.7%) was nominally statistically significant (p<0.0001).
- Thirteen (13) patients treated with Xenpozyme had a mean improvement in platelet count by 18.3% from baseline (109.3x109/L) to Week 52 (126.4x109/L) compared to increase by 2.7% for the 16 patients in the placebo group from baseline (115.6x109/L) to Week 52 (120.2x109/L). The difference between the two arms (15.6%) was nominally statistically significant (p=0.0280).
- All ASCEND patients treated with Xenpozyme showed improvement in key endpoints (DLco and spleen and liver volume).
- Most frequently reported adverse drug reactions in adults (incidence ≥10%) were headache, cough, diarrhea, hypotension, and ocular hyperemia.
The single-arm ASCEND-Peds trial studied 8 pediatric patients younger than 12 years of age with ASMD type A/B or type B who all received Xenpozyme, with a primary objective of evaluating the safety and tolerability of Xenpozyme for 64 weeks. All patients completed the study and continued in an extension trial. The ASCEND-Peds trial also explored efficacy endpoints of progressive lung disease, spleen and liver enlargement, and platelet count. After one year of treatment (52 weeks):
- Three (3) patients who were able to perform the test at baseline treated with Xenpozyme had a mean relative improvement of 45.9% in percent predicted DLco from baseline (48.5%) to Week 52 (70.9%) (children over the age of five were assessed if they were able to perform the test).
- Eight (8) patients treated with Xenpozyme had mean reduction in spleen volume by 46.7% from baseline (18.3 MN) to Week 52 (9.5 MN).
- Eight (8) patients treated with Xenpozyme had a mean reduction in liver volume by 38.1% from baseline (2.5 MN) to Week 52 (1.6 MN).
- Seven (7) patients treated with Xenpozyme had a mean improvement in platelet count by 37.6% from baseline (136.7x109/L; n=8) to Week 52 (184.5x109/L).
- Serious adverse reactions of anaphylactic reaction were reported in 2 (25%) Xenpozyme-treated pediatric patients.
- Treatment-related serious adverse reactions, hypersensitivity reactions including anaphylaxis, and infusion associated reactions occurred within 24 hours of infusion and were observed in a higher percentage of pediatric patients than in adult patients.
- Most frequently reported adverse drug reactions in pediatric patients (incidence ≥20%) were pyrexia, cough, diarrhea, rhinitis, abdominal pain, vomiting, headache, urticaria, nausea, rash, arthralgia, pruritus, fatigue, and pharyngitis.
A scientific innovation for patients living with ASMD
Xenpozyme, a hydrolytic lysosomal sphingomyelin-specific enzyme replacement therapy, is designed to replace deficient or defective acid sphingomyelinase (ASM), an enzyme that allows for the breakdown of the lipid sphingomyelin. In individuals with ASMD, the deficiency in the ASM enzyme leads to sphingomyelin accumulation in various tissues. Xenpozyme is not expected to cross the blood-brain barrier or modulate CNS manifestations of ASMD. Xenpozyme has not been studied in patients with ASMD type A.
Xenpozyme is adminstered intravenously every two weeks, and its administration requires a dose escalation phase followed by a maintenance phase.
Xenpozyme is expected to be available in the U.S. in the coming weeks. The U.S. list price, or wholesale acquisition cost, of Xenpozyme is $7,142.00 per vial. Actual patient out-of-pocket costs may be lower, as the list price does not reflect insurance coverage, co-pay support for eligible patients, or financial assistance from patient support programs.
Sanofi is committed to helping eligible U.S. patients access the support they need and to help reduce barriers throughout their treatment journey. As part of its commitment to treatment access and affordability for innovative therapies, Sanofi provides disease education, financial and co-pay assistance programs, and other support services to eligible patients. For more information, patients can call 1-800-745-4447 and select Option 3, contact Info@CareConnectPSS.com, or visit www.Xenpozyme.com.
About Sanofi
We are an innovative global healthcare company, driven by one purpose: we chase the miracles of science to improve people’s lives. Our team, across some 100 countries, is dedicated to transforming the practice of medicine by working to turn the impossible into the possible. We provide potentially life-changing treatment options and life-saving vaccine protection to millions of people globally, while putting sustainability and social responsibility at the center of our ambitions.
Sanofi is listed on EURONEXT: SAN and NASDAQ: SNY
FDA approves Sanofi's Xenpozyme for the treatment of rare genetic disease ASMD
Aug. 31, 2022 2:09 PM ET
By: Anuron Mitra, SA News Editor
- The U.S. Food and Drug Administration (FDA) on Wednesday approved Genzyme's Xenpozyme drug for intravenous infusion for the treatment of kids and adults with acid sphingomyelinase deficiency (ASMD), a rare genetic disease.
- Genzyme is a Sanofi (NASDAQ:SNY) company.
- https://seekingalpha.com/news/3879049-fda-approves-sanofis-xenpozyme-for-the-treatment-of-rare-genetic-disease-asmd
- https://seekingalpha.com/symbol/SNY
- https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-acid-sphingomyelinase-deficiency-rare-genetic-disease
- https://www.sanofi.com/en/
Lomecel-B™
XenpozymeTM (olipudase alfa-rpcp)
XenpozymeTM (olipudase alfa-rpcp)
U.S. Food and Drug Administration (FDA) Grants Fast Track Designation for Longeveron’s Lomecel-B™ Product for Treatment of Hypoplastic Left Heart Syndrome (HLHS) in Infants
08/31/2022New designation may expedite FDA review and potential approval to address this life-threatening heart condition affecting approximately 1,000 babies per year
MIAMI, Aug. 31, 2022 (GLOBE NEWSWIRE) -- Longeveron Inc. (NASDAQ: LGVN) ("Longeveron" or "Company"), a clinical stage biotechnology company developing cellular therapies for chronic aging-related and life-threatening conditions, today announced the U.S. Food and Drug Administration (FDA) has granted Fast Track Designation to Lomecel-B™ for the treatment of Hypoplastic Left Heart Syndrome (HLHS), a rare and life-threatening congenital heart defect affecting approximately 1,000 infants per year. Lomecel-B™, an investigational allogeneic, bone marrow-derived medicinal signaling cell (MSC) product, is currently in a Phase 2a trial for HLHS.
Fast Track Designation is intended to facilitate development and expedite the review of drugs that treat serious conditions and fill an unmet medical need so a product can potentially be approved and reach patients more quickly. Fast Track Designation enables the company to have more frequent interactions with the FDA throughout the drug development process and allows for eligibility for priority review and accelerated approval if certain criteria are met, as well as a rolling review. The Fast Track Designation must continue to be met or FDA can withdraw the designation. The FDA previously granted Longeveron’s Lomecel-B™ Orphan Drug and Rare Pediatric Disease designations in November of 2021 for HLHS.
“Fast Track Designation represents a significant milestone in our efforts to develop Lomecel-B™ as a treatment for infants with HLHS,” said Chris Min, M.D., Ph.D., Longeveron’s Interim Chief Executive Officer and Chief Medical Officer. “Fast Track Designation underscores the urgent need in HLHS, and we look forward to continuing to work closely with the FDA to bring this potential new therapy to infants as expeditiously as possible.”
HLHS is a rare congenital heart defect that affects approximately 1,000 babies per year in the U.S. Infants born with HLHS have an underdeveloped or absent left ventricle, which impairs the heart’s ability to pump adequate amounts of blood throughout the body. Patients require three reconstructive heart surgeries within the first five years of life, and many require a heart transplant. Without treatment, the condition is always fatal. Even with reconstructive surgical interventions, HLHS is still associated with high mortality. Overall survival from birth to adolescence is estimated to be 50% to 60%.
Longeveron is currently evaluating Lomecel-B™ in ELPIS II, an ongoing 38-patient, randomized (1:1), blinded, controlled Phase 2a clinical trial intended to evaluate the safety and efficacy of intramyocardial (directly into the heart) injection of the Lomecel-B™ product in infants with HLHS who are undergoing Stage II reconstructive cardiac surgery. In ELPIS, a Phase 1 open-label trial in ten HLHS patients, Lomecel-B™ was found to be well tolerated with no major adverse cardiac events one-year post-surgery, and/or treatment-related infections.
One hundred percent of the infants enrolled in the ELPIS Phase 1 trial (n=10) were alive and had not required a transplant between 2-3.5 years post-surgery. Normally, approximately 20% of patients require heart transplants to survive within one year of Stage II reconstructive surgery. Longeveron recently announced the release of a manuscript entitled “Intramyocardial cell-based therapy during bidirectional cavopulmonary anastomosis for hypoplastic left heart syndrome: The ELPIS phase I trial” on MedRxiv, a preprint server that posts papers before they are peer reviewed. The paper will now undergo peer review prior to publication of the final study report.
About Longeveron Inc.
Longeveron is a clinical stage biotechnology company developing cellular therapies for specific aging-related and life-threatening conditions. The Company’s lead investigational product is the Lomecel-B™ cell-based therapy product, which is derived from culture-expanded medicinal signaling cells (MSCs) that are sourced from bone marrow of young, healthy adult donors. Longeveron believes that by using the same cells that promote tissue repair, organ maintenance, and immune system function, it can develop safe and effective therapies for some of the most difficult disorders associated with the aging process and other medical disorders. Longeveron is currently sponsoring Phase 1 and 2 clinical trials in the following indications: Alzheimer’s disease, hypoplastic left heart syndrome (HLHS), Aging Frailty, and Acute Respiratory Distress Syndrome (ARDS). Additional information about the Company is available at www.longeveron.com.
Source: Longeveron
Longeveron spikes after FDA’s Fast Track Designation for lead candidate
Aug. 31, 2022 8:45 AM ET
By: Dulan Lokuwithana, SA News Editor
- The shares of clinical-stage biotech Longeveron Inc. (NASDAQ:LGVN) jumped in the pre-market trading Wednesday after the company announced that the FDA issued Fast Track Designation for its lead asset Lomecel-B as a treatment for Hypoplastic Left Heart Syndrome (HLHS).
- https://seekingalpha.com/news/3878887-lgvn-stock-spikes-after-fdas-fast-track-designation-for-lead-candidate
- https://seekingalpha.com/symbol/LGVN
- https://www.longeveron.com/lomecel-b
- https://www.longeveron.com/
biotecHOPE™ 2022
RGX-121
Cemdisiran (ALN-CC5)
RGX-121
REGENXBIO PRESENTS ADDITIONAL POSITIVE INTERIM DATA FROM THE PHASE I/II/III CAMPSIITE™ TRIAL OF RGX-121 FOR THE TREATMENT OF MPS II (HUNTER SYNDROME) AT THE SOCIETY FOR THE STUDY OF INBORN ERRORS OF METABOLISM (SSIEM) ANNUAL SYMPOSIUM
August 31, 2022 at 7:05 AM EDT
- New data in Cohort 3 using pivotal program dose level demonstrates largest median reduction in CSF GAGs, continuing to approach normal levels at 48 weeks
- RGX-121, a one-time gene therapy for MPS II, continues to be well-tolerated with no drug-related SAEs across three dose levels
- Positive interim data supports recently announced plan to file Biologics License Application in 2024 using the accelerated approval pathway
ROCKVILLE, Md., Aug. 31, 2022 /PRNewswire/ -- REGENXBIO Inc. (Nasdaq: RGNX) today announced additional positive interim data from the Phase I/II/III CAMPSIITE™ trial of RGX-121 for the treatment of patients up to 5 years old diagnosed with Mucopolysaccharidosis Type II (MPS II), also known as Hunter Syndrome. The results were presented at the Society for the Study of Inborn Errors of Metabolism (SSIEM) Annual Symposium.
"We are pleased to share new, positive interim data from our Phase I/II/III CAMPSIITE trial that continues to demonstrate encouraging reductions of CSF GAGs and supports the selection of dose level 3 for our pivotal program," said Steve Pakola, M.D., Chief Medical Officer of REGENXBIO. "This interim data of Cohorts 1-3 demonstrate dose-dependent reductions in CSF GAGs, key biomarkers of I2S enzyme activity, in additional patients and at longer timepoints than previously presented. RGX-121 has also demonstrated positive impact on neurodevelopmental function. We believe the data supports our plan to advance RGX-121 as quickly as possible using the accelerated approval pathway with the aim of providing a much-needed new treatment option for the MPS II community."
"RGX-121 continues to demonstrate compelling data showing its potential to impact the neurodevelopmental decline of MPS II patients, which remains an unmet need for most affected individuals," said Roberto Giugliani, M.D., Ph.D., Professor, Department of Genetics, UFRGS, Medical Genetics Service, HCPA, Porto Alegre, Brazil. "A successful gene therapy with the potential to provide advantages over current standard of care is something that could provide a meaningful treatment option to the MPS II patient community. I look forward to continuing to follow this trial as the recently announced pivotal program progresses."
RGX-121 is an investigational, one-time gene therapy designed to deliver the gene that encodes the iduronate-2-sulfatase (I2S) enzyme using the AAV9 vector. Data presented at SSIEM was from the Phase I/II portion of the CAMPSIITE trial where the primary endpoint is to evaluate the safety of RGX-121. Secondary and exploratory endpoints include cerebral spinal fluid (CSF) glycosaminoglycans (GAGs), neurodevelopmental assessments, caregiver reported outcomes and systemic biomarkers. RGX-121 is administered directly to the central nervous system (CNS). As of August 1, 2022, patients had been treated across three dose levels, 1.3x1010 genome copies per gram (GC/g) of brain mass (n=3), 6.5x1010 GC/g of brain mass (n=7), and 2.9x1011 GC/g of brain mass (n=4).
Data Summary and Safety Update
As of August 1, 2022, RGX-121 is reported to be well-tolerated across all cohorts with no drug-related serious adverse events (SAEs) in 14 patients dosed with RGX-121. Time of post-administration follow-up ranges from eight weeks to two years. Eleven patients have completed the 48-week immunosuppression regimen per study protocol. Twelve patients were receiving weekly, intravenous enzyme replacement therapy (ERT) at the time of enrollment, per standard of care; three of these patients have discontinued ERT, per investigator discretion, as allowed in the protocol.
CSF GAGs Data
Biomarker data from patients in all three cohorts indicate encouraging, dose-dependent reductions of CSF GAGs following one-time administration of RGX-121. Heparan sulfate (HS) and D2S6, a component of HS closely correlated with severe MPS II, are GAGs that are key biomarkers of I2S enzyme activity and are being measured in the CSF at baseline and after administration of RGX-121. GAGs in the CSF have the potential to be considered a surrogate biomarker that is reasonably likely to predict clinical benefit in MPS II disease under the accelerated approval pathway, as buildup of GAGs in the CSF of MPS II patients correlates with clinical manifestations, including neurodevelopmental deficits.
The majority of patients in all three cohorts demonstrated reductions of HS in the CSF following RGX-121 administration at the last time point available with dose-dependent reductions seen at Weeks 8, 24, and 48 post RGX-121 administration. At Week 48, median reduction of CSF HS from baseline was 33.5% in Cohort 1, 52.9% in Cohort 2 and 62.5% in Cohort 3.
Similarly, dose-dependent reductions of CSF HS D2S6 were observed at last time point available following RGX-121 administration in the majority of patients, with Cohort 3 patients approaching normal levels at 48 weeks. All three cohorts demonstrated reduction in HS D2S6 with dose-dependent reductions seen at Weeks 8, 24, and 48. Median reduction from baseline of 31.9% in Cohort 1, 69.4% in Cohort 2 and 83.1% in Cohort 3 was seen at Week 48.
In addition, I2S protein concentration in the CSF, which was undetectable in all patients prior to dosing, was measurable in Cohort 2 and 3 patients after RGX-121 administration.
Neurodevelopmental and Systemic Data
As previously reported at the 2022 WORLDSymposium™, improvements in neurodevelopmental function and caregiver reported outcomes in Cohorts 1 and 2 demonstrated CNS activity up to 2 years after RGX-121 administration. Additionally, evidence of systemic enzyme expression and biomarker activity was observed in patients across all three cohorts following RGX-121 administration. The majority of patients demonstrated increases in I2S protein concentration levels in plasma following administration of RGX-121. Total urine GAG measures demonstrated evidence of a systemic effect of RGX-121, independent of ERT treatment.
The study findings presented at the SSIEM Annual Symposium will be available under the Presentations & Publications page in the Media section of REGENXBIO's website located at www.regenxbio.com.
About the CAMPSIITE™ Trial
CAMPSIITE is a multicenter, open-label trial enrolling boys with MPS II, aged 4 months up to five years of age. CAMPSIITE is expected to enroll up to 10 MPS II patients to support the BLA filing using the accelerated approval pathway, with the potential to enroll additional patients. These patients will receive a dose of 2.9x1011 GC/g of brain mass of RGX-121, which is the same dose being evaluated in Cohort 3 of the Phase I/II trial. The pivotal program is using commercial-scale cGMP material from REGENXBIO's proprietary, high-yielding suspension-based manufacturing process, named NAVXPress™. In addition to measuring GAGs in the CSF, the trial will continue to collect neurodevelopmental data and caregiver-reported outcomes.
CAMPSIITE is a global trial, which is expected to include sites in the United States, Brazil and Canada. REGENXBIO has begun dosing patients in the pivotal program.
About RGX-121
RGX-121 is designed to use the AAV9 vector to deliver the human iduronate-2-sulfatase gene (IDS) which encodes the iduronate-2-sulfatase (I2S) enzyme to the central nervous system (CNS). Delivery of the IDS gene within cells in the CNS could provide a permanent source of secreted I2S beyond the blood-brain barrier, allowing for long-term cross correction of cells throughout the CNS. RGX-121 has received orphan drug product, rare pediatric disease and Fast Track designations from the U.S. Food and Drug Administration.
About REGENXBIO Inc.
REGENXBIO is a leading clinical-stage biotechnology company seeking to improve lives through the curative potential of gene therapy. REGENXBIO's NAV Technology Platform, a proprietary adeno-associated virus (AAV) gene delivery platform, consists of exclusive rights to more than 100 novel AAV vectors, including AAV7, AAV8, AAV9 and AAVrh10. REGENXBIO and its third-party NAV Technology Platform Licensees are applying the NAV Technology Platform in the development of a broad pipeline of candidates, including late-stage and commercial programs, in multiple therapeutic areas. REGENXBIO is committed to a "5x'25" strategy to progress five AAV Therapeutics from our internal pipeline and licensed programs into pivotal-stage or commercial products by 2025.
View original content to download multimedia:https://www.prnewswire.com/news-releases/regenxbio-presents-additional-positive-interim-data-from-the-phase-iiiiii-campsiite-trial-of-rgx-121-for-the-treatment-of-mps-ii-hunter-syndrome-at-the-society-for-the-study-of-inborn-errors-of-metabolism-ssiem-annual-sympo-301615279.html
SOURCE REGENXBIO Inc.
REGENXBIO shares more data for Hunter Syndrome candidate
Aug. 31, 2022 8:07 AM ET
By: Dulan Lokuwithana, SA News Editor
REGENXBIO Inc. (NASDAQ:RGNX), a biotech focused on gene therapies, announced Wednesday new data supporting the pivotal program for RGX-121, its candidate for the genetic disorder Hunter Syndrome.
https://seekingalpha.com/news/3878866-regenxbio-shares-more-data-for-hunter-syndrome-candidate
https://seekingalpha.com/symbol/RGNX
https://regenxbio.com/rgx-121/
BCX9250
Cemdisiran (ALN-CC5)
RGX-121
FDA Grants Orphan Drug Designation for BioCryst’s ALK-2 Inhibitor, BCX9250, for the Treatment of Fibrodysplasia Ossificans Progressiva
RESEARCH TRIANGLE PARK, N.C., Aug. 31, 2022 (GLOBE NEWSWIRE) -- BioCryst Pharmaceuticals, Inc. (Nasdaq: BCRX) today announced the U.S. Food and Drug Administration (FDA) has granted orphan drug designation for BCX9250 for the treatment of fibrodysplasia ossificans progressiva (FOP).
The FDA has the option to grant orphan drug designation to applicants for the purpose of supporting the development of a drug or biologic intended to treat a disease or condition that affects fewer than 200,000 individuals in the U.S. Companies that receive this designation are eligible for incentives, including tax credits for qualified clinical trials, exemption from user fees and up to seven years of market exclusivity after approval.
“We appreciate the FDA’s decision to grant orphan drug designation to BCX9250 as we work toward our goal of bringing this important oral investigational therapy to FOP patients. The benefits available to us through this designation – and the designations we previously received from the FDA and the EMA – have the potential to advance our ALK-2 inhibitor program as efficiently as possible as we move towards beginning trials in FOP patients next year,” said Dr. Helen Thackray, chief research and development officer of BioCryst.
FOP is an ultra-rare, severely disabling genetic disorder characterized by heterotopic ossification (HO), or the irregular formation of bone outside the normal skeleton. HO can occur in muscles, tendons, ligaments and other connective tissues. Patients with FOP become bound by this irregular ossification over time, with restricted movement and fused joints, resulting in deformities, restricted mobility and premature mortality.
Earlier this year, BioCryst announced that BCX9250 has received Fast Track designation from the FDA, in addition to orphan drug designation and PRIME designation from the European Medicines Agency (EMA).
BioCryst will present three posters featuring data from non-clinical studies and first-in-human Phase 1 safety, tolerability and pharmacokinetics study in healthy subjects from the BCX9250 program at the American Society for Bone and Mineral Research Annual Meeting, which is being held in Austin, Texas, from Sept. 9-12, 2022. As the company previously reported in the Phase 1 study, BCX9250 was safe and well tolerated at all doses studied, with linear and dose-proportional exposure supporting the potential for once-daily dosing.
About BCX9250
BCX9250 is a novel, oral activin receptor-like kinase-2 (ALK-2) inhibitor designed to inhibit the ALK-2 enzyme, which is a part of the normal signaling pathway for bone formation and responds to binding its specific ligands (bone morphogenic proteins, BMPs) by stimulating normal bone growth and renewal in healthy children and adults. Specific activating mutations of the ALK-2 gene are seen in all cases of fibrodysplasia ossificans progressiva (FOP). An activating mutation in ALK-2 is necessary for the disease to occur, making the ALK-2 enzyme an ideal drug target for treatment of FOP. In a Phase 1 clinical trial in healthy subjects, BCX9250 was safe and well tolerated at all doses studied, with linear and dose-proportional exposure supporting the potential for once-daily dosing.
About BioCryst Pharmaceuticals
BioCryst Pharmaceuticals discovers novel, oral, small-molecule medicines that treat rare diseases in which significant unmet medical needs exist and an enzyme plays a key role in the biological pathway of the disease. Oral, once-daily ORLADEYO® (berotralstat) is approved in the United States and multiple global markets. BioCryst has several ongoing development programs including BCX9930, an oral Factor D inhibitor for the treatment of complement-mediated diseases, BCX9250, an ALK-2 inhibitor for the treatment of fibrodysplasia ossificans progressiva, and galidesivir, a potential treatment for Marburg virus disease and yellow fever. RAPIVAB® (peramivir injection) is approved in the U.S. and multiple global markets, with post-marketing commitments ongoing. For more information, please visit the company’s website at www.biocryst.com.
BioCryst wins FDA’s Orphan Drug status for bone disorder therapy
Aug. 31, 2022 7:34 AM ET
BioCryst Pharmaceuticals, Inc. (BCRX)
By: Dulan Lokuwithana, SA News Editor1 Comment
- Commercial-stage biotech BioCryst Pharmaceuticals, Inc. (NASDAQ:BCRX) announced Wednesday that the FDA granted the orphan drug designation for its experimental drug BCX9250 for the treatment of the rare genetic disorder fibrodysplasia ossificans progressiva (FOP).
- https://seekingalpha.com/news/3878846-biocryst-wins-fdas-orphan-drug-status-for-bone-disorder-therapy
- https://seekingalpha.com/symbol/BCRX
- https://www.biocryst.com/our-pipeline/
- https://www.biocryst.com/
Cemdisiran (ALN-CC5)
Cemdisiran (ALN-CC5)
Cemdisiran (ALN-CC5)
Alnylam Reports Positive Results from Phase 2 Study of Investigational Cemdisiran for the Treatment of IgA Nephropathy
Aug 29, 2022
-Treatment with Cemdisiran Resulted in a Higher Proportion of Patients Achieving Clinically Meaningful Reductions in 24-Hour Urine Protein to Creatinine Ratio, as Compared to Patients on Placebo -
- Consistent Proteinuria Reduction Seen with Secondary Endpoints -
- Cemdisiran Was Generally Well-Tolerated in Patients with IgA Nephropathy -
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Aug. 29, 2022-- Alnylam Pharmaceuticals, Inc. (Nasdaq: ALNY) today announced positive results from a Phase 2 study of cemdisiran, an investigational RNAi therapeutic targeting the C5 component of the complement pathway, in development in collaboration with Regeneron Pharmaceuticals for the treatment of adult patients with immunoglobulin A nephropathy (IgAN). The results were presented at the 18th European Meeting on Complement in Human Disease (EMCHD) being held in Bern, Switzerland on August 26-28.
“We are pleased to present additional data from our Phase 2 study demonstrating that cemdisiran had favorable effects on different measures of proteinuria – a strong risk factor for disease progression in patients with IgAN,” said Sonalee Agarwal, Ph.D., Vice President and Program Leader for the Cemdisiran program at Alnylam. “IgAN is an inflammatory disease that can lead to severe loss of kidney function. Thus, given the persistent unmet need in the treatment landscape of this progressive disease, we, together with our partners at Regeneron, are working expeditiously to advance this investigational RNAi therapeutic into Phase 3 clinical development.”
The data showed that at Week 32, as previously reported, cemdisiran demonstrated a clinically meaningful reduction in 24-hour urine protein to creatinine ratio (UPCR) – the primary endpoint of this Phase 2 study – with a 37 percent (90 percent CI: -0.5, 61) reduction in 24-hour UPCR observed relative to placebo. New results that were presented demonstrated an equivalent (36 percent [90 percent CI: -6, 62]) reduction in 24-hour urine total protein and a higher proportion, 32 versus 13 percent, of patients treated with cemdisiran as compared to those on placebo, respectively, achieving greater than or equal to 50 percent reduction in 24-hour UPCR. Spot urine data were consistent with 24-hour urine data, with the initial onset of treatment effect emerging as early as Week 8 and remaining stable over time. Specifically, patients on cemdisiran achieved a 46 percent (90 percent CI: 26, 60) placebo-adjusted reduction from baseline in spot UPCR at 32 weeks.
Furthermore, the results showed that cemdisiran was generally well tolerated in patients with IgAN with no adverse events (AEs) leading to treatment or study discontinuation during the double-blind treatment period. One death occurred in the cemdisiran arm due to cardiorespiratory collapse; this was not considered related to study drug by the study investigator. AEs reported by greater than or equal to 10 percent of patients in the cemdisiran arm were injection site reactions (41 percent) and peripheral edema (14 percent). There were no drug-related serious or severe AEs.
To view all results presented by Alnylam and collaborators at EMCHD please visit Capella.
About the Phase 2 Study
The Phase 2 trial is a randomized, double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of cemdisiran in adult patients with immunoglobulin A nephropathy (IgAN). Thirty-one adult patients (≥18 years and ≤ 65 years of age) with a clinical diagnosis of primary IgAN were randomized in a 2:1 cemdisiran to placebo ratio. The study was conducted in three periods. The first was an observational 14-week run-in period during which patients’ blood pressure, kidney function, degree of hematuria, and proteinuria were measured, and the standard of care remained unchanged. Patients did not receive study drug (cemdisiran or placebo) during this time. The second period was a 32-week treatment period, during which patients were dosed with 600 mg of cemdisiran or placebo every 4 weeks in combination with standard of care (angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARB)). The third period is a 52-week open-label extension (OLE) period to further evaluate the long-term safety and clinical activity of cemdisiran. During the OLE, all patients (including those initially on placebo) are treated with cemdisiran in combination with standard of care. The primary endpoint of the study is the percent change from baseline in 24-hour urine protein to creatinine ratio at week 32. Secondary endpoints include additional measures of proteinuria, changes in hematuria, percent of patients with partial clinical remission, and frequency of adverse events.
About Cemdisiran
Cemdisiran (ALN-CC5) is a subcutaneously administered, investigational RNAi therapeutic targeting the C5 component of the complement pathway. It is being developed in partnership with Regeneron Pharmaceuticals for the treatment of complement-mediated diseases. Cemdisiran utilizes Alnylam’s Enhanced Stabilization Chemistry (ESC)-GalNAc delivery platform.
About Alnylam Pharmaceuticals
Alnylam (Nasdaq: ALNY) has led the translation of RNA interference (RNAi) into a whole new class of innovative medicines with the potential to transform the lives of people afflicted with rare and prevalent diseases with unmet need. Based on Nobel Prize-winning science, RNAi therapeutics represent a powerful, clinically validated approach yielding transformative medicines. Since its founding 20 years ago, Alnylam has led the RNAi Revolution and continues to deliver on a bold vision to turn scientific possibility into reality. Alnylam’s commercial RNAi therapeutic products are ONPATTRO® (patisiran), GIVLAARI® (givosiran), OXLUMO® (lumasiran), AMVUTTRA® (vutrisiran) and Leqvio® (inclisiran) being developed and commercialized by Alnylam’s partner, Novartis. Alnylam has a deep pipeline of investigational medicines, including multiple product candidates that are in late-stage development. Alnylam is executing on its “Alnylam P5x25” strategy to deliver transformative medicines in both rare and common diseases benefiting patients around the world through sustainable innovation and exceptional financial performance, resulting in a leading biotech profile. Alnylam is headquartered in Cambridge, MA. For more information about our people, science and pipeline, please visit www.alnylam.com and engage with us on Twitter at @Alnylam, on LinkedIn, or on Instagram.
Source: Alnylam Pharmaceuticals, Inc.
Alnylam says trial of RNAi therapeutic cemdisiran achieves goals for IgA nephropathy
Aug. 29, 2022 11:18 AM ET
Alnylam Pharmaceuticals, Inc. (ALNY)
By: Jonathan Block, SA News Editor
Alnylam Pharmaceuticals (NASDAQ:ALNY) said that a phase 2 trial of its RNAi therapeutic cemdisiran for immunoglobulin A nephropathy achieved positive results.
- https://seekingalpha.com/news/3877481-alnylam-says-trial-of-rnai-therapeutic-cemdisiran-achieves-goals-for-iga-nephropathy
- https://seekingalpha.com/symbol/ALNY
- https://clinicaltrials.gov/ct2/show/NCT03841448
- https://www.alnylam.com/alnylam-rnai-pipeline
- https://www.alnylam.com/
BCX9930
ROCTAVIAN™ (valoctocogene roxaparvovec)
Cemdisiran (ALN-CC5)
BioCryst Presents Data Demonstrating >99 Percent Suppression of Alternative Pathway Complement Activity with BCX9930 in C3G Patients
Study represents first data with BCX9930 in C3G patients
RESEARCH TRIANGLE PARK, N.C., Aug. 26, 2022 (GLOBE NEWSWIRE) -- BioCryst Pharmaceuticals, Inc. (Nasdaq: BCRX) today announced that its oral Factor D inhibitor, BCX9930, demonstrated >99 percent suppression of the alternative pathway (AP), and that >98 percent suppression was maintained for 24 hours post-dosing, in patients with C3 glomerulopathy (C3G), a rare renal disease that is characterized by dysregulation of the AP of the complement system.
The data, which are the first data with BCX9930 in patients with C3G, are being presented in a poster session at the 18th European Meeting on Complement in Human Disease, which is being held in Bern, Switzerland, from August 26-29, 2022.
“The analyses from this study add to the body of evidence that show Factor D inhibition can correct dysregulation of the alternative pathway and has the potential to be a meaningful treatment approach for multiple complement-mediated diseases. The data are consistent using both commercially available assays and sophisticated proprietary assays our team has developed, which we can also utilize with our next-generation pipeline programs to quickly assess complement activation in vivo early in development,” said Dr. Yarlagadda S. Babu, chief discovery officer of BioCryst.
BioCryst EMCHD 2022 Presentation Highlights
BCX9930, an Oral Factor D Inhibitor, Suppresses Complement Alternative Pathway C3 Convertase Activity in vitro, and in Patients with Complement 3 Glomerulopathy (Poster #80); Sunday, August 28, 2022; 11:45am-1:30pm CET; Hintere Gasse, Building Fab8
- The study assessed the effects of oral BCX9930 on AP activity in ex vivo activated serum from healthy volunteers (n=16) and C3G patients (n=6) who participated in a phase 1, open-label study to evaluate the pharmacokinetics and pharmacodynamics of a single dose of BCX9930.
- One assay was used to assess the ability of BCX9930 to inhibit formation of AP C3 convertase in vitro (Elisa-detecting properdin (P)-bound C3 convertase), two assays were used to assess the ability of BCX9930 to inhibit AP complement activity ex vivo (AP Wieslab kit and multiplex assays), and another assay was used to assess the ability of BCX9930 to inhibit formation of AP C3 convertase ex vivo (immunofixation electrophoresis).
- The analyses found that a single oral dose (600 mg) of BCX9930:
- Demonstrated >99 percent (median) suppression of the AP, and that >98 percent (median) suppression was maintained for 24 hours post-dosing, in C3G patients.
- Achieved rapid (within two hours) and maximal (median >99 percent relative to pre-dose levels) suppression of the generation of C3a, a product of C3 convertase activity, in both healthy volunteers and C3G patients.
- Demonstrated >99 percent (median) suppression of the AP, and that >98 percent (median) suppression was maintained for 24 hours post-dosing, in C3G patients.
- These data support further development of Factor D inhibitors for the treatment of complement-mediated diseases, including C3G and other diseases driven by dysregulation of the AP.
In the study, a single dose of BCX9930 600 mg was generally safe and well-tolerated. Based on prior work with BCX9930, the proposed clinical dose of 400 mg (bid) provides a similar level of AP suppression as the 600 mg single dose used in this study in C3G patients.
Currently, BioCryst is conducting the RENEW proof-of-concept basket study evaluating BCX9930 in C3G, immunoglobulin A nephropathy (IgAN) and primary membranous nephropathy (PMN), all rare renal diseases caused by dysregulation of the alternative pathway.
BioCryst is also currently conducting the REDEEM-1 and REDEEM-2 pivotal trials evaluating BCX9930 in paroxysmal nocturnal hemoglobinuria (PNH).
About BioCryst Pharmaceuticals
BioCryst Pharmaceuticals discovers novel, oral, small-molecule medicines that treat rare diseases in which significant unmet medical needs exist and an enzyme plays a key role in the biological pathway of the disease. Oral, once-daily ORLADEYO® (berotralstat) is approved in the United States and multiple global markets. BioCryst has several ongoing development programs including BCX9930, an oral Factor D inhibitor for the treatment of complement-mediated diseases, BCX9250, an ALK-2 inhibitor for the treatment of fibrodysplasia ossificans progressiva, and galidesivir, a potential treatment for Marburg virus disease and yellow fever. RAPIVAB® (peramivir injection) is approved in the U.S. and multiple global markets, with post-marketing commitments ongoing. For more information, please visit the company’s website at www.biocryst.com.
BioCryst BCX9930 for rare kidney disorder shows promise in early-stage study
Aug. 26, 2022 7:44 AM ET
BioCryst Pharmaceuticals, Inc. (BCRX)
By: Ravikash, SA News Editor
BioCryst Pharmaceuticals (NASDAQ:BCRX) said that a single oral dose of its Factor D inhibitor BCX9930 showed >99% suppression of alternative pathway (AP) in a phase 1 trial in patients with C3 glomerulopathy (C3G).
https://seekingalpha.com/symbol/BCRX
Lifileucel
ROCTAVIAN™ (valoctocogene roxaparvovec)
ROCTAVIAN™ (valoctocogene roxaparvovec)
Iovance Biotherapeutics Initiates Biologics License Application (BLA) Submission for Lifileucel in Advanced Melanoma
First TIL Therapy BLA Submission Initiated with U.S. Food and Drug Administration
Complete BLA Submission on Track for Fourth Quarter 2022
SAN CARLOS, Calif., Aug. 25, 2022 (GLOBE NEWSWIRE) -- Iovance Biotherapeutics, Inc. (NASDAQ: IOVA), a late-stage biotechnology company developing novel T cell-based cancer immunotherapies, today announced that it has initiated a rolling Biologics License Application (BLA) submission to the U.S. Food and Drug Administration (FDA) for lifileucel, a tumor infiltrating lymphocyte (TIL) therapy, in patients with advanced (unresectable or metastatic) melanoma who progressed on or after prior anti-PD-1/L1 therapy, and if BRAF mutation positive, also prior BRAF or BRAF/MEK inhibitor therapy. There are no FDA approved therapies in this treatment setting.
Frederick Vogt, Ph.D., J.D., Interim President and Chief Executive Officer of Iovance, stated, “Initiating our rolling BLA submission for lifileucel is a significant step towards our goal to deliver the first individualized, one-time cell therapy for melanoma patients with significant unmet need. In parallel, we are executing our on-boarding and personnel training at authorized treatment centers, education and awareness initiatives, internal capacity planning, and launch readiness activities to prepare for commercialization. The FDA is supportive of our regulatory approach, and we look forward to continuing this collaboration throughout the submission and review process.”
A rolling BLA allows Iovance to submit portions of the BLA to the FDA on an ongoing basis, which enables the FDA to begin review as early as possible while documents are received. Iovance expects to complete the BLA submission in the fourth quarter of 2022. The rolling BLA submission and eligibility for priority review are benefits available under the FDA’s guidance on expedited programs for serious conditions. The FDA previously granted a regenerative medicine advanced therapy (RMAT) designation for lifileucel in advanced melanoma.
“Lifileucel represents hope and a new treatment for thousands of people with advanced melanoma who have very limited options after they progress on available standard of care,” said Kyleigh LiPira, CEO, Melanoma Research Foundation. “Cell immunotherapies are revolutionizing cancer treatment, and we are excited about the potential for the first FDA-approved TIL cell therapy for the treatment of melanoma, which helps us take another step towards finding a cure.”
The BLA submission for lifileucel is supported by positive clinical data from the C-144-01 clinical trial in patients with advanced melanoma. Iovance plans to present additional results from the C-144-01 trial at a medical meeting later this year.
About Iovance Biotherapeutics, Inc.
Iovance Biotherapeutics aims to be the global leader in innovating, developing and delivering tumor infiltrating lymphocyte (TIL) therapies for patients with cancer. We are pioneering a transformational approach to cure cancer by harnessing the human immune system’s ability to recognize and destroy diverse cancer cells in each patient. Our lead late-stage TIL product candidate, lifileucel for metastatic melanoma, has the potential to become the first approved one-time cell therapy for a solid tumor cancer. The Iovance TIL platform has demonstrated promising clinical data across multiple solid tumors. We are committed to continuous innovation in cell therapy, including gene-edited cell therapy, that may extend and improve life for patients with cancer. For more information, please visit www.iovance.com.
Source: Iovance Biotherapeutics, Inc.
Iovance submits rolling license application to FDA for skin cancer treatment lifileucel
Aug. 25, 2022 9:21 AM ET
Iovance Biotherapeutics, Inc. (IOVA)
By: Anuron Mitra, SA News Editor1 Comment
- Iovance Biotherapeutics (NASDAQ:IOVA) on Thursday said it had submitted a rolling biologics license application (BLA) to the U.S. FDA for its cancer therapy lifileucel for the treatment of advanced melanoma, the most serious type of skin cancer.
- IOVA said it expects to complete the BLA submission in Q4.
- https://seekingalpha.com/news/3876644-iovance-submits-rolling-license-application-to-fda-for-skin-cancer-treatment-lifileucel
- https://www.iovance.com/clinical-pipeline/
- https://www.iovance.com/
- https://seekingalpha.com/symbol/IOVA
ROCTAVIAN™ (valoctocogene roxaparvovec)
ROCTAVIAN™ (valoctocogene roxaparvovec)
ROCTAVIAN™ (valoctocogene roxaparvovec)
First Gene Therapy for Adults with Severe Hemophilia A, BioMarin's ROCTAVIAN™ (valoctocogene roxaparvovec), Approved by European Commission (EC)
Aug 24, 2022
Maintains Orphan Drug Designation (ODD) in the EU Providing 10-years of Market Exclusivity
Significant Benefit Over Existing Therapies for Patients with Severe Hemophilia A in EU Based on EMA Determination of ODD
Conference Call and Webcast to be Held Wed., Aug. 24th at 8:00 pm Eastern
SAN RAFAEL, Calif., Aug. 24, 2022 /PRNewswire/ -- BioMarin Pharmaceutical Inc. (NASDAQ: BMRN) today announced that the European Commission (EC) has granted conditional marketing authorization (CMA) to ROCTAVIAN™ (valoctocogene roxaparvovec) gene therapy for the treatment of severe hemophilia A (congenital Factor VIII deficiency) in adult patients without a history of Factor VIII inhibitors and without detectable antibodies to adeno-associated virus serotype 5 (AAV5). The EC also endorsed EMA's recommendation for Roctavian to maintain orphan drug designation, thereby granting a 10-year period of market exclusivity. The EMA recommendation noted that, even in light of existing treatments, Roctavian may potentially offer a significant benefit to those affected with severe Hemophilia A. The one-time infusion is the first approved gene therapy for hemophilia A and works by delivering a functional gene that is designed to enable the body to produce Factor VIII on its own without the need for continued hemophilia prophylaxis, thus relieving patients of their treatment burden relative to currently available therapies. People with hemophilia A have a mutation in the gene responsible for producing Factor VIII, a protein necessary for blood clotting.
It is estimated that more than 20,000 adults are affected by severe hemophilia A across more than 70 countries in Europe, the Middle East, and Africa. Of the 8,000 adults with severe hemophilia A in the 24 countries within BioMarin's footprint covered by today's EMA approval, there are an estimated 3,200 patients who will be indicated for Roctavian. BioMarin anticipates additional access to ROCTAVIAN™ for patients outside of the EU through named patient sales based on the European Medicines Agency (EMA) approval in countries in the Middle East, Africa and Latin America and expects additional market registrations to be facilitated by the EMA license.
"This approval in the EU represents a medical breakthrough in the treatment of patients with severe hemophilia A that expands the conversation between a patient and physician on treatment choices to now include a one-time infusion that protects from bleeds for several years," said Professor Johannes Oldenburg, Director of the Institute of Experimental Haematology and Transfusion Medicine and the Haemophilia Centre at the University Clinic in Bonn, Germany. "It is exciting to imagine the possibilities of this approved gene therapy, which has demonstrated a substantial and sustained reduction in bleeding for patients, who potentially could be freed from the burden of regular infusions."
"Roctavian approval in Europe is a historic milestone in medicine and is built upon almost four decades of scientific discovery, innovation, and perseverance. We thank the European Commission for recognizing Roctavian's value as the first gene therapy for hemophilia A, a feat that we believe will transform how healthcare professionals and the patient community think about caring for bleeding disorders," said Jean-Jacques Bienaimé, Chairman and Chief Executive Officer of BioMarin. "We are grateful to the patients, investigators and community, who dedicated their time and effort to this achievement and whose aspirations provided the driving force behind making this one-time therapy a reality."
The EC based its decision on a significant body of data from the Roctavian clinical development program, the most extensively studied gene therapy for hemophilia A, including two-year outcomes from the global GENEr8-1 Phase 3 study. The GENEr8-1 Phase 3 study demonstrated stable and durable bleed control, including a reduction in the mean annualized bleeding rate (ABR) and the mean annualized Factor VIII infusion rate. In addition, the data included five and four years of follow-up from the 6e13 vg/kg and 4e13 vg/kg dose cohorts, respectively, in the ongoing Phase 1/2 dose escalation study. BioMarin has committed to continue working with the broader community and the EMA to monitor the long-term effects of treatment. The Product Information will be available shortly on the EMA website under the Medicines tab. Search for "ROCTAVIAN" and select "Human medicine European public assessment report (EPAR): Roctavian. Then select "Product Information" in the Table of Contents and then select "Roctavian: EPAR – Product Information."
A Conditional Marketing Authorization (CMA) recognizes that the medicine fulfils an unmet medical need based on a positive benefit-risk assessment, and that the benefit to public health of the immediate availability on the market outweighs the uncertainties inherent to the fact that additional data are still required. BioMarin will provide further data from ongoing studies within defined timelines to confirm that the benefits continue to outweigh the risks, building on what already constitutes the largest clinical data package for gene therapy in hemophilia A. Conversion to a standard marketing authorization will be contingent on the provision of additional data from currently ongoing Roctavian clinical studies, including longer-term follow up of patients enrolled in the pivotal trial GENEr8-1, as well as a study investigating efficacy and safety of ROCTAVIAN with prophylactic use of corticosteroids (Study 270-303), for which enrollment is now complete.
Orphan drug designation is reserved for medicines treating rare (affecting not more than five in 10,000 people in the EU), life-threatening or chronically debilitating diseases. Authorized orphan medicines benefit from ten years of market exclusivity, protecting them from competition with similar medicines with the same therapeutic indication, which cannot be marketed during the exclusivity period.
BioMarin remains committed to bringing Roctavian to eligible patients with severe hemophilia A in the United States and is targeting a Biologics License Application (BLA) resubmission for Roctavian by the end of September 2022. Typically, BLA resubmissions are followed by a six-month review procedure. However, the Company anticipates three additional months of review may be necessary based on the number of data read-outs that will emerge during the procedure.
Robust Clinical Program
BioMarin has multiple clinical studies underway in its comprehensive gene therapy program for the treatment of hemophilia A. In addition to the global Phase 3 study GENEr8-1 and the ongoing Phase 1/2 dose escalation study, the Company is also conducting a Phase 3B, single arm, open-label study to evaluate the efficacy and safety of Roctavian at a dose of 6e13 vg/kg with prophylactic corticosteroids in people with hemophilia A (Study 270-303). Also ongoing are a Phase 1/2 Study with the 6e13 vg/kg dose of Roctavian in people with hemophilia A with pre-existing AAV5 antibodies (Study 270-203) and aa Phase 1/2 Study with the 6e13 vg/kg dose of Roctavian in people with hemophilia A with active or prior Factor VIII inhibitors (Study 270-205).
About BioMarin
BioMarin is a global biotechnology company that develops and commercializes innovative therapies for people with serious and life-threatening genetic diseases and medical conditions. The Company selects product candidates for diseases and conditions that represent a significant unmet medical need, have well-understood biology and provide an opportunity to be first-to-market or offer a significant benefit over existing products. The Company's portfolio consists of eight commercial products and multiple clinical and preclinical product candidates for the treatment of various diseases. For additional information, please visit www.biomarin.com.
SOURCE BioMarin Pharmaceutical Inc.
BioMarin to resubmit hemophilia therapy for FDA approval after EU nod
Aug. 25, 2022 6:53 AM ET
BioMarin Pharmaceutical Inc. (BMRN)
By: Dulan Lokuwithana, SA News Editor6 Comments
- Announcing the EU approval of Roctavian for hemophilia A, BioMarin Pharmaceutical (NASDAQ:BMRN) disclosed its plans to resubmit the U.S. marketing application for the gene therapy to the FDA by the end of next month.
- https://seekingalpha.com/news/3876536-bmrn-stock-watch-plans-to-resubmit-hemophilia-therapy-for-fda-approval
- https://seekingalpha.com/symbol/BMRN
- https://www.biomarin.com/our-treatments/pipeline/valoctocogene-roxaparvovec-for-severe-hemophilia-a/
MYTESI® (crofelemer) delayed-release tablets
FUJOVEE™ (Abivertinib) (Cytokine Storm – STI 5656)
FUJOVEE™ (Abivertinib) (Cytokine Storm – STI 5656)
Jaguar Health Announces that Orphan Drug Designation Application Submitted to the FDA for Crofelemer for a Severe Congenital Diarrheal Disorder (CDD) Has Been Accepted for Review
Microvillus Inclusion Disease (MVID), a CDD, Is a Life-Threatening and Rare Autosomal Recessive Disease That Affects Newborns and Children and Leads to Significant Morbidity and Mortality From Severe Secretory Diarrhea
Replay Link for Jaguar's August 22, 2022 Investor Webcast Can Be Accessed by Clicking Here; Q2 2022 Represented the Fourth Consecutive Quarter of Growth in Mytesi® Net Revenue
SAN FRANCISCO, CA / ACCESSWIRE / August 23, 2022 / Jaguar Health (NASDAQ:JAGX) today announced that its Orphan Drug Designation (ODD) application for crofelemer submitted to the U.S. Food and Drug Administration for a rare congenital diarrheal disorder called microvillus inclusion disease (MVID) has been accepted by the FDA for review. A response from the FDA on the application is expected by the end of September 2022.
Jaguar today also provided the replay link for the company's August 22, 2022 investor webcast, which can be accessed by clicking here.
"Although our message may have been lost with the overall market turndown yesterday, we were very pleased to announce that our prescription product net revenue was approximately $2.9 million in the second quarter of 2022, representing an increase of approximately 12% over Mytesi net revenue in the first quarter of 2022, which totaled approximately $2.6 million, and an increase of approximately 641% over Mytesi net revenue in the second quarter of 2021, which totaled approximately $0.4 million," said Lisa Conte, Jaguar's president and CEO. "This is the FOURTH consecutive quarter of growth in Mytesi net revenue - which largely represents the funds collected after various insurance and government chargebacks. The continued improvement in net revenue - a key reportable financial measure of commercial performance under GAAP (generally accepted accounting principles) - is largely a result of the efficiencies realized by the transition we completed this past January to a closed network of specialty pharmacies - an initiative that resulted in a meaningful reduction in Mytesi distribution costs as well as a higher average net price."
As announced, Napo Therapeutics, the Italian corporation Jaguar established in Italy in 2021 that focuses on expanding crofelemer access in Europe with an initial focus on orphan designated diseases, submitted an ODD application for crofelemer this past May for MVID to the European Medicines Agency (EMA).
"CDDs are a group of inherited chronic enteropathies characterized by heterogeneous etiology, and each type of CDD is thus a different disease with a different pathogenetic mechanism," said Martire Particco, MD, Chief Medical Officer of Napo Therapeutics. "MVID is a life-threatening and rare autosomal recessive disease that affects newborns and children and leads to significant morbidity and even death from severe secretory diarrhea."
CDDs share a primary common symptom: chronic diarrhea, and therefore secondary symptoms associated with diarrhea, including significant dehydration, metabolic acidosis or alkalosis and malnutrition, among other secondary symptoms, and these symptoms expeditiously emerge and become life-threatening.
Napo Therapeutics' mission is to provide access to Jaguar's proprietary first-in-class plant-based medicine crofelemer in Europe to address such significant rare disease indications. Under its license to crofelemer from Jaguar, Napo Therapeutics' initial focus is on clinical development and future registration in Europe of crofelemer for debilitating orphan disease target indications, starting with short bowel syndrome (SBS) and CDD.
Crofelemer has received ODD from the EMA and the FDA for SBS, which is a complex condition characterized by severe malabsorption of fluids and nutrients due to surgical resection of bowel segments, congenital anomalies, or disease-associated loss of absorption. For SBS patients who endure the catastrophic loss of their bowel, the resulting excessive intestinal fluid output and lifelong restriction and adjustment of oral intake of food and liquids leads to the requirement to receive intravenous fluids for most of every day (parenteral nutrition). This challenges their ability to carry out activities of daily living, or to attend school or work, and has a significant impact on their daily quality of life. Furthermore, lifelong parenteral nutrition leads to potentially life-threatening complications like sepsis and organ failure. SBS affects approximately 10,000 to 20,000 people in the United States1, according to the Crohn's & Colitis Foundation, and it is estimated that the population of SBS patients in Europe is approximately the same size.2
Jaguar anticipates the completion in 2022 of an investigator-initiated proof-of-concept study of crofelemer for SBS, supporting the potential for expanded patient access to crofelemer in Europe in 2023 for this disease. The company has approved this planned trial of crofelemer for SBS, and the third-party investigator is targeting the presentation in December 2022 of results from the SBS study at a global GI conference in Dubai.
About Crofelemer
Crofelemer is a botanical (plant-based) drug extracted and purified from the red bark sap, also referred to as "dragon's blood," of the medicinal Croton lechleri tree in the Amazon Rainforest. Napo Pharmaceuticals, Jaguar Health's wholly owned U.S. subsidiary, has established a sustainable harvesting program, under fair trade practices, for crofelemer to ensure a high degree of quality, ecological integrity, and support for Indigenous communities.
About Jaguar Health, Jaguar Animal Health, Napo Pharmaceuticals, & Napo Therapeutics
Jaguar Health, Inc. is a commercial stage pharmaceuticals company focused on developing novel, plant-based, non-opioid, and sustainably derived prescription medicines for people and animals with GI distress, including chronic, debilitating diarrhea. Jaguar Animal Health is a tradename of Jaguar Health. Jaguar Health's wholly owned subsidiary, Napo Pharmaceuticals, Inc., focuses on developing and commercializing proprietary plant-based human pharmaceuticals from plants harvested responsibly from rainforest areas. Jaguar Health is the majority shareholder of Napo Therapeutics S.p.A. (f/k/a Napo EU S.p.A.), an Italian corporation established by Jaguar Health in Milan, Italy in 2021 that focuses on expanding crofelemer access in Europe.
For more information about Jaguar Health, please visit https://jaguar.health. For more information about Napo Pharmaceuticals, visit www.napopharma.com.
SOURCE: Jaguar Health, Inc.
accesswire.com
https://www.accesswire.com/713157/Jaguar-Health-Announces-that-Orphan-Drug-Designation-Application-Submitted-to-the-FDA-for-Crofelemer-for-a-Severe-Congenital-Diarrheal-Disorder-CDD-Has-Been-Accepted-for-Review
Jaguar's diarrhea disorder therapy gets FDA review for orphan drug status
Aug. 23, 2022 9:42 AM ET
By: Ravikash, SA News Editor
- The U.S. Food and Drug Administration (FDA) accepted to review Jaguar Health's (NASDAQ:JAGX) application seeking orphan drug designation (ODD) for crofelemer to treat microvillus inclusion disease (MVID).
- https://seekingalpha.com/news/3875810-jaguars-diarrhea-disorder-therapy-gets-fda-review-for-orphan-drug-status
- https://seekingalpha.com/symbol/JAGX
- https://mytesi.com/
FUJOVEE™ (Abivertinib) (Cytokine Storm – STI 5656)
FUJOVEE™ (Abivertinib) (Cytokine Storm – STI 5656)
FUJOVEE™ (Abivertinib) (Cytokine Storm – STI 5656)
Sorrento Announces Significant Positive Pivotal Trial Results as Assessed by an Independent Review Committee (IRC) With Matured Long-Term (Over Three Years) Follow-Up Data of Abivertinib for the Treatment of Advanced Non-Small Cell Lung Cancer (NSCLC)
August 23, 2022 at 9:00 AM EDTDownload PDF
- Abivertinib is a novel third-generation epidermal growth factor receptor (EGFR) inhibitor that irreversibly targets mutant forms of EGFR in advanced NSCLC patients who are resistant to first-line EGFR kinase inhibitor therapies.
- In this pivotal study conducted in China, matured data of 209 response evaluable NSCLC patients were assessed by an IRC. The overall response rate (ORR) as confirmed by the IRC was 56.5% (118/209) and among them, 11 patients had complete responses (CR) with a CR rate of 5.3% (11/209) and median overall survival (OS) of 28.2 months.
- Based on these significant positive results from the IRC assessment, Sorrento is closing the study and preparing the materials for a pre-New Drug Application (NDA) meeting with the FDA and potentially submitting for approvals to regulatory agencies of other countries.
SAN DIEGO, Aug. 23, 2022 (GLOBE NEWSWIRE) -- Sorrento Therapeutics, Inc. (Nasdaq: SRNE, "Sorrento") today announced positive results from a pivotal study of Abivertinib on 209 response evaluable, heavily pretreated NSCLC patients by an IRC assessment with matured long-term follow up data.
Abivertinib is a pyrrolopyrimidine-based, third-generation EGFR inhibitor, which is structurally distinct from osimertinib. Abivertinib selectively inhibits EGFR-activating and resistant mutation with nearly 300-fold greater potency as compared with wild-type EGFR. Previously, a positive interim result assessed by investigators was published in the peer-reviewed Clinical Cancer Research journal with interim data (https://clincancerres.aacrjournals.org/content/early/2021/11/04/1078-0432.CCR-21-2595). In these IRC-assessed preliminary topline results with more matured long-term follow up data (previously 16.8 months, now 38.8 months), Abivertinib showed significant treatment benefits in 209 response evaluable, heavily treated NSCLC patients with ORR of 56.5%, and notably a significant CR rate was seen with Abivertinib (5.3%) in comparison with that of osimertinib (Tagrisso) (0.5%)*, while the ORR rate is comparable between the two drugs. This combined data, the ORR of 56.5%, the CR rate of 5.3%, and median OS of 28.2 months (versus Tagrisso’s median OS of 26.8 months)**, is potentially superior to that of the approved third generation EGFR inhibitor (osimertinib). Abivertinib demonstrated significantly efficacious effects in overcoming the resistant mutation in NSCLC. Based on these results, Sorrento is closing the study and preparing the pre-NDA materials and NDA package. Sorrento will request a pre-NDA meeting with the FDA and other regulatory agencies around the world with potential NDA filings pending agreements with the regulatory agencies in different countries.
“We are very encouraged by the significant positive results of Abivertinib assessed by the IRC with long-term follow up data and look forward to meeting with the FDA and other regulatory authorities for the possibility of bringing Abivertinib to the U.S. and global markets,” said Dr. Henry Ji, Chairman and CEO of Sorrento. Abivertinib is one of the multiple clinical and pre-clinical stage assets obtained by Sorrento in the previously completed acquisition of ACEA Therapeutics, Inc. in June of 2021.
*https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/208065Orig1s000MedR.pdf
** https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/208065s025lbl.pdf
About Sorrento Therapeutics, Inc.
Sorrento is a clinical and commercial stage biopharmaceutical company developing new therapies to treat cancer, pain (non-opioid treatments), autoimmune disease and COVID-19. Sorrento's multimodal, multipronged approach to fighting cancer is made possible by its extensive immuno-oncology platforms, including key assets such as next-generation tyrosine kinase inhibitors (TKIs), fully human antibodies (“G-MAB™ library”), immuno-cellular therapies (“DAR-T™”), antibody-drug conjugates (“ADCs”), and oncolytic virus (“Seprehvec™”). Sorrento is also developing potential antiviral therapies and vaccines against coronaviruses, including STI-1558, COVISHIELD™ and COVIDROPS™; and diagnostic test solutions, including COVIMARK™.
Sorrento's commitment to life-enhancing therapies for patients is also demonstrated by our effort to advance a first-in-class (TRPV1 agonist) non-opioid pain management small molecule, resiniferatoxin (“RTX”), and SP-102 (10 mg, dexamethasone sodium phosphate viscous gel) (SEMDEXA™), a novel, viscous gel formulation of a widely used corticosteroid for epidural injections to treat lumbosacral radicular pain, or sciatica, and to commercialize ZTlido® (lidocaine topical system) 1.8% for the treatment of postherpetic neuralgia (PHN). RTX has been cleared for a Phase II trial for intractable pain associated with cancer and a Phase II trial in osteoarthritis patients. Positive final results from the Phase III Pivotal Trial C.L.E.A.R. Program for SEMDEXA™, its novel, non-opioid product for the treatment of lumbosacral radicular pain (sciatica), were announced in March 2022. ZTlido® was approved by the FDA on February 28, 2018.
For more information visit www.sorrentotherapeutics.com
Source: Sorrento Therapeutics, Inc.
Sorrento achieves positive results in pivotal trial for abivertinib in NSCLC
Aug. 23, 2022 10:45 AM ET
Sorrento Therapeutics, Inc. (SRNE)
By: Jonathan Block, SA News Editor
- Sorrento Therapeutics (NASDAQ:SRNE) said that a pivotal study of its candidate abivertinib in non-small cell lung cancer demonstrated an overall response rate of 56.5%.
- https://seekingalpha.com/news/3875837-sorrento-achieves-positive-results-in-pivotal-trial-for-abivertinib-in-nsclc
- https://seekingalpha.com/symbol/SRNE
- https://sorrentotherapeutics.com/research/immuno-oncology/abivertinib/
- https://sorrentotherapeutics.com/
Quizartinib
FUJOVEE™ (Abivertinib) (Cytokine Storm – STI 5656)
CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide)
Quizartinib Marketing Authorization Application Validated by EMA for Treatment of Adult Patients with Newly Diagnosed FLT3- ITD Positive Acute Myeloid Leukemia • Submission based on QuANTUM-First results showing quizartinib plus chemotherapy significantly improved overall survival compared to chemotherapy alone Tokyo & Munich –August 23, 2022 – Daiichi Sankyo (TSE: 4568) today announced that the European Medicines Agency (EMA) has validated the marketing authorization application (MAA) for quizartinib in combination with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and as continuation monotherapy following consolidation, for the treatment of adult patients with newly diagnosed acute myeloid leukemia (AML) that is FMS-like tyrosine kinase 3 internal tandem duplication (FLT3-ITD) positive. AML is one of the most common forms of leukemia in adults, representing about one-third of all cases. 1 In Europe, approximately 18,000 people are diagnosed with AML each year and the five-year survival rate is reported at 17% for adult patients. 2,3 Of all newly diagnosed cases of AML, approximately 25% carry the FLT3-ITD gene mutation, which is associated with a particularly unfavorable prognosis including increased risk of relapse and shorter overall survival.4 “There is a need to improve survival for the majority of patients with acute myeloid leukemia, particularly those with the FLT3-ITD subtype, which is aggressive and difficult to treat,” said Ken Takeshita, MD, Global Head, R&D, Daiichi Sankyo. “We look forward to working with the EMA to support their review of quizartinib as a potential option for patients with newly diagnosed FLT3-ITD positive acute myeloid leukemia.” Validation confirms that the application is complete and commences the scientific review process by the EMA’s Committee for Medicinal Products for Human Use (CHMP). The application is based on data from the QuANTUM-First phase 3 trial recently presented at the European Hematology Association (#EHA2022) Congress. In QuANTUM-First, quizartinib combined with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and continued as monotherapy following consolidation, demonstrated a statistically significant and clinically meaningful improvement in overall survival (OS) in adult patients with newly diagnosed FLT3-ITD positive AML 2 compared to chemotherapy alone. The safety of quizartinib combined with intensive chemotherapy and as continuation monotherapy in QuANTUM-First was generally manageable and consistent with previous clinical trials. The incidence of Grade ≥3 QT prolongation was low, with uncommon ventricular arrythmia events. Overall, the risk of QT prolongation was manageable with ECG monitoring, quizartinib dose modification and correction/elimination of additional risk factors. About QuANTUM-First QuANTUM-First is a randomized, double-blind, placebo-controlled global phase 3 study evaluating quizartinib in combination with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and as continuation monotherapy following consolidation, in adult patients aged 18-75 with newly diagnosed FLT3-ITD positive AML. Patients were randomized 1:1 into two treatment groups to receive quizartinib or placebo combined with anthracycline- and cytarabine-based regimens. Eligible patients, including those who underwent hematopoietic stem cell transplant (HSCT), continued with quizartinib or placebo for up to 36 cycles. The primary study endpoint was OS. Secondary endpoints include event-free survival (EFS), postinduction rates of complete remission (CR) and composite complete remission (CRc), and the percentage of patients who achieve CR or CRc with FLT3-ITD minimal residual disease negativity. Safety and pharmacokinetics, along with exploratory efficacy and biomarker endpoints, also were evaluated. QuANTUM-First enrolled 539 patients at 193 study sites across Asia, Europe, North America, Oceania and South America. For more information, visit Clinicaltrialsregister.eu or ClinicalTrials.gov.
About FLT3-ITD FLT3 (FMS-like tyrosine kinase 3) is a tyrosine kinase receptor protein normally expressed by hematopoietic stem cells that plays an important role in cell development, promoting cell survival, growth and differentiation through various signaling pathways. 4 Mutations of the FLT3 gene, which occur in approximately 30% of AML patients, can drive oncogenic signaling.4 FLT3-ITD (internal tandem 3 duplication) is the most common type of FLT3 mutation in AML, occurring in about 25% of all newly diagnosed patients, and is associated with increased risk of relapse and shorter overall survival.4 About Quizartinib Quizartinib is an oral, selective type II FLT3 inhibitor currently in clinical development for treatment of FLT3-ITD positive AML. In addition to QuANTUM-First, the quizartinib development program includes a phase 1/2 trial in pediatric and young adult patients with relapsed/ refractory FLT3-ITD positive AML in Europe and North America. Several phase 1/2 combination studies with quizartinib are also underway at The University of Texas MD Anderson Cancer Center as part of a strategic research collaboration focused on accelerating development of Daiichi Sankyo pipeline therapies for AML. Quizartinib, which is currently not approved in Europe, has been granted Orphan Drug Designation for the treatment of AML in Europe, Japan and the U.S. Quizartinib has received Fast Track Designation from the U.S. Food and Drug Administration for the treatment of adult patients with newly diagnosed AML that is FLT3-ITD positive, in combination with standard cytarabine and anthracycline induction and cytarabine consolidation chemotherapy. Quizartinib is currently approved for use in Japan for the treatment of adult patients with relapsed/refractory FLT3-ITD AML, as detected by an approved test. Quizartinib is an investigational medicine in all countries outside of Japan. About Daiichi Sankyo Daiichi Sankyo is dedicated to creating new modalities and innovative medicines by leveraging our world-class science and technology for our purpose “to contribute to the enrichment of quality of life around the world.” In addition to our current portfolio of medicines for cancer and cardiovascular disease, Daiichi Sankyo is primarily focused on developing novel therapies for people with cancer as well as other diseases with high unmet medical needs. With more than 100 years of scientific expertise and a presence in more than 20 countries, Daiichi Sankyo and its 16,000 employees around the world draw upon a rich legacy of innovation to realize our 2030 Vision to become an “Innovative Global Healthcare Company Contributing to the Sustainable Development of Society.” For more information, please visit www.daiichisankyo.com.
Daiichi Sankyo's quizartinib gets EMA review to treat blood cancer subtype
Aug. 23, 2022 4:48 AM ET
Daiichi Sankyo Company, Limited (DSNKY), DSKYF
By: Ravikash, SA News Editor
- The European Medicines Agency (EMA) validated Daiichi Sankyo's (OTCPK:DSKYF) (OTCPK:DSNKY) application seeking approval of quizartinib in combination with standard cytarabine and anthracycline induction and standard cytarabine consolidation chemotherapy, and as continuation standalone therapy after consolidation, to treat adult patients with newly diagnosed acute myeloid leukemia (AML) which is FMS-like tyrosine kinase 3 internal tandem duplication (FLT3-ITD) positive.
- https://seekingalpha.com/news/3875634-daiichi-sankyos-quizartinib-gets-ema-review-to-treat-blood-cancer-subtype
- https://seekingalpha.com/symbol/DSKYF
- https://seekingalpha.com/symbol/DSNKY
- https://www.daiichisankyo.com/
CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide)
CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide)
CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide)
07:49
22 August 2022
Novo Nordisk successfully completes phase 2 trial with CagriSema in people with type 2 diabetes
Bagsværd, Denmark ,
2 2 August 2022 – Novo Nordisk today announced headline results from a phase 2 clinical trial with CagriSema, a once-weekly subcutaneous combination of semaglutide and a novel amylin analogue, cagrilintide.
The trial investigated the efficacy and safety of a fixed dose combination of CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide) compared to the individual components semaglutide 2.4 mg and cagrilintide 2.4 mg, all administered once weekly, in 92 people with type 2 diabetes and overweight. People were equally randomised among the three treatment arms. In the trial, the mean baseline HbA1c was 8.4% and the mean baseline body weight was 106 kg.
After 32 weeks of treatment, people treated with CagriSema achieved a numerically higher HbA1c reduction of 2.18%-points compared to a reduction of 1.79%-points for people treated with semaglutide and 0.93%-points with cagrilintide alone. People treated with CagriSema achieved a numerically higher body weight reduction of 15.6% compared to a reduction of 5.1% for people treated with semaglutide and 8.1% with cagrilintide alone1. In the trial, CagriSema appeared to have a safe and well-tolerated profile.
“We are encouraged by the impressive phase 2 results for CagriSema in people with type 2 diabetes,” said Martin Holst Lange, executive vice president for Development at Novo Nordisk. “The results indicate that CagriSema reduces blood sugar more than semaglutide alone and the weight loss seen in the trial confirms the substantial weight lowering potential of CagriSema”.
Based on the results, Novo Nordisk is now planning to initiate a phase 3 development programme for CagriSema in people with type 2 diabetes in 2023. The CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide) phase 3 programme in people with overweight and obesity, REDEFINE, is expected to begin in the fourth quarter of 2022.
About Novo Nordisk
Novo Nordisk is a leading global healthcare company, founded in 1923 and headquartered in Denmark. Our purpose is to drive change to defeat diabetes and other serious chronic diseases such as obesity and rare blood and endocrine disorders. We do so by pioneering scientific breakthroughs, expanding access to our medicines and working to prevent and ultimately cure disease. Novo Nordisk employs about 50 , 8 00 people in 80 countries and markets its products in around 170 countries. Novo Nordisk's B shares are listed on Nasdaq Copenhagen (Novo-B). Its ADRs are listed on the New York Stock Exchange (NVO) . For more information, visit novonordisk.com , Facebook, Twitter , LinkedIn and YouTube.
Novo Nordisk CagriSema helps reduce blood sugar, weight in diabetics/overweight in phase 2 trial
Aug. 23, 2022 5:32 AM ET
By: Ravikash, SA News Editor
Novo Nordisk (NVO) said its medicine CagriSema was better at reducing blood sugar levels and weight compared to its other diabetes drug semaglutide and a novel amylin analogue, cagrilintide, in a phase 2 trial in people with type 2 diabetes and overweight.
https://seekingalpha.com/symbol/NVO
ZYNTEGLO® (betibeglogene autotemcel) or beti-cel
CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide)
ZYNTEGLO® (betibeglogene autotemcel) or beti-cel
bluebird bio Announces FDA Approval of ZYNTEGLO®, the First Gene Therapy for People with Beta-Thalassemia Who Require Regular Red Blood Cell Transfusions
ZYNTEGLO offers potentially curative benefit across ages and genotypes, through the achievement of durable transfusion independence and normal or near normal total hemoglobin levels
Management team to host conference call Thursday, August 18 at 8:00 am ET
SOMERVILLE, Mass.--(BUSINESS WIRE)--Aug. 17, 2022-- bluebird bio, Inc. (Nasdaq: BLUE) today announced the U.S. Food and Drug Administration (FDA) has approved ZYNTEGLO® (betibeglogene autotemcel), also known as beti-cel, a one-time gene therapy custom-designed to treat the underlying genetic cause of beta‑thalassemia in adult and pediatric patients who require regular red blood cell (RBC) transfusions.
“The FDA approval of ZYNTEGLO offers people with beta-thalassemia the possibility of freedom from burdensome regular red blood cell transfusions and iron chelation, and unlocks new possibilities in their daily lives,” said Andrew Obenshain, chief executive officer, bluebird bio. “After more than a decade of research and clinical development, and through the perseverance of clinicians, patients, and their families, the approval of ZYNTEGLO marks a watershed moment for the field of gene therapy. As the first ex-vivo lentiviral vector gene therapy approved in the U.S. for the treatment of people with beta-thalassemia, we are ushering in a new era in which gene therapy has the potential to transform existing treatment paradigms for diseases that currently carry a lifelong burden of care.”
Beta-thalassemia is a rare, genetic blood disease caused by mutations in the beta-globin gene and characterized by significantly reduced or absent adult hemoglobin production. Patients with the most severe form, sometimes called transfusion-dependent beta-thalassemia or beta-thalassemia major, experience severe anemia and lifelong dependence on regular red blood cell transfusions, a lengthy process that patients typically undergo every 2-5 weeks. Despite advances in treatment and improved transfusion techniques, transfusions only temporarily address symptoms of anemia and people with beta‑thalassemia who require regular transfusions have an increased risk for morbidity and mortality due to complications from treatment-related iron overload. Data from the Cooley’s Anemia Foundation indicate that the median age of death of patients with transfusion-dependent beta‑thalassemia in the U.S. who died during the last decade was just 37 years. bluebird estimates that there are approximately 1,300-1,500 individuals with transfusion-dependent beta-thalassemia in the U.S.
“Transfusion-dependent beta-thalassemia is associated with an intense treatment burden and significant health risks related to regular red blood transfusions and iron management,” said Alexis A. Thompson, MD, MPH, Chief of the Division of Hematology, Children's Hospital of Philadelphia. “As a clinician and an investigator in the ZYNTEGLO clinical development program, I celebrate the therapeutic potential of this treatment for patients and its implications for the field of gene therapy, all made possible through the incredible courage of patients and families who participated in the clinical trials.”
“The Cooley’s Anemia Foundation applauds the FDA’s approval of ZYNTEGLO for people with beta‑thalassemia who require regular red blood cell transfusions. The availability of a one-time gene therapy which offers the possibility of transfusion independence opens up new and exciting opportunities for those who are medically eligible to receive this treatment option,” said Craig Butler, National Executive Director, Cooley’s Anemia Foundation. “While advances in treatment have been of enormous benefit to those with beta-thalassemia, a potentially curative therapy may offer a true life-changing experience.”
The approval of ZYNTEGLO is the culmination of nearly 10 years of clinical research of gene therapy in patients with transfusion-dependent beta-thalassemia. ZYNTEGLO works by adding functional copies of a modified form of the beta-globin gene (βA-T87Q-globin gene) into a patient’s own hematopoietic (blood) stem cells (HSCs) to allow them to make normal to near normal levels of total hemoglobin without regular RBC transfusions. The functional beta-globin gene is added into a patient’s cells outside of the body (ex-vivo), and then infused into the patient. Though ZYNTEGLO is designed to be administered to the patient once, the treatment process is comprised of several steps that may take place over the course of several months.
Due to the complex nature of gene therapy, ZYNTEGLO will be available exclusively at Qualified Treatment Centers (QTCs) which are carefully selected based on their expertise in relevant areas such as stem cell transplantation, cell and gene therapy, and beta-thalassemia; and receive specialized training to administer ZYNTEGLO. Information on bluebird’s QTC network, as well as personalized support focused on the needs of each patient throughout their treatment journey and information on insurance coverage and access will be available through bluebird’s patient support program, my bluebird support. Patients can call 833-888-NEST (833-888-6378) for more information, and additional details will be available at mybluebirdsupport.com in the coming days.
ZYNTEGLO was reviewed under Priority Review, and the Company received a Priority Review voucher upon approval. ZYNTEGLO was previously granted Orphan Drug designation and Breakthrough Therapy designation.
Clinical Data Supporting Approval of ZYNTEGLO
bluebird bio has the longest and most robust clinical program in transfusion-dependent beta‑thalassemia (TDT) in the field of gene therapy. The approval of ZYNTEGLO is based on data from bluebird bio’s Phase 3 studies HGB-207 (Northstar-2) and HGB-212 (Northstar-3), and the long-term follow-up study LTF-303.
The single-arm, open-label, 24-month Phase 3 studies of ZYNTEGLO included 41 patients aged 4 to 34 years with both non-β0/β0 and β0/β0 genotypes, with longest follow up out to 4 years. Eighty-nine percent (32/36) of evaluable patients across ages and genotypes achieved transfusion independence (TI), which is defined as no longer needing red blood cell transfusions for at least 12 months while maintaining a weighted average total hemoglobin of at least 9 g/dL. Results in these patients were durable as of last follow-up.
The most common non-laboratory adverse reactions (≥20%) were mucositis, febrile neutropenia, vomiting, pyrexia, alopecia, epistaxis, abdominal pain, musculoskeletal pain, cough, headache, diarrhea, rash, constipation, nausea, decreased appetite, pigmentation disorder, and pruritus. The most common Grade 3 or 4 laboratory abnormalities (>50%) include neutropenia, thrombocytopenia, leukopenia, anemia, and lymphopenia.
Enrollment is complete and all patients have been treated in the Phase 3 Northstar-2 (HGB-207) and Northstar-3 (HGB-212) studies evaluating ZYNTEGLO. Follow-up in HGB-212 is ongoing. bluebird bio is also conducting a long-term follow-up study, LTF-303, to monitor safety and efficacy for patients with TDT who have participated in bluebird bio-sponsored clinical studies of lentiviral vector (LVV) gene therapy through 15 years post-treatment.
Across all studies, all patients who achieved transfusion independence have remained transfusion-free.
About ZYNTEGLO® (betibeglogene autotemcel) or beti-cel
ZYNTEGLO is a first-in-class, one-time ex-vivo LVV gene therapy approved for the treatment of beta-thalassemia in adult and pediatric patients who require regular red blood cell (RBC) transfusions. ZYNTEGLO works by adding functional copies of a modified form of the beta-globin gene (βA-T87Q-globin gene) into a patient’s own hematopoietic (blood) stem cells to enable the production of a modified functional adult hemoglobin (HbAT87Q). Once a patient has the βA-T87Q-globin gene, they have the potential to increase ZYNTEGLO-derived adult hemoglobin (HbAT87Q) and total hemoglobin to normal or near normal levels that can eliminate the need for regular RBC transfusions.
Indication
ZYNTEGLO is indicated for the treatment of adult and pediatric patients with beta-thalassemia who require regular red blood cell (RBC) transfusions.
Please see full Prescribing Information for ZYNTEGLO.
About bluebird bio, Inc.
bluebird bio is pursuing curative gene therapies to give patients and their families more bluebird days. With a dedicated focus on severe genetic diseases, bluebird has industry-leading clinical and research programs for sickle cell disease, beta-thalassemia and cerebral adrenoleukodystrophy and is advancing research to apply new technologies to these and other diseases. We custom design each of our therapies to address the underlying cause of disease and have developed in-depth and effective analytical methods to understand the safety of our lentiviral vector technologies and drive the field of gene therapy forward.
Founded in 2010, bluebird has the largest and deepest ex-vivo gene therapy data set in the world—setting the standard for industry. Today, bluebird continues to forge new paths, combining our real‑world experience with a deep commitment to patient communities and a people-centric culture that attracts and grows a diverse flock of dedicated birds.
For more information, visit bluebirdbio.com or follow us on social media at @bluebirdbio, LinkedIn, Instagram and YouTube.
ZYNTEGLO and bluebird bio are trademarks of bluebird bio, Inc.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220817005667/en/
Source: bluebird bio, Inc.
FDA approves bluebird bio's Zynteglo gene therapy for beta thalassemia; shares up 7%
Aug. 17, 2022 1:57 PM ET
By: Jonathan Block, SA News Editor3 Comments
Note: This article has been updated with bluebird bio share movement and the company's reimbursement program with payers.
- The U.S. FDA has approved bluebird bio's (NASDAQ:BLUE) Zynteglo (betibeglogene autotemcel), a gene therapy for the treatment of the blood disorder β-thalassemia.
- https://seekingalpha.com/news/3874245-fda-approves-bluebird-bio-zynteglo-beti-cel-gene-therapy-beta-thalassemia
- https://seekingalpha.com/symbol/BLUE
- https://www.bluebirdbio.com/
- https://www.bluebirdbio.com/our-science/pipeline
INBRX-109
CagriSema (2.4 mg semaglutide and 2.4 mg cagrilintide)
ZYNTEGLO® (betibeglogene autotemcel) or beti-cel
European Medicines Agency Grants Orphan Drug Designation to INBRX-109 for the Treatment of Chondrosarcoma
SAN DIEGO, Aug. 15, 2022 /PRNewswire/ --
Inhibrx, Inc. (Nasdaq: INBX), a biotechnology company with four clinical programs in development and a strong emerging pipeline, today announced that the European Commission ("EC"), based on a positive opinion issued by the European Medicines Agency ("EMA"), has granted orphan medicinal product designation to INBRX-109 for the treatment of chondrosarcoma.
"We are highly optimistic about the potential of INBRX-109 in chondrosarcoma to address a high unmet medical need," said Inhibrx Chief Executive Officer, Mark Lappe. "The positive opinion issued by the EMA is excellent news and acknowledges the potential of INBRX-109 as a treatment for patients throughout Europe who suffer from this debilitating, rare condition."
The EC grants orphan designation to drugs and biologics intended for the safe and effective treatment, prevention, or diagnosis of a disease that is life-threatening or chronically debilitating impacting fewer than five in 10,000 patients in the European Union ("EU"). Orphan drug designation in the EU can provide certain benefits, including reduced regulatory fees, clinical protocol assistance and the potential for up to ten years of market exclusivity following regulatory approval.
About INBRX-109
INBRX-109 is a precision-engineered, tetravalent death receptor 5 (DR5) agonist antibody designed to exploit the tumor-biased cell death induced by DR5 activation.
In 2021, the FDA granted Fast Track designation to INBRX-109 for the treatment of patients with unresectable or metastatic conventional chondrosarcoma and orphan-drug designation to INBRX-109 for chondrosarcoma in the United States.
In June 2021, Inhibrx initiated a randomized, blinded, placebo-controlled, potential registration-enabling Phase 2 trial of INBRX-109 in conventional chondrosarcoma, which is currently ongoing.
In November 2021, Inhibrx provided updated results from its ongoing Phase 1 clinical trial evaluating the efficacy and safety of INBRX-109 in patients with conventional chondrosarcoma. Preliminary disease control was observed in 16 of the 18 evaluable patients (89%) measured by RECISTv1.1, with two of the 18 achieving partial responses (11%). Based on preliminary results of the ongoing Phase 1 trial at that time, the median progression-free survival (PFS) was 7.4 months, and the median overall survival had not been reached. Three patients had exceeded 61 weeks on treatment with INBRX-109, with 77 weeks being the longest duration of stable disease observed at that time.
About Inhibrx, Inc.
Inhibrx is a clinical-stage biotechnology company focused on developing a broad pipeline of novel biologic therapeutic candidates in oncology and orphan diseases. Inhibrx utilizes diverse methods of protein engineering to address the specific requirements of complex target and disease biology, including its proprietary sdAb platform. Inhibrx has collaborations with 2seventy bio (formerly bluebird bio), Bristol-Myers Squibb and Chiesi. For more information, please visit www.inhibrx.com.
SOURCE Inhibrx Inc.
Europe drug regulator grants orphan designation to Inhibrx's drug for type of bone cancer
Aug. 15, 2022 4:38 PM ET
By: Anuron Mitra, SA News Editor
- Inhibrx (NASDAQ:INBX) on Monday said the European Commission had granted an orphan drug designation to the biotech's antibody INBRX-109 for the treatment of chondrosarcoma, a type of bonce cancer.
- https://seekingalpha.com/news/3873205-europe-drug-regulator-grants-orphan-designation-to-inhibrxs-drug-for-type-of-bone-cancer
- https://inhibrx.com/inbrx-109/
- https://seekingalpha.com/symbol/INBX
- https://inhibrx.com/
biotecHOPE™ 2022
Picankibart (IBI112)
KarXT (xanomeline-trospium)
Picankibart (IBI112)
Innovent Announces Phase 2 Clinical Study of Picankibart (IBI112) in Chinese Patients with Moderate-to-severe Plaque Psoriasis Met Primary Endpoint
Published on: Aug 10th, 2022
SAN FRANCISCO, US and SUZHOU, China, Aug 10, 2022 — Innovent Biologics, Inc. (“Innovent”) (HKEX: 01801), a world-class biopharmaceutical company that develops, manufactures and commercializes high-quality medicines for the treatment of oncology, autoimmune, metabolic, ophthalmology and other major diseases, announces that the primary endpoint was met in a multicenter, randomized, double-blind, placebo-controlled phase 2 study (clinicaltrials.gov, NCT 05003531) of picankibart (R&D code: IBI112), a recombinant anti-interleukin 23p19 subunit antibody injection, in Chinese patients with moderate-to-severe plaque psoriasis. This study (CIBI112A201) was designed to evaluate the efficacy and safety of picankibart under various administration in the treatment of moderate-to-severe plaque psoriasis. A total of 250 subjects were randomized 1:1:1:1:1 to receive 50 mg (once at week 0, 4, then every 12 weeks), 100mg (once at week 0, 4, then every 12 weeks), 100mg (once at week 0, 4, then every 8 weeks), 200mg (once at week 0, 4, then every 12 weeks) of picankibart or placebo. The primary endpoint of the study was the proportion of subjects who achieved a ≥90% improvement in the Psoriasis Area and Severity Index (PASI) at week 16 (PASI 90) and the total study period is 52 weeks. To date, a total of 245 subjects (98.0%) have completed the primary endpoint at week 16, and a total of 236 subjects (94.4%) have completed the visit at week 28.
- In terms of efficacy, 52.0%~54.9% of the subjects achieved PASI 90 after picankibart treatment at week 16, which was significantly higher than that in the placebo group and reached the primary endpoint, in addition, the proportions of subjects who achieved PASI 75 and PASI 100 were also significantly higher than that in the placebo group (all P-values<0.001). The study results through 28 weeks showed a long-term efficacy of picankibart, with 61.2%~72.5% of the subjects who received picankibart achieving PASI 90, 78.4%~88.0% of the subjects achieved PASI 75, and in one of the groups received picankibart, about 40.0 % of subjects achieved complete skin lesions clearance (PASI 100).
- In terms of safety, picankibart is generally well tolerated, and no new safety signals occurred compared with previous clinical studies. The overall safety profile is similar to other IL-23p19 mAbs. The most frequently reported (incidence ≥10%) treatment-emergent adverse events were upper respiratory tract infection with mild to moderate severity.
- In addition, we observed a significant increase from baseline in the Dermatology Life Quality Index (DLQI) of subjects treated with each dose of picankibart compared to placebo (all P-values<0.0001).
Clinical study results showed that 50-200mg picankibart administered every 12 or 8 weeks significantly improved the skin lesions and quality of life of subjects with moderate to severe plaque psoriasis, demonstrating the significant improvement effect at long-dose interval. It is worth noting that, at the 16-week primary endpoint assessment, subjects received only two administrations, significantly less than other similar biologics. Moreover, continued improvement in efficacy across the picankibart treatment was observed after reaching the primary endpoint (up to 28 weeks), demonstrating the potential sustained advantage of long interval dosing. The study period is 52 weeks (one year), and currently, subjects in the placebo group have been treated with IBI112, and the dosing and follow-up of the study are ongoing. Full data on the study will be published at future academic conferences or peer-reviewed journals. Professor Jianzhong Zhang of Peking University People’s Hospital, the principal investigator of the study, stated, “Psoriasis is a life-long disease, which has a huge impact on the physical and mental health and quality of life, while the current traditional treatment is not ideal. We are pleased to find significant clinical benefit and improved quality of life in subjects with moderate to severe plaque psoriasis in the phase 2 clinical study of picankibart. Meanwhile, picankibart also shows potential advantages in long dosing intervals and long-term efficacy. I am confident and looking forward to the success of its upcoming phase 3 study, and hope it will provide an alternative treatment option for Chinese psoriasis patients.” Dr. Lei Qian , Vice President of Clinical Development of Innovent, stated: “We are happy that phase 2 study of picankibart in Chinese patients with moderate-to-severe plaque psoriasis achieved primary clinical endpoint. As a new generation of IL-23p19 target drug, picankibart shows clear advantages in the long-dose interval and long-term efficacy. The dosing frequency is only 5 times annually, and it shows a great potential for both efficacy and safety, and could be offered as a more friendly treatment option compared to the current ones on the market whose dosing frequency is 7-16 times annually. Currently, there is no IL-23p19 target drug independently developed by Chinese pharmaceutical companies in the domestic market. We are greatly encouraged by the results of good efficacy, safety and tolerability of picankibart in the phase 2 clinical study. Based on this, we are confident and will actively advance the phase 3 clinical study of picankibart in patients with moderate to severe plaque psoriasis, and we plan to optimize the dosing regimen scientifically based on quantitative pharmacology to further improve efficacy, and synchronize the use of auto-injector in the phase 3 clinical study. We are striving to provide more convenient, user-friendly and effective treatment options for patients with moderate to severe plaque psoriasis as soon as possible and to fulfill our mission of providing high-quality innovative biopharmaceutical products that are accessible to patients.” About Picankibart (IBI112)Picankibart (IBI112) is a monoclonal antibody independently developed by Innovent, with independent intellectual property rights. This product specifically binds to IL-23p19 subunit, thereby preventing IL-23 from binding to cell surface receptors, resulting in the inhibition of the IL-23 receptor-mediated signaling pathway. Preclinical data demonstrated that IBI112 has a clear target and well-elucidated mechanism of action and significant anti-inflammatory effect. Further, good safety and tolerability have been verified in the phase 1 clinical study. At present, the phase 2 clinical studies of IBI112 in the indications of moderate to severe plaque psoriasis and ulcerative colitis are ongoing, and the primary clinical study endpoint has been met in the phase 2 clinical study of psoriasis, suggesting that it may provide a more effective treatment option for patients with psoriasis or other autoimmune diseases.
About Innovent
Inspired by the spirit of "Start with Integrity, Succeed through Action,” Innovent’s mission is to develop, manufacture and commercialize high-quality biopharmaceutical products that are affordable to ordinary people. Established in 2011, Innovent is committed to developing, manufacturing and commercializing high-quality innovative medicines for the treatment of oncology, autoimmune, metabolic, ophthalmology and other major diseases. On October 31, 2018, Innovent was listed on the Main Board of the Stock Exchange of Hong Kong Limited with the stock code: 01801. HK.
Since its inception, Innovent has developed a fully integrated multi-functional platform that includes R&D, CMC (Chemistry, Manufacturing, and Controls), clinical development and commercialization capabilities. Leveraging the platform, the company has built a robust pipeline of 34 valuable assets in the fields of cancer, autoimmune, metabolic, ophthalmology and other major therapeutic areas, among them, 7 varieties were selected for the national "Major New Drug Creation" special project, 7 products approved for marketing in China – TYVYT® (sintilimab injection), BYVASDA® (bevacizumab biosimilar injection), SULINNO® (adalimumab biosimilar injection), HALPRYZA® (rituximab biosimilar injection), Pemazyre® (pemigatinib oral inhibitor) and olverembatinib (BCR-ABL TKI) and Cyramza® (ramucirumab), 3 asset under NMPA NDA review, 4 assets in Phase 3 or pivotal clinical trials, and an additional 20 molecules in clinical studies.
Innovent has built an international team with advanced talent in high-end biological drug development and commercialization, including many global experts. The company has also entered into strategic collaborations with Eli Lilly and Company, Sanofi, Adimab, Incyte, MD Anderson Cancer Center, and other international partners. Innovent strives to work with many collaborators to help advance China’s biopharmaceutical industry, improve drug availability and enhance the quality of the patients’ lives. For more information, please visit: www.innoventbio.com.
Note:
TYVYT® (Sintilimab Injection) is not an approved product in the United States.
BYVASDA® (bevacizumab biosimilar injection), HALPRYZA® (rituximab biosimilar injection), and SULINNO® (adalimumab biosimilar injection) are not approved products in the United States.
TYVYT® (sintilimab injection, Innovent)
BYVASDA® (bevacizumab biosimilar injection, Innovent)
HALPRYZA® (rituximab biosimilar injection, Innovent)
SULINNO® (adalimumab biosimilar injection, Innovent)
Pemazyre® (pemigatinib oral inhibitor, Incyte Corporation). Pemazyre® was discovered by Incyte Corporation and licensed to Innovent for development and commercialization in Mainland China, Hong Kong, Macau and Taiwan.
CYRAMZA® (ramucirumab, Eli Lilly). Cyramza® was discovered by Eli Lilly and licensed to Innovent for commercialization in Mainland China.
Innovent psoriasis drug reduces disease severity, meets main goal in mid-stage study
Aug. 10, 2022 6:01 AM ET
Innovent Biologics, Inc. (IVBIY)
By: Ravikash, SA News Editor
Innovent Biologics (OTCPK:IVBIY) medicine picankibart helped reduce the severity of disease in Chinese patients with moderate-to-severe plaque psoriasis, meeting the main goal of a phase 2 trial.
https://seekingalpha.com/symbol/IVBIY
GFH009
KarXT (xanomeline-trospium)
Picankibart (IBI112)
SELLAS Life Sciences’ GFH009 Demonstrates Cancer Cell Growth Inhibition in Preclinical In Vitro Studies in Solid Cancer and Acute Myeloid Leukemia Cell Lines
PDF Format (opens in new window) (PDF)
- Results Demonstrate Significant Anti-Tumor Effects on All Selected Cell Lines -
- In Three of the Four Cell Lines, GFH009 Inhibited Cancer Growth by 90 to 100 Percent -
NEW YORK, Aug. 09, 2022 (GLOBE NEWSWIRE) --
SELLAS Life Sciences Group, Inc. (NASDAQ: SLS) (“SELLAS" or the “Company”), a late-stage clinical biopharmaceutical company focused on the development of novel therapies for a broad range of cancer indications, today announced results from preclinical in vitro studies for its highly selective CDK9 inhibitor, GFH009, in solid cancer and acute myeloid leukemia (AML) cell lines. The data shows that GFH009 demonstrated significant anti-tumor effects in all four selected cell lines. In three out of the four cell lines, GFH009 inhibited cancer cell growth by 90 to 100 percent.
The in vitro studies were conducted at an independent, third-party contract research organization, Translational Drug Development (TD2), and the following cell lines were selected for the studies based on their unique characteristics, combined with GFH009’s mechanism of action:
- RH30: a pediatric soft tissue sarcoma cell line that is a model for studying high-risk pediatric rhabdomyosarcoma, an indication for which currently available treatments are limited to high-dose chemotherapy with unsatisfactory results. RH30 cells are driven by PAX3-FOXO1, a transcription factor whose expression is strictly needed for tumor cell survival. RH30 is also dependent on MYCN, a major target of CDK9 inhibition. Treatment with GFH009 resulted in 90 percent or more cancer inhibition at dose levels equivalent to those already demonstrated to be safe in patients in the ongoing Phase 1 trial with no viable cancer cells at the highest dose levels.
- NCI-H209: a small cell lung cancer cell line characterized by the loss of function of two major tumor suppressor genes, RB1 and TP53. This cell line also expresses MCL-1, a major target of CDK9 inhibition. Treatment with GFH009 resulted in 90 percent or more cancer inhibition at dose levels equivalent to those already demonstrated to be safe in patients in the ongoing Phase 1 trial with no viable cancer cells at highest dose levels.
- SKOV-3: an ovarian cancer cell line containing the wild type BRCA1 gene and highly expresses CDK9. Treatment with GFH009 resulted in more than 50 percent cancer inhibition at dose levels equivalent to those already demonstrated to be safe in patients in the ongoing Phase 1 trial.
- OCI-AML-2: an AML cell line that develops resistance to the chemotherapy venetoclax on exposure. Treatment with GFH009 resulted in 90 to 100 percent cancer inhibition at dose levels equivalent to those already demonstrated to be safe in patients in the ongoing Phase 1 trial with no viable cancer cells at the highest dose levels.
“The data from preclinical studies that we are reporting today demonstrates that certain cancer cell lines, whose survival depends on specific changes in the cell, can be identified and treated with GFH009,” said Dragan Cicic, MD, Senior Vice President, Clinical Development, of SELLAS. “Through identifying specific genes in cancer cells, GFH009 has shown in these preclinical studies the ability to stop the transcription and expression from gene to protein, inhibiting cancer cell growth altogether. We will utilize this important information as we design our clinical development program for GFH009 in adult and pediatric tumor types.”
About Translational Drug Development (TD2)
TD2 is an oncology development organization that provides innovative services for oncology-focused companies. Using a dedicated team of professionals with broad experience and understanding in drug development, TD2 is uniquely positioned to support improved and accelerated development of medicines for life-threatening oncology diseases. TD2 applies rigorous and high-throughput translational preclinical development, combined with regulatory affairs expertise, to customize clinical trial design and execution. TD2’s suite of capabilities encourages the timely selection of patient populations who are most likely to benefit from a new agent, and the rapid identification of clinically significant endpoints. TD2 is committed to reducing the risks and uncertainty inherent in the drug development process and to the acceleration of patient access to promising treatments. For more information, visit www.TD2inc.com.
About SELLAS Life Sciences Group, Inc.
SELLAS Life Sciences Group, Inc. (NASDAQ: SLS) is a late-stage clinical biopharmaceutical company focused on the development of novel therapeutics for a broad range of cancer indications. SELLAS’ lead product candidate, galinpepimut-S (GPS), is licensed from Memorial Sloan Kettering Cancer Center and targets the WT1 protein, which is present in an array of tumor types. GPS has potential as a monotherapy or in combination with other therapies to address a broad spectrum of hematologic malignancies and solid tumor indications. The Company is also developing GFH009, a small molecule, highly selective CDK9 inhibitor, which is licensed from GenFleet Therapeutics (Shanghai), Inc., for all therapeutic and diagnostic uses in the world outside of Greater China.
For more information on SELLAS, please visit www.sellaslifesciences.com.
Source: SELLAS Life Sciences Group, Inc.
SELLAS Life Sciences rises 9% after cancer drug shows promising result in animal study
Aug. 09, 2022 9:33 AM ET
SELLAS Life Sciences Group, Inc. (SLS)
By: Dania Nadeem, SA News Editor
- SELLAS Life Sciences (NASDAQ:SLS) is trading 9.2% higher on Tuesday after the company announced results from preclinical studies for its CDK9 inhibitor, GFH009, to treat solid cancer and acute myeloid leukemia (AML) cell lines.
- https://seekingalpha.com/news/3869812-sellas-life-sciences-cancer-drug-shows-promising-result-in-animal-study
- https://seekingalpha.com/symbol/SLS
- https://www.sellaslifesciences.com/pipeline/sellas-pipeline/default.aspx
KarXT (xanomeline-trospium)
KarXT (xanomeline-trospium)
KarXT (xanomeline-trospium)
Karuna Therapeutics Announces Positive Results from Phase 3 EMERGENT-2 Trial of KarXT in Schizophrenia
Aug 8, 2022 at 6:30 AM EDT
Trial met primary endpoint, with KarXT demonstrating a statistically significant 9.6-point reduction in PANSS Total Score compared to placebo at Week 5 (p<0.0001)
Trial also met key secondary endpoints, demonstrating statistically significant reductions in positive and negative symptoms of schizophrenia, as measured by the PANSS positive, PANSS negative and PANSS negative Marder factor subscales
KarXT was generally well tolerated, with a side effect profile substantially consistent with prior trials of KarXT in schizophrenia
The Company plans to submit a New Drug Application (NDA) with the U.S. Food & Drug Administration (FDA) in mid-2023
Conference call and webcast to take place today at 8:00 a.m. ET
BOSTON--(BUSINESS WIRE)--Aug. 8, 2022-- Karuna Therapeutics, Inc. (NASDAQ: KRTX), a clinical-stage biopharmaceutical company driven to create and deliver transformative medicines for people living with psychiatric and neurological conditions, today announced positive topline results from its Phase 3 EMERGENT-2 trial evaluating the efficacy, safety, and tolerability of its lead investigational therapy, KarXT (xanomeline-trospium), in adults with schizophrenia. The trial met its primary endpoint, with KarXT demonstrating a statistically significant and clinically meaningful 9.6-point reduction in the Positive and Negative Syndrome Scale (PANSS) total score compared to placebo (-21.2 KarXT vs. -11.6 placebo, p<0.0001) at Week 5 (Cohen’s d effect size of 0.61). KarXT also demonstrated an early and sustained statistically significant reduction of symptoms, as assessed by PANSS total score, starting at Week 2 and maintained such reduction through all timepoints in the trial.
“We are thrilled that these topline results from the Phase 3 EMERGENT-2 trial confirm what was seen in our Phase 2 EMERGENT-1 trial and underscore the potential for KarXT, with its novel and unique mechanism of action, to redefine what successful treatment looks like for the 21 million people living with schizophrenia worldwide, and potentially usher in the first new class of medicine for these patients in more than 50 years,” said Steve Paul, M.D., chief executive officer, president and chairman of Karuna Therapeutics. “These results represent our second positive registrational trial. We look forward to continuing to gather long-term safety data to support our submission of a New Drug Application with the U.S. Food and Drug Administration for KarXT as a treatment for schizophrenia, which we expect to occur in mid-2023.”
KarXT also met key secondary endpoints in the Phase 3 EMERGENT-2 trial, demonstrating a statistically significant reduction in both positive symptoms (e.g., hallucinations or delusions) and negative symptoms (e.g., difficulty enjoying life or withdrawal from others) of schizophrenia as measured by the PANSS positive, PANSS negative and PANSS negative Marder factor subscales. Results at Week 5 include:
- 2.9-point reduction in the PANSS positive subscale with KarXT compared to placebo (-6.8 KarXT vs. -3.9 placebo, p<0.0001).
- 1.8-point reduction in the PANSS negative subscale with KarXT compared to placebo (-3.4 KarXT vs. -1.6 placebo, p=0.0055).
- 2.2-point reduction in the PANSS negative Marder factor subscale with KarXT compared to placebo (-4.2 KarXT vs. -2.0 placebo, p=0.0022).
KarXT was generally well tolerated. Overall discontinuation rates were similar between KarXT and placebo groups (25% vs. 21%). The overall treatment-emergent adverse events (TEAEs) rate for KarXT and placebo was 75% and 58%, respectively. Discontinuation rates related to TEAEs were similar between KarXT (7%) and placebo (6%). Equal rates of serious TEAEs were observed between KarXT and placebo (2% in each group) and included suicidal ideation, worsening of schizophrenia symptoms, and appendicitis. None of the serious TEAEs were determined to be drug related. The most common TEAEs (>5%) in the KarXT arm were all mild to moderate in severity and included constipation, dyspepsia, nausea, vomiting, headache, increases in blood pressure, dizziness, gastroesophageal reflux disease (acid reflux), abdominal discomfort, and diarrhea. Mean blood pressure measures were similar between KarXT and placebo throughout the trial, and no syncopal events were observed. In the subset of patients with a TEAE of blood pressure increases, mean blood pressure at endpoint was similar to baseline and did not lead to trial discontinuation. Similar to prior trials, an increase in heart rate was associated with KarXT treatment and decreased in magnitude by the end of the trial. Consistent with EMERGENT-1, KarXT was not associated with common problematic side effects of current treatments, including sedation (somnolence), weight gain, and extrapyramidal symptoms.
“Despite the number of available treatment options, there continues to be a tremendous unmet need in the treatment of schizophrenia, placing an immense burden on both patients and their caregivers,” said Rishi Kakar, M.D., chief scientific officer, Segal Trials and lead investigator of the Phase 3 EMERGENT-2 trial. “These data build on the growing body of clinical evidence supporting the potential of KarXT as a new and differentiated approach for schizophrenia, demonstrating notable improvements across both positive and negative symptoms, while not being associated with common problematic side-effects of current therapies, such as weight gain, sedation and movement disorders. This unique profile of KarXT has the potential to provide a new meaningful treatment option for our patients and their families beyond the current standard of care.”
The EMERGENT program consists of the completed positive Phase 2 EMERGENT-1 and Phase 3 EMERGENT-2 trials, as well as three ongoing trials evaluating the acute efficacy and long-term safety of KarXT (EMERGENT-3, EMERGENT-4, and EMERGENT-5). Topline data from the Phase 3 EMERGENT-3 trial are expected in the first quarter of 2023. The data from our EMERGENT program will be used to support submission of an NDA with the U.S. FDA for KarXT as a treatment for schizophrenia, which is expected in mid-2023. Additional analysis of data from the Phase 3 EMERGENT-2 trial is ongoing, with plans to present these results at future medical meetings.
About the Phase 3 EMERGENT-2 Trial
The Phase 3 EMERGENT-2 trial is a double-blind, placebo-controlled, five-week, inpatient trial evaluating the efficacy, safety, and tolerability of our lead investigational therapy, KarXT, as compared to placebo in adults with schizophrenia in the United States. The primary endpoint was change from baseline in Positive and Negative Syndrome Scale (PANSS) total score, a scale for measuring schizophrenia symptom severity, of KarXT compared to placebo at Week 5. Key secondary endpoints included change from baseline in PANSS positive, PANSS negative and PANSS negative Marder factor subscale of KarXT compared to placebo at Week 5.
A total of 252 adults (between the ages of 18-65 years) with a confirmed diagnosis of schizophrenia who were experiencing symptoms of psychosis enrolled in the trial. Patients were randomized 1:1 to receive either a flexible dose of KarXT (n=126) or placebo (n=126) two times a day (BID) for five weeks. On Days 1-2, patients received a dose of 50/20 KarXT (50mg xanomeline/20mg trospium) BID or matching placebo. On Day 3, patients escalated to a dose of 100/20 BID, and starting on Day 8, patients could increase to 125/30 BID based on tolerability. In the trial, 81% of patients on KarXT compared to 90% on placebo titrated to the highest dose level (125/30).
About KarXT
KarXT (xanomeline-trospium) is an oral, investigational M1/M4-preferring muscarinic agonist in development for the treatment of psychiatric and neurological conditions, including schizophrenia and psychosis in Alzheimer’s disease. Comprised of muscarinic agonist xanomeline and muscarinic antagonist trospium, it is designed to preferentially stimulate muscarinic receptors in the central nervous system. KarXT is the first potential medicine of its kind with a truly new and unique dual mechanism that does not rely on the dopaminergic or serotonergic pathway to treat symptoms of serious mental illness. This approach has the potential to provide a differentiated therapy, and, if approved, to beneficially impact the lives of millions of people with serious mental illness.
About Karuna Therapeutics
Karuna Therapeutics is a clinical-stage biopharmaceutical company driven to create and deliver transformative medicines for people living with psychiatric and neurological conditions. At Karuna, we understand there is a need for differentiated and more effective treatments that can help patients navigate the challenges presented by serious mental illness. Utilizing our extensive knowledge of neuroscience, we are harnessing the untapped potential of the brain in pursuit of novel pathways to develop medicines that make meaningful differences in peoples’ lives. For more information, please visit www.karunatx.com.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220808005222/en/
Source: Karuna Therapeutics, Inc.
Karuna Therapeutics jumps 52% as schizophrenia trial meets key goal
Aug. 08, 2022 8:29 AM ET
Karuna Therapeutics, Inc. (KRTX)ZLAB
By: Dulan Lokuwithana, SA News Editor3 Comments
The shares of Karuna Therapeutics (NASDAQ:KRTX) surged ~52% in the pre-market on Monday after the clinical-stage biotech announced that its late-stage trial for experimental schizophrenia therapy KarXT met the primary endpoint. The ADRs of Chinese biotech Zai Lab Limited (ZLAB), Karuna's (KRTX) partner for the program also added ~15% in reaction.
https://seekingalpha.com/news/3868667-krtx-stock-jumps-as-schizophrenia-trial-meets-key-goals
https://seekingalpha.com/symbol/KRTX
Fruquintinib
TPOXX® (Tecovirimat)
KarXT (xanomeline-trospium)
Announcements & Press Releases, Oncology / Immunology | 8 Aug 2022
HUTCHMED Announces that Fruquintinib Global Phase III FRESCO-2 Study Has Met Its Primary Endpoint in Metastatic Colorectal Cancer
— Trial met primary endpoint of overall survival and all secondary endpoints —
— Overall safety consistent with fruquintinib known profile —
— Plans for regulatory submissions underway in the U.S., Europe and Japan —
— Results to be submitted to an upcoming medical meeting —
Hong Kong, Shanghai & Florham Park, NJ — Monday, August 8, 2022: HUTCHMED (China) Limited (“HUTCHMED”) (Nasdaq/AIM: HCM, HKEX: 13) today announces that the pivotal global Phase 3 FRESCO-2 trial evaluating the investigational use of fruquintinib met its primary endpoint of overall survival (“OS”) in patients with advanced, refractory metastatic colorectal cancer (“CRC”).
The FRESCO-2 study was a multi-regional clinical trial conducted in the U.S., Europe, Japan and Australia that investigated fruquintinib plus best supportive care (“BSC”) vs placebo plus BSC in patients with metastatic CRC who had progressed on standard chemotherapy and relevant biologic agents and who had progressed on, or were intolerant to, TAS-102 and/or regorafenib. In addition to OS, a statistically-significant improvement in progression-free survival (“PFS”), a key secondary endpoint, was observed. The safety profile of fruquintinib in FRESCO-2 was consistent with previously reported studies. Full results will be submitted for presentation at an upcoming medical meeting.
HUTCHMED has been in communication with regulatory agencies globally regarding the FRESCO-2 trial design and conduct and will discuss these data with the agencies in the U.S., Europe and Japan with the intent to submit marketing authorization applications as soon as possible. The U.S. FDA granted Fast Track Designation for the development of fruquintinib for the treatment of patients with metastatic CRC in June 2020.
“We are very happy to see the positive outcomes of the FRESCO-2 study which offers a potential new treatment for patients with advanced metastatic colorectal cancer, where the unmet need is very high and patients have limited treatment options,” said Dr Marek Kania, Executive Vice President, Managing Director and Chief Medical Officer of HUTCHMED International. “Results from the global FRESCO-2 study supplement findings from the original FRESCO study that led to the marketing approval and commercialization of fruquintinib in China. We would like to thank the patients, their families, and the healthcare professionals who participated in this study and helped achieve this important milestone.”
Professor Cathy Eng, MD, FACP, FASCO, David H. Johnson Endowed Chair in Surgical and Medical Oncology and Co-Leader, Gastrointestinal Cancer Research Program, at the Vanderbilt-Ingram Cancer Center, who served as the FRESCO2 co-PI and Steering Committee member said: “Completion of the international FRESCO-2 phase III trial in a timely fashion during the era of COVID-19 isolation demonstrates the unmet need for new therapeutic agents in metastatic colorectal cancer. By meeting the primary endpoint of OS with a secondary endpoint of PFS, fruquintinib provides a significant potential new option for our refractory colorectal cancer patients. As an oral agent, fruquintinib also provides added convenience for our patients. Based on fruquintinib’s profile, we will likely see further exploration in future clinical trials in different settings. This is extremely encouraging, and I look forward to seeing the final results.”
Dr Weiguo Su, Chief Executive Officer and Chief Scientific Officer of HUTCHMED, said: “We are pleased to have successfully completed our first multi-regional clinical trial, FRESCO-2, to support the global registration of fruquintinib. It has already benefited patients with advanced CRC in China since its launch in 2018. It is also being evaluated alone and in combination with other agents in various tumor types in ongoing studies around the world.”
HUTCHMED retains all commercial rights to fruquintinib outside of China. In China, where fruquintinib is marketed under the brand name ELUNATE®, HUTCHMED is partnered with Eli Lilly and Company and is responsible for development and execution of all on-the-ground medical detailing, promotion and local and regional marketing. Fruquintinib is not approved for use outside of China.
About Fruquintinib
Fruquintinib is a highly selective and potent oral inhibitor of VEGFR-1, -2 and -3. VEGFR inhibitors play a pivotal role in blocking tumor angiogenesis. Fruquintinib was designed to improve kinase selectivity to minimize off-target toxicities, improve tolerability and provide more consistent target coverage. The generally good tolerability in patients to date, along with fruquintinib’s low potential for drug-drug interaction based on preclinical assessment, suggests that it may also be highly suitable for combinations with other anti-cancer therapies.
About Fruquintinib Approval in China
Metastatic CRC in China: Fruquintinib was approved for marketing by the China National Medical Products Administration (NMPA) in September 2018 and commercially launched in China in late November 2018 under the brand name ELUNATE®. It has been included in the China National Reimbursement Drug List (NRDL) since January 2020. ELUNATE® is indicated for the treatment of patients with metastatic CRC who have been previously treated with fluoropyrimidine, oxaliplatin and irinotecan, including those who have previously received anti-VEGF therapy and/or anti-EGFR therapy (RAS wild type). Results of the FRESCO study[iii], a Phase III pivotal registration trial of fruquintinib in 416 patients with metastatic CRC in China, were published in The Journal of the American Medical Association, JAMA, in June 2018 (clinicaltrials.gov identifier: NCT02314819).
About HUTCHMED
HUTCHMED (Nasdaq/AIM: HCM; HKEX: 13) is an innovative, commercial-stage, biopharmaceutical company. It is committed to the discovery and global development and commercialization of targeted therapies and immunotherapies for the treatment of cancer and immunological diseases. It has more than 4,900 personnel across all its companies, at the center of which is a team of about 1,800 in oncology/immunology. Since inception it has advanced 13 cancer drug candidates from in-house discovery into clinical studies around the world, with its first three oncology drugs now approved and marketed in China. For more information, please visit: www.hutch‑med.com or follow us on LinkedIn.
Hutchmed fruquintinib improves survival, meets main goal of colorectal cancer study
Aug. 08, 2022 5:55 AM ETHUTCHMED (China) Limited (HCM), LLYBAYRY, BAYZFBy: Ravikash, SA News Editor

Hutchmed (China) (NASDAQ:HCM) said its medicine fruquintinib met the main goal of overall survival (OS) in patients with advanced, refractory metastatic colorectal cancer (CRC) in a phase 3 trial.
The study called FRESCO-2 evaluated fruquintinib plus best supportive care (BSC) versus placebo plus BSC in patients with metastatic CRC who had progressed on standard chemotherapy and relevant biologic agents and who had progressed on, or were intolerant to, TAS-102 and/or regorafenib, sold as Stivarga by Bayer (OTCPK:BAYRY) (OTCPK:BAYZF).
https://seekingalpha.com/symbol/HCM
https://www.hutch-med.com/pipeline-and-products/our-pipeline/
TPOXX® (Tecovirimat)
TPOXX® (Tecovirimat)
TPOXX® (Tecovirimat)
Siga’s Monkeypox Drug to Start Human Testing in September
Aug. 5, 2022, 4:11 PM
- Studied only in animals, Tpoxx will undergo thorough review
- Therapy is now available through an expanded access protocol
SIGA's Tpoxx antiviral to undergo human testing for monkeypox in September - Bloomberg
Aug. 05, 2022 4:53 PM ET
SIGA Technologies, Inc. (SIGA)
By: Jonathan Block, SA News Editor1 Comment
- Tpoxx (tecovirimat), an antiviral medication from SIGA Technologies (NASDAQ:SIGA), will begin testing in humans as soon as September, Bloomberg reported.
- https://seekingalpha.com/news/3868451-sigas-tpoxx-antiviral-to-undergo-human-testing-for-monkeypox-in-september-bloomberg
- https://seekingalpha.com/symbol/SIGA
- https://www.siga.com/wp-content/themes/sigahba/TPOXX-Fact-Sheet.pdf
SIGA Announces Approximately $28 Million of International Procurement Orders for Oral TPOXX® (Tecovirimat)
July 12, 2022 at 4:15 PM EDT
- Approximately $26 Million of Orders Received from Canada under
Existing Procurement Contracts –
- Approximately $2 Million of Orders Received from
Two New Jurisdictions -
NEW YORK, July 12, 2022 (GLOBE NEWSWIRE) -- SIGA Technologies, Inc. (SIGA) (NASDAQ: SIGA),
Information for Healthcare Providers on Obtaining and Using TPOXX (Tecovirimat) for Treatment of Monkeypox
Updated July 22, 2022Print
CDC, in partnership with FDA, has made it easier for healthcare providers to provide tecovirimat (TPOXX) treatment to patients with monkeypox under the expanded access investigational new drug (EA-IND).
The streamlined process allows healthcare providers to start treatment before the paperwork is submitted, and reduces the number of required forms, patient samples, photos, and gives patients the option to see their doctor virtually.
https://www.cdc.gov/poxvirus/monkeypox/clinicians/obtaining-tecovirimat.html
VAX-24
TPOXX® (Tecovirimat)
TPOXX® (Tecovirimat)
Vaxcyte Provides Positive Regulatory Updates for VAX-24 Adult and Pediatric Programs
August 4, 2022PDF Version
-- Company Receives FDA Fast Track Designation for VAX-24 in Adults --
-- Vaxcyte Completes Successful Pre-IND Meeting with FDA Regarding VAX-24 Pediatric Program, Supporting Path to Proceed Directly into Infants --
-- VAX-24 is 24-Valent Pneumococcal Conjugate Vaccine Designed to Deliver Broad-Spectrum Protection to Prevent Invasive Pneumococcal Disease --
SAN CARLOS, Calif., Aug. 04, 2022 (GLOBE NEWSWIRE) -- Vaxcyte, Inc. (Nasdaq: PCVX), a clinical-stage vaccine innovation company engineering high-fidelity vaccines to protect humankind from the consequences of bacterial diseases, today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation to VAX-24, the Company’s 24-valent pneumococcal conjugate vaccine (PCV) candidate designed to prevent invasive pneumococcal disease (IPD), in adults ages 18 and older. The Fast Track designation is an FDA process that has been designed to facilitate the development and expedite the review of drugs, including vaccines, that treat or prevent serious conditions and fill an unmet medical need.
The Company also completed a successful pre-Investigational New Drug (IND) meeting with the FDA regarding the VAX-24 pediatric program. Vaxcyte received positive written feedback from the FDA supporting the initiation of a pediatric study that proceeds directly into infants, contingent on satisfactory topline safety, tolerability and immunogenicity results from the ongoing VAX-24 Phase 1/2 clinical proof-of-concept study in adults 18 to 64 years of age. This approach provides the Company with an accelerated clinical path to deliver a potentially best-in-class PCV, VAX-24, to the pediatric population, which represents the largest portion of the pneumococcal vaccine market in the United States.
“We are very pleased with the FDA’s feedback, which we believe provides an expedited path to deliver VAX-24 to adults and children, while also underscoring the need for a PCV that provides broader protection to prevent this serious disease,” said Grant Pickering, Chief Executive Officer and Co-Founder of Vaxcyte. “By leveraging our site-specific technology, the XpressCF™ cell-free protein synthesis platform, VAX-24 is designed to improve upon the standard-of-care PCVs and surpass the coverage of those currently available without compromising overall immune response.”
“Despite high vaccination rates, a broader spectrum PCV remains an important public health need, especially in vulnerable populations such as infants and older adults, due to substantial disease driven by emerging serotypes not covered by currently available vaccines,” said Jim Wassil, Executive Vice President and Chief Operating Officer of Vaxcyte. “With multiple milestones anticipated over the next 12 months for VAX-24, we expect strong, continued momentum.”
About VAX-24 and the Ongoing Adult Clinical Program
VAX-24 is an investigational 24-valent PCV candidate designed to prevent IPD, which can be most serious for infants, young children, older adults and those with immune deficiencies or certain chronic health conditions.
VAX-24 is intended to improve upon the standard-of-care PCVs for both children and adults by covering the serotypes that are responsible for most of the pneumococcal disease currently in circulation. Vaxcyte aims to efficiently create and deliver high-fidelity, broad-spectrum vaccines, such as VAX-24, by using modern synthetic techniques, including advanced chemistry and the XpressCF™ cell-free protein synthesis platform. Vaxcyte is deploying this approach with VAX-24 in order to add more pneumococcal strains without compromising the overall immune response.
VAX-24 is currently being evaluated in two clinical studies in adults:
- A Phase 1/2 Clinical Proof-of-Concept Study in Adults Aged 18-64: The Phase 1/2 clinical proof-of-concept study is now fully enrolled and the Company expects to announce topline safety and tolerability results from the Phase 1 portion of the study and safety, tolerability and immunogenicity results from the Phase 2 portion of the study in October or November 2022.
- The VAX-24 Phase 1/2 clinical proof-of-concept study (VAX-24 Study 101, NCT05266456) is a randomized, observer-blind, dose-finding, controlled study designed to evaluate the safety, tolerability and immunogenicity of VAX-24 in healthy adults 18-64 years of age.
- The Phase 1 portion of the study is evaluating safety and tolerability of a single injection of VAX-24 at three dose levels and compared to Prevnar 20™ in 64 healthy adults 18 to 49 years of age.
- The Phase 2 portion is evaluating the safety, tolerability and immunogenicity of a single injection of VAX-24 at three dose levels and compared to a single injection of Prevnar 20™ in approximately 800 healthy adults 50 to 64 years of age.
- A Separate Phase 2 Clinical Study in Adults Aged 65 and Older: Vaxcyte announced the dosing of the first participants in a separate Phase 2 study in adults 65 years of age and older in July 2022. Topline safety, tolerability and immunogenicity results from this study are expected in the first half of 2023, further building upon the body of clinical evidence to support the potential of VAX-24 as the broadest-spectrum PCV.
- This VAX-24 Phase 2 clinical study (VAX-24 Study 102, NCT05297578) is a randomized, observer-blind, dose-finding, controlled study designed to evaluate the safety, tolerability and immunogenicity of VAX-24 in approximately 200 healthy adults 65 years of age and older.
- The study is evaluating the safety, tolerability and immunogenicity of a single injection of VAX-24 at three dose levels and compared to a single injection of Prevnar 20™.
About Vaxcyte
Vaxcyte is a vaccine innovation company engineering high-fidelity vaccines to protect humankind from the consequences of bacterial diseases. The Company is developing broad-spectrum conjugate and novel protein vaccines to prevent or treat bacterial infectious diseases. Vaxcyte’s lead candidate, VAX-24, is a 24-valent, broad-spectrum pneumococcal conjugate vaccine being developed for the prevention of IPD. Vaxcyte is re-engineering the way highly complex vaccines are made through modern synthetic techniques, including advanced chemistry and the XpressCFTM cell-free protein synthesis platform, exclusively licensed from Sutro Biopharma, Inc. Unlike conventional cell-based approaches, the Company’s system for producing difficult-to-make proteins and antigens is intended to accelerate its ability to efficiently create and deliver high-fidelity vaccines with enhanced immunological benefits. Vaxcyte’s pipeline also includes VAX-XP, a PCV with an expanded breadth of coverage of greater than 30 strains; VAX-A1, a prophylactic vaccine candidate designed to prevent Group A Strep infections; and VAX-PG, a therapeutic vaccine candidate designed to slow or stop the progression of periodontal disease. Vaxcyte is driven to eradicate or treat invasive bacterial infections, which have serious and costly health consequences when left unchecked. For more information, visit www.vaxcyte.com.
Vaxcyte wins FDA’s Fast Track designation for pneumococcal vaccine candidate
Aug. 04, 2022 9:30 AM ET
By: Dulan Lokuwithana, SA News Editor
Clinical-stage biotech Vaxcyte, Inc. (NASDAQ:PCVX) announced on Thursday that the FDA awarded the Fast Track designation to the company's pneumococcal conjugate vaccine (PCV) candidate VAX-24 in adults aged 18 years and older.
https://seekingalpha.com/symbol/PCVX
RGX-121
HyBryte™ (research name SGX301)
ONPATTRO® (Patisiran)
REGENXBIO ANNOUNCES INTENTION TO FILE A BIOLOGICS LICENSE APPLICATION USING THE ACCELERATED APPROVAL PATHWAY FOR RGX-121, AN AAV THERAPEUTIC FOR THE TREATMENT OF MPS II
August 3, 2022 at 7:05 AM EDT
- FDA will consider an accelerated approval pathway for RGX-121; BLA filing expected in 2024
- Pivotal program is active and enrolling patients
- RGX-121 is a potential first-in-class, one-time gene therapy for the treatment of MPS II
- Internal cGMP manufacturing process expected to support BLA
ROCKVILLE, Md., Aug. 3, 2022 /PRNewswire/ -- REGENXBIO Inc. (Nasdaq: RGNX) today announced its intention to file a Biologics License Application (BLA) in 2024 using the FDA's accelerated approval pathway for RGX-121 for the treatment of Mucopolysaccharidosis Type II (MPS II), also known as Hunter Syndrome. The Company also announced that a pivotal program for RGX-121 is active and enrolling patients. RGX-121 is an investigational, one-time AAV Therapeutic using the NAV AAV9 vector to deliver the gene that encodes the iduronate-2-sulfatase (I2S) enzyme.
"We are pleased to share that our recent discussions with the FDA support our plans to submit a BLA for RGX-121 in 2024 using the accelerated approval pathway, which was created to allow for expedited development of drugs that treat serious conditions and provide a meaningful advantage over available therapies based on a surrogate endpoint," said Kenneth T. Mills, President and Chief Executive Officer of REGENXBIO. "We believe RGX-121 for the treatment of Hunter Syndrome has demonstrated emerging positive impact on neurodevelopmental function, and we intend to advance this program as quickly as possible with the aim of providing a much-needed new treatment option for the MPS II community."
"The accelerated approval pathway gives patients access to potentially life-changing therapeutics sooner, which is why it is a critical tool for the over 7,000 rare diseases, most of which lack FDA-approved treatments," said Joseph Muenzer, MD, PhD, Bryson Distinguished Professor in Pediatrics Genetics, and Director, MPS Research and Treatment Program, University of North Carolina at Chapel Hill. "Boys with MPS II do not have time to wait. I am encouraged by FDA's commitment to advance therapies for rare diseases and their willingness to consider this important pathway for RGX-121."
The ongoing Phase I/II trial of RGX-121 in children up to five years old has been expanded into a pivotal Phase I/II/III trial, named CAMPSIITE™. A BLA filing in 2024 is expected to be supported by endpoints in the pivotal program, including changes from baseline of glycosaminoglycans (GAGs) in the cerebrospinal fluid (CSF) at four months. GAGs in the CSF have the potential to be considered a surrogate biomarker that is reasonably likely to predict clinical benefit in MPS II disease under the accelerated approval pathway, as buildup of GAGs in the CSF of MPS II patients correlates with clinical manifestations, including neurodevelopmental deficits.
As presented in February 2022, preliminary results from REGENXBIO's Phase I/II trial of RGX-121 indicated that RGX-121 continued to be well-tolerated with dose-dependent reductions of GAGs in the CSF, with patients in Cohort 3 approaching normal levels of certain GAGs in the CSF. Measures of neurodevelopmental function from patients in Cohorts 1 and 2 demonstrated continued developmental skill acquisition up to 2 years after RGX-121 administration.
"MPS II families are in need of a treatment option that can address the neurodevelopmental decline associated with this disease that available enzyme replacement therapies cannot," said Terri Klein, President and CEO of the National MPS Society. "We are encouraged by today's announcement and the hope that a one-time gene therapy offers this community."
Pivotal Program (CAMPSIITE Trial)
CAMPSIITE is a multicenter, open-label trial enrolling boys with MPS II, aged 4 months up to five years of age. CAMPSIITE is now expected to enroll up to 10 MPS II patients to support the BLA filing using the accelerated approval pathway, with the potential to enroll additional patients. These patients will receive a dose of 2.9x1011 GC/g of brain mass of RGX-121, which is the same dose being evaluated in Cohort 3 of the Phase I/II trial. The pivotal program is using commercial-scale cGMP material from REGENXBIO's proprietary, high-yielding suspension-based manufacturing process, named NAVXPress™. In addition to measuring GAGs in the CSF, the trial will continue to collect neurodevelopmental data and caregiver-reported outcomes.
CAMPSIITE is a global trial, which is expected to include sites in the United States, Brazil and Canada. REGENXBIO has begun dosing patients in the pivotal program.
"MPS II patients face irreversible neurodevelopmental decline that significantly impacts a child's daily life and life expectancy," said Paul Harmatz, MD, professor, UCSF Department of Pediatrics, and principal investigator of the CAMPSIITE study. "Current therapies are inadequate, so we are excited to be a part of this study and eager to see the potential impact on patients."
REGENXBIO plans to share new RGX-121 data at the Society for the Study of Inborn Errors of Metabolism (SSIEM) Annual Symposium on August 31, 2022.
About RGX-121
RGX-121 is designed to use the NAV AAV9 vector to deliver the human iduronate-2-sulfatase gene (IDS) which encodes the iduronate-2-sulfatase (I2S) enzyme to the central nervous system (CNS). Delivery of the IDS gene within cells in the CNS could provide a permanent source of secreted I2S beyond the blood-brain barrier, allowing for long-term cross correction of cells throughout the CNS and consequent reduction of GAGs. RGX-121 has received orphan drug product, rare pediatric disease and Fast Track designations from the U.S. Food and Drug Administration.
RGX-121 is being evaluated in two on-going studies, CAMPSIITE, a Phase I/II/III multicenter, open-label clinical trial of patients up to five years old with MPS II and a Phase I/II multicenter, open-label clinical trial in patients over the age of five years old with MPS II.
About REGENXBIO Inc.
REGENXBIO is a leading clinical-stage biotechnology company seeking to improve lives through the curative potential of gene therapy. REGENXBIO's NAV Technology Platform, a proprietary adeno-associated virus (AAV) gene delivery platform, consists of exclusive rights to more than 100 novel AAV vectors, including AAV7, AAV8, AAV9 and AAVrh10. REGENXBIO and its third-party NAV Technology Platform Licensees are applying the NAV Technology Platform in the development of a broad pipeline of candidates, including late-stage and commercial programs, in multiple therapeutic areas. REGENXBIO is committed to a "5x'25" strategy to progress five AAV Therapeutics from our internal pipeline and licensed programs into pivotal-stage or commercial products by 2025.
View original content to download multimedia:https://www.prnewswire.com/news-releases/regenxbio-announces-intention-to-file-a-biologics-license-application-using-the-accelerated-approval-pathway-for-rgx-121-an-aav-therapeutic-for-the-treatment-of-mps-ii-301598783.html
SOURCE REGENXBIO Inc.
Regenxbio to seek FDA's accelerated approval for Hunter Syndrome treatment, shares rise 8%
Aug. 03, 2022 10:02 AM ET
By: Anuron Mitra, SA News Editor
- Regenxbio (NASDAQ:RGNX) on Wednesday said it intends to file a biologics license application (BLA) in 2024 using the U.S. FDA's accelerated approval process for its RGX-121 treatment candidate for Mucopolysaccharidosis Type II (MPS II).
- https://seekingalpha.com/news/3865767-regenxbio-to-seek-fdas-accelerated-approval-for-hunter-syndrome-treatment-shares-rise-8
- https://seekingalpha.com/symbol/RGNX
- https://regenxbio.com/
ONPATTRO® (Patisiran)
HyBryte™ (research name SGX301)
ONPATTRO® (Patisiran)
Alnylam Reports Positive Topline Results from APOLLO-B Phase 3 Study of Patisiran in Patients with ATTR Amyloidosis with Cardiomyopathy
Aug 03, 2022
– Patisiran Met the Primary Endpoint with a Statistically Significant Improvement in 6-Minute Walk Test Compared to Placebo at 12 Months –
– Patisiran Also Met the First Secondary Endpoint with a Statistically Significant Improvement in Quality of Life, as Measured by the Kansas City Cardiomyopathy Questionnaire, Compared to Placebo at 12 Months –
– Patisiran Demonstrated Encouraging Safety and Tolerability Profile in Patients with ATTR Amyloidosis with Cardiomyopathy –
– Company Plans to File a Supplemental New Drug Application in U.S. in Late 2022 –
– Full Data Will Be Presented at the 18th International Symposium on Amyloidosis –
– Alnylam to Host Conference Call Today at 8:00 am ET –
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Aug. 3, 2022-- Alnylam Pharmaceuticals, Inc. (Nasdaq: ALNY), the leading RNAi therapeutics company, today announced that the APOLLO-B Phase 3 study of patisiran, an investigational RNAi therapeutic in development for the treatment of transthyretin-mediated (ATTR) amyloidosis with cardiomyopathy, met the primary endpoint of change from baseline in the 6-Minute Walk Test (6-MWT) at 12 months compared to placebo (p-value 0.0162). The study also met the first secondary endpoint of change from baseline in quality of life compared to placebo, as measured by the Kansas City Cardiomyopathy Questionnaire (KCCQ) (p-value 0.0397).
The study also included additional secondary composite outcome endpoints to be tested in a hierarchical manner. A non-significant result (p-value 0.0574) was found on the secondary composite endpoint of all-cause mortality, frequency of cardiovascular events, and change from baseline in 6-MWT over 12 months compared to placebo. As a result, formal statistical testing was not performed on the final two composite endpoints, which were not powered for statistical significance given the short duration of the study — all-cause mortality and frequency of all-cause hospitalizations and urgent heart failure visits in patients not on tafamidis at baseline (nominal p-value 0.9888), and in the overall population (nominal p-value 0.5609). Patisiran also demonstrated an encouraging safety and tolerability profile, with deaths numerically favoring the patisiran arm.
“We are thrilled that APOLLO-B successfully met all its major objectives, which we believe for the first time validates the hypothesis that TTR silencing by an RNAi therapeutic can be an effective approach for treating the cardiomyopathy of ATTR amyloidosis,” said Pushkal Garg, M.D., Chief Medical Officer of Alnylam. “ATTR amyloidosis with cardiomyopathy is an increasingly recognized cause of heart failure, affecting greater than 250,000 patients around the world. These patients have limited treatment options, and disease progression is common. As such, we are encouraged to see the potential of patisiran to improve the functional capacity and quality of life of patients living with this fatal, multi-system disease. I want to thank all the patients, caregivers, investigators, and study staff who have and continue to participate in APOLLO-B. We look forward to sharing full results at an upcoming conference in September, and based on these positive results, we plan to submit a supplemental NDA for patisiran with the U.S. Food and Drug Administration in late 2022.”
APOLLO-B is a Phase 3, randomized, double-blind, placebo-controlled multicenter global study designed and powered to evaluate the effects of patisiran on functional capacity and quality of life in patients with ATTR amyloidosis with cardiomyopathy. The study enrolled 360 adult patients with ATTR amyloidosis (hereditary or wild-type) with cardiomyopathy at 69 sites in 21 countries. Patients were randomized 1:1 to receive 0.3 mg/kg of patisiran or placebo intravenously administered every three weeks over a 12-month double-blind treatment period. After 12 months, all patients will receive patisiran in an open-label extension period.
The primary endpoint of APOLLO-B is the change from baseline in the 6-MWT at 12 months compared to placebo. The secondary endpoints evaluate the efficacy of patisiran vs. placebo over 12 months in a hierarchical manner with the following measures:
- Health-related quality of life with the KCCQ change from baseline at 12 months;
- Composite of all-cause mortality, frequency of cardiovascular (CV) events (CV hospitalizations and urgent heart failure (HF) visits) and change from baseline in 6-MWT;
- Composite of all-cause mortality and frequency of all-cause hospitalizations and urgent HF visits in patients not on tafamidis at baseline; and
- Composite of all-cause mortality and frequency of all-cause hospitalizations and urgent HF visits in the overall study population.
Exploratory endpoints included cardiac biomarkers and various imaging tools to further characterize the potential burden of cardiac involvement in these patients.
The overall safety profile of patisiran during the 12-month double-blind period was encouraging.
- 5 patients (2.8 percent) on patisiran and 8 patients (4.5 percent) on placebo died. Furthermore, the number of deaths in the all-cause mortality efficacy analysis was 4 (2.2 percent) in the patisiran arm and 10 (5.6 percent) in the placebo arm, determined in accordance with the pre-defined statistical analysis plan, which excluded death due to COVID-19, and treated cardiac transplant as a death event consistent with other studies in the field.
- The patisiran and placebo arms had similar frequencies of adverse events (AEs) (91.2 percent and 94.4 percent, respectively) and serious adverse events (SAEs) (33.7 percent and 35.4 percent, respectively). AEs reported in greater than or equal to 5 percent of patisiran patients and seen at least 3 percent more frequently with patisiran compared with placebo were infusion-related reactions (12.2 percent vs. 9 percent, respectively), arthralgia (7.7 percent vs. 4.5 percent, respectively), and muscle spasms (6.6 percent vs. 2.2 percent, respectively). No SAEs occurred at least 2 percent more frequently in patisiran versus placebo treated patients.
“I am delighted by the results of the APOLLO-B study, which suggest the potential for patisiran to be a treatment option for patients with ATTR amyloidosis with cardiomyopathy, assuming favorable regulatory review. In addition, the APOLLO-B data further strengthen our confidence in our Phase 3 HELIOS-B study of vutrisiran in ATTR amyloidosis with cardiomyopathy, which is expected to report out in early 2024,” said Yvonne Greenstreet, MBChB, Chief Executive Officer of Alnylam. “Today’s positive results advance our goal to establish an industry leading TTR franchise, which currently includes ONPATTRO® and AMVUTTRATM for the polyneuropathy of hereditary ATTR amyloidosis. We believe these data take us one step closer to achieving our Alnylam P5x25 vision of becoming a leading biopharma company.”
Full results of the APOLLO-B study will be presented as part of a late-breaker session at the 18th International Symposium on Amyloidosis on September 8, 2022, in Heidelberg, Germany.
Patisiran is the established name for ONPATTRO, which is approved in the United States and Canada for the treatment of the polyneuropathy of hATTR amyloidosis in adults. ONPATTRO is also approved in the European Union, Switzerland and Brazil for the treatment of hATTR amyloidosis in adults with Stage 1 or Stage 2 polyneuropathy, and in Japan for the treatment of hATTR amyloidosis with polyneuropathy.
About ONPATTRO® (Patisiran)
ONPATTRO is an RNAi therapeutic that is approved in the United States and Canada for the treatment of the polyneuropathy of hATTR amyloidosis in adults. ONPATTRO is also approved in the European Union, Switzerland and Brazil for the treatment of hATTR amyloidosis in adults with Stage 1 or Stage 2 polyneuropathy, and in Japan for the treatment of hATTR amyloidosis with polyneuropathy. ONPATTRO is an intravenously administered RNAi therapeutic targeting transthyretin (TTR). It is designed to target and silence TTR messenger RNA, thereby reducing the production of TTR protein before it is made. Reducing the pathogenic protein leads to a reduction in amyloid deposits in tissues. For more information about ONPATTRO, including full Prescribing Information, visit ONPATTRO.com.
ONPATTRO Indication and ISI
Indication
ONPATTRO is indicated for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis in adults.
Important Safety Information
Infusion-Related Reactions
Infusion-related reactions (IRRs) have been observed in patients treated with ONPATTRO. In a controlled clinical study, 19% of ONPATTRO-treated patients experienced IRRs, compared to 9% of placebo-treated patients. The most common symptoms of IRRs with ONPATTRO were flushing, back pain, nausea, abdominal pain, dyspnea, and headache.
To reduce the risk of IRRs, patients should receive premedication with a corticosteroid, acetaminophen, and antihistamines (H1 and H2 blockers) at least 60 minutes prior to ONPATTRO infusion. Monitor patients during the infusion for signs and symptoms of IRRs. If an IRR occurs, consider slowing or interrupting the infusion and instituting medical management as clinically indicated. If the infusion is interrupted, consider resuming at a slower infusion rate only if symptoms have resolved. In the case of a serious or life-threatening IRR, the infusion should be discontinued and not resumed.
Reduced Serum Vitamin A Levels and Recommended Supplementation
ONPATTRO treatment leads to a decrease in serum vitamin A levels. Supplementation at the recommended daily allowance (RDA) of vitamin A is advised for patients taking ONPATTRO. Higher doses than the RDA should not be given to try to achieve normal serum vitamin A levels during treatment with ONPATTRO, as serum levels do not reflect the total vitamin A in the body.
Patients should be referred to an ophthalmologist if they develop ocular symptoms suggestive of vitamin A deficiency (e.g. night blindness).
Adverse Reactions
The most common adverse reactions that occurred in patients treated with ONPATTRO were upper respiratory tract infections (29%) and infusion‑related reactions (19%).
About Alnylam Pharmaceuticals
Alnylam (Nasdaq: ALNY) has led the translation of RNA interference (RNAi) into a whole new class of innovative medicines with the potential to transform the lives of people afflicted with rare and prevalent diseases with unmet need. Based on Nobel Prize-winning science, RNAi therapeutics represent a powerful, clinically validated approach yielding transformative medicines. Since its founding 20 years ago, Alnylam has led the RNAi Revolution and continues to deliver on a bold vision to turn scientific possibility into reality. Alnylam’s commercial RNAi therapeutic products are ONPATTRO® (patisiran), GIVLAARI® (givosiran), OXLUMO® (lumasiran), AMVUTTRA™ (vutrisiran) and Leqvio® (inclisiran) being developed and commercialized by Alnylam’s partner, Novartis. Alnylam has a deep pipeline of investigational medicines, including multiple product candidates that are in late-stage development. Alnylam is executing on its “Alnylam P5x25” strategy to deliver transformative medicines in both rare and common diseases benefiting patients around the world through sustainable innovation and exceptional financial performance, resulting in a leading biotech profile. Alnylam is headquartered in Cambridge, MA. For more information about our people, science and pipeline, please visit www.alnylam.com and engage with us on Twitter at @Alnylam, on LinkedIn, or on Instagram.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220803005528/en/
Alnylam Pharmaceuticals, Inc.
Source: Alnylam Pharmaceuticals, Inc.
Alnylam soars 42% as Phase 3 trial for ATTR amyloidosis therapy meets main goal
Aug. 03, 2022 9:33 AM ET
Alnylam Pharmaceuticals, Inc. (ALNY)
By: Dulan Lokuwithana, SA News Editor1 Comment
Alnylam Pharmaceuticals (NASDAQ:ALNY) added nearly 42% in the morning hours Wednesday after the RNAi therapeutics company said that its Phase 3 trial for patisiran reached the primary goal in transthyretin-mediated (ATTR) amyloidosis with cardiomyopathy.
https://seekingalpha.com/symbol/ALNY
HyBryte™ (research name SGX301)
HyBryte™ (research name SGX301)
Tofersen (formerly IONIS-SOD1Rx), also known as BIIB067
Soligenix Receives Agreement from FDA on Initial Pediatric Study Plan for HyBryte™ for the Treatment of Cutaneous T-Cell Lymphoma
PRINCETON, N.J., July 27, 2022 /PRNewswire/ -- Soligenix, Inc. (Nasdaq: SNGX) (Soligenix or the Company), a late-stage biopharmaceutical company focused on developing and commercializing products to treat rare diseases where there is an unmet medical need, announced today that it has received agreement from the US Food & Drug Administration (FDA) on an initial pediatric study plan (iPSP) for HyBryte™ (synthetic hypericin) for the treatment of cutaneous T-cell lymphoma (CTCL). The agreed iPSP stipulates that Soligenix intends on requesting a full waiver of pediatric studies upon submission of a new drug application (NDA). Agreement with FDA on an iPSP is one of the regulatory requirements that must be met prior to submitting a NDA.
"We are pleased to have FDA's agreement on our proposal to request a full waiver of pediatric studies at the time of our HyBryte™ NDA filing later this year," stated Christopher J. Schaber, PhD, President & Chief Executive Officer of Soligenix. "This is consistent with decisions by the European Medicines Agency (EMA) and Medicines and Healthcare products Regulatory Agency (MHRA) in the United Kingdom which have previously granted product-specific waivers from the requirement for pediatric studies in applications for marketing authorization of HyBryte™ in the UK and Europe."
About HyBryte™
HyBryte™ (research name SGX301) is a novel, first-in-class, photodynamic therapy utilizing safe, visible light for activation. The active ingredient in HyBryte™ is synthetic hypericin, a potent photosensitizer that is topically applied to skin lesions that is taken up by the malignant T-cells, and then activated by visible light 16 to 24 hours later. The use of visible light in the red-yellow spectrum has the advantage of penetrating more deeply into the skin (much more so than ultraviolet light) and therefore potentially treating deeper skin disease and thicker plaques and lesions. This treatment approach avoids the risk of secondary malignancies (including melanoma) inherent with the frequently employed DNA-damaging drugs and other phototherapy that are dependent on ultraviolet exposure. Combined with photoactivation, hypericin has demonstrated significant anti-proliferative effects on activated normal human lymphoid cells and inhibited growth of malignant T-cells isolated from CTCL patients. In a published Phase 2 clinical study in CTCL, patients experienced a statistically significant (p=0.04) improvement with topical hypericin treatment whereas the placebo was ineffective. HyBryte™ has received orphan drug and fast track designations from the FDA, as well as orphan designation from the European Medicines Agency (EMA).
The recently published Phase 3 FLASH trial trial enrolled a total of 169 patients (166 evaluable) with Stage IA, IB or IIA CTCL. The trial consisted of three treatment cycles. Treatments were administered twice weekly for the first 6 weeks and treatment response was determined at the end of the 8th week of each cycle. In the first double-blind treatment cycle, 116 patients received HyBryte™ treatment (0.25% synthetic hypericin) and 50 received placebo treatment of their index lesions. A total of 16% of the patients receiving HyBryte™ achieved at least a 50% reduction in their lesions (graded using a standard measurement of dermatologic lesions, the CAILS score) compared to only 4% of patients in the placebo group at 8 weeks (p=0.04) during the first treatment cycle (primary endpoint). HyBryte™ treatment in the first cycle was safe and well tolerated.
In the second open-label treatment cycle (Cycle 2), all patients received HyBryte™ treatment of their index lesions. Evaluation of 155 patients in this cycle (110 receiving 12 weeks of HyBryte™ treatment and 45 receiving 6 weeks of placebo treatment followed by 6 weeks of HyBryte™ treatment), demonstrated that the response rate among the 12-week treatment group was 40% (p<0.0001 vs the placebo treatment rate in Cycle 1). Comparison of the 12-week and 6-week treatment groups also revealed a statistically significant improvement (p<0.0001) between the two groups, indicating that continued treatment results in better outcomes. HyBryte™ continued to be safe and well tolerated. Additional analyses also indicated that HyBryte™ is equally effective in treating both plaque (response 42%, p<0.0001 relative to placebo treatment in Cycle 1) and patch (response 37%, p=0.0009 relative to placebo treatment in Cycle 1) lesions of CTCL, a particularly relevant finding given the historical difficulty in treating plaque lesions in particular.
The third (optional) treatment cycle (Cycle 3) was focused on safety and all patients could elect to receive HyBryte™ treatment of all their lesions. Of note, 66% of patients elected to continue with this optional compassionate use / safety cycle of the study. Of the subset of patients that received HyBryte™ throughout all 3 cycles of treatment, 49% of them demonstrated a positive treatment response (p<0.0001 vs patients receiving placebo in Cycle 1). Moreover, in a subset of patients evaluated in this cycle, it was demonstrated that HyBryte™ is not systemically available, consistent with the general safety of this topical product observed to date. At the end of Cycle 3, HyBryte™ continued to be well tolerated despite extended and increased use of the product to treat multiple lesions.
Overall safety of HyBryte™ is a critical attribute of this treatment and was monitored throughout the three treatment cycles (Cycles 1, 2 and 3) and the 6-month follow-up period. HyBryte's™ mechanism of action is not associated with DNA damage, making it a safer alternative than currently available therapies, all of which are associated with significant and sometimes fatal, side effects. Predominantly these include the risk of melanoma and other malignancies, as well as the risk of significant skin damage and premature skin aging. Currently available treatments are only approved in the context of previous treatment failure with other modalities and there is no approved front-line therapy available. Within this landscape, treatment of CTCL is strongly motivated by the safety risk of each product. HyBryte™ potentially represents the safest available efficacious treatment for CTCL. With no systemic absorption, a compound that is not mutagenic and a light source that is not carcinogenic, there is no evidence to date of any potential safety issues.
The Phase 3 CTCL clinical study was partially funded by the National Cancer Institute via a Phase II SBIR grant (#1R44CA210848-01A1) awarded to Soligenix, Inc.
About Soligenix, Inc.
Soligenix is a late-stage biopharmaceutical company focused on developing and commercializing products to treat rare diseases where there is an unmet medical need. Our Specialized BioTherapeutics business segment is developing and moving toward potential commercialization of HyBryte™ (SGX301 or synthetic hypericin) as a novel photodynamic therapy utilizing safe visible light for the treatment of cutaneous T-cell lymphoma (CTCL). With a successful Phase 3 study completed, regulatory approval is being sought and commercialization activities for this product candidate are being advanced initially in the U.S. Development programs in this business segment also include our first-in-class innate defense regulator (IDR) technology, dusquetide (SGX942) for the treatment of inflammatory diseases, including oral mucositis in head and neck cancer, and proprietary formulations of oral beclomethasone 17,21-dipropionate (BDP) for the prevention/treatment of gastrointestinal (GI) disorders characterized by severe inflammation including pediatric Crohn's disease (SGX203).
Our Public Health Solutions business segment includes active development programs for RiVax®, our ricin toxin vaccine candidate, and SGX943, our therapeutic candidate for antibiotic resistant and emerging infectious disease, and our vaccine programs targeting filoviruses (such as Marburg and Ebola) and CiVax™, our vaccine candidate for the prevention of COVID-19 (caused by SARS-CoV-2). The development of our vaccine programs incorporates the use of our proprietary heat stabilization platform technology, known as ThermoVax®. To date, this business segment has been supported with government grant and contract funding from the National Institute of Allergy and Infectious Diseases (NIAID), the Defense Threat Reduction Agency (DTRA) and the Biomedical Advanced Research and Development Authority (BARDA).
For further information regarding Soligenix, Inc., please visit the Company's website at https://www.soligenix.com and follow us on LinkedIn and Twitter at @Soligenix_Inc.
SOURCE Soligenix, Inc.
Soligenix gets agreement from FDA for photodynamic therapy study in kids for lymphoma
Jul. 27, 2022 8:22 AM ET
By: Ravikash, SA News Editor
- Soligenix (NASDAQ:SNGX) said it received agreement from the U.S. Food & Drug Administration (FDA) on an initial pediatric study plan ((iPSP)) of its photodynamic therapy HyBryte (synthetic hypericin) to treat cutaneous T-cell lymphoma (CTCL).
- https://seekingalpha.com/news/3861272-soligenix-gets-agreement-from-fda-for-photodynamic-therapy-study-in-kids-for-lymphoma
- https://seekingalpha.com/symbol/SNGX
- https://www.soligenix.com/pipeline-programs/
- https://www.soligenix.com/
- https://www.hybryte.com/
Tofersen (formerly IONIS-SOD1Rx), also known as BIIB067
Tofersen (formerly IONIS-SOD1Rx), also known as BIIB067
Tofersen (formerly IONIS-SOD1Rx), also known as BIIB067
FDA Accepts Biogen’s New Drug Application and Grants Priority Review of Tofersen for a Rare, Genetic Form of ALS
JULY 26, 2022 • INVESTOR RELATIONS
- SOD1-ALS is a rare genetic form of ALS that affects approximately 330 people in the U.S.,1 it is progressive, leads to the loss of everyday functions and is uniformly fatal
- If approved, tofersen would be the first treatment to target a genetic cause of ALS
- 12-month data included in the filing show that earlier initiation of tofersen slowed decline across measures of clinical and respiratory function, strength, and quality of life
CAMBRIDGE, Mass., July 26, 2022 (GLOBE NEWSWIRE) -- Biogen Inc. (Nasdaq: BIIB) today announced that the U.S. Food and Drug Administration (FDA) has accepted a New Drug Application (NDA) for tofersen, an investigational drug for superoxide dismutase 1 (SOD1) amyotrophic lateral sclerosis (ALS). The application has been granted priority review and given a Prescription Drug User Fee Act action date of January 25, 2023. The FDA has noted that it is currently planning to hold an Advisory Committee meeting for this application, on a yet-to-be determined date. The average life expectancy for people with ALS is three to five years from time of symptom onset. There is currently no treatment targeted for SOD1-ALS.2
“The available data show that tofersen has the potential to make a meaningful difference for people with SOD1-ALS,” said Priya Singhal, M.D., M.P.H., Head of Global Safety and Regulatory Sciences and Interim Head of R&D at Biogen. “Pursuing the FDA’s accelerated approval pathway offers the potential to make tofersen available to people living with this fatal, neurodegenerative disease as quickly as possible. If approved, tofersen will be the first treatment to target a genetic cause of ALS and we hope this will pave the way for further advances in this relentless disease.”
Biogen is seeking approval of tofersen under the FDA’s accelerated approval pathway, based on the use of neurofilament as a surrogate biomarker that is reasonably likely to predict clinical benefit. Neurofilaments are normal proteins found in healthy neurons, that are increased in blood and cerebrospinal fluid when damage has been done to neurons or their axons and are a marker of neurodegeneration. In ALS, higher levels of neurofilaments have been found to predict more rapid decline in clinical function and shortened survival.3 Tofersen study results suggest reductions in neurofilament preceded and predicted slowing of decline in measures of clinical and respiratory function, strength, and quality of life. Biogen is committed to ongoing data generation and finalizing the confirmatory data package with the FDA.
“The 12-month results showed that individuals with SOD1-ALS who started tofersen earlier experienced a slower rate of decline in clinical and respiratory function, strength and quality of life. These are critical measures for people living with this devastating disease,” said Timothy Miller, M.D., Ph.D., principal investigator of VALOR and ALS Center co-Director at Washington University School of Medicine, St. Louis. “For people in my clinic living with SOD1-ALS, tofersen may meaningfully slow the rapid progression of their disease and the impact it has on their lives.”
The tofersen NDA included results from a Phase 1 study in healthy volunteers, a Phase 1/2 study evaluating ascending dose levels, the Phase 3 VALOR study, and the open label extension (OLE) study. Also included are the most current 12-month integrated results from VALOR and the OLE study, recently presented at the European Network to Cure ALS (ENCALS) annual meeting.
As previously reported in October 2021, VALOR, a six-month Phase 3 randomized study, did not meet the primary endpoint of change from baseline to week 28 in the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale. However, trends of reduced disease progression across multiple secondary and exploratory endpoints were observed. The 12-month integrated data showed that earlier initiation of tofersen led to sustained reductions in neurofilament, a marker of neurodegeneration and slowed decline across multiple efficacy endpoints.
In the 12-month data, the most common adverse events (AEs) in participants receiving tofersen in VALOR and the OLE study were headache, procedural pain, fall, back pain and pain in extremities. Most AEs in both VALOR and the OLE were mild to moderate in severity. Serious neurologic events including myelitis, radiculitis, aseptic meningitis, and papilledema, were reported in 6.7 percent of participants receiving tofersen in VALOR and its OLE.
During the FDA review period Biogen will maintain its early access program for tofersen, now with participants in over a dozen countries. The open-label extension and Phase 3 ATLAS study in presymptomatic individuals with a SOD1 genetic mutation remain ongoing. Biogen is actively engaging with other regulators around the world and will provide updates when appropriate.
About Tofersen
Tofersen is an antisense drug being evaluated for the potential treatment of SOD1-ALS. Tofersen binds to SOD1 mRNA, allowing for its degradation by RNase-H in an effort to reduce synthesis of SOD1 protein production. In addition to the ongoing open label extension of VALOR, tofersen is being studied in the Phase 3 ATLAS study designed to evaluate whether tofersen can delay clinical onset when initiated in presymptomatic individuals with a SOD1 genetic mutation and biomarker evidence of disease activity. Biogen licensed tofersen from Ionis Pharmaceuticals, Inc. under a collaborative development and license agreement.
About Biogen
As pioneers in neuroscience, Biogen discovers, develops, and delivers worldwide innovative therapies for people living with serious neurological diseases as well as related therapeutic adjacencies. One of the world’s first global biotechnology companies, Biogen was founded in 1978 by Charles Weissmann, Heinz Schaller, Sir Kenneth Murray, and Nobel Prize winners Walter Gilbert and Phillip Sharp. Today, Biogen has a leading portfolio of medicines to treat multiple sclerosis, has introduced the first approved treatment for spinal muscular atrophy, and developed the first and only approved treatment to address a defining pathology of Alzheimer’s disease. Biogen is also commercializing biosimilars and focusing on advancing one of the industry’s most diversified pipelines in neuroscience that will transform the standard of care for patients in several areas of high unmet need.
In 2020, Biogen launched a bold 20-year, $250 million initiative to address the deeply interrelated issues of climate, health, and equity. Healthy Climate, Healthy Lives™ aims to eliminate fossil fuels across the company’s operations, build collaborations with renowned institutions to advance the science to improve human health outcomes, and support underserved communities.
We routinely post information that may be important to investors on our website at www.biogen.com. Follow us on social media - Twitter, LinkedIn, Facebook, YouTube.
Biogen/Ionis ALS therapy tofersen gets FDA priority review
Jul. 26, 2022 9:14 AM ET
By: Ravikash, SA News Editor1 Comment
The U.S. Food and Drug Administration (FDA) granted priority review to Biogen's (NASDAQ:BIIB) and Ionis' (NASDAQ:IONS) tofersen to treat patients with superoxide dismutase 1 (SOD1) amyotrophic lateral sclerosis (ALS).
https://seekingalpha.com/news/3860495-biogenionis-als-therapy-tofersen-gets-fda-priority-review
https://seekingalpha.com/symbol/BIIB
https://seekingalpha.com/symbol/IONS
TRUSELTIQ (infigratinib) capsules
Tofersen (formerly IONIS-SOD1Rx), also known as BIIB067
TRUSELTIQ (infigratinib) capsules
BridgeBio Pharma Announces Positive Interim Results from a Phase 2 Trial of Infigratinib in Achondroplasia Demonstrating an Increase in Annualized Height Velocity of 1.52 cm/year in Children 5 Years of Age and Older, and Adds 5th Cohort to Trial
– At the highest dose level evaluated to date (Cohort 4, 0.128 mg/kg once daily), the mean change from baseline in annualized height velocity (AHV) was +1.52 cm/yr (p=0.02, n=11) and the responder rate was 64% in children 5 years and older 1
– Infigratinib was well-tolerated with no serious adverse events (SAE) and no discontinuations due to adverse events (AE) including in Cohort 5 (dose: 0.25 mg/kg once daily) participants dosed to date, with a median duration of follow-up of 48.1 weeks; only a limited number of AEs were assessed as related to study drug and all were Grade 1, the lowest level
– Given infigratinib’s profile to date, and after discussions with regulators, BridgeBio has begun dosing children in Cohort 5 (dose: 0.25 mg/kg once daily)
– Infigratinib is the only known oral product candidate currently under clinical investigation for achondroplasia, with granted and filed patent applications expiring as late as 2041
PALO ALTO, CA – July 26, 2022 — BridgeBio Pharma, Inc. (Nasdaq: BBIO) (BridgeBio), a commercial-stage biopharmaceutical company focused on genetic diseases and cancers, today announced positive interim results from PROPEL 2, a Phase 2 trial of the investigational therapy infigratinib in children with achondroplasia. Achondroplasia (ACH) is the most common cause of disproportionate short stature. Achondroplasia impacts health and can lead to medical complications such as obstructive sleep apnea, middle ear dysfunction, kyphosis, and spinal stenosis. Achondroplasia affects approximately 55,000 people in the United States (US) and Europe, including up to 13,000 children and adolescents with open growth plates. The condition is uniformly caused by an activating mutation in fibroblast growth factor receptor 3 (FGFR3). Infigratinib is an oral small molecule that inhibits FGFR3, therefore designed to target this well-described disease at its source.
At the highest dose level evaluated to date (0.128 mg/kg once daily), mean increase in annualized height velocity (AHV) was 1.52 cm/yr over baseline (p=0.02, n=11) for all follow-up data available at time of data cut in children 5 years of age and older. In this group, 64% were responders (defined with a strict criterion of an increase ≥25% in AHV from baseline) and the average percent change from baseline in AHV was 60%.
Earlier cohorts in PROPEL 2 did not achieve the target efficacious exposure as suggested by our preclinical data and no dose response was observed. An increase in AHV over baseline of 0.22 cm/yr (p=0.54, n=38) was observed across these earlier combined cohorts for children 5 years of age and older.
PROPEL 2 enrolled children as young as 3 years of age in the study. Consistent with other trials in the younger age population, both AHV and height Z-scores were analyzed to help control for greater variability in growth seen by age and sex in children 3 to <5 years old. In this age group, the average increase in ACH height Z-score at 6 months was 0.21 standard deviation score (SDS) and an increase in AHV of 0.61 cm/yr over baseline (n=5) was observed. Across Cohort 4, the median duration of follow-up was 26.9 weeks at time of data cut.
“These interim data demonstrate compelling initial proof-of-concept for an oral FGFR inhibitor in children with achondroplasia. We are encouraged by what we have seen to date, including the overall safety profile and promising initial efficacy data of infigratinib. We look forward to completing enrollment in Cohort 5 with the goal of presenting the full study results next year,” said Professor Ravi Savarirayan, M.D., Ph.D., clinical geneticist and group leader of skeletal therapies research at the Murdoch Children’s Research Institute in Australia, the lead investigator for PROPEL 2.
Median follow-up across the entire study is 48.1 weeks across 62 participants included in the safety population at time of data cut. No treatment-related SAEs have been reported to date in any cohort. 90.3% of participants experienced at least one treatment-emergent adverse event (TEAE), the majority of which were Grade 1, unrelated to study drug, and consistent with a pediatric achondroplasia population. Only 9.7% of participants had a TEAE related to study drug, all of which were Grade 1, and included dyspepsia, decreased appetite, flatulence, hypercholesterolemia, hyperphosphatemia, and vitamin D decrease.
A single case of mild hyperphosphatemia (Grade 1) led to a dose reduction in a participant in Cohort 3 (dose: 0.064 mg/kg once daily), the only dose adjustment made to date in the study. Phosphorus levels for this participant only exceeded upper limit of normal by <10% and returned to and remain normal at the reduced dose (0.032 mg/kg once daily). No other cases of hyperphosphatemia have been observed in any other cohort (including Cohort 5) to date, and no trends in phosphorous by dose have been observed. No other AEs required dose modifications or interruptions.
No children have discontinued treatment as the result of an adverse event. No bone-related AEs were observed to date.
“I am encouraged by this interim efficacy and safety data and thankful, as ever, to be partnered with the healthcare providers, children, and families who are making this study possible. These data, combined with our positive proof-of-concept data in LGMD2i and ADH1 earlier this year, highlight BridgeBio’s ability to efficiently prosecute high value programs in large areas of unmet need. We look forward to exploring the potential of infigratinib in achondroplasia and related skeletal dysplasias in the near future,” said Neil Kumar, Ph.D., founder and CEO of BridgeBio.
BridgeBio, after discussions with regulatory agencies, has begun enrolling Cohort 5. Cohort 5 participants are receiving approximately twice the dose of Cohort 4 (0.25 mg/kg once daily vs 0.128 mg/kg once daily in Cohort 4). At the conclusion of the ongoing trial, BridgeBio intends to present full data at a medical conference in the first half of 2023. Additionally, BridgeBio expects to evaluate development of infigratinib in other FGFR-driven skeletal dysplasias, which affect more than 50,000 people in the US and Europe, building on this positive interim data from PROPEL 2 as well as preclinical data in hypochondroplasia presented at the Endocrine Society (ENDO) 2022 Annual Conference earlier this year.
Infigratinib is not approved in any country for the treatment of children or adults with achondroplasia. For more information on infigratinib, please see the following link.
About BridgeBio Pharma, Inc.
BridgeBio Pharma (BridgeBio) is a commercial-stage biopharmaceutical company founded to discover, create, test and deliver transformative medicines to treat patients who suffer from genetic diseases and cancers with clear genetic drivers. BridgeBio’s pipeline of development programs ranges from early science to advanced clinical trials. BridgeBio was founded in 2015 and its team of experienced drug discoverers, developers and innovators are committed to applying advances in genetic medicine to help patients as quickly as possible. For more information visit bridgebio.com and follow us on LinkedIn and Twitter.
BridgeBio up 11% following positive mid-stage results of infigratinib in achondroplasia
Jul. 26, 2022 9:27 AM ET
By: Jonathan Block, SA News Editor
- Shares of BridgeBio Pharma (NASDAQ:BBIO) are up 11% in premarket trading after reporting positive phase 2 results for infigratinib in children with achondroplasia.
- https://seekingalpha.com/news/3860508-bridgebio-up-11-following-positive-mid-stage-results-of-infigratinib-in-achondroplasia
- https://seekingalpha.com/symbol/BBIO
- https://www.truseltiq.com/
- https://www.truseltiq.com/pdfs/prescribing-information.pdf
- https://bridgebio.com/
TX200
Tofersen (formerly IONIS-SOD1Rx), also known as BIIB067
TRUSELTIQ (infigratinib) capsules
European Orphan Medicinal Product Designation Granted to Sangamo Therapeutics Investigational CAR-Treg Cell Therapy TX200 for Solid Organ Transplantation
July 21, 2022 at 8:05 AM EDTPDF Version
BRISBANE, Calif.--(BUSINESS WIRE)--Jul. 21, 2022-- Sangamo Therapeutics, Inc. (Nasdaq: SGMO), a genomic medicine company, today announced that the European Commission (EC) has granted Orphan Medicinal Product Designation (OMPD) to TX200, a wholly-owned autologous Chimeric Antigen Receptor Regulatory T Cell (CAR-Treg) cell therapy product candidate for treatment in solid organ transplantation.
“Patients who have received a solid organ transplant require lifelong surveillance and chronic immunosuppressive medications to manage the risk of transplant rejection,” said Rob Schott, MD, MPH, FACC, Head of Development for Sangamo. “Our goal with TX200 is to create a transformative therapy that reduces the risk of organ rejection, while reducing the patient burden from chronic immunosuppressive therapy. Achieving this important regulatory milestone takes us one step closer to realizing that goal for patients.”
Dosing of the first patient in the STEADFAST Phase 1/2 clinical study took place in March 2022, with the second patient dosing planned later this quarter.
The EC granted OMPD to TX200 following a positive opinion from the European Medicines Agency’s Committee for Orphan Medicinal Products. To qualify for orphan designation, a treatment must be intended for a life-threatening or chronically debilitating disease affecting fewer than 5 in 10,000 people. Importantly, no satisfactory method of treatment must exist, or if such a method exists, the treatment must be of significant benefit to patients.
The OMPD status offers a range of incentives to encourage the development of orphan medicines, including protocol assistance on study protocols, potential fee reductions, and 10 years of market exclusivity upon regulatory approval.
About TX200
TX200 is a cell therapy composed of autologous regulatory T cells (Tregs) engineered to express an HLA-A2 Chimeric Antigen Receptor (CAR), with the aim of preventing immune-mediated rejection in HLA-A2 mismatched kidney transplants from a living donor. TX200 is intended to reduce the risk of transplant rejection by suppressing local inflammation and promoting immunological tolerance to the graft. TX200 is being assessed in HLA-A2 negative patients receiving a mismatched HLA-A2 positive kidney from a living donor. TX200 CAR-Treg cells are expected to localize to the graft and activate upon binding to the HLA-A2 antigen. Through their ability to regulate the immune system, TX200 cells may protect the graft from immune-mediated rejection and reduce or eliminate the need for lifelong treatment with immunosuppressants. The first patient in the ongoing STEADFAST Phase 1/2 study was dosed in March 2022.
About Sangamo Therapeutics
Sangamo Therapeutics is a clinical-stage biopharmaceutical company with a robust genomic medicines pipeline. Using ground-breaking science, including our proprietary zinc finger genome engineering technology and manufacturing expertise, Sangamo aims to create new genomic medicines for patients suffering from diseases for which existing treatment options are inadequate or currently don’t exist. For more information about Sangamo, visit www.sangamo.com.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220721005330/en/
Source: Sangamo Therapeutics, Inc.
Sangamo's TX200 gets orphan drug tag in EU for use in organ transplant
Jul. 21, 2022 8:30 AM ET
Sangamo Therapeutics, Inc. (SGMO)
By: Ravikash, SA News Editor1 Comment
The European Commission (EC) granted orphan medicinal product designation to Sangamo Therapeutics' (NASDAQ:SGMO) CAR-Treg cell therapy TX200 for treatment in solid organ transplantation.
- https://seekingalpha.com/news/3859037-sangamos-tx200-gets-orphan-drug-tag-in-eu-for-use-in-organ-transplant
- https://seekingalpha.com/symbol/SGMO
- https://www.sangamo.com/programs/
biotecHOPE™ 2022
Eltanexor (KPT-8602)
Eltanexor (KPT-8602)
Eltanexor (KPT-8602)
Karyopharm Granted Regulatory Designations for Eltanexor for the Treatment of Myelodysplastic Syndromes
– FDA Fast Track Designation and European Commission Orphan Medicinal Product Designation Underscore the Significant Need for New Treatment Options for MDS –
NEWTON, Mass., July 20, 2022 /PRNewswire/ -- Karyopharm Therapeutics Inc. (Nasdaq: KPTI), a commercial-stage pharmaceutical company pioneering novel cancer therapies, today announced new regulatory designations for eltanexor, a novel oral, Selective Inhibitor of Nuclear Export (SINE) investigational compound being studied for the treatment of myelodysplastic syndromes (MDS): (i) the U.S. Food and Drug Administration (FDA) has granted fast track designation for the development program of eltanexor as monotherapy for the treatment of patients with relapsed or refractory intermediate, high-, or very high-risk MDS; (ii) the European Commission (EC) adopted the Committee for Orphan Medicinal Products (COMP) opinion to designate eltanexor as an orphan medicinal product for the treatment of MDS in the European Union (EU). Karyopharm also received orphan drug designation from the FDA in January 2022. MDS are a group of diseases characterized by ineffective production of the components of the blood due to poor bone marrow function with a risk of progression to acute myeloid leukemia.
Karyopharm is currently investigating eltanexor in an ongoing open-label Phase 1/2 study in patients with relapsed/refractory MDS. Previously, Karyopharm reported initial data from the Phase 1 portion of this study evaluating single-agent eltanexor in patients with hypomethylating agent (HMA)-refractory MDS.
Approximately 15,000 people in the U.S.1 and 14,000 people in the EU2 are expected to be diagnosed with intermediate-to-high risk MDS in 2022. HMAs are the current standard of care for newly diagnosed, higher-risk MDS patients. However, only 40-60% of patients respond, with these responses typically lasting less than two years.3 The prognosis in HMA-refractory disease is poor, with a median overall survival of four to six months.4,5 There are currently no approved therapies for HMA- refractory MDS.
"These recent designations from the FDA and EC reinforce eltanexor's potential to improve clinical outcomes for patients with relapsed/refractory MDS," said Richard Paulson, President and Chief Executive Officer of Karyopharm. "We are dedicated to advancing our ongoing clinical trials and remain committed to bringing eltanexor to these patients and their families as a new treatment option."
Fast track is a process designed by the FDA to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need. The purpose is to get important new drugs to the patient earlier. Fast Track addresses a broad range of serious conditions. Once a drug receives Fast Track designation, early and frequent communication between the FDA and the drug company is encouraged throughout the entire drug development and review process.
Orphan Medicinal Product Designation is granted by the EC to promote the development of drugs that target rare (less than 5 in 100,000 people across the EU), seriously debilitating and/or life-threatening diseases, and are expected to provide a significant benefit over existing authorized treatments. Orphan designation qualifies a company for certain incentives that apply across all stages of drug development, including the potential for ten years of market exclusivity following marketing approval, fee reductions, and eligibility for orphan drug grants.
About Eltanexor
Eltanexor (KPT-8602) is an investigational novel SINE compound that functions by binding with, and inhibiting, the nuclear export protein, XPO1, leading to the accumulation of tumor suppressor proteins in the cell nucleus. This reinitiates and amplifies their tumor suppressor function and is believed to lead to the selective induction of apoptosis in cancer cells, while largely sparing normal cells.
In preclinical models, eltanexor has a broad therapeutic window with minimal penetration of the blood brain barrier and, therefore, has the potential to serve as another SINE compound for cancer indications. Following oral administration, animals treated with eltanexor show lower percentage of body weight loss and improved food consumption than animals similarly treated with selinexor. This allows more frequent dosing of eltanexor, enabling a longer period of exposure than is possible with selinexor.
Eltanexor is an investigational medicine and has not been approved by the United States Food and Drug Administration or any other regulatory agency.
About Karyopharm Therapeutics
Karyopharm Therapeutics Inc. (Nasdaq: KPTI) is a commercial-stage pharmaceutical company pioneering novel cancer therapies. Since its founding, Karyopharm has been the industry leader in oral Selective Inhibitor of Nuclear Export (SINE) compound technology, which was developed to address a fundamental mechanism of oncogenesis: nuclear export dysregulation. Karyopharm's lead SINE compound and first-in-class, oral exportin 1 (XPO1) inhibitor, XPOVIO® (selinexor), is approved in the U.S. and marketed by the Company in three oncology indications and has received regulatory approvals in various indications in a growing number of ex-U.S. territories and countries, including Europe and the United Kingdom (as NEXPOVIO®) and China. Karyopharm has a focused pipeline targeting multiple high unmet need cancer indications, including in multiple myeloma, endometrial cancer, myelodysplastic syndromes and myelofibrosis. For more information about our people, science and pipeline, please visit www.karyopharm.com, and follow us on Twitter at @Karyopharm and LinkedIn.
SOURCE Karyopharm Therapeutics Inc.
Karyopharm cancer therapy eltanexor gets FDA fast track status, orphan drug tag in EU
Jul. 20, 2022 8:31 AM ET
Karyopharm Therapeutics Inc. (KPTI)
By: Ravikash, SA News Editor
- Karyopharm Therapeutics (NASDAQ:KPTI) said eltanexor was granted fast track designation by the U.S. Food and Drug Administration (FDA) as monotherapy to treat patients with relapsed or refractory intermediate, high-, or very high-risk myelodysplastic syndromes (MDS).
- https://seekingalpha.com/news/3858479-karyopharm-cancer-drug-eltanexor-gets-fda-fast-track-status-orphan-drug-tag-in-eu
- https://www.karyopharm.com/pipeline/oral-eltanexor/
- https://www.karyopharm.com/
- https://seekingalpha.com/symbol/KPTI
Olverembatinib
Eltanexor (KPT-8602)
Eltanexor (KPT-8602)
Innovent and Ascentage Pharma Announce the China NMPA Accepted and Granted Priority Review Designation to a New Drug Application for Olverembatinib for the Treatment of Drug-Resistant CML
Published on: Jul 20th, 2022
SUZHOU, China, SAN FRANCISCO, CA. and ROCKVILLE, MD., U.S., Jul 19, 2022 — Innovent Biologics, Inc. (“Innovent”) (HKEX: 01801), a world-class biopharmaceutical company that develops, manufactures and commercializes high quality medicines for the treatment of oncology, metabolic, autoimmune, ophthalmology and other major diseases, and Ascentage Pharma (6855.HK), a global biopharmaceutical company engaged in developing novel therapies for cancers, chronic hepatitis B (CHB), and age-related diseases, today announce that the Center for Drug Evaluation (CDE) of China National Medical Products Administration (NMPA) has accepted and granted Priority Review designation (in a CDE’s public notice ended on July 18, 2022) to a New Drug Application (NDA) that will support the full approval of olverembatinib in patients with chronic-phase chronic myeloid leukemia (CML-CP) who are resistant and/or intolerant of first- and second-generation tyrosine kinase inhibitors (TKIs). Following the conditional NDA approval in November 2021, the acceptance for the latest application marks another milestone and will potentially bring olverembatinib to benefit a broader population of patients with CML. Innovent and Ascentage are mutually committed to the commercialization of olverembatinib in the China market.
In November 2021, the NMPA granted a conditional approval to olverembatinib for the treatment of adult patients with TKI-resistant CML-CP or CML-AP harboring the T315I mutation as confirmed by a validated diagnostic test, thus filling an urgent treatment gap that has long hindered the clinical outcome in Chinese patients with TKI-resistant CML harboring the T315I mutation.
The acceptance and Priority Review designation for this application are based on the results from an open-label, randomized, controlled, confirmatory Phase II pivotal study (study code: HQP1351CC203) which previously served as the basis for a Breakthrough Therapy designation to olverembatinib by the CDE in March 2021. The study is designed to evaluate the efficacy and safety of olverembatinib in patients with CML-CP who are resistant and/or intolerant to first- and second-generation TKIs, with the event-free survival (EFS) as its primary endpoint. A total of 144 patients were enrolled and randomized to either receive olverembatinib or the control group to receive the current best available treatment (BAT). Results show that olverembatinib significantly improved the EFS compared to the control group and has met the pre-specified superiority criteria. Detailed results from this study will be released at an upcoming academic conference.
CML is a hematologic malignancy of the white blood cells. The introduction of BCR-ABL TKIs has significantly improved the clinical practice and management of CML. However, acquired resistance to TKIs remains a major challenge in the treatment of CML. BCR-ABL tyrosine kinase mutations represent a key mechanism of acquired drug resistance and there is an urgent unmet medical need for a safe and effective treatment. Olverembatinib is a potentially global best-in-class drug that has been developed by Ascentage Pharma and supported by the National Major New Drug Discovery and Manufacturing Program in China. As the first and only third-generation BCR-ABL inhibitor approved for the treatment of drug-resistant CML in China, olverembatinib is able to effectively target a spectrum of BCR-ABL mutants, including T315I.
The leading principal investigator of olverembatinib in China, Prof. Xiaojun Huang, MD, Director of the Institute of Hematology, Peking University, Director of the Hematology Department at Peking University People’s Hospital, commented: “The approval for olverembatinib last year has brought a breakthrough therapy for patients with drug-resistant CML harboring the T315I mutation. Meanwhile, many patients who are resistant to first- and second-generation TKIs still lack effective treatment and drug resistance to TKIs and this remains a major clinical challenge in the treatment of CML. In recent years, results from multiple clinical studies have validated olverembatinib’s therapeutic efficacy in CML patients. We hope that the second Priority Review designation granted to olverembatinib will allow more patients with CML to soon benefit from this novel drug.”
Dr. Hui Zhou, Senior Vice President of Innovent, stated: “We are pleased about the acceptance and Priority Review designation for the application for olverembatinib, as it will potentially allow a broader population of patients with TKI-resistant CML to benefit from this novel therapeutic. Innovent has established a robust pipeline and franchise in hematology and we are fully committed to bringing forth more ‘high-quality biopharmaceutical products that are affordable to ordinary people’ and serve the unmet medical needs from Chinese patients as early as possible.”
Dr. Yifan Zhai, Chief Medical Officer of Ascentage Pharma, commented, “As an innovative biopharmaceutical company dedicated to addressing the unmet medical needs of patients in China and around the world, Ascentage Pharma is forging ahead with its clinical development programs to allow more patients to benefit from our innovative drugs. Having this application for olverembatinib accepted and granted the Priority Review designation by the CDE highlights the authority’s commitment to filling the treatment gap in patients with drug-resistant CML and its strong recognition of olverembatinib’s therapeutic efficacy. We will work closely with the CDE to bring this innovative therapeutic to more patients as soon as possible.”
About Chronic Myeloid Leukemia
Chronic myeloid leukemia (CML) is a malignancy caused by the clonal proliferation of hematopoietic stem cell in the bone marrow. Also referred to as chronic myelocytic leukemia, CML is one of the most common subtypes of chronic leukemia, accounting for 15% of all leukemia cases in adults. According to epidemiology data, the onset of CML in Chinese patients happens at a younger age than that in the West; the median age of onset of CML in China is around 45 – 50 years old, while it is 67 years old in the west.
BCR-ABL TKIs have significantly improved the clinical management of CML. However, acquired resistance to TKIs remains a major challenge in the treatment of CML, while BCR-ABL tyrosine kinase mutations represent a key mechanism of acquired drug resistance.
About Olverembatinib
Developed by Ascentage Pharma with support from the National Major New Drug Discovery and Manufacturing Program in China, the orally active, third-generation BCR-ABL inhibitor olverembatinib is the first China-approved third-generation BCR-ABL inhibitor targeting drug-resistant CML. Olverembatinib can effectively target a spectrum of BCR-ABL mutants, including the T315I mutation.
In November 2021, olverembatinib was approved by the NMPA of China for the treatment of adult patients with TKI-resistant CML-CP or CML-AP harboring the T315I mutation as confirmed by a validated diagnostic test. In March 2021, it was granted the Breakthrough Therapy designation by the CDE for the treatment of patients with CML-CP who are resistant and/or intolerant of first- and second-generation TKIs.
In overseas, olverembatinib was cleared by the US FDA in July 2019 to directly enter a Phase Ib study. Since 2018, the clinical results of olverembatinib have been selected for oral presentations at the American Society of Hematology (ASH) Annual Meetings for four consecutive years, and was nominated for “Best of ASH” in 2019. To date, olverembatinib has been granted one Fast Track designation and three Orphan Drug designations from the US FDA for the treatment of CML, acute lymphoblastic leukemia (ALL), and acute myeloid leukemia (AML); and one Orphan Designation from the European Medicines Agency (EMA) of the European Union for the treatment of CML.
In July 2021, Ascentage Pharma (6855.HK) and Innovent Biologics (1801.HK) reached the agreement regarding the joint development and commercialization of olverembatinib in China.
*Olverembatinib has not been approved for any indication in the U.S.
About Innovent
Inspired by the spirit of "Start with Integrity, Succeed through Action,” Innovent’s mission is to develop, manufacture and commercialize high-quality biopharmaceutical products that are affordable to ordinary people. Established in 2011, Innovent is committed to developing, manufacturing and commercializing high-quality innovative medicines for the treatment of cancer, autoimmune, metabolic, ophthalmology and other major diseases. On October 31, 2018, Innovent was listed on the Main Board of the Stock Exchange of Hong Kong Limited with the stock code: 01801.HK.
Since its inception, Innovent has developed a fully integrated multi-functional platform which includes R&D, CMC (Chemistry, Manufacturing, and Controls), clinical development and commercialization capabilities. Leveraging the platform, the company has built a robust pipeline of 32 valuable assets in the fields of cancer, metabolic, autoimmune disease and other major therapeutic areas, with 7 products approved for marketing in China – TYVYT® (sintilimab injection), BYVASDA® (bevacizumab biosimilar injection), SULINNO® (adalimumab biosimilar injection), HALPRYZA® (rituximab biosimilar injection) , Pemazyre® (pemigatinib oral inhibitor) , olverembatinib (BCR-ABL TKI) and Cyramza® (ramucirumab), 3 assets under NMPA NDA review, 3 assets in Phase 3 or pivotal clinical trials, and an additional 19 molecules in clinical studies.
Innovent has built an international team with advanced talent in high-end biological drug development and commercialization, including many global experts. The company has also entered into strategic collaborations with Eli Lilly and Company, Adimab, Incyte, MD Anderson Cancer Center, Hanmi and other international partners. Innovent strives to work with many collaborators to help advance China’s biopharmaceutical industry, improve drug availability and enhance the quality of the patients’ lives. For more information, please visit: www.innoventbio.com. and www.linkedin.com/company/innovent-biologics/.
Note:
TYVYT® (sintilimab injection) is not an approved product in the United States.
BYVASDA® (bevacizumab biosimilar injection), SULINNO®, and HALPRYZA® (rituximab biosimilar injection) are not approved products in the United States.
TYVYT® (sintilimab injection, Innovent)
BYVASDA® (bevacizumab biosimilar injection, Innovent)
HALPRYZA® (rituximab biosimilar injection, Innovent)
SULINNO® (adalimumab biosimilar injection, Innovent)
Pemazyre® (pemigatinib oral inhibitor, Incyte Corporation). Pemazyre® was discovered by Incyte Corporation and licensed to Innovent for development and commercialization in Mainland China, Hong Kong, Macau and Taiwan.
CYRAMZA® (ramucirumab, Eli Lilly). Cyramza® was discovered by Eli Lilly and licensed to Innovent for commercialization in Mainland China.
About Ascentage Pharma
Ascentage Pharma (6855.HK) is a globally focused biopharmaceutical company engaged in developing novel therapies for cancers, chronic hepatitis B, and age-related diseases. On October 28, 2019, Ascentage Pharma was listed on the Main Board of the Stock Exchange of Hong Kong Limited with the stock code 6855.HK.
Ascentage Pharma focuses on developing therapeutics that inhibit protein-protein interactions to restore apoptosis, or programmed cell death. The company has built a pipeline of eight clinical drug candidates, including novel, highly potent Bcl-2, and dual Bcl-2/Bcl-xL inhibitors, as well as candidates aimed at IAP and MDM2-p53 pathways, and next-generation tyrosine kinase inhibitors (TKIs). Ascentage Pharma is also the only company in the world with active clinical programs targeting all three known classes of key apoptosis regulators. The company is conducting more than 50 Phase I/II clinical trials in the US, Australia, Europe, and China. Olverembatinib, the company's core drug candidate developed for the treatment of drug-resistant chronic myeloid leukemia (CML), was granted Priority Review status and a Breakthrough Therapy Designation (BTD) by the Center for Drug Evaluation (CDE) of the China National Medical Products Administration (NMPA) and is already approved for the indication. In addition, olverembatinib was also granted an Orphan Drug Designation (ODD) and a Fast Track Designation (FTD) by the US FDA, and an Orphan Designation by the EU. To date, Ascentage Pharma has obtained a total of 15 ODDs, 2 FTDs, and 2 Rare Pediatric Disease (RPD) designations from the FDA and 1 ODD from the EU for four of the company's investigational drug candidates. Ascentage Pharma has been designated for multiple Major National R&D Projects, including 5 National Major New Drug Discovery and Manufacturing projects, 1 New Drug Incubator status, 4 Innovative Drug Programs, and 1 Major Project for the Prevention and Treatment of Infectious Diseases.
Leveraging its robust R&D capabilities, Ascentage Pharma has built a portfolio of global intellectual property rights and entered into global partnerships with numerous renowned biotechnology and pharmaceutical companies and research institutes such as UNITY Biotechnology, MD Anderson Cancer Center, Mayo Clinic, Dana-Farber Cancer Institute, Merck, AstraZeneca, and Pfizer. The company has built a talented team with global experience in discovering, developing, launching, and commercializing innovative drugs and is setting up world-class commercial manufacturing and Sales & Marketing teams. One pivotal aim of Ascentage Pharma is to continuously strengthen its R&D capabilities and accelerate its clinical development programs, in order to fulfil its mission of addressing unmet clinical needs in China and around the world for the benefit of more patients.
Innovent, Ascentage's cancer drug gets priority review in China for expanded use
Jul. 20, 2022 5:04 AM ET
Innovent Biologics, Inc. (IVBIY)
By: Ravikash, SA News Editor
- China's National Medical Products Administration (NMPA) granted priority review designation to Innovent Biologics (OTCPK:IVBIY) and Ascentage Pharma's application seeking full approval of olverembatinib to treat patients with chronic-phase chronic myeloid leukemia (CML-CP) who are resistant and/or intolerant of first- and second-generation tyrosine kinase inhibitors (TKIs).
- https://seekingalpha.com/news/3858381-innovent-ascentage-cancer-drug-get-priority-review-in-china-for-expanded-use
- https://seekingalpha.com/symbol/IVBIY
- https://www.innoventbio.com/
- https://www.ascentage.com/science/pipeline/
INNOVENT BIOLOGICS, INC. (1801)
https://www.hkex.com.hk/Market-Data/Securities-Prices/Equities/Equities-Quote?sym=1801&sc_lang=en
AVR-RD-05
Eltanexor (KPT-8602)
Cabozantinib in Combination with Nivolumab and Ipilimumab
AVROBIO Receives Orphan Drug Designation from the U.S. Food and Drug Administration for AVR-RD-05, a Gene Therapy for Mucopolysaccharidosis Type II (MPSII) or Hunter Syndrome
AVR-RD-05 is the fourth AVROBIO gene therapy to receive orphan drug designation
FDA previously granted rare pediatric disease designation for AVR-RD-05
CAMBRIDGE, Mass.--(BUSINESS WIRE)--Jul. 13, 2022-- AVROBIO, Inc. (Nasdaq: AVRO), a leading clinical-stage gene therapy company with a shared purpose to free people from a lifetime of genetic disease, today announced that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation for AVR-RD-05, its gene therapy for the treatment of mucopolysaccharidosis type II (MPSII), or Hunter syndrome, a rare and seriously debilitating lysosomal disorder that primarily affects young boys.
Orphan drug designation is granted by FDA to drugs and biologics that are intended for the safe and effective treatment, diagnosis or prevention of rare diseases or conditions that affect fewer than 200,000 people in the U.S. Orphan drug designation provides certain incentives, which may include tax credits towards the cost of clinical trials and prescription drug user fee waivers.
Hunter syndrome is caused by a deficiency in the lysosomal enzyme iduronate-2-sulfatase (IDS), which is essential for breaking down large sugar molecules. The gene therapy uses a patient’s own hematopoietic stem cells (HSCs) that are transduced ex vivo with a lentiviral vector encoding the human IDS enzyme. The company’s planned collaborator-sponsored Phase 1/2 clinical trial for Hunter syndrome is expected to commence in 2023 under the company’s collaboration with the University of Manchester, UK. The program was developed by Brian Bigger, Ph.D., professor of cell and gene therapy at the University of Manchester, who has previously published preclinical data demonstrating that HSC gene therapy deploying an optimized, proprietary tag has the potential to correct peripheral disease and normalize brain pathology.
About AVROBIO
Our vision is to bring personalized gene therapy to the world. We aim to prevent, halt or reverse disease throughout the body with a single dose of gene therapy designed to drive durable expression of therapeutic protein, even in hard-to-reach tissues and organs including brain, muscle and bone. AVROBIO’s pipeline is powered by our industry-leading plato® gene therapy platform, our foundation designed to deliver gene therapy worldwide. It includes clinical programs in cystinosis and Gaucher disease type 1, as well as preclinical programs in Gaucher disease type 3, Hunter syndrome and Pompe disease. We are headquartered in Cambridge, Mass. For additional information, visit avrobio.com, and follow us on Twitter and LinkedIn.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220713005196/en/
Source: AVROBIO, Inc.
AVROBIO granted FDA’s orphan drug designation for metabolic disorder therapy
Jul. 13, 2022 7:25 AM ET
By: Dulan Lokuwithana, SA News Editor
- The shares of gene therapy company AVROBIO (NASDAQ:AVRO) jumped 9% in the pre-market Wednesday after the company announced that the FDA awarded the orphan drug designation for AVR-RD-05, a gene therapy candidate for mucopolysaccharidosis type II (MPSII), or Hunter syndrome.
- https://seekingalpha.com/news/3856326-avro-stock-gains-on-fdas-orphan-drug-status-for-metabolic-disorder-therapy
- https://seekingalpha.com/symbol/AVRO
- https://www.avrobio.com/our-pipeline
Cabozantinib in Combination with Nivolumab and Ipilimumab
Cabozantinib in Combination with Nivolumab and Ipilimumab
Cabozantinib in Combination with Nivolumab and Ipilimumab
Exelixis Announces Cabozantinib in Combination with Nivolumab and Ipilimumab Significantly Improved Progression-Free Survival in Phase 3 COSMIC-313 Pivotal Trial in Patients with Previously Untreated Advanced Kidney Cancer
– Exelixis intends to discuss the results with the U.S. FDA to determine next steps toward a potential regulatory submission –
– Trial to continue until the next analysis of the secondary endpoint of overall survival –
ALAMEDA, Calif.--(BUSINESS WIRE)--Jul. 11, 2022-- Exelixis, Inc. (Nasdaq: EXEL) today announced that COSMIC-313 met its primary endpoint, demonstrating significant improvement in progression-free survival (PFS) at the primary analysis. COSMIC-313 is an ongoing phase 3 pivotal trial evaluating the combination of cabozantinib (CABOMETYX®), nivolumab and ipilimumab versus the combination of nivolumab and ipilimumab in patients with previously untreated advanced intermediate- or poor-risk renal cell carcinoma (RCC). At a prespecified interim analysis for the secondary endpoint of overall survival (OS), the combination of cabozantinib, nivolumab and ipilimumab versus the combination of nivolumab and ipilimumab did not demonstrate a significant benefit. Therefore, the trial will continue to the next analysis of OS.
“As the treatment landscape continues to evolve, resulting in more options for advanced kidney cancer, there is still a need for additional effective first-line treatment options for patients with intermediate- or poor-risk disease,” said Toni Choueiri, M.D., Director of the Lank Center for Genitourinary Oncology at Dana-Farber Cancer Institute and the Jerome and Nancy Kohlberg Professor of Medicine at Harvard Medical School. “These initial findings from COSMIC-313 suggest that the triplet combination of cabozantinib, nivolumab and ipilimumab may have potential to serve as an additional option for this patient population.”
In the primary analysis of PFS per Response Evaluation Criteria in Solid Tumors version 1.1, as assessed by Blinded Independent Radiology Committee, cabozantinib in combination with nivolumab and ipilimumab significantly reduced the risk of disease progression or death compared with the combination of nivolumab and ipilimumab (hazard ratio: 0.73; 95% confidence interval: 0.57-0.94; P=0.01). The safety profile observed in the trial was reflective of the known safety profiles for each single agent, as well as the combination regimens used in this study. No new safety signals were identified.
Exelixis intends to discuss the results with the U.S. Food & Drug Administration (FDA) to determine next steps toward a potential regulatory submission for the combination regimen for patients with previously untreated advanced intermediate- or poor-risk RCC. Detailed findings will be submitted for presentation at a future medical meeting.
“COSMIC-313 is the first trial to show that a tyrosine kinase inhibitor added to dual checkpoint inhibition can improve progression-free survival in patients with advanced kidney cancer,” said Vicki L. Goodman, M.D., Executive Vice President, Product Development & Medical Affairs, and Chief Medical Officer, Exelixis. “With these findings in hand, we look forward discussing the results with the FDA and presenting the data at a future medical meeting.”
About COSMIC-313
COSMIC-313 is a multicenter, randomized, double-blinded, controlled phase 3 pivotal trial that enrolled 855 patients at 177 sites globally. Patients were randomized 1:1 into the experimental or control arms of the study. Patients in the experimental arm received cabozantinib (40 mg, once daily) in combination with nivolumab (3 mg/kg infusion, once every 3 weeks for 4 doses total) and ipilimumab (1 mg/kg infusion, once every 3 weeks for 4 doses total) followed by cabozantinib (40 mg, once daily) and nivolumab (480 mg/kg flat dose infusion, once every 4 weeks for up to 2 years). Patients in the control arm received cabozantinib-matched placebo in combination with nivolumab (3 mg/kg infusion, once every 3 weeks for 4 doses total) and ipilimumab (1 mg/kg infusion, once every 3 weeks for 4 doses total) followed by cabozantinib-matched placebo and nivolumab (480 mg/kg flat dose infusion, once every 4 weeks for up to 2 years). The primary endpoint is PFS; the secondary endpoint is OS. Exelixis is funding the trial, and Bristol Myers Squibb is providing nivolumab and ipilimumab for use in this trial. More information about this trial is available at ClinicalTrials.gov.
About CABOMETYX® (cabozantinib)
In the U.S., CABOMETYX tablets are approved for the treatment of patients with advanced RCC; for the treatment of patients with hepatocellular carcinoma who have been previously treated with sorafenib; for patients with advanced RCC as a first-line treatment in combination with nivolumab; and for adult and pediatric patients 12 years of age and older with locally advanced or metastatic differentiated thyroid cancer that has progressed following prior VEGFR-targeted therapy and who are radioactive iodine-refractory or ineligible. CABOMETYX tablets have also received regulatory approvals in the European Union and additional countries and regions worldwide. In 2016, Exelixis granted Ipsen Pharma SAS exclusive rights for the commercialization and further clinical development of cabozantinib outside of the U.S. and Japan. In 2017, Exelixis granted exclusive rights to Takeda Pharmaceutical Company Limited for the commercialization and further clinical development of cabozantinib for all future indications in Japan. Exelixis holds the exclusive rights to develop and commercialize cabozantinib in the U.S.
CABOMETYX in combination with nivolumab and ipilimumab is not indicated as a treatment for previously untreated advanced RCC.
About Exelixis
Founded in 1994, Exelixis, Inc. (Nasdaq: EXEL) is a commercially successful, oncology-focused biotechnology company that strives to accelerate the discovery, development and commercialization of new medicines for difficult-to-treat cancers. Following early work in model system genetics, we established a broad drug discovery and development platform that has served as the foundation for our continued efforts to bring new cancer therapies to patients in need. Our discovery efforts have resulted in four commercially available products, CABOMETYX® (cabozantinib), COMETRIQ® (cabozantinib), COTELLIC® (cobimetinib) and MINNEBRO® (esaxerenone), and we have entered into partnerships with leading pharmaceutical companies to bring these important medicines to patients worldwide. Supported by revenues from our marketed products and collaborations, we are committed to prudently reinvesting in our business to maximize the potential of our pipeline. We are supplementing our existing therapeutic assets with targeted business development activities and internal drug discovery — all to deliver the next generation of Exelixis medicines and help patients recover stronger and live longer. Exelixis is a member of the Standard & Poor’s (S&P) MidCap 400 index, which measures the performance of profitable mid-sized companies. For more information about Exelixis, please visit www.exelixis.com, follow @ExelixisInc on Twitter or like Exelixis, Inc. on Facebook.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220710005054/en/
Source: Exelixis, Inc.
Exelixis says phase 3 trial evaluating its kidney cancer combo treatment met main goal
Jul. 11, 2022 9:54 AM ETExelixis, Inc. (EXEL)By: Anuron Mitra, SA News Editor2 Comments
- Exelixis (NASDAQ:EXEL) on Monday said its phase 3 trial evaluating its cabozantinib medicine in combination with two other cancer drugs for the treatment of kidney cancer met its main goal.
- https://seekingalpha.com/news/3855690-exelixis-says-phase-3-trial-evaluating-its-kidney-cancer-combo-treatment-met-main-goal
- https://seekingalpha.com/symbol/EXEL
- https://www.cabometyx.com/
TUKYSA® (tucatinib) in Combination with Trastuzumab
Cabozantinib in Combination with Nivolumab and Ipilimumab
TUKYSA® (tucatinib) in Combination with Trastuzumab
Seagen Announces Results from Pivotal MOUNTAINEER Trial Demonstrating Clinically Meaningful Antitumor Activity of TUKYSA® (tucatinib) in Combination with Trastuzumab in Previously Treated HER2-Positive Metastatic Colorectal Cancer
07/02/2022
–Phase 2 trial showed chemotherapy-free TUKYSA combination resulted in clinically meaningful and durable tumor responses–
–Results presented in late-breaking oral session at the ESMO World Congress on Gastrointestinal Cancer–
BOTHELL, Wash.--(BUSINESS WIRE)-- Seagen Inc. (Nasdaq:SGEN) today announced full results from the pivotal phase 2 MOUNTAINEER trial, which showed TUKYSA® (tucatinib) in combination with trastuzumab was well-tolerated with durable responses in patients with previously treated HER2-positive metastatic colorectal cancer (mCRC). These late-breaking data were presented in an oral session at the European Society for Medical Oncology (ESMO) World Congress on Gastrointestinal Cancer on July 2 in Barcelona, Spain.
“Patients with chemotherapy-refractory HER2-positive metastatic colorectal cancer receive limited clinical benefit with currently available therapies,” said John H. Strickler, M.D., Associate Professor of Medicine, Duke University School of Medicine and lead trial investigator. “With sustained responses and favorable tolerability in heavily pretreated patients, tucatinib in combination with trastuzumab has the potential to be a new treatment option for previously treated HER2-positive mCRC.”
“This study has shown the benefits of dual-HER2 inhibition with tucatinib and trastuzumab in patients with HER2-positive metastatic colorectal cancer, including many whose cancer had spread to the liver or lungs before joining the trial,” said Roger Dansey, M.D., interim CEO and Chief Medical Officer, Seagen. “We believe this chemotherapy-free combination may play an important role in addressing the unmet needs of patients with this disease.”
At a median duration of follow-up of 20.7 months (interquartile range: 11.7, 39.0), results of the MOUNTAINEER trial showed a 38.1% confirmed objective response rate (cORR) (95% Confidence Interval [CI]: 27.7, 49.3) per blinded independent central review (BICR) in the HER2-positive patients who were assigned to receive tucatinib in combination with trastuzumab (n=84 with a median age of 55.0 years [range 24 to 77]). In these patients, the median duration of response (DoR) per BICR was 12.4 months (95% CI: 8.5, 20.5). Median progression-free survival per BICR was 8.2 months (95% CI: 4.2, 10.3), and median overall survival was 24.1 months (95% CI: 20.3, 36.7). At study entry, 64.3% and 70.2% of these patients had liver or lung metastases, respectively, and had received a median of 3.0 (1, 6) prior lines of systemic therapy.
In a cohort of patients who received tucatinib monotherapy (n=30), the ORR per BICR by 12 weeks was 3.3% (95% CI: 0.1, 17.2) and the disease control rate was 80.0%. Participants who did not respond to tucatinib monotherapy by 12 weeks or progressed at any time had the option to receive the combination of tucatinib and trastuzumab.
The most common (greater than or equal to 20%) treatment-emergent adverse events (AEs) in patients assigned to receive tucatinib and trastuzumab (n=86) were diarrhea (Grade 1 or 2: 60.5%, Grade 3: 3.5%), fatigue (Grade 1 or 2: 41.9%, Grade 3: 2.3%), nausea (Grade 1 or 2: 34.9%) and infusion-related reaction (Grade 1 or 2: 20.9%). The most common Grade ≥3 AE was hypertension (Grade 3: 7.0%). AEs leading to discontinuation of any treatment occurred in 5.8% of patients. No deaths due to AEs were reported. Please see Important Safety Information at the end of this press release for further safety information regarding tucatinib.
Data from this trial will form the basis of a planned supplemental New Drug Application to the U.S. Food and Drug Administration under the Accelerated Approval Program. Merck, known as MSD outside the U.S. and Canada, has exclusive rights to commercialize TUKYSA in regions outside of the U.S., Canada and Europe and plans to discuss these results with certain global health authorities.
About MOUNTAINEER
MOUNTAINEER is a U.S. and European multicenter, open-label, randomized phase 2 clinical trial of tucatinib in combination with trastuzumab or as a single agent that enrolled 117 patients with HER2-positive metastatic or unresectable colorectal cancer following previous standard-of-care therapies. MOUNTAINEER began as a U.S. investigator-sponsored trial and initially consisted of a single cohort (Cohort A) of patients who received tucatinib (300 mg) twice per day orally in combination with trastuzumab intravenously (8 mg/kg loading dose, then 6 mg/kg every three weeks thereafter). The trial was then expanded globally to include patients who were randomized to receive tucatinib plus trastuzumab (Cohort B) or tucatinib monotherapy (Cohort C).
The primary endpoint of the trial is confirmed objective response rate by RECIST (Response Evaluation Criteria in Solid Tumors) version 1.1 criteria per blinded independent central review in patients receiving the combination of tucatinib and trastuzumab (Cohorts A and B). Duration of response, progression-free survival, overall survival and safety and tolerability of the combination regimen are secondary objectives.
About TUKYSA
TUKYSA is an oral medicine that is a tyrosine kinase inhibitor of the HER2 protein. In vitro (in lab studies), TUKYSA inhibited phosphorylation of HER2 and HER3, resulting in inhibition of downstream MAPK and AKT signaling and cell growth (proliferation), and showed anti-tumor activity in HER2-expressing tumor cells. In vivo (in living organisms), TUKYSA inhibited the growth of HER2-expressing tumors. The combination of TUKYSA and the anti-HER2 antibody trastuzumab showed increased anti-tumor activity in vitro and in vivo compared to either medicine alone.
TUKYSA is approved in 36 countries. It was approved by the U.S. FDA in April 2020 and by the European Medicines Agency and the UK Medicines and Healthcare Products Regulatory Agency in February 2021. Merck, known as MSD outside the U.S. and Canada, has exclusive rights to commercialize TUKYSA in Asia, the Middle East and Latin America and other regions outside of the U.S., Canada and Europe.
U.S. Indication and Important Safety Information
TUKYSA is indicated in combination with trastuzumab and capecitabine for treatment of adult patients with advanced unresectable or metastatic HER2-positive breast cancer, including patients with brain metastases, who have received one or more prior anti-HER2-based regimens in the metastatic setting.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220702005001/en/
Source: Seagen Inc.
Seagen's Tukysa garners promising results in mid-stage colorectal cancer trial
Jul. 05, 2022 11:59 AM ET
By: Jonathan Block, SA News Editor
Seagen (NASDAQ:SGEN) has reported positive results in a mid-stage trial for Tukysa (tucatinib) in metastatic colorectal cancer.
- https://seekingalpha.com/news/3854241-seagen-tukysa-garners-promising-results-in-mid-stage-colorectal-cancer-trial
- https://seekingalpha.com/symbol/SGEN
- https://www.tukysa.com/
- https://www.seagen.com/
CAR-T Candidate BNT211
Cabozantinib in Combination with Nivolumab and Ipilimumab
TUKYSA® (tucatinib) in Combination with Trastuzumab
BioNTech Receives Priority Medicines (PRIME) Designation from EMA for Enhanced Regulatory Support of CAR-T Candidate BNT211 in Testicular Cancer
- First BioNTech product candidate to receive priority medicines (PRIME) designation by the European Medicines Agency for enhanced regulatory support facilitating the clinical development of the investigational cell therapy candidate BNT211 in the third- or later-line setting in patients with heavily pretreated testicular cancer
- Designation follows positive interim Phase 1/2 data for BNT211 demonstrating an encouraging safety profile and early signs of anti-tumor activity in testicular cancer patients
- BNT211 combines two innovative approaches in one regimen, an autologous chimeric antigen receptor (CAR) T cell therapy targeting the oncofetal antigen Claudin-6 (CLDN6) and a CLDN6-encoding CAR-T cell amplifying RNA vaccine (CARVac) to improve persistence and functionality of the adoptively transferred cells
- The European Medicines Agency’s priority medicines status is granted to drug candidates that may offer a major therapeutic advantage over existing treatments, or benefit patients without treatment options
MAINZ, Germany, June 23, 2022 (GLOBE NEWSWIRE) – BioNTech SE (Nasdaq: BNTX, “BioNTech” or “the Company”) today announced that that the European Medicines Agency (EMA) has granted Priority Medicines (PRIME) designation to BioNTech’s fully owned product candidate BNT211 for the third- or later-line treatment of testicular germ cell tumors. BNT211 is a potential first-in-class therapeutic approach which comprises a synergistic combination of two of the Company’s proprietary drug products, an autologous chimeric antigen receptor (CAR) T cell therapy targeting the oncofetal antigen Claudin-6 (CLDN6) and a CLDN6-encoding CAR-T cell amplifying RNA vaccine (CARVac). The product candidate is currently being investigated in an ongoing Phase 1/2 study (NCT04503278; 2019-004323-20) that aims to evaluate the safety and preliminary efficacy in heavily pretreated patients with relapsed or refractory advanced solid tumors.
“Patients with relapsed or treatment refractory testicular cancers have a poor prognosis with limited remaining treatment options. The PRIME designation underlines the potential of our approach in this high medical need setting. Our approach brings together several new elements: Firstly, targeting CLDN6, a pan-cancer cell surface marker, secondly, our CAR design, and thirdly, “remote control” of CAR T cells by our uridine RNA-lipoplex based vaccine. We believe that a combination of engineered T cells and mRNA vaccines in one treatment regimen can stimulate and expand T cells. This could enable us to develop truly powerful precision immunotherapies,” said Prof. Özlem Türeci, M.D., Co-Founder and Chief Medical Officer at BioNTech. “With the PRIME status and support by the EMA, we aim to expedite the further development of the BNT211 program to bring a novel therapeutic option for patients with life-threatening testicular cancer, and thus to extend the successes of CAR-T therapy also to hard-to-treat solid tumors.”
The designation is based on positive preliminary Phase 1/2 data from the ongoing study that was presented at the AACR Annual Meeting in April 2022. The results demonstrated that treatment with CLDN6 CAR-T alone or in combination with CARVac was well tolerated and showed encouraging signs of anti-tumor activity in testicular cancer patients at the first evaluated dose levels. In the study all six patients with heavily pretreated testicular cancer eligible for efficacy analysis showed clinical benefits highlighting the potential of this novel approach. One patient achieved a complete response 18 weeks after infusion. Three patients achieved a partial response and showed deepening and durability of responses (one of them in the lowest CAR-T dose level cohort in combination with CARVac). One patient had stable disease with shrinkage of target lesions.
The PRIME scheme is a regulatory mechanism introduced by the EMA that provides early and proactive support to developers of promising medicines, to optimize development plans and speed up evaluations so these medicines can reach patients faster. The goal is to help patients benefit as early as possible from innovative new therapies that have demonstrated the potential to significantly address an unmet medical need.
About BNT211
Aiming to harness the power of cell therapies for solid cancers and to overcoming hurdles to date, BioNTech has combined their CAR-T and FixVac platform technologies to develop a highly tumor-specific CAR-T cell therapy product which is consecutively enhanced by a CAR-T Cell Amplifying RNA Vaccine (CARVac) that is based on BioNTech`s mRNA-lipoplex technology and encodes for the respective CAR-T target antigen. The CARVac is based on BioNTech’s backbone-optimized uridine mRNA (uRNA)-lipoplex technology which through its inherent adjuvant function enables a potent T cell stimulation to improve persistence and functionality of the adoptively transferred CAR-T cells, thus enabling and maintaining a therapeutic effect even at low CAR-T doses. BNT211 is an investigational CAR-T cell therapy directed against the novel oncofetal antigen Claudin-6 (CLDN6), a target discovered by BioNTech founders and expressed on multiple solid tumors such as ovarian cancer, sarcoma, testicular cancer, endometrial cancer and gastric cancer. The program is currently being evaluated in a first-in-human Phase 1/2 trial as a monotherapy and in combination with a CLDN6-encoding CARVac, aiming to boost persistence and functionality of the CLDN6-CAR-T cells, in patients with CLDN6-positive relapsed or refractory advanced solid tumors.
About BioNTech
Biopharmaceutical New Technologies (BioNTech) is a next generation immunotherapy company pioneering novel therapies for cancer and other serious diseases. The Company exploits a wide array of computational discovery and therapeutic drug platforms for the rapid development of novel biopharmaceuticals. Its broad portfolio of oncology product candidates includes individualized and off-the-shelf mRNA-based therapies, innovative chimeric antigen receptor T cells, bispecific checkpoint immuno-modulators, targeted cancer antibodies and small molecules. Based on its deep expertise in mRNA vaccine development and in-house manufacturing capabilities, BioNTech and its collaborators are developing multiple mRNA vaccine candidates for a range of infectious diseases alongside its diverse oncology pipeline. BioNTech has established a broad set of relationships with multiple global pharmaceutical collaborators, including Genmab, Sanofi, Genentech, a member of the Roche Group, Regeneron, Genevant, Fosun Pharma and Pfizer.
For more information, please visit www.BioNTech.com
BioNTech testicular cancer candidate receives priority designation from EMA
Jun. 23, 2022 11:23 AM ET
By: Jonathan Block, SA News Editor1 Comment
- The European Medicines Agency has awarded priority medicines designation (PRIME) to BioNTech's (NASDAQ:BNTX) CAR-T therapy BNT211 for testicular cancer.
- https://seekingalpha.com/news/3851282-biontech-testicular-cancer-candidate-receives-priority-designation-from-ema
- https://seekingalpha.com/symbol/BNTX
- https://www.biontech.com/int/en/home.html
- https://www.nasdaq.com/market-activity/stocks/bntx/dividend-history
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Ionis announces eplontersen met co-primary and secondary endpoints in interim analysis of the Phase 3 NEURO-TTRansform study for hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN)
June 21, 2022 at 2:00 AM EDT
- Eplontersen showed statistically significant and clinically meaningful improvements in mNIS+7 and Norfolk QoL-DN
- Eplontersen demonstrated a favorable safety profile
- Ionis and AstraZeneca expect to file a New Drug Application this year
CARLSBAD, Calif., June 21, 2022 /PRNewswire/ -- Ionis Pharmaceuticals, Inc. (Nasdaq: IONS) today announced positive topline results from a 35-week interim analysis of the Phase 3 NEURO-TTRansform study of Ionis and AstraZeneca's eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN). Eplontersen demonstrated a statistically significant and clinically meaningful change from baseline for the co-primary endpoints of percent change in serum transthyretin (TTR) concentration and the modified Neuropathy Impairment Score +7 (mNIS+7), a measure of neuropathic disease progression, versus the historical placebo group. Eplontersen also met its key secondary endpoint of change from baseline in the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy (Norfolk QoL-DN), showing treatment with eplontersen significantly improved patient-reported quality of life versus the historical placebo group.
In the study, eplontersen demonstrated a favorable safety and tolerability profile with no specific concerns. The study data are consistent with the clinical profile seen across Ionis' other LICA programs, further validating how advancements in the company's LIgand-Conjugated Antisense technology position Ionis to deliver potentially transformative treatments for a range of unmet medical needs.
Based on these study results, the companies will seek regulatory approval for eplontersen for ATTRv-PN and plan to file a new drug application with the U.S. Food and Drug Administration this year.
"These encouraging data reinforce the safety profile of eplontersen and demonstrate clear evidence of its potential to provide much needed therapeutic benefit to patients living with hereditary transthyretin-mediated amyloid polyneuropathy," said Teresa Coelho, M.D., a neurologist and neurophysiologist at Hospital Santo António, Centro Hospitalar Universitário do Porto, Portugal and an investigator for the NEURO-TTRansform study.
"We are pleased that the data in the NEURO-TTRansform study demonstrate eplontersen had a positive impact on disease progression, including improvement in neuropathy impairment and quality of life in a substantial number of patients. These highly statistically significant and clinically meaningful results put us on the cusp of providing a new therapeutic option for polyneuropathy patients living with this debilitating and fatal disease," said Eugene Schneider, M.D., Ionis' executive vice president and chief clinical development officer. "We are grateful to the patients, families and clinicians who are participating in NEURO-TTRansform. Without their commitment the eplontersen program would not have progressed as successfully as it has."
The data from the 35-week interim analysis will be presented at an upcoming medical meeting later this year.
As part of a global development and commercialization agreement between Ionis and AstraZeneca, eplontersen is being jointly developed and commercialized by both companies in the U.S. and will be developed and commercialized in the rest of the world by AstraZeneca (with the exception of Latin America).
Eplontersen was granted Orphan Drug Designation in the U.S. It is also currently being evaluated in the Phase 3 CARDIO-TTRansform study for amyloid transthyretin cardiomyopathy (ATTR-CM), a systemic, progressive and fatal condition that leads to progressive heart failure and death within four years from diagnosis.
For more information on the NEURO-TTRansform study, please visit: https://clinicaltrials.gov/ct2/show/NCT04136184.
About the NEURO-TTRansform Study
NEURO-TTRansform is a global, open-label, randomized study evaluating the efficacy and safety of eplontersen in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN). The study has enrolled adult patients with stage 1 or stage 2 polyneuropathy and will compare efficacy of eplontersen to the historical placebo arm from the TEGSEDI® (inotersen) NEURO-TTR registrational study that Ionis completed in 2017. The final primary endpoint analysis will be completed at week 66 and all patients will be followed until week 85 when they will have the option to transition into the open label extension study.
The co-primary efficacy endpoints at week 66 are:
- Percent change from baseline in serum TTR concentration
- Change from baseline in the modified Neuropathy Impairment Score +7 (mNIS+7), a measure of neuropathic disease progression
- Change from baseline in the Norfolk Quality of Life Questionnaire-Diabetic Neuropathy (Norfolk QoL-DN)
About Eplontersen
Eplontersen is an investigational antisense medicine that uses Ionis' advanced LIgand-Conjugated Antisense, or LICA, technology designed to inhibit the production of the transthyretin (TTR) protein at its source. Eplontersen, which is planned to be delivered to patients via an autoinjector, is in development to treat all types of ATTR, a systemic, progressive and fatal disease.
About Ionis Pharmaceuticals, Inc.
For more than 30 years, Ionis has been the leader in RNA-targeted therapy, pioneering new markets and changing standards of care with its novel antisense technology. Ionis currently has three marketed medicines and a premier late-stage pipeline highlighted by industry-leading cardiovascular and neurological franchises. Our scientific innovation began and continues with the knowledge that sick people depend on us, which fuels our vision of becoming a leading, fully integrated biotechnology company.
To learn more about Ionis, visit www.ionispharma.com and follow us on Twitter @ionispharma.
View original content to download multimedia:https://www.prnewswire.com/news-releases/ionis-announces-eplontersen-met-co-primary-and-secondary-endpoints-in-interim-analysis-of-the-phase-3-neuro-ttransform-study-for-hereditary-transthyretin-mediated-amyloid-polyneuropathy-attrv-pn-301571475.html
SOURCE Ionis Pharmaceuticals, Inc.
AstraZeneca/Ionis rare disease drug shows positive data in late stage study
Jun. 21, 2022 5:01 AM ET
Ionis Pharmaceuticals, Inc. (IONS), AZN
By: Ravikash, SA News Editor4 Comments
AstraZeneca (NASDAQ:AZN) and Ionis Pharmaceuticals (NASDAQ:IONS) said they would seek regulatory approval for eplontersen in the U.S. after the drug showed clinically meaningful changes on the co-primary goals of a phase 3 trial in patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN).
https://seekingalpha.com/symbol/IONS
https://seekingalpha.com/symbol/AZN
https://www.ionispharma.com/medicines/akcea-ttr-l/
elivaldogene autotemcel (eli-cel)
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
FDA Advisory Committee Unanimously Endorses eli-cel Gene Therapy for Cerebral Adrenoleukodystrophy
If approved, eli-cel will be the first and only gene therapy for the treatment of early active CALD, a rare neurodegenerative disease that primarily affects young children and leads to irreversible loss of neurologic function and death
PDUFA goal date is set for September 16, 2022
SOMERVILLE, Mass.--(BUSINESS WIRE)--Jun. 9, 2022--
bluebird bio, Inc. (Nasdaq: BLUE) today announced the outcome of the U.S. Food and Drug Administration’s (FDA) Cellular, Tissue, and Gene Therapies Advisory Committee (CTGTAC) discussion of elivaldogene autotemcel (eli-cel) for the treatment of early active cerebral adrenoleukodystrophy (CALD) in patients less than 18 years of age who do not have an available and willing human leukocyte antigen (HLA)-matched sibling hematopoietic stem cell (HSC) donor.
On the question “Do the benefits of eli-cel outweigh the risks, for the treatment of any sub-population of children with early active cerebral adrenoleukodystrophy (CALD)?” the CTGTAC voted 15 (yes) to 0 (no).
“For decades, the CALD community has fought for the opportunity to stave off the rapid, irreversible decline associated with this devastating disease,” said Andrew Obenshain, chief executive officer, bluebird bio. “Today we are one step closer to delivering a potentially lifesaving therapy for CALD. We are grateful to the families, clinicians and committee members who participated in today’s advisory committee discussion and remain committed to working with the FDA as it completes its review of the eli-cel Biologics License Application.”
CALD is a rare, progressive, neurodegenerative disease that primarily affects young boys and causes behavioral, cognitive, and neurological deficits. Nearly half of patients who do not receive treatment die within five years of symptom onset. Allogeneic hematopoietic stem cell transplant (allo-HSCT) is currently the only effective treatment option but is associated with serious potential complications and mortality that increase in patients without a matched sibling donor. If approved, eli-cel will be the first approved gene therapy to address the underlying genetic cause of disease for patients living with CALD in the U.S. – offering the more than 70% of patients diagnosed with CALD who do not have a matched sibling donor an alternative to allo-HSCT.
The committee’s recommendation is based on the Biologics License Application (BLA) currently under priority review by the FDA with a PDUFA goal date set for September 16, 2022. The BLA for eli-cel is supported by efficacy and safety data from the completed Phase 2/3 Starbeam study (ALD-102) (N=32). Additionally, the BLA contains data for 35 subjects dosed in the Phase 3 ALD-104 study. In clinical studies, patients treated with eli-cel were more likely to achieve both overall and event-free survival than allo-HSCT patients without a matched sibling donor, with the clearest benefit for patients without a matched donor of any type.
The eli-cel clinical program was placed on a clinical hold following a Suspected Unexpected Serious Adverse Reaction (SUSAR) of myelodysplastic syndrome (MDS) in August 2021. Consistent with this known risk, two additional cases of MDS have subsequently been reported. All patients who received eli-cel in the clinical program continue to be closely monitored, per study protocols.
The CTGTAC also discussed the overall safety of lentiviral vector (LVV) gene therapies, concluding in a 13 to 1 vote that the safety data from lovo-cel for sickle cell disease is not relevant to the review of eli-cel. In addition to granting eli-cel BLA priority review, the FDA previously granted eli-cel Orphan Drug status, Rare Pediatric Disease designation, and Breakthrough Therapy designation. bluebird bio is eligible to receive a priority review voucher upon potential approval of eli-cel.
Tomorrow, June 10, 2022, the CTGTAC will convene to discuss the efficacy and safety of betibeglogene autotemcel (beti-cel), an investigational LVV gene therapy for patients with beta-thalassemia who require regular red blood cell transfusions.
About elivaldogene autotemcel (eli-cel) gene therapy
eli-cel (pronounced ELL ee cell) uses ex vivo transduction with the Lenti-D lentiviral vector (LVV) to add functional copies of the ABCD1 gene into a patient’s own hematopoietic stem cells (HSCs). The addition of the functional ABCD1 gene allows patients to produce the ALD protein (ALDP), which is thought to facilitate the breakdown of very long-chain fatty acids (VLCFAs). The expression of ALDP and effect of eli-cel is expected to be life-long. The goal of treatment with eli-cel is to stop the progression of CALD and, consequently, preserve as much neurological function as possible, including the preservation of motor function and communication ability. Importantly, with eli-cel, there is no need for donor HSCs from another person.
bluebird bio’s clinical development program for eli-cel includes the completed pivotal Phase 2/3 Starbeam study (ALD-102) and the ongoing Phase 3 ALD-104 study, which has completed enrollment and treatment of all patients. Additionally, bluebird bio is conducting a long-term safety and efficacy follow-up study (LTF-304) for patients who have received eli-cel for CALD and completed two years of follow-up in ALD-102 or ALD-104. Enrollment into studies of eli-cel is currently on hold with the FDA and follow-up of all patients continues, per protocol.
In ALD-102, 90.6% (29/32) of patients met the primary endpoint of Major Functional Disabilities (MFD)-free survival at 24 months. As previously reported, two patients withdrew from study ALD-102 at investigator discretion, and one additional subject experienced rapid disease progression early after treatment, resulting in MFDs and subsequent death. All patients who completed ALD-102 enrolled in a long-term follow-up study (LTF-304). The median duration of follow-up is approximately four years (49 months; 13.4, 88.1).
Adverse reactions attributed to eli-cel observed in clinical trials include myelodysplastic syndrome, viral cystitis, pancytopenia, and nausea and vomiting. There have been no reports of graft-versus-host-disease, graft failure or rejection, transplant-related mortality, or replication competent lentivirus in the 67 patients who received eli-cel in clinical studies (ALD-102, ALD-104, LTF-304).
About bluebird bio, Inc.
bluebird bio is pursuing curative gene therapies to give patients and their families more bluebird days.
With a dedicated focus on severe genetic diseases, bluebird has industry-leading clinical and research programs for sickle cell disease, beta-thalassemia and cerebral adrenoleukodystrophy and is advancing research to apply new technologies to these and other diseases. We custom design each of our therapies to address the underlying cause of disease and have developed in-depth and effective analytical methods to understand the safety of our lentiviral vector technologies and drive the field of gene therapy forward.
Founded in 2010, bluebird has the largest and deepest ex-vivo gene therapy data set in the world—setting the standard for industry. Today, bluebird continues to forge new paths, combining our real-world experience with a deep commitment to patient communities and a people-centric culture that attracts and grows a diverse flock of dedicated birds.
For more information, visit bluebirdbio.com or follow us on social media at @bluebirdbio, LinkedIn, Instagram and YouTube.
Lenti-D and bluebird bio are trademarks of bluebird bio, Inc.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220609006060/en/
Source: bluebird bio, Inc.
Bluebird bio neuro disorder gene therapy gets FDA panel nod, awaits meeting on another
Jun. 10, 2022 5:35 AM ET
By: Ravikash, SA News Editor1 Comment
Bluebird bio (NASDAQ:BLUE) said a panel of the U.S. Food and Drug Administration (FDA) voted in favor of its gene therapy candidate elivaldogene autotemcel (eli-cel) for cerebral adrenoleukodystrophy (CALD).
The company's stock had been halted for trading by Nasdaq on June 9 for 2 days (including today) ahead of the FDA committee meeting.
Inaxaplin (VX-147)
Eplontersen, formerly known as IONIS-TTR-LRx and AKCEA-TTR-LRx
Inaxaplin (VX-147)
BackPDF VersionJun 8, 2022
Vertex Announces Inaxaplin (VX-147) Granted Breakthrough Therapy Designation by U.S. FDA and Priority Medicines (PRIME) Designation by the EMA
- Vertex granted nine Breakthrough Therapy Designations and three PRIME designations across its pipeline programs to date –
BOSTON--(BUSINESS WIRE)--Jun. 8, 2022-- Vertex Pharmaceuticals Incorporated (Nasdaq: VRTX) today announced the U.S. Food and Drug Administration (FDA) has granted inaxaplin (VX-147) Breakthrough Therapy Designation for APOL1-mediated focal segmental glomerulosclerosis (FSGS) and the European Medicines Agency (EMA) has granted inaxaplin Priority Medicines (PRIME) designation for APOL1-mediated chronic kidney disease (AMKD). Inaxaplin is the first investigational therapy aimed at treating the underlying cause of AMKD.
The FDA's Breakthrough Therapy Designation is intended to expedite development and review of medicines that aim to address a serious condition with preliminary clinical evidence indicating that the drug may demonstrate substantial improvement over existing treatments on one or more clinically significant endpoints. The Breakthrough Therapy Designation was granted based on the Phase 2 clinical study of inaxaplin in patients with APOL1-mediated FSGS, a form of AMKD.
The EMA’s PRIME designation is a regulatory mechanism that provides early and proactive support to developers of promising medicines, to optimize the generation of robust data and enable accelerated assessment so these medicines can potentially reach patients faster. The goal of PRIME is to help patients benefit as early as possible from innovative new therapies that have the potential to significantly address an unmet medical need. PRIME designation was granted based on clinical proof-of-concept data from Vertex’s Phase 2 study of inaxaplin in APOL1-mediated FSGS. Inaxaplin is only the second nephrology product to be granted PRIME designation.
Vertex now holds three of the approximately 70 non-oncological PRIME designations granted to date, including its two PRIME designations for exagamglogene autotemcel (exa-cel), formerly known as CTX001, one for transfusion-dependent beta thalassemia and one for sickle cell disease. In the US, this is the ninth breakthrough therapy designation granted to Vertex across its portfolio programs.
About the Inaxaplin (VX-147) Pivotal Program
A randomized, double-blind, placebo-controlled Phase 2/3 adaptive study is ongoing and will first evaluate two doses of inaxaplin for 12 weeks to select a dose for Phase 3 and subsequently evaluate the efficacy and safety of the single, selected dose in the Phase 3 portion of the study.
Patients aged 18 to 60 years, with two APOL1 mutations, urine protein to creatinine ratio (UPCR) ≥0.7 g/g to <10 g/g, estimated glomerular filtration rate (eGFR) ≥25 to <75 mL/min/1.73m2 and on stable doses of standard of care medications are eligible to enroll. Approximately 66 patients are planned to be enrolled in the Phase 2 dose-ranging portion of the study, and approximately 400 additional patients are planned to be enrolled in the Phase 3 portion of the study.
The primary efficacy endpoint for the final analysis is eGFR slope in patients receiving the inaxaplin selected dose compared to placebo. The secondary efficacy endpoint is time to composite clinical outcome, which will also be assessed at the final analysis and is defined as a sustained decline of ≥30% from baseline in eGFR, the onset of end-stage kidney disease (i.e., maintenance dialysis for ≥28 days, kidney transplantation, or a sustained eGFR of <15 mL/min/1.73 m2), or death. The final study analysis will occur when subjects have at least two years of eGFR data and when approximately 187 composite clinical outcomes have occurred.
The study is also designed to have a pre-planned interim analysis at Week 48 evaluating eGFR slope, supported by a percent change from baseline in UPCR in the inaxaplin arm versus placebo. If positive, the interim analysis may serve as the basis for Vertex to seek accelerated approval of inaxaplin in the U.S. for patients with AMKD.
About Vertex
Vertex is a global biotechnology company that invests in scientific innovation to create transformative medicines for people with serious diseases. The company has multiple approved medicines that treat the underlying cause of cystic fibrosis (CF) — a rare, life-threatening genetic disease — and has several ongoing clinical and research programs in CF. Beyond CF, Vertex has a robust pipeline of investigational small molecule, cell and genetic therapies in other serious diseases where it has deep insight into causal human biology, including sickle cell disease, beta thalassemia, APOL1-mediated kidney disease, pain, type 1 diabetes, alpha-1 antitrypsin deficiency and Duchenne muscular dystrophy.
Founded in 1989 in Cambridge, Mass., Vertex's global headquarters is now located in Boston's Innovation District and its international headquarters is in London. Additionally, the company has research and development sites and commercial offices in North America, Europe, Australia and Latin America. Vertex is consistently recognized as one of the industry's top places to work, including 12 consecutive years on Science magazine's Top Employers list and one of the 2021 Seramount (formerly Working Mother Media) 100 Best Companies. For company updates and to learn more about Vertex's history of innovation, visit www.vrtx.com or follow us on Facebook, Twitter, LinkedIn, YouTube and Instagram.
View source version on businesswire.com: https://www.businesswire.com/news/home/20220608005181/en/
Source: Vertex Pharmaceuticals Incorporated
Vertex wins key FDA and EU designations for kidney disease drug
Jun. 08, 2022 8:26 AM ET
Vertex Pharmaceuticals Incorporated (VRTX)
By: Dulan Lokuwithana, SA News Editor2 Comments
- Vertex Pharmaceuticals (NASDAQ:VRTX) announced on Wednesday that U.S. and European regulators issued key designations for its kidney disease candidate inaxaplin (VX-147) that would enable the company to speed up its regulatory work.
- https://seekingalpha.com/news/3846657-vrtx-stock-gains-on-fda-and-eu-designations-for-kidney-disease-drug
- https://seekingalpha.com/symbol/VRTX
BCX9250
Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
Inaxaplin (VX-147)
FDA Grants Fast Track Designation for BioCryst’s ALK-2 Inhibitor, BCX9250
RESEARCH TRIANGLE PARK, N.C., June 08, 2022 (GLOBE NEWSWIRE) -- BioCryst Pharmaceuticals, Inc. (Nasdaq: BCRX) today announced the U.S. Food and Drug Administration (FDA) has granted Fast Track designation for BCX9250 for the prevention of heterotopic ossification (HO) in patients with fibrodysplasia ossificans progressiva (FOP).
According to the FDA, the purpose of the Fast Track designation is to get important new drugs to patients earlier by facilitating the development, and expediting the review, of drugs to treat serious conditions and fill an unmet medical need. Companies that receive this designation are eligible for benefits including more frequent meetings with and written communication from the FDA, eligibility for accelerated approval and priority review, if relevant criteria are met, and rolling review of the new drug application (NDA).
“We are pleased with the FDA’s decision to grant Fast Track designation to BCX9250, as there is a significant unmet need among patients living with FOP. With this designation following the EMA’s recent decision to grant PRIME eligibility for BCX9250 in Europe, we believe the non-clinical data and the first-in-human Phase 1 safety, tolerability and pharmacokinetics study in healthy subjects support the potential of our ALK-2 inhibitor program to be a meaningful therapeutic advance for the FOP community,” said Dr. Helen Thackray, chief research and development officer of BioCryst.
FOP is an ultra-rare, severely disabling genetic disorder characterized by HO, or the irregular formation of bone outside the normal skeleton. HO can occur in muscles, tendons, ligaments and other connective tissues. Patients with FOP become bound by this irregular ossification over time, with restricted movement and fused joints, resulting in deformities, restricted mobility and premature mortality.
BCX9250 is designed to inhibit the ALK-2 enzyme, which is a part of the normal signaling pathway for bone formation and responds to binding its specific ligands (bone morphogenic proteins, BMPs) by stimulating normal bone growth and renewal in healthy children and adults. Specific activating mutations of the ALK-2 gene are seen in all cases of FOP. An activating mutation in ALK-2 is necessary for the disease to occur, making the ALK-2 enzyme an ideal drug target for treatment of FOP.
In a Phase 1 clinical trial in healthy subjects, BCX9250 was safe and well tolerated at all doses studied, with linear and dose-proportional exposure supporting the potential for once-daily dosing.
About BioCryst Pharmaceuticals
BioCryst Pharmaceuticals discovers novel, oral, small-molecule medicines that treat rare diseases in which significant unmet medical needs exist and an enzyme plays a key role in the biological pathway of the disease. Oral, once-daily ORLADEYO® (berotralstat) is approved in the United States and multiple global markets. BioCryst has several ongoing development programs including BCX9930, an oral Factor D inhibitor for the treatment of complement-mediated diseases, BCX9250, an ALK-2 inhibitor for the treatment of fibrodysplasia ossificans progressiva, and galidesivir, a potential treatment for Marburg virus disease and yellow fever. RAPIVAB® (peramivir injection) is approved in the U.S. and multiple global markets, with post-marketing commitments ongoing. For more information, please visit the company’s website at www.biocryst.com.
BioCryst nabs FDA’s Fast Track status for candidate targeting rare bone forming disorder
Jun. 08, 2022 10:01 AM ET
BioCryst Pharmaceuticals, Inc. (BCRX)
By: Dulan Lokuwithana, SA News Editor
- Commercial-stage biotech BioCryst Pharmaceuticals (NASDAQ:BCRX) announced on Wednesday that the FDA granted its Fast Track designation for BCX9250 for the prevention of heterotopic ossification (HO) in ultra-rare genetic disorder fibrodysplasia ossificans progressiva (FOP).
- https://seekingalpha.com/news/3846729-bcrx-stock-gains-on-fda-fast-track-status-for-drug-for-bone-forming-disorder
- https://seekingalpha.com/symbol/BCRX
- https://www.biocryst.com/our-pipeline/
Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
Jazz Pharmaceuticals Presents Positive Data from Phase 2/3 Trial of Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn) in Acute Lymphoblastic Leukemia or Lymphoblastic Lymphoma at the ASCO 2022 Annual Meeting
June 07, 2022
Oral presentation confirms patients achieved clinically meaningful nadir serum asparaginase activity throughout the course of Rylaze treatment with intramuscular dosing regimen administered 25/25/50 mg/m2 on Monday/Wednesday/Friday
DUBLIN, June 7, 2022 /PRNewswire/ -- Jazz Pharmaceuticals plc (Nasdaq: JAZZ) today announced positive results from a Phase 2/3 trial, developed and conducted in close collaboration with the Children's Oncology Group (COG), evaluating the intramuscular (IM) administration of Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn) in adult and pediatric patients with acute lymphoblastic leukemia (ALL) and lymphoblastic lymphoma (LBL) who have developed hypersensitivity to an E. coli-derived asparaginase. These results will be presented as an oral presentation today at the American Society of Clinical Oncology (ASCO) 2022 Annual Meeting.
These results confirm the interim trial analysis presented in December 2021 at the 63rd American Society of Hematology (ASH) Annual Meeting, and demonstrated that ≥90% of patients in Cohort 1c receiving the IM dosing regimen of 25/25/50 mg/m2 administered Monday/Wednesday/Friday (MWF) achieved nadir serum asparaginase activity (NSAA) levels ≥0.1 IU/mL at 48 and 72 hours, with a safety profile consistent with what has been described for other asparaginases.
"We are excited to share these results from the Phase 2/3 trial of Rylaze highlighting the clinically meaningful nadir serum asparaginase activity from the Monday/Wednesday/Friday dosing regimen, which supports a new dosing schedule that aligns with current clinical practice," said Rob Iannone, M.D., M.S.C.E., executive vice president, global head of research and development of Jazz Pharmaceuticals. "Rylaze is an example of how Jazz and the Children's Oncology Group have advanced a critically needed treatment from development through FDA approval, and then continue to explore additional dosing and administration options to address the needs of patients."
"Asparaginase-based therapies remain a cornerstone in ALL and LBL treatment, and Rylaze has been an important option for patients who develop a hypersensitivity to an E. coli-derived asparaginase since its approval last year," said trial primary investigator Dr. Luke Maese, associate professor of pediatric hematology-oncology at the University of Utah, Primary Children's Hospital and Huntsman Cancer Institute. "It's encouraging to see these data further support an IM Monday/Wednesday/Friday dosing schedule for Rylaze, which is more in line with clinical practice in the U.S., in addition to the currently approved schedule of every 48 hours."
Rylaze was approved in the U.S. in 2021 for use as a component of a multi-agent chemotherapeutic regimen for the treatment of ALL and LBL in adult and pediatric patients one month or older who have developed hypersensitivity to E. coli-derived asparaginase. It was approved with an IM dosing schedule of 25 mg/m2 every 48 hours based on observed data from the Phase 2/3 trial, in conjunction with data produced by a population pharmacokinetic (PPK) model. Data from the Phase 2/3 trial supported additional regulatory filings for Rylaze, including two supplemental Biologics Licensing Applications (sBLA) to the U.S. FDA to support MWF IM dosing completed in January 2022 and IV administration options completed in April 2022.
Trial Results
Data presented at ASCO include efficacy and safety results from the Phase 2/3 open-label, multicenter, pharmacokenitic (PK) trial of Rylaze (also known as JZP458) in patients with ALL/LBL who developed hypersensitivity or silent inactivation to a long-acting E. coli-derived asparaginase. These results are from Part A of the trial, which investigated three cohorts via IM administration:
- Cohort 1a (n=33): studied a dose of 25 mg/m2 Monday/Wednesday/Friday
- Cohort 1b (n=83): studied a dose of 37.5 mg/m2 Monday/Wednesday/Friday
- Cohort 1c (n=51): studied a dose of 25 mg/m2 on Monday and Wednesday and 50 mg/m2 on Friday
Efficacy Findings
The primary efficacy endpoint of the trial was the proportion of patients with NSAA levels ≥0.1 IU/mL at the last 72-hours during the first treatment course.
The key secondary endpoint was the proportion of patients with NSAA levels ≥0.1 IU/mL at the last 48-hours during the first treatment course.
A population PK (PPK) model was developed based on SAA data from the clinical trial to characterize the PK of JZP458 when given IM and to inform dosing decisions. Simulated data from the PPK model matched the observed data well.
Based on a PPK modeling and simulation analysis, the proportion of patients predicted to achieve NSAA levels ≥0.1 IU/mL with a 95% CI in Cohort 1c at the last 72- and 48-hour in Course 1 were 92% (91%, 93%) and 94% (93%, 95%) respectively, based on modeled data.
About Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
Rylaze, also known as JZP458, is approved in the U.S. for use as a component of a multi-agent chemotherapeutic regimen for the treatment of acute lymphoblastic leukemia (ALL) and lymphoblastic lymphoma (LBL) in adult and pediatric patients one month or older who have developed hypersensitivity to E. coli-derived asparaginase. Rylaze has orphan drug designation for the treatment of ALL/LBL in the United States. Rylaze is a recombinant erwinia asparaginase that uses a novel Pseudomonas fluorescens expression platform. JZP458 was granted Fast Track designation by the U.S. Food and Drug Administration (FDA) in October 2019 for the treatment of this patient population. Rylaze was approved as part of the Real-Time Oncology Review (RTOR) program, an initiative of the FDA's Oncology Center of Excellence designed for efficient delivery of safe and effective cancer treatments to patients.
The full U.S. Prescribing Information for Rylaze is available at: <https://pp.jazzpharma.com/pi/rylaze.en.USPI.pdf>
About Jazz Pharmaceuticals plc
Jazz Pharmaceuticals plc (Nasdaq: JAZZ) is a global biopharmaceutical company whose purpose is to innovate to transform the lives of patients and their families. We are dedicated to developing life-changing medicines for people with serious diseases –often with limited or no therapeutic options. We have a diverse portfolio of marketed medicines and novel product candidates, from early-to late-stage development, in neuroscience and oncology. Within these therapeutic areas, we are identifying new options for patients by actively exploring small molecules and biologics, and through innovative delivery technologies and cannabinoid science. Jazz is headquartered in Dublin, Ireland and has employees around the globe, serving patients in nearly 75 countries. For more information, please visit www.jazzpharmaceuticals.com and follow @JazzPharma on Twitter.

View original content to download multimedia:https://www.prnewswire.com/news-releases/jazz-pharmaceuticals-presents-positive-data-from-phase-23-trial-of-rylaze-asparaginase-erwinia-chrysanthemi-recombinant-rywn-in-acute-lymphoblastic-leukemia-or-lymphoblastic-lymphoma-at-the-asco-2022-annual-meeting-301562729.html
SOURCE Jazz Pharmaceuticals plc
Jazz's new dosing regimen of Rylaze as part of cancer chemotherapy shows promise in trial
Jun. 07, 2022 8:49 AM ET
Jazz Pharmaceuticals plc (JAZZ)
By: Ravikash, SA News Editor
Jazz Pharmaceuticals plc (NASDAQ:JAZZ) reported data from a phase 2/3 trial of a new dosing regimen of its therapy Rylaze (asparaginase erwinia chrysanthemi (recombinant)-rywn).
The results — which were presented at the American Society of Clinical Oncology (ASCO) meeting — were from Part A of the study, which included three groups.
https://seekingalpha.com/symbol/JAZZ
SEASONAL INFLUENZA VACCINE CANDIDATE (MRNA-1010)
Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
Rylaze® (asparaginase erwinia chrysanthemi (recombinant)-rywn)
MODERNA ANNOUNCES FIRST PARTICIPANTS DOSED IN PHASE 3 STUDY OF SEASONAL INFLUENZA VACCINE CANDIDATE (MRNA-1010)
mRNA-1010 is Moderna's first seasonal influenza vaccine candidate to enter a Phase 3 trial
mRNA-1010 is one of several influenza vaccine candidates being developed in Moderna's respiratory portfolio
Moderna now has four programs in Phase 3 studies: Omicron-containing bivalent COVID booster, influenza, RSV, CMV
CAMBRIDGE, MA / ACCESSWIRE / June 7, 2022 / Moderna, Inc. (NASDAQ:MRNA), a biotechnology company pioneering messenger RNA (mRNA) therapeutics and vaccines, today announced the first participants have been dosed in a Phase 3 study of the Company's seasonal influenza vaccine candidate (mRNA-1010). The trial is expected to enroll approximately 6,000 adults in Southern Hemisphere countries.
"We are pleased to begin this Phase 3 study of our seasonal influenza vaccine candidate, mRNA-1010, our fourth mRNA vaccine candidate to begin a pivotal Phase 3 study. mRNA-1010 is the first of several influenza vaccine candidates we are developing with the aim of iteratively improving traditional vaccines by inducing broad and robust immune responses. We believe our mRNA platform, with the flexibility and speed of our manufacturing process, is well-positioned to address the significant unmet need in seasonal flu, said Stéphane Bancel, Chief Executive Officer of Moderna. "Influenza vaccines are a key pillar in our respiratory vaccine strategy that includes the development of combination candidates targeting multiple viruses in a single vaccine, including influenza with SARS-CoV-2 and respiratory syncytial virus. With the start of dosing for its mRNA-1010 program, Moderna now has four programs in late stage Phase 3 studies, including its SARS-CoV-2 booster, RSV, seasonal flu and CMV vaccine candidates. Beginning in the fall of 2022, the Company's Phase 3 pipeline could lead to three respiratory commercial launches over the next two to three years."
This Phase 3 randomized, observer-blind study is designed to evaluate the safety and immunological non-inferiority of mRNA-1010 to a licensed seasonal influenza vaccine in adults 18 years and older. Participants will be randomly assigned on a 1:1 ratio to receive either a single dose of mRNA-1010 or a single dose of a licensed seasonal influenza vaccine as a comparator.
About mRNA-1010 & Seasonal Influenza
mRNA-1010 is a vaccine candidate that encodes for hemagglutinin (HA) glycoproteins of the four influenza strains recommended by the World Health Organization (WHO) for the prevention of influenza, including influenza A/H1N1, A/H3N2, and influenza B/Yamagata- and B/Victoria-lineages. HA is a major influenza surface glycoprotein that is considered an important target to generate broad protection against influenza and is the primary target of currently available influenza vaccines. Moderna is proactively preparing for a confirmatory efficacy study for mRNA-1010 as early as the 2022/2023 Northern Hemisphere influenza season, if needed.
Influenza (influenza A and influenza B) epidemics occur seasonally and vary in severity each year, causing respiratory illnesses and placing a substantial burden on healthcare systems. Worldwide, influenza leads to 3-5 million severe cases of influenza and 290,000-650,000 influenza-related respiratory deaths annually, despite the availability of current influenza vaccines. Although both influenza A and B cause seasonal epidemics, it is the influenza A viruses that lead to >95% of influenza-related hospitalization in adults.
Moderna's Respiratory Vaccine Program
Moderna is advancing a portfolio of respiratory candidates, including five influenza mRNA vaccine candidates. In addition to mRNA-1010, Moderna is developing influenza vaccine candidates that include additional HA antigens for broader coverage of circulating influenza A strains (mRNA-1011 and mRNA-1012), and vaccine candidates that incorporate both HA and neuraminidase (NA) antigens to target multiple proteins involved in the influenza virus lifecycle to reduce the potential of viral antigenic escape (mRNA-1020 and mRNA-1030).
Moderna is also developing two combination vaccine candidates, including a vaccine candidate against influenza and SARS-CoV-2 (mRNA-1073), and another candidate against influenza, SARS-CoV-2, and RSV (mRNA-1230). The goal of Moderna's combination vaccine candidates is to provide protection against multiple respiratory pathogens in a single vaccine.
About Moderna
In over 10 years since its inception, Moderna has transformed from a research-stage company advancing programs in the field of messenger RNA (mRNA), to an enterprise with a diverse clinical portfolio of vaccines and therapeutics across seven modalities, a broad intellectual property portfolio in areas including mRNA and lipid nanoparticle formulation, and an integrated manufacturing plant that allows for rapid clinical and commercial production at scale. Moderna maintains alliances with a broad range of domestic and overseas government and commercial collaborators, which has allowed for the pursuit of both groundbreaking science and rapid scaling of manufacturing. Most recently, Moderna's capabilities have come together to allow the authorized use and approval of one of the earliest and most effective vaccines against the COVID-19 pandemic.
Moderna's mRNA platform builds on continuous advances in basic and applied mRNA science, delivery technology and manufacturing, and has allowed the development of therapeutics and vaccines for infectious diseases, immuno-oncology, rare diseases, cardiovascular diseases and auto-immune diseases. Moderna has been named a top biopharmaceutical employer by Science for the past seven years. To learn more, visit www.modernatx.com.
Moderna has been named a top biopharmaceutical employer by Science for the past seven years. To learn more, visit www.modernatx.com.
Moderna begins dosing in phase 3 trial of influenza vaccine mRNA-1010
Jun. 07, 2022 10:52 AM ET
By: Ravikash, SA News Editor5 Comments
- Moderna (NASDAQ:MRNA) said the first participants were dosed in a phase 3 trial of its seasonal influenza vaccine mRNA-1010.
- https://seekingalpha.com/news/3846333-moderna-begins-dosing-in-phase-3-trial-of-influenza-vaccine-mrna-1010
- https://seekingalpha.com/symbol/MRNA
- https://investors.modernatx.com/overview/default.aspx
- https://clinicaltrials.gov/ct2/show/NCT04956575
Copyright © 2018 seeking biotech alpha - All Rights Reserved. City Photos from Pixabay
Powered by GoDaddy Website Builder
- biotecMAX
- bioHazzard2023-10
- bioHazard2022-9
- biohazard2022-8
- BioHazard2022-7
- BioHazard2021-6
- BioHazard2021-5
- biohazard2021-4
- BioHazard2020-3
- BioHazard2020-2
- BioHazard2020-1
- BioHazard2020-0
- 2023-6
- 2022/23-5
- 2022-4
- 2022-3
- 2021-2
- biotecHOPE-5
- biotecHOPE-4
- biotecHOPE-3
- biotecHOPE-1
- biotecHEART
- medicines
- biotecNOVA-4
- biotecNOVA-3
- biotecNOVA 2
- BiotecNOVA 1
- BiotecWARS
- blogs
- about